Professional Documents
Culture Documents
Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth Asphyxia
Uploaded by
Agus WijataOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth Asphyxia
Uploaded by
Agus WijataCopyright:
Available Formats
0031-3998/01/4904-0502
PEDIATRIC RESEARCH
Copyright 2001 International Pediatric Research Foundation, Inc.
Vol. 49, No. 4, 2001
Printed in U.S.A.
Early Biochemical Indicators of Hypoxic-Ischemic
Encephalopathy after Birth Asphyxia
NICOLE NAGDYMAN, WOLFGANG KMEN, HAE-KYUNG KO, CHRISTIAN MLLER, AND
MICHAEL OBLADEN
Department of Neonatology [N.N., W.K., H.-K.K., M.O.] and Institute of Laboratory Medicine [C.M.],
Charit University Hospital, Humboldt University Berlin, 13353 Berlin, Germany
ABSTRACT
Hypoxic-ischemic encephalopathy (HIE) after perinatal asphyxia is a condition in which serum concentrations of brainspecific biochemical markers may be elevated. Neuroprotective
interventions in asphyxiated newborns require early indicators of
brain damage to initiate therapy. We examined brain-specific
creatine kinase (CK-BB), protein S-100, and neuron-specific
enolase in cord blood and 2, 6, 12, and 24 h after birth in 29
asphyxiated and 20 control infants. At 2 h after birth, median
(quartiles) serum CK-BB concentration was 10.0 U/L (6.0 13.0
U/L) in control infants, 16.0 U/L (13.0 23.5 U/L) in infants with
no or mild HIE, and 46.5 U/L (21.4 83.0 U/L) in infants with
moderate or severe HIE. Serum protein S-100 was 1.6 g/L
(1.4 2.5 g/L) in control infants, 2.9 g/L (1.8 4.7 g/L) in
asphyxiated infants with no or mild HIE, and 17.0 g/L (3.2
34.1 g/L) in infants with moderate or severe HIE 2 h after birth.
No significant difference was detectable in serum neuron-specific
Perinatal asphyxia is a common cause of neonatal morbidity
and mortality and neurologic disabilities among survivors. In
addition to pulmonary, renal, and cardiac dysfunction, HIE
develops in one third of asphyxiated newborns (1). Mild
encephalopathy carries a good prognosis, although in moderate
and severe encephalopathy the risk of death or neurologic
sequelae increases greatly (2). Neuroprotective interventions
are increasingly in the forefront of interest and have been
shown to be effective in animal models. For clinical intervention, it is important to identify infants at a high risk for brain
damage soon after birth and within the therapeutic window (3).
Several indicators of brain damage have been investigated in
the last decade (4 10). We examined the serum levels of three
different brain proteins during the first day of life after birth
asphyxia. Protein S-100 is a dimeric acidic calcium-binding
protein constituting a major component of the cytosol of
various cell types. Protein S-100B ( subunits) and S-100A1
( subunits) are predominantly present in astrocytes and
Received April 6, 2000; accepted October 17, 2000.
Correspondence and reprint requests: Nicole Nagdyman, M.D., Department of Neonatology, Charit University Hospital, Humboldt University Berlin, Augustenburger Platz 1,
13353 Berlin, Germany; e-mail: nicole.nagdyman@charite.de
enolase between infants with no or mild and moderate or severe
HIE 2 and 6 h after birth. A combination of serum protein S-100
(cutoff value, 8.5 g/L) and CK-BB (cutoff value, 18.8 U/L) 2 h
after birth had the highest predictive value (83%) and specificity
(95%) of predicting moderate and severe HIE. Cord blood pH
(cutoff value, 6.9) and cord blood base deficit (cutoff value,
17 mM) increase the predictive values of protein S-100 and
CK-BB. We conclude that elevated serum concentrations of
protein S-100 and CK-BB reliably indicate moderate and severe
HIE as early as 2 h after birth. (Pediatr Res 49: 502506, 2001)
Abbreviations:
HIE, hypoxic, ischemic encephalopathy
NSE, neuron-specific enolase
CK-BB, brain-specific creatine kinase (E.C. 2.7.3.2)
aEEG, amplitude-integrated continuous EEG
Schwann cells (11). NSE is the neuronal form of the intracytoplasmic glycolytic enolase. It is found in neuronal cell bodies, axons, and neuroendocrine cells and in neuroendocrine
tumors (12). CK-BB is found in both neurons and astrocytes.
CK-BB and NSE levels have been found to be elevated after
birth asphyxia, but few data exist that concern the early time
course of these factors after the hypoxic-ischemic event (13
17). Serum concentration of protein S-100 after birth asphyxia
has not been assessed yet.
Our objectives were to investigate the postnatal time course
of these markers in serum and to determine whether hypoxicischemic brain damage alters these markers and whether moderate or severe HIE can be predicted by elevated serum concentrations soon after birth.
METHODS
The study was performed from June 1998 to December 1999
and was approved by the Ethical Committee of the Medical
Faculty, and written informed consent was given by the parents. We expected approximately one third of asphyxiated
infants to exhibit moderate or severe HIE. Therefore, we
decided to recruit approximately 30 infants in the asphyxia
502
503
EARLY INDICATORS AFTER BIRTH ASPHYXIA
group and 20 control infants. The protocol included two study
groups.
Asphyxia group. Twenty-nine subsequently full-term newborn infants (gestational age, 37 42 wk) who fulfilled the
following criteria were included in the study: arterial blood
cord pH value 7.0, or arterial blood cord pH value between
7.01 and 7.1 and also an Apgar score after 5 min of 7. The
asphyxia group was subdivided according to the clinical examination: no or mild HIE with a good prognosis, and moderate or severe HIE with a greater risk of neural handicap (18).
Control group. Twenty full-term infants who fulfilled all the
following criteria were enrolled in the study: no maternal
illness, arterial blood cord pH 7.2, after 5 min an Apgar score
of 7, and an uneventful course during the first 3 d of life.
