Professional Documents
Culture Documents
Suppositories
Uploaded by
Jerome Rivera Castro0 ratings0% found this document useful (0 votes)
89 views3 pagesSuppositories
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSuppositories
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
89 views3 pagesSuppositories
Uploaded by
Jerome Rivera CastroSuppositories
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
1.
A suppository is a drug delivery system that is inserted into the rectum
(rectal suppository), vagina (vaginal suppository) or urethra (urethral
suppository), where it dissolves or melts and is absorbed into the blood
stream. The use of rectal suppositories has been documented since the
civilization of Ancient Egypt
2. Vaginal inserts, formerly called suppositories or pessaries, are usually
globular, oviform, or cone shaped and weigh about 5 g when cocoa butter is the
base. Urethral inserts, also called bougies, are slender, pencil-shaped
suppositories intended for insertion into the male or female urethra.
3. Rectal suppositories intended for local action are most frequently used to
relieve constipation or the pain, irritation, itching, and inflammation associated
with hemorrhoids or other anorectal conditions. Antihemorrhoidal suppositories
frequently contain a number of components, including local anesthetics,
vasoconstrictors, astringents, analgesics, soothing emollients, and protective
agents. A popular laxative, glycerin suppositories promote laxation by local
irritation of the mucous membranes, probably by the dehydrating effect of the
glycerin on those membranes. Vaginal suppositories or inserts intended for local
effects are employed mainly as contraceptives, as antiseptics in feminine
hygiene, and as specific agents to combat an invading pathogen. Urethral
suppositories may be antibacterial or a local anesthetic preparative for a urethral
examination.
4. Examples of drugs administered rectally in the form of suppositories for their
systemic effects include (a) prochlorperazine and chlorpromazine for the relief of
nausea and vomiting and as a tranquilizer; (b) morphine and oxymorphone for
opioid analgesia; (c) ergotamine tartrate for the relief of migraine syndrome; (d)
indomethacin, a nonsteroidal anti-inflammatory analgesic and antipyretic; and
(e) ondansetron for the relief of nausea and vomiting.
5. The advantages of rectal administration include the following:
1. First-pass effect: Avoiding, at least partially, the first-pass effect that may
result in higher blood levels for those drugs subject to extensive first-pass
metabolism upon oral administration.
2. Drug stability: Avoiding the breakdown of certain drugs that are susceptible
to gastric degradation.
3. Large dose drugs: Ability to administer somewhat larger doses of drugs
than using oral administration.
4. Irritating drugs: Ability to administer drugs that may have an irritating
effect on the oral or gastrointestinal mucosa when administered orally.
5. Unpleasant tasting or smelling drugs: Ability to administer unpleasant
tasting or smelling drugs whose oral administration is limited.
6. In children, the rectal route is especially useful. An ill child may refuse oral
medication and may fear injections.
7. In patients experiencing nausea and vomiting or when the patient is
unconscious.
8. The presence of disease of the upper gastrointestinal tract that may
interfere with drug absorption.
9. Objectionable taste or odor of a drug (especially important in children).
10. Achievement of a rapid drug effect systemically (as an alternate to
injection).
6. Among the physiologic factors that affect drug absorption from the rectum
are the circulation route, colonic contents, and the pH and lack of buffering
capacity of the rectal fluids.
7.
8. Cocoa butter (theobroma oil) melts quickly at body temperature, but because
it is immiscible with body fluids, fat-soluble drugs tend to remain in the oil and
have little tendency to enter the aqueous physiologic fluids. For water-soluble
drugs in cocoa butter, the reverse is usually true and good release results. Fatsoluble drugs seem to be released more readily from bases of glycerinated
gelatin or polyethylene glycol, both of which dissolve slowly in body fluids. When
irritation or inflammation is to be relieved, as in the treatment of anorectal
disorders, cocoa butter appears to be the superior base because of its emollient
or soothing, spreading action.
9. Suppositories are prepared by two methods: (a) molding from a melt and (b)
hand rolling and shaping.
10. The steps in molding include (a) melting the base, (b) incorporating any
required medicaments, (c) pouring the melt into molds, (d) allowing the melt to
cool and congeal into suppositories, and (e) removing the formed suppositories
from the mold.
11. Depending on the formulation, suppository molds may require lubrication
before the melt is poured to facilitate clean and easy removal of the molded
suppositories.
12. Glycerin suppositories promote laxation by local irritation of the mucous
membranes, probably by the dehydrating effect of the glycerin on those
membranes. A glycerinated gelatin base is most frequently used in the
preparation of vaginal suppositories, with which prolonged local action of the
medicinal agent is usually desired.
