Professional Documents
Culture Documents
Journal of Pediatric Surgery: Eileen Kelleher, Elizabeth Taylor-Linzey, Lisa Ferrigno, Julia Bryson, Stephen Kaminski
Uploaded by
Begoña MartinezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal of Pediatric Surgery: Eileen Kelleher, Elizabeth Taylor-Linzey, Lisa Ferrigno, Julia Bryson, Stephen Kaminski
Uploaded by
Begoña MartinezCopyright:
Available Formats
Journal of Pediatric Surgery 49 (2014) 341344
Contents lists available at ScienceDirect
Journal of Pediatric Surgery
journal homepage: www.elsevier.com/locate/jpedsurg
A community return-to-play mTBI clinic: Results of a pilot program and survey of
high school athletes
Eileen Kelleher , Elizabeth Taylor-Linzey, Lisa Ferrigno, Julia Bryson, Stephen Kaminski
Santa Barbara Cottage Hospital, Rehabilitation and Pediatric Trauma Services, Santa Barbara, CA, USA
a r t i c l e
i n f o
Article history:
Received 16 October 2013
Accepted 16 October 2013
Key words:
Mild traumatic brain injury
mTBI
Concussion
Return to play
RTP
Underreported concussion
Underreported mTBI
mTBI legislation
mTBI clinic
Pediatric
Adolescent
Athlete
High school
a b s t r a c t
Background: High school athletes who sustain a mild traumatic brain injury (mTBI) or concussion are required
to be removed from play until clearance by a provider. A regional pediatric trauma center offered an mTBI
clinic to evaluate students for return to play (RTP).
Methods: An mTBI clinic was developed in collaboration with a high school district containing three schools.
This program evaluated students suffering from sports-related head trauma, specically football injuries.
Community mTBI education was performed, a standardized RTP algorithm was developed, and a postseason
survey was administered to football players.
Results: Twenty-eight students playing football were seen by the mTBI clinic. The average time until RTP for
clinic patients was 16.9 days. Four hundred ve players were surveyed. Of players responding to the survey,
40 (15%) reported sustaining an mTBI during the football season. Of those sustaining an mTBI, 9 (22.5%) did
not report their symptoms.
Conclusion: Although the mTBI rate is similar to reported rates, the unreported mTBI episodes were lower
(22.5%) than previously published self-reported mTBI rates. The RTP algorithm was successful in returning
athletes in 16.9 days. The algorithm and data can be utilized by other organizations in establishment of an
mTBI clinic and RTP program.
Mild traumatic brain injury (mTBI) or concussion, while lacking
a clear denition, carries uncertain management guidelines
despite mandated directives for athletes injured while participating
in high schools sports. At a regional pediatric trauma center, in
conjunction with three local area high schools, we asked if an mTBI
clinic, run by the trauma center, could evaluate and manage
adolescent athletes suffering from concussive events with a standardized return-to-play algorithm.
mTBI is dened as a complex pathophysiological process affecting
the brain, which is caused by a direct or indirect blow to the head [1].
It has also been dened as force transmitted to the head resulting in
an alteration of consciousness. The precipitating event may not
include complete loss of consciousness [2]. This application of force
causes neurochemical, metabolic and physiologic changes within the
brain and throughout the nervous system [2,3]. The period for
recovery from these changes can vary depending on age, history of
previous mTBIs, preexisting conditions and gender [35].
Corresponding author at: Santa Barbara Cottage Hospital, 400 Pueblo W. Pueblo St,
Santa Barbara, CA 93102, USA. Tel.: +1 805 259 5646.
E-mail address: ekelleher@sbch.org (E. Kelleher).
0022-3468/$ see front matter 2014 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.jpedsurg.2013.10.016
2014 Elsevier Inc. All rights reserved.
The Center for Disease Control (CDC) estimates that sports-related
mTBIs occur at a rate of 1.6 to 3.8 million annually [6]. While
substantial barriers of estimating the incidence of mTBI in adolescent
youth exist, activities where impact to the head occurs put
participants at risk. Powel and Barber-Foss [7] found that mTBIs
were responsible for 5.5% of high school sports injuries, with 63.4% of
these mTBIs occurring in football. Current guidelines from the
American Academy of Neurology (AAN) [8] and American Academy
of Pediatrics (AAP) [9] recommend no return to play on day of injury
or while symptomatic, but specic duration of rest (cognitive or
physical) is not established.
1. Methods
1.1. Program initiation
The Santa Barbara Cottage Hospital (SBCH) pediatric trauma
service and ofcials of a local school district containing three high
schools agreed to pilot a program to provide concussion evaluation to
assist students in return to play (RTP). Of 7500 students, it is
estimated that 1500 students participate in school-sponsored athletics. A subset of 405 high school students playing football became the
focus of the program. The purposes were to evaluate students after a
suspected mTBI and to provide education and guidance on RTP.