Predefined exclusion criteria for both groups were congenital
anomalies, tumors, maternal drug addiction, severe infections,
and congenital metabolic disorders, but no infant was excluded. Clinical data are given in Table 1.
Study design. Blood samples were collected from cord
blood and 2, 6, 12, and 24 h after birth. Standardized neurologic examinations were performed at 6, 12, 24, 48, and 72 h
of age. Mild HIE was assumed according to Sarnat and Sarnat
(19) if hyperexcitability or hypotonia persisted without seizures for 72 h after birth; moderate if the newborn was
lethargic, had hypotonia, weak primitive reflexes, and seizures;
and severe if the infant had apnea, flaccid weakness, frequent
seizures, or coma.
Analysis of CK-BB, protein S-100, and NSE. Creatine
kinase was determined at 25C according to the optimized
German standard method on Dax 72 (Bayer, Munich, Germany) or Modular PP (Roche, Mannheim, Germany) random
assessment clinical analyzers. To quantify CK-BB, creatine
kinase isoenzymes were fractionated electrophoretically on
agarose gels, visualized by in-gel substrate reaction for fluorometric scanning using Helena (Greiner, Flacht, Germany) gel
kits and rapid electrophoresis system. The area under the
CK-BB curve was used to calculate its concentration.
Protein S-100 was measured manually with a sandwich type
immunoluminometric assay kit (Byk Sangtec, Dietzenbach,
Germany) that used MAb and an LB952 luminometer
(Berthold, Wildbad, Germany). The assay uses three MAbs to
detect the chains in the (S-100B) and (S-100A1)
dimers. We have used the term protein S-100 for simplicity,
which refers to both of these dimers.
NSE was measured on a Cobas Core II immunoanalyzer
with the NSE ELISA II kit (Roche), a one-step sandwich type
enzyme immunoassay that used two specific mouse MAbs.
Free Hb, as an indicator of hemolysis, was quantified by
bichromatic photometric measurement on Hitachi 911 or Modular PP analyzers (Roche). The manufacturer claims low detection limits of 0.1 g/L for NSE and 0.02 g/L for protein
S-100. In 45 cases of low sample volumes, we reduced the
amount of serum for protein S-100 assay from 100 L to 25
L, and 0.08 g/L as the lower detection limit. Least square
regression analysis for 18 samples were performed with both
the original and the diluted protocol, and gave y (25 L)
1.019 x (100 L) 0.04 with a regression coefficient of
0.98. Time required for the measurement of CK-BB, protein
S-100, and NSE was 0.5, 3.5, and 0.75 h, respectively.
Data analysis. All values were presented as medians and
interquartile ranges. Group comparisons were performed with
the Mann-Whitney U test. Positive predictive value, negative
predictive value, sensitivity, and specificity for development of
moderate or severe asphyxia were obtained using optimal
cutoff levels and were calculated on the material used in our
study. Receiver operating characteristic curves were assessed
using the areas under the curves. Correlations were calculated
by the Spearman rank method. For statistical analysis, the
SPSS 5.02 for Windows (SPSS, Chicago, IL, U.S.A.) was
used. Probability values 0.05 were considered to be
significant.
RESULTS
Birth weight, gestational age, sex, and mode of delivery
were similar among the control infants, infants with asphyxia
without or with mild HIE, and asphyxiated newborns with
moderate or severe HIE (Table 1). Of the 29 newborns with
asphyxia, seven did not develop HIE but 22 did. Fifteen
newborns had mild, four moderate, and three severe HIE. Both
Table 1. Characteristics of 29 infants with asphyxia and 20 control infants
Infants with asphyxia
Characteristics
Birth weight (g)
Gestational age (wk)
Sex (M/F)
Mode of delivery
Cesarean section
Vaginal spontaneous
Vacuum extraction
Inborns/outborns
Apgar score (1 min)
Apgar score (5 min)
Arterial cord blood pH
Arterial cord blood base deficit
Control group n 20
No or mild HIE n 22
Moderate or severe HIE n 7
p value
3318 (29623886)
40 (38 42)
6/14
3540 (3070 3800)
40 (39 41)
13/9
3155 (26253640)
40 (38 40)
2/5
NS*
NS*
NS*
NS*
10
6
4
18/2
8 (79)
9 (8 10)
7.25 (7.227.28)
5 (3 6)
9
8
5
15/7
4 (27)
6 (5 8)
6.98 (6.877.01)
13 (1116)
4
2
1
1/6
2 (12)
5 (35)
6.75 (6.62 6.90)
22 (1728)
0.026
0.01
0.03
0.008
0.03
Results are presented as medium (quartiles).
* p values are for comparison between control infants (n 20) and infants with asphyxia (n 29). p values are for comparison between infants with no
or mild HIE and moderate or severe HIE.
504
NAGDYMAN ET AL.
groups with asphyxia differed in Apgar scores at 1 and 5 min,
arterial blood cord pH, and base deficit (Table 1). Two asphyxiated infants with severe HIE died; one within 12 h because of
multiorgan failure, the other at d 26 with grade 4 intraventricular hemorrhage and renal and cardiac dysfunction. The third
infant with severe HIE suffered from meconium aspiration and
needed artificial respiration for 4 d. No artificial respiration
was necessary in the four infants with moderate HIE, but one
of them had renal failure.
CK-BB. At every time interval there was a significant difference (p 0.05) in serum CK-BB concentrations between
the asphyxia and the control groups (Table 2). Serum CK-BB
was significantly higher in infants with moderate or severe HIE
when compared with infants with no or mild HIE 2, 6, and 12 h
after birth (Table 2). No difference was found between the two
asphyxia groups in cord blood and 24 h after birth.
Protein S-100. At every time interval there was a significant
difference (p 0.05) in serum protein S-100 concentrations
between the asphyxia group and the control group (Table 2).
Serum protein S-100 was significantly higher in infants with
moderate or severe HIE when compared with infants with no or
mild HIE 2 and 6 h after birth (Table 2). No difference was
observed between the two asphyxia groups at birth and 12 and
24 h after birth.