13. If they must be stored in the refrigerator, suppositories should be allowed to
warm to room temperature before insertion. The patient should be advised to rub
cocoa butter suppositories gently with the fingers to melt the surface to provide
lubrication for insertion. Glycerinated gelatin or polyethylene glycol suppositories
should be moistened with water to enhance lubrication. If the polyethylene glycol
suppository formulation does not contain at least 20% water, dipping it into
water just prior to insertion prevents moisture from being drawn from rectal
tissues after insertion and decreases subsequent irritation. The shape of the
suppository determines how it will be inserted. Bullet-shaped rectal suppositories
should be inserted point-end first. When the patient is instructed to use one-half
suppository, the patient should be told to cut the suppository in half lengthwise
with a clean razor blade. Most suppositories are dispensed in paper, foil, or
plastic wrappings, and the patient must be instructed to completely remove the
wrapping before insertion. Depending upon the medication, purpose of the
suppository, and associated factors, the administration of an enema prior to a
suppository may increase the absorption of the drug. Additional information on
inserting rectal suppositories and and informed consent has been published and
may be useful for patient counseling
14. Page 384, please paraphrase Love
You might also like
- Overlord v13 c2 + Intermission All Parts EnglishDocument85 pagesOverlord v13 c2 + Intermission All Parts EnglishJerome Rivera CastroNo ratings yet
- HospitalsDocument1 pageHospitalsJerome Rivera CastroNo ratings yet
- Performance Report For:: Executive SummaryDocument23 pagesPerformance Report For:: Executive SummaryJerome Rivera CastroNo ratings yet
- Traffic OverviewDocument2 pagesTraffic OverviewJerome Rivera CastroNo ratings yet
- Three Letter Abbrevi Ation Line-Dash ModelDocument11 pagesThree Letter Abbrevi Ation Line-Dash ModelJerome Rivera CastroNo ratings yet
- Philo Homework Aug 17Document3 pagesPhilo Homework Aug 17Jerome Rivera CastroNo ratings yet
- CLE I Semifinal Test GabDocument2 pagesCLE I Semifinal Test GabJerome Rivera CastroNo ratings yet
- Overlord v13 c1 All Parts EnglishDocument86 pagesOverlord v13 c1 All Parts EnglishJerome Rivera CastroNo ratings yet
- Overlord Volume 12 - The Paladin of The Holy Kingdom - Black EditionDocument398 pagesOverlord Volume 12 - The Paladin of The Holy Kingdom - Black EditionJerome Rivera CastroNo ratings yet
- Philo Homework Aug 17Document3 pagesPhilo Homework Aug 17Jerome Rivera CastroNo ratings yet
- To Paste Nov8Document194 pagesTo Paste Nov8Jerome Rivera CastroNo ratings yet
- 36" Single RX Metal Bay Unit - 329 USDDocument5 pages36" Single RX Metal Bay Unit - 329 USDJerome Rivera CastroNo ratings yet
- b09 1414 PDFDocument8 pagesb09 1414 PDFJerome Rivera CastroNo ratings yet
- Steph Sked Sem 1 2016Document2 pagesSteph Sked Sem 1 2016Jerome Rivera CastroNo ratings yet
- HomeworksDocument6 pagesHomeworksJerome Rivera CastroNo ratings yet
- Biochem Structures and FunctionsDocument7 pagesBiochem Structures and FunctionsJerome Rivera CastroNo ratings yet
- AlaaDocument1 pageAlaaJerome Rivera CastroNo ratings yet
- Auditory Pathway PDFDocument35 pagesAuditory Pathway PDFJohnson JayarajNo ratings yet
- Anatomy of The EyeDocument3 pagesAnatomy of The EyeJerome Rivera CastroNo ratings yet
- Transdermal SDocument5 pagesTransdermal SJerome Rivera CastroNo ratings yet
- AntifungalsDocument1 pageAntifungalsJerome Rivera CastroNo ratings yet
- Table TennisDocument18 pagesTable TennisJoslin RozNo ratings yet
- Experiment 8Document1 pageExperiment 8Jerome Rivera CastroNo ratings yet
- Experiment 8Document1 pageExperiment 8Jerome Rivera CastroNo ratings yet
- ReflexesDocument1 pageReflexesJerome Rivera CastroNo ratings yet