342
E. Kelleher et al. / Journal of Pediatric Surgery 49 (2014) 341344
Awareness of this clinic was provided by a series of public interest
events that were held in the local community focusing on mTBI in high
school athletes. This occurred just prior to the start of preseason
training for the fall 2012 high school football season. The rst event was
directed to health care providers which included physicians, nurses and
rst responders. The second event was directed to schools and
attended by coaches, athletic trainers, school administrators, student
athletes and their parents. Students playing football at the three high
schools were strongly encouraged to attend by coaching staff at all
three schools, but attendance was not mandatory. The third event was
provided for the community at large. All events featured medical
experts and recognizable spokespersons in the area of concussion.
The clinic became operational to coincide with the rst day of local
high school football practice in August of 2012. The clinic was
conducted through SBCH and was staffed by pediatric trauma service
nurse practitioners. Student athletes sustaining an mTBI were
removed from play after injury by athletic trainers and coaches in
accordance with California law. There was no required symptom
pattern for removal. Removal was performed at the discretion of
trainers and coaches. After removal athletic trainers provided athletes
the option to receive RTP clearance through a health care provider of
their choice or the trauma clinic mTBI program.
1.2. Evaluation algorithm
In collaboration with Pediatric Neurology and Physical Medicine
and Rehabilitation (PMR) departments, the pediatric trauma service
developed an algorithm for treatment and RTP for use in a new mTBI
clinic. Two assessment tools were utilized in the program. ImPACT is
a computerized neurocognitive evaluation that is administered prior
to exposure to at-risk sports. It may also be utilized in evaluation after
concussion and prior to RTP by comparing to preinjury results. All
students playing football underwent ImPACT testing. The Acute
Concussion Evaluation (ACE) [10] is endorsed by the CDC. It provides
information about initial injury and symptoms, persisting symptoms,
concussion history and other risk factors for longer recovery periods.
Additionally, it incorporates management guidelines by provision of
red ags necessitating clinician reassessment and the effects of
exertion as at rest symptoms resolve. The school version also contains
a graded return-to-play explanation and recommendations for
student reintegration into school.
Atthetimeofinjury,athletictrainerscompletedtheAcuteConcussion
Evaluation(ACE)formwiththedetailsoftheinjury.Thisformwasgivento
theparentsofstudentathletes.ParentschoosingtousethemTBIclinicfor
RTP clearance for their child were then scheduled for the next available
appointment. Those appointments included mTBI symptom screening
andaneurologicalexam,andifIMPACTscoreswereavailable,theywere
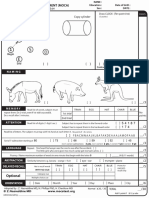
reviewed. Athletes were evaluated according to the RTP algorithm
(Fig. 1). This was developed based on assessment tools, the neurologic
examoftheathleteandthe1997AANguidelines[11].Thenumberofprior
concussions, grade of concussion, and duration and type of symptoms
were incorporated into an individualized RTP plan.
For athletes who were asymptomatic at their clinic visit, the
completed ACE form for return to school was reviewed with students
Fig. 1. Pediatric RTP.
E. Kelleher et al. / Journal of Pediatric Surgery 49 (2014) 341344
and their parents. This outlined that they could return to school when
symptom-free and after an additional RTP algorithm specied rest
period as well as additional recommendations for school reintegration. Athletes and their parents were educated on brain rest and the
risk of reinjury including second impact syndrome. Athletes and
parents were also educated on a graded return to homework and
school. For symptomatic athletes rescreening occurred after the RTP
algorithm specied interval and, if appropriate, athletes were cleared
for graded return to play at that time. If symptoms persisted beyond
2-week referral to a specialist (i.e., cognitive therapy, neurocognitive
testing, and neurology) was performed. Data collected included
information based on ACE evaluation, including initial and ongoing
symptoms. Data were de-identied and collection was approved by
the institutional review board of SBCH.
1.3. Postseason survey
A post-football season survey was provided to all football
participants in the pilot program high schools. The time period
evaluated in the survey was the football season, from the preseason in
August 2012 through the end of the season in November 2012. The
survey provided a basic denition of an mTBI and asked seven
questions related to mTBIs, including 1) whether the athlete sustained
an mTBI this season and/or in past seasons, and 2) if sustained during
this season if and to whom he reported the mTBI, and 3) the licensed
provider who performed the RTP clearance. Surveys were administered by the athletic trainers at the end of the last football game and
returned to trauma services. No personal identifying information was
required on the survey and data collection was approved by the
institutional review board of SBCH.
2. Results
2.1. Clinic demographics
Twenty-eight male football players were evaluated in the clinic.
The average age of students evaluated in the clinic was 15.3 years
[1318]. The most commonly reported symptom by patients seen for
RTP was headache (90%) (Fig. 2). Most students seen in the clinic had
at least one prior concussion (17/28; Fig. 3). The mean amount of time
until RTP was 16.9 days (range = 539).
2.2. Postseason survey
A postseason survey was distributed to the 405 high school
students playing football eligible for the program. There were 266
respondents