NSE. At any time interval we could not detect a significant
difference in serum NSE concentrations between the control
group and the asphyxiated infants (Table 2). However, serum
NSE was higher in infants with moderate or severe HIE
compared with infants with no or mild HIE 12 and 24 h after
birth (Table 2). No difference was found between the two
asphyxia groups at birth and 2 and 6 h after birth. Blood
hemolysis increased the serum NSE levels, but no significant
difference in hemolysis was detectable in the different groups.
The predictive capacities for serum CK-BB, protein S-100,
NSE, pH, base deficit, and Apgar score (at 1 min) for HIE of
moderate or severe degree are shown in Table 3. Combinations
of biochemical measurements and combinations of biochemical markers with cord blood pH, cord blood base deficit, and
Apgar score at 1 min are given in Table 4. The combination of
serum protein S-100 (cutoff value, 8.5 g/L) and CK-BB
(cutoff value, 18.8 U/L) at 2 h had the highest positive predictive value and specificity (Table 4) for biochemical markers. A
combination of serum protein S-100 at 2 h after birth with cord
blood pH (cutoff value, 6.9) or cord blood base deficit (cutoff
value, 17 mM/L) increased the positive predictive value and
specificity. Correlation between the serum concentrations of
protein S-100 and CK-BB at 2 h are given in Figure 1 (s
0.66; p 0.001).
DISCUSSION
In adults, neuronal necrosis and apoptosis after global ischemia are slow, and last for several hours to several days (20).
Studies in perinatal animals suggest a quicker cellular destruction (3). It is not known how long the window of opportunity
remains open for intervention, but any intervention will be
more successful early after the insult (21). Energy substrates in
the neonatal brain continue to run down for 12 to 48 h after
hypoxia (22). Therefore an intervention might be effective 2 to
6 h after birth asphyxia. As neuroprotective interventions may
be harmful (23), it is important to find early and reliable
indicators of brain damage or of poor long-term prognosis to
initiate or end neuroprotective treatment. Cranial tomography,
somatosensory evoked potentials, and magnetic resonance tomography are useful for prognosis, but not in the first 24 h after
birth (24, 25). Magnetic resonance spectroscopy reveals brain
energy compromise (6), but is not practicable in most clinical
situations. aEEG is a useful diagnostic tool for assessing
encephalopathy. Previous reports (4, 5) established a high
predictive value of postnatal aEEG for neurologic outcome.
Several studies measured biochemical factors in serum and
cerebrospinal fluid glial fibrillary acidic protein after 12 48 h
Table 2. Serum concentrations of CK-BB, protein S-100, and NSE at different times after asphyxia
Biochemical markers
(median/interquartiles)
CK-BB (U/L)
Cord blood
2h
6h
12 h
24 h
Protein S-100 (g/L)
Cord blood
2h
6h
12 h
24 h
NSE (g/L)
Cord blood
2h
6h
12 h
24 h
Infants with asphyxia
Control group
No or mild HIE
Moderate or severe HIE
p value*
p value
3.0 (1.7511.5)
10.0 (6.0 13.0)
7.0 (4.3 8.8)
5.0 (4.0 6.8)
5.0 (3.0 6.8)
24.5 (7.5 48.5)
16.0 (13.0 23.5)
10.4 (6.0 16.0)
12.5 (6.0 15.6)
6.5 (4.0 14.0)
15.0 (14.0 40.0)
46.5 (21.4 83.0)
27.0 (18.0 55.0)
33.3 (18.152.0)
9.5 (7.0 17.5)
0.005
0.0001
0.002
0.0001
0.028
NS
0.003
0.002
0.012
NS
0.8 (0.71.0)
1.6 (1.4 2.5)
1.5 (1.22.3)
1.2 (1.11.5)
1.0 (0.9 1.4)
1.5 (1.11.9)
2.9 (1.8 4.7)
2.5 (1.6 3.8)
1.8 (1.52.3)
1.6 (1.0 2.6)
2.5 (1.53.7)
17.0 (3.234.1)
27.6 (2.6 52.3)
3.1 (1.323.1)
3.9 (1.29.0)
0.0001
0.0001
0.001
0.001
0.04
NS
0.008
0.015
NS
NS
48.9 (20.174.7)
32.5 (20.8 60.7)
35.6 (30.170.3)
34.0 (24.6 48.7)
34.8 (21.4 44.4)
106.8 (60.5108.1)
60.8 (49.3 89.0)
52.7 (48.779.3)
54.3 (46.8 78.8)
50.7 (41.8 70.9)
NS
NS
NS
NS
NS
NS
NS
NS
0.028
0.033
29.6 (17.8 55.9)
30.3 (24.8 47.6)
37.1 (19.0 48.8)
28.7 (19.8 39.4)
24.3 (17.239.5)
* p values are for comparison between all asphyxiated infants and controls. p values are for comparison between asphyxiated infants with no or mild HIE
and infants with moderate or severe HIE.
505
EARLY INDICATORS AFTER BIRTH ASPHYXIA
Table 3. Values for predicting moderate or severe HIE
Variable
Cutoff value
Protein S-100
2h
6h
CK-BB
2h
6h
NSE
2h
6h
Arterial cord blood pH
Cord blood base deficit
Apgar score (1 min)
PPV (%)
NPV (%)
Sens (%)
Spec (%)
AUC
71
63
90
90
71
71
90
86
0.832
0.805
18.8 U/L
17.0 U/L
46
55
100
94
100
86
65
77
0.879
0.877
44 g/L
46 g/L
6.9
17 mM/L
3
46
42
46
50
50
93
93
89
94
94
83
83
71
83
73
68
65
73
77
86
0.768
0.763
0.838
0.905
0.825
8.5 g/L
4.6 g/L
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; Sens, sensitivity, Spec, specificity; AUC, area under the curve. It is important
that markers demonstrate high specificity and high positive predictive value.