- Magmas and Gels: Dr. Mehwish Qayyum Pharm.d Ms - Drug Design and Discovery (University of Surrey) Senior LecturerDocument22 pagesMagmas and Gels: Dr. Mehwish Qayyum Pharm.d Ms - Drug Design and Discovery (University of Surrey) Senior LecturerJerome Rivera CastroNo ratings yet
- Dobaria Final 10 (1) 3-13Document11 pagesDobaria Final 10 (1) 3-13Jerome Rivera CastroNo ratings yet
- FAQ and Known BugsDocument3 pagesFAQ and Known BugsJerome Rivera CastroNo ratings yet
- Location List+Evolution NotesDocument9 pagesLocation List+Evolution NotesJerome Rivera CastroNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 01 1 PDFDocument8 pages01 1 PDFpravikumar1989No ratings yet
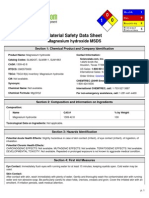
- Msds MgOHDocument5 pagesMsds MgOHCahyaGeriyanaNo ratings yet
- Sample 20715Document16 pagesSample 20715Sachin KumarNo ratings yet
- Not Eligible As No Experience of Teaching and ResearchDocument5 pagesNot Eligible As No Experience of Teaching and ResearchVasanth Kumar AllaNo ratings yet
- 0100 Sigmazam ReducerDocument2 pages0100 Sigmazam ReducerAhmed SaadNo ratings yet
- Top 10 Pharma Companies in India 2022Document8 pagesTop 10 Pharma Companies in India 2022Royal MarathaNo ratings yet
- Plotting Immunisation Monitoring ChartDocument10 pagesPlotting Immunisation Monitoring Chartthusegomokone09No ratings yet
- Aims and Applications: Aims: The Three Aims of Pharmacoepidemiology AreDocument10 pagesAims and Applications: Aims: The Three Aims of Pharmacoepidemiology Aregowtham0% (1)
- ECG Identification QuizDocument40 pagesECG Identification QuizRahul AudenesenNo ratings yet
- A Brief History of Evidence-Based Medicine in Four PeriodsDocument31 pagesA Brief History of Evidence-Based Medicine in Four PeriodsSaad MotawéaNo ratings yet
- Tza STG Neml 2007 PDFDocument220 pagesTza STG Neml 2007 PDFJohnny EmperorNo ratings yet
- IPE Zoology Model Paper 1 Question PaperDocument2 pagesIPE Zoology Model Paper 1 Question PaperFgkew DjgsNo ratings yet
- Spatial Analysis of Pulmonary TB Distribution and Risk FactorsDocument7 pagesSpatial Analysis of Pulmonary TB Distribution and Risk FactorsAhmad RivaiNo ratings yet
- AnupanaDocument60 pagesAnupanaVaidya Nur50% (4)
- Synthesis of Novel Amino Acid Derivative of 7-AVCADocument4 pagesSynthesis of Novel Amino Acid Derivative of 7-AVCAIOSRjournal0% (1)
- Ayurveda Today IndexDocument15 pagesAyurveda Today IndexrajrajNo ratings yet
- Psychiatric Case History NotesDocument8 pagesPsychiatric Case History NotesTysle100% (1)
- Trace Elements Deficiencies in Belgian CattleDocument8 pagesTrace Elements Deficiencies in Belgian CattleHuber RizzoNo ratings yet
- 08 ICSH Recommendations For Measurement of ESRDocument6 pages08 ICSH Recommendations For Measurement of ESRMuslim Majlis UojNo ratings yet
- Young FrankensteinDocument109 pagesYoung FrankensteinColleen Hawks-Pierce83% (6)
- Acute otitis media in adults: An overviewDocument15 pagesAcute otitis media in adults: An overviewchristineNo ratings yet
- Diet CounsellingDocument11 pagesDiet CounsellingDrBhawna AroraNo ratings yet
- Overdentures Improve Chewing Efficiency and Bone SupportDocument8 pagesOverdentures Improve Chewing Efficiency and Bone SupportMezo SalahNo ratings yet
- Edna K.huffman - Health Information Managemen 1994Document36 pagesEdna K.huffman - Health Information Managemen 1994gspot967% (6)
- Isolating Staphylococcus SPDocument4 pagesIsolating Staphylococcus SPHani HairullaNo ratings yet
- Reasoning BookDocument38 pagesReasoning BookAshish Sharma100% (1)
- Partners Case CCMNDocument4 pagesPartners Case CCMNapi-314349758No ratings yet
- September 15, 2016Document20 pagesSeptember 15, 2016CassieNo ratings yet
- It PDFDocument385 pagesIt PDFCosmina UngurNo ratings yet
- Reading Sub-Test: Answer Key - Part ADocument23 pagesReading Sub-Test: Answer Key - Part AAlwin BrightNo ratings yet