Table 4. Combination of factors for predicting moderate or severe HIE
Variable
PPV (%)
NPV (%)
Sens (%)
Spec (%)
Protein S-100 and CK-BB
CK-BB and cord blood pH
CK-BB and cord blood base deficit
CK-BB and Apgar score (1 min)
Protein S-100 and cord blood pH
Protein S-100 and cord blood base deficit
Protein S-100 and Apgar score (1 min)
83
71
67
83
100
100
80
91
91
91
96
88
92
88
71
71
67
83
57
67
57
95
91
91
95
100
100
96
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; Sens, sensitivity; Spec, specificity. Values of serum factors are at 2 h after birth.
Cutoff values are given in Table 3.
Fig. 1. Correlation of serum CK-BB and protein S-100 in 45 infants at an age
of 2 h. Measurements for control infants (), asphyxiated infants with no or
mild HIE (), and asphyxiated infants with moderate or severe HIE () are
shown.
(7); excitatory amino acids after 18 66 h (8); and IL-6 12 h
after the hypoxic-ischemic event (9). Urinary lactate:creatine
ratio predicts HIE within 6 h with 1H nuclear magnetic resonance spectroscopy (10), but a useful indicator for HIE should
be specific even earlier, and requires a rapid and readily
available laboratory technique. Besides this, infants with asphyxia often have oliguria, and urine sampling may not be
possible (26). Our results do not confirm serum NSE as an
early predictor of HIE. As late as 12 h after birth, serum
concentrations of NSE increased significantly in the infants
with moderate and severe HIE when compared with infants
with no or mild HIE. Results of other studies (16, 17) with
serum NSE in asphyxiated newborns are in concordance with
our data, whereas NSE in cerebrospinal fluid seems to be more
favorable.
Concerning CK-BB, these results are in accordance with studies where the increase was within the first 4 15 h of life (1315).
Our serum CK-BB activities were lower than in the studies of
Walsh et al. (14) and Fernandez et al. (15), which was probably
related to the measurement of total creatine kinase activity at
different temperatures. CK-BB is also expressed in placenta,
lungs, gastrointestinal tract, and kidneys, all of which might be
involved in the sequelae of asphyxia. Although the placenta is rich
in CK-BB activity, it seems that its contribution to serum CK-BB
levels in the neonate is negligible (27). Cuestas (13) found that the
blood CK-BB levels were not increased in neonates with renal or
gastrointestinal tract disorders. Therefore, we assume that the
increased levels originate mainly from the brain of the asphyxiated infants.
Protein S-100 is also known to be present in the striated
muscle, heart, kidneys, adipocytes, and thymus of newborns
(28, 29). Until now, no study has examined the serum values of
protein S-100 in asphyxiated and age-related control infants. In
adults, protein S-100 is not detectable in serum under normal
conditions (30); however, in cerebral diseases it ranged from
zero (31) to highly predictive values (32). Additionally, clinical
studies in adults evaluated different time patterns for the increase of serum protein S-100, such as transient increase after
cardiac operations (33), peak level within 24 h after cerebral
hemorrhage (34) or global cerebral ischemia (32), and a peak
level at d 3 after an acute ischemic stroke (34, 35). In the serum
of infants, protein S-100 has been determined after cardiac
506
NAGDYMAN ET AL.
operations and extracorporeal circulation, demonstrating agerelated concentrations that were highest in neonates and infants
with Downs syndrome with a pattern of transient increase
similar to adult patients (36). In asphyxia, serum protein S-100
release follows a pattern similar to the transient increase
observed after cardiac operations. We postulate that in case of
asphyxia, elevated levels in serum are caused by leakage of
protein S-100 into the extracellular fluid after hypoxic damage
of glial cell and neuronal membranes and by lower renal
excretion. The integrity of the blood brain barrier seems to
influence its levels in serum, which explains why serum protein
S-100 concentration is lower in adults than in infants (36).
Recent studies detected transient serum elevations of protein
S-100 without any relationship to permanent neuronal damage,
and the question has arisen as to whether protein S-100 arises
from noncerebral sources (37, 38).
We could not exclude the possibility that protein S-100 and
CK-BB release comes only from the brain. In regard to this, it
might be a simple epiphenomenon of general ischemia related to
asphyxia. Asphyxia may involve the whole body, and the release
of proteins into the blood might be a general sign of change in cell
membrane integrity and vascular permeability caused by the
whole body ischemic-reperfusion injury. In our opinion, no single
diagnostic marker should form the basis for decisions on neuroprotective therapy. But the decision as to which infants could be
candidates for postasphyxial treatment should probably be based
on several findings, which include aEEG, cord blood pH, cord
blood base deficit, Apgar score, and serum protein S-100 and
CK-BB. These biochemical markers may be helpful in deciding
whether an early initiated neuroprotective therapy should be continued or stopped. However, our data, obtained from a small
number of infants, refer to HIE and not permanent brain damage.
Neurodevelopment follow-up studies in our infants in the next
few years will show whether elevated serum protein S-100 and
CK-BB will also predict developmental delay.
REFERENCES
1. Goodwin TM, Belai I, Hernandez P, Durand M, Paul RH 1992 Asphyxial complications in the term newborn with severe umbilical acidemia. Am J Obstet Gynecol
167:1506 1512
2. Finer NN, Robertson CM, Richards RT, Pinnel LE, Peters KL 1981 Hypoxicischemic encephalopathy in term neonates: perinatal factors and outcome. J Pediatr
98:112117
3. Vannucci RC, Perlman JM 1997 Interventions for perinatal hypoxic-ischemic encephalopathy. Pediatrics 100:1004 1014
4. Hellstrm-Westas L, Rosn I, Svenningsen NW 1995 Predictive value of early
continuous amplitude integrated EEG recordings on outcome after severe birth
asphyxia in full term infants. Arch Dis Child 72:F34 F38
5. Al Naqeeb N, Edwards AD, Cowan FM, Azzopardi D 1999 Assessment of neonatal
encephalopathy by amplitude-integrated electroencephalography. Pediatrics
103:12631271
6. Thoresen M, Penrice J, Lorek A, Cady EB, Wylezinska M, Kirkbride V, Cooper CE,
Brown GC, Edwards AD, Wyatt JS, Reynolds EOR 1995 Mild hypothermia after
severe transient hypoxia-ischemia ameliorates delayed cerebral energy failure in
newborn piglets. Pediatr Res 37:667 670
7. Blennow M, Hagberg H, Rosengren L 1995 Glial fibrillary acidic protein in the
cerebrospinal fluid: a possible indicator of prognosis in full-term asphyxiated newborn infants? Pediatr Res 37:260 264
8. Hagberg H, Thornberg E, Blennow M, Kjellmer I, Lagercrantz H, Thiringer K,
Hamberger A, Sandberg M 1993 Excitatory amino acids in the cerebrospinal fluid of
asphyxiated infants: relationship to hypoxic-ischemic encephalopathy. Acta Paediatr
82:925929
9. Martin-Ancel A, Garcia-Alix A, Pascual-Salcedo D, Cabanas F, Valcarce M, Quero
J 1997 Interleukin-6 in the cerebrospinal fluid after perinatal asphyxia is related to
early and late neurological manifestations. Pediatrics 100:789 794
10. Huang CC, Wang ST, Chang YC, Lin KP, Wu PL 1999 Measurement of the urinary
lactate: creatinine ratio for the early identification of newborn infants at risk for
hypoxic-ischemic encephalopathy. N Engl J Med 341:328 335
11. Kligman D, Hilt DC 1988 The protein S 100 family. Trends Biochem Sci 13:437 443
12. Rider CC, Taylor CB 1975 Evidence for a new form of enolase in rat brain. Biochem
Biophy Res Commun 66:814 820
13. Cuestas RA 1980 Creatine kinase isoenzymes in high risk infants. Pediatr Res
14:935938
14. Walsh P, Jedeikin R, Ellis G, Primhak R, Maleka SK 1982 Assessment of neurologic
outcome in asphyxiated term infants by use of serial CK-BB isoenzyme measurement.
J Pediatr 101:988 992
15. Fernandez F, Verdu A, Quero J, Perez-Higueras A 1987 Serum CKP-BB isoenzyme
in the assessment of brain damage in asphyxiated term infants. Acta Pediatr Scand
76:914 918
16. Garcia-Alix A, Cabanas F, Pellicer A, Hernanz A, Stiris TA, Quero J 1994 Neuronspecific enolase and myelin basic protein: relationship of cerebrospinal fluid concentrations to the neurologic condition of asphyxiated full-term infants. Pediatrics
93:234 240
17. Thornberg E, Thiringer K, Hagberg H, Kjellmer I 1995 Neuron specific enolase in
asphyxiated newborns: association with encephalopathy and cerebral function monitor trace. Arch Dis Child Fetal Neonatal Ed 72:F39 F42
18. Levene MI, Sands C, Grindulis H, Moore JR 1986 Comparison of two methods of
predicting outcome in perinatal asphyxia. Lancet 1:67 69
19. Sarnat HB, Sarnat MS 1976 Neonatal encephalopathy following fetal distress: a
clinical and electroencephalographic study. Arch Neurol 33:696 705
20. Horn M, Schlote W 1992 Delayed neuronal death and delayed neuronal recovery in
the human brain following global ischemia. Acta Neuropathol 85:79 87
21. Levene MI, Evans DJ, Mason S, Brown J 1999 An international network for
evaluating neuroprotective therapy after severe birth asphyxia. Semin Perinatol
23:226 233
22. Lorek A, Takei Y, Cady EB, Wyatt JS, Penrice J, Edwards AD, Peebles D,
Wylezinska M, Owen-Reece H, Kirkbride V, Cooper CE, Aldridge RF, Roth SC,
Brown G, Delpy DT, Reynolds EOR 1994 Delayed (secondary) cerebral energy
failure after acute hypoxia-ischemia in the newborn piglet: continuous 48-hour studies
by phosphorus magnetic resonance spectroscopy. Pediatr Res 36:699 706
23. Levene M, Gibson N, Fenton A, Papathoma E, Barnett D 1990 The use of a
calcium-channel blocker, nicardipine, for severely asphyxiated newborn infants. Dev
Med Child Neurol 32:567574
24. de Vries LS, Pierrat V, Eken P, Minami T, Daniels H, Casaer P 1991 Prognostic value
of early somatosensory evoked potentials for adverse outcome in full-term infants
with birth asphyxia. Brain Dev 13:320 325
25. Fitzhardinge PM, Flodmark O, Fitz CR, Ashby S 1981 The prognostic value of
computed tomography as an adjunct to assessment of the term infants with postasphyxial encephalopathy. J Pediatr 99:777781
26. Perlman JM, Tack ED 1988 Renal injury in asphyxiated newborn infant: relation to
neurologic outcome. J Pediatr 113:875 879
27. Laboda HM, Britton VJ 1977 Creatine kinase isoenzyme activity in human placenta
and in serum of women in labour. Clin Chem 23:1329 1335
28. Suzuki F, Kato K 1986 Induction of adipose S-100 protein release by free fatty acids
in adipocytes. Biochim Biophys Acta 889:84 90
29. Kojima K, Wekerle H, Lassmann H, Berger T, Linington C 1997 Induction of
experimental autoimmune encephalitis by CD 4 T cells specific for an astrocyte
protein, S100 beta. J Neural Transm Suppl 49:4351
30. Fassbender K, Schmidt R, Schreiner A, Fatar M, Mhlhauser F, Daffertshofer M,
Hennerici M 1997 Leakage of brain-originated proteins in peripheral blood: temporal
profile and diagnostic value in early ischemic stroke. J Neurol Sci 148:101105
31. Bttner T, Lack B, Jger M, Wnsche W, Kuhn W, Mller T, Przuntek H, Postert T
1999 Serum levels of neuron-specific enolase and protein S-100 after single tonicclonic seizures. J Neurol 246:459 461
32. Martens P, Raabe A, Johnsson P 1998 Serum S-100 and neuron-specific enolase for
prediction of regaining consciousness after global cerebral ischemia. Stroke 29:2363
2366
33. Westaby S, Johnsson P, Parry AJ, Blomquist S, Solem JO, Alling C, Pillai R, Taggert
DP, Grebenik C, Stahl E 1996 Serum S100 protein: a potential marker for cerebral
events during cardiopulmonary bypass. Ann Thorac Surg 61:88 92
34. Kim JS, Yoon SS, Kim YH, Ryu JS 1996 Serial measurement of interleukin-6,
transforming growth factor-, and S-100 protein in patients with acute stroke. Stroke
27:15531557
35. Missler U, Wiesmann M, Friedrich C, Kaps M 1997 S-100 protein and neuronspecific enolase concentrations in blood as indicators of infarction volume and
prognosis in acute ischemic stroke. Stroke 28:1956 1960
36. Lindberg L, Olsson AK, Anderson K, Jgi P 1998 Serum S-100 protein levels after
pediatric cardiac operations: a possible new marker for postperfusion cerebral injury.
J Thorac Cardiovasc Surg 116:281285
37. Jnsson H, Blomquist S, Alling C, Johnsson P 1998 Early release of S100 after
cardiac surgery: interference from extracerebral sources. Ann Thorac Surg 66:1493
(abstr)
38. Westaby S, Saatvedt K, White S, Katsumata T, Oeveren W, Bhatnagar NK, Brown S,
Halligan PW 2000 Is there a relationship between serum S-100 and neuropsychologic dysfunction after cardiopulmonary bypass? J Thorac Cardiovasc Surg 119:132
137
You might also like
- D&D5e - Encounters in The Savage JungleDocument86 pagesD&D5e - Encounters in The Savage Junglewebreveur91% (11)
- The Orrery - A Handbook To The Spheres of PowerDocument113 pagesThe Orrery - A Handbook To The Spheres of PowerAnonymous PtMxUHm9RoNo ratings yet
- Sound Devices Used in PoetryDocument10 pagesSound Devices Used in PoetryPrince Ronson SabadoNo ratings yet
- BDSM Trial and ErrorDocument12 pagesBDSM Trial and ErrorAmit Saha0% (1)
- Dental Trauma Guidelines II Avulsion - Flores Anderson AndreassenDocument7 pagesDental Trauma Guidelines II Avulsion - Flores Anderson Andreassenapi-265532519No ratings yet
- SCIENCE 6 Summative Test #1 QTR 2Document4 pagesSCIENCE 6 Summative Test #1 QTR 2Jovelyn L. Lucio100% (1)
- d100 Wild Magic SurgesDocument6 pagesd100 Wild Magic SurgesStephan ChiariniNo ratings yet
- Lecture 3, Principles of Cavity Preparation IDocument23 pagesLecture 3, Principles of Cavity Preparation IJustDen09100% (3)
- Polio Vaccine Genocide in UgandaDocument12 pagesPolio Vaccine Genocide in UgandaJonathan Robert Kraus (OutofMudProductions)No ratings yet
- Biochemical MarkerDocument6 pagesBiochemical MarkerrantiadrianiNo ratings yet
- Neuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic EncephalopathyDocument5 pagesNeuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic EncephalopathyAgus WijataNo ratings yet
- Early Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsDocument8 pagesEarly Life Serum Neurofilament Dynamics Predict Neurodevelopmental Outcome of Preterm InfantsKatharina GoeralNo ratings yet
- Umbilical Cord Interleukin-6 Levels Are Elevated in Term Neonates With Perinatal AsphyxiaDocument7 pagesUmbilical Cord Interleukin-6 Levels Are Elevated in Term Neonates With Perinatal AsphyxiaRafa NaufalinNo ratings yet
- Del Toro 2006Document5 pagesDel Toro 2006NATALIA MARTINEZ CORDOBANo ratings yet
- Hearing Loss in Term Newborn Infants With Hypoxic-Ischemic Encephalopathy Treated With Therapeutic Hypothermia PDFDocument8 pagesHearing Loss in Term Newborn Infants With Hypoxic-Ischemic Encephalopathy Treated With Therapeutic Hypothermia PDFstefanp89No ratings yet
- Human Recombinant Erythropoietin in Asphyxia Neonatorum Pilot TrialDocument8 pagesHuman Recombinant Erythropoietin in Asphyxia Neonatorum Pilot TrialImran A. IsaacNo ratings yet
- International Journal of Developmental NeuroscienceDocument6 pagesInternational Journal of Developmental NeuroscienceFarin MauliaNo ratings yet
- Interictal Serum S-100B Protein Levels in Intractable Epilepsy: A Case-Control StudyDocument4 pagesInterictal Serum S-100B Protein Levels in Intractable Epilepsy: A Case-Control StudyArdiya OktamaNo ratings yet
- Hipo Glice MiaDocument7 pagesHipo Glice MiaRosita Aguirre FloresNo ratings yet
- IVIgG AmiloidDocument4 pagesIVIgG AmiloidyinvilllNo ratings yet
- ArticleDocument7 pagesArticleLinda RahayueNo ratings yet
- Biochemical Marker As Predictor of Outcome in Perinatal AsphyxiaDocument4 pagesBiochemical Marker As Predictor of Outcome in Perinatal AsphyxiaAgus WijataNo ratings yet
- Birnbaum 2018 - Sdr. Sjogren - AnticorpiDocument17 pagesBirnbaum 2018 - Sdr. Sjogren - AnticorpiSimina BarbuNo ratings yet
- 005Document7 pages005Andreea AvasiloaieiNo ratings yet
- Archive of SID: Early Diagnosis of Perinatal Asphyxia by Nucleated Red Blood Cell Count: A Case-Control StudyDocument7 pagesArchive of SID: Early Diagnosis of Perinatal Asphyxia by Nucleated Red Blood Cell Count: A Case-Control Studyeen265No ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- NEUROLOGY2016771188Document7 pagesNEUROLOGY2016771188csuheena.chamandNo ratings yet
- 23 - 224Praktis-Strategi Terapi Cairan Pada DehidrasiDocument8 pages23 - 224Praktis-Strategi Terapi Cairan Pada DehidrasiRahmat AbbasNo ratings yet
- Espr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedDocument1 pageEspr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedAgus WijataNo ratings yet
- Spasm PDFDocument4 pagesSpasm PDFRidho ArendoNo ratings yet
- Neurofilament Light (NFL) As Biomarker in Serum and CSF in Status Epilepticus - 2023Document11 pagesNeurofilament Light (NFL) As Biomarker in Serum and CSF in Status Epilepticus - 2023Reny Wane Vieira dos SantosNo ratings yet
- Case Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusDocument4 pagesCase Series: Neuropsychiatric Symptoms With Pediatric Systemic Lupus ErythematosusJosue LayedraNo ratings yet
- Ref 12Document12 pagesRef 12Tiago BaraNo ratings yet
- 25-Elevated Interleukin-6 in The Cerebrospinal Fluid of A Previously Delineated Schizophrenia SubtypeDocument7 pages25-Elevated Interleukin-6 in The Cerebrospinal Fluid of A Previously Delineated Schizophrenia SubtypeAli Emre KöseNo ratings yet
- Biochemical Markers For Brain Damage After CarbonDocument5 pagesBiochemical Markers For Brain Damage After CarbonAna CortezNo ratings yet
- Moll Cellproteomic PDFDocument49 pagesMoll Cellproteomic PDFGLORIA ESTEFANI YANTAS ALCANTARANo ratings yet
- Seizstroke in ChildDocument6 pagesSeizstroke in ChildDian Isti AngrainiNo ratings yet
- Efficacy of The Anti-Seizure Medications in Acute Symptomatic Neonatal Seizures Caused by Stroke. A Systematic ReviewDocument9 pagesEfficacy of The Anti-Seizure Medications in Acute Symptomatic Neonatal Seizures Caused by Stroke. A Systematic ReviewSultan Rahmat SeptianNo ratings yet
- 1456 FullDocument7 pages1456 Fulldrmanishmahajan79No ratings yet
- NCC Case StudyDocument4 pagesNCC Case StudyMasego MekgoeNo ratings yet
- Nejmoa 067514Document11 pagesNejmoa 067514Andrea Sandoval OteroNo ratings yet
- Cytokine and Chemokine Expression in CSF May Differentiate Viral ADocument7 pagesCytokine and Chemokine Expression in CSF May Differentiate Viral AMiguel Angel Villarreal YbazetaNo ratings yet
- Whole-Body Hypothermia For Term and Near-TermDocument9 pagesWhole-Body Hypothermia For Term and Near-TermNATALY HASTAMORY VANEGASNo ratings yet
- CK and LBMDocument8 pagesCK and LBMSarathNo ratings yet
- Cannabinoids Promote Embryonic and Adult Hippocampus Neurogenesis and Produce Anxiolytic-And Antidepressant-Like EffectsDocument13 pagesCannabinoids Promote Embryonic and Adult Hippocampus Neurogenesis and Produce Anxiolytic-And Antidepressant-Like EffectsDouglas Maestro FranciscoNo ratings yet
- Biomarkers of Alzheimer Disease in Children With Obstructive Sleep ApneaDocument8 pagesBiomarkers of Alzheimer Disease in Children With Obstructive Sleep ApneaZeljko LekovicNo ratings yet
- Cerebral Palsy Article 2Document6 pagesCerebral Palsy Article 2ChrismoonNo ratings yet
- Ref 7Document12 pagesRef 7Tiago BaraNo ratings yet
- HHS Public Access: Serum Biomarkers of Brain Injury After Pediatric Cardiac ArrestDocument40 pagesHHS Public Access: Serum Biomarkers of Brain Injury After Pediatric Cardiac ArrestsylvetriNo ratings yet
- Brain Perfusion in Asphyxiated Newborns Treated With Therapeutic HypothermiaDocument7 pagesBrain Perfusion in Asphyxiated Newborns Treated With Therapeutic HypothermiafrostyNo ratings yet
- Kolicheski Et Al-2017-Journal of Veterinary Internal MedicineDocument9 pagesKolicheski Et Al-2017-Journal of Veterinary Internal MedicineDulce Lucia ChacónNo ratings yet
- Abstract Booklet 2010Document50 pagesAbstract Booklet 2010Danijela VukicevicNo ratings yet
- Epo EhiDocument12 pagesEpo EhiUriel MartzNo ratings yet
- 27 Pain Control and Nursing During Minor Painful Procedure in Newborns A Randomized Controlled TrialDocument1 page27 Pain Control and Nursing During Minor Painful Procedure in Newborns A Randomized Controlled TrialDaniella AwurumibeNo ratings yet
- 2011 BakirciogluDocument13 pages2011 BakirciogluMestrado EducacaoNo ratings yet
- Intrauterine Administration of EndotoxinDocument7 pagesIntrauterine Administration of EndotoxinMaria SilvaNo ratings yet
- Sparks 2015Document9 pagesSparks 2015jorge.gruizNo ratings yet
- Fetal and Neonatal Effects of N Acetylcysteine When Used - 2016 - The Journal oDocument16 pagesFetal and Neonatal Effects of N Acetylcysteine When Used - 2016 - The Journal oNiluh SukreniNo ratings yet
- Ref 5Document11 pagesRef 5Tiago BaraNo ratings yet
- Epilepsia EpicongressDocument245 pagesEpilepsia EpicongressВасилий КоптеловNo ratings yet
- Melatonin Use For Neuroprotection in Perinatal Asphyxia: A Randomized Controlled Pilot StudyDocument6 pagesMelatonin Use For Neuroprotection in Perinatal Asphyxia: A Randomized Controlled Pilot StudyJavier Miranda MalleaNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- Cei 13095Document6 pagesCei 13095karen rinconNo ratings yet
- Awab 134Document12 pagesAwab 134yi1zhangNo ratings yet
- Early Discontinuation of ASM in Neonatal Seizure - CommentDocument5 pagesEarly Discontinuation of ASM in Neonatal Seizure - CommentMariela Nadir Guerreros De VelasquezNo ratings yet
- Poor Sleep and Altered Hypothalamic-Pituitary-Adrenocortical and Sympatho-Adrenal-Medullary System Activity in ChildrenDocument8 pagesPoor Sleep and Altered Hypothalamic-Pituitary-Adrenocortical and Sympatho-Adrenal-Medullary System Activity in Childrenapi-25984288No ratings yet
- cYCLIC ALTERNATING PATTERN IN INFNATS WITH CONGENITAL HYPOTHYROIDISM RAFA SANTANA GERARDO ALVARADODocument6 pagescYCLIC ALTERNATING PATTERN IN INFNATS WITH CONGENITAL HYPOTHYROIDISM RAFA SANTANA GERARDO ALVARADOGerardo Alvarado RuizNo ratings yet
- Krabbe DiseaseDocument20 pagesKrabbe Diseasepediatria hgz2No ratings yet
- Flyer Asmpid 2021Document2 pagesFlyer Asmpid 2021Agus WijataNo ratings yet
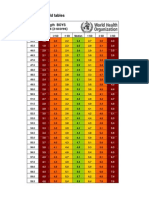
- WHO New Zscore WLZ Boys 0-2yrsDocument5 pagesWHO New Zscore WLZ Boys 0-2yrsAgus WijataNo ratings yet
- Kids Games Powerpoint TemplateDocument26 pagesKids Games Powerpoint TemplateAgus WijataNo ratings yet
- Nna en November09Document3 pagesNna en November09Agus WijataNo ratings yet
- Status of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaDocument4 pagesStatus of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaAgus WijataNo ratings yet
- Edwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCDocument1 pageEdwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCAgus WijataNo ratings yet
- Biochemical Marker As Predictor of Outcome in Perinatal AsphyxiaDocument4 pagesBiochemical Marker As Predictor of Outcome in Perinatal AsphyxiaAgus WijataNo ratings yet
- Espr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedDocument1 pageEspr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedAgus WijataNo ratings yet
- KBM0701 Stern 21Document6 pagesKBM0701 Stern 21Agus WijataNo ratings yet
- Bloody DDocument31 pagesBloody DAgus WijataNo ratings yet
- MML Test Setup PDFDocument1 pageMML Test Setup PDFAgus WijataNo ratings yet
- Alice in WonderlandDocument2 pagesAlice in WonderlandMukhlas NuriNo ratings yet
- Introduction To Shareera Kriya PhysiologyDocument2 pagesIntroduction To Shareera Kriya PhysiologyRoshan BaskotaNo ratings yet
- First Aid & BandagingDocument35 pagesFirst Aid & BandagingDemocrito JasaNo ratings yet
- Exercise 1Document13 pagesExercise 1Estephen FortelaNo ratings yet
- V EVS Question Bank For SA-1: by Mazumdar Sankar, PRT (SS), AECS, ManuguruDocument41 pagesV EVS Question Bank For SA-1: by Mazumdar Sankar, PRT (SS), AECS, Manuguruspanja_barcNo ratings yet
- Dolphins On Duty: Dolphins On Duty The U.S. Navy Trains These Supersmart Animals To Work On Lifesaving MissionsDocument3 pagesDolphins On Duty: Dolphins On Duty The U.S. Navy Trains These Supersmart Animals To Work On Lifesaving MissionsAira Ysabel PutunganNo ratings yet
- Test Bank For Purchasing and Supply Chain Management 7th Edition Robert M Monczka Robert B Handfield Larry C Giunipero James L PattersonDocument23 pagesTest Bank For Purchasing and Supply Chain Management 7th Edition Robert M Monczka Robert B Handfield Larry C Giunipero James L PattersonArthurRamirezcmya100% (42)
- HypersensitivityDocument15 pagesHypersensitivityTejpalNo ratings yet
- Autonomic NotesDocument4 pagesAutonomic NotesYeyeth Jabaybay TabolongNo ratings yet
- A NEW CLASSIFICATION OF MAMMALS, SimpsonDocument36 pagesA NEW CLASSIFICATION OF MAMMALS, SimpsoneligeokNo ratings yet
- VB Neregulate ToateeeeDocument5 pagesVB Neregulate ToateeeeCazanNo ratings yet
- Hyperthermia and PregnancyDocument10 pagesHyperthermia and PregnancyAnnisa Nurfiatul AiniNo ratings yet
- Proximal Stripping PDFDocument11 pagesProximal Stripping PDFsmilecarekkmNo ratings yet
- Dairy Bull - 551BS01414 - Brown Heaven R Famous-ETDocument1 pageDairy Bull - 551BS01414 - Brown Heaven R Famous-ETJonasNo ratings yet
- Reinforcement: Name: Date: ClassDocument3 pagesReinforcement: Name: Date: ClassCarmen M. JiménezNo ratings yet
- Vinciane Despret: Angelaki April 2015Document6 pagesVinciane Despret: Angelaki April 2015Mateus Raynner AndréNo ratings yet
- Prenatal Period of Development EportfolioDocument4 pagesPrenatal Period of Development Eportfolioapi-367895274No ratings yet
- SyllogismDocument54 pagesSyllogismMaryTherese VillanuevaNo ratings yet
- HasbroDocument2 pagesHasbroSyed Faisal RazaNo ratings yet
- PuntilascanDocument67 pagesPuntilascanMaria Silvia BettiNo ratings yet
- Tariffs For 2020 Hunting SeasonDocument2 pagesTariffs For 2020 Hunting SeasonTheodore ReaderNo ratings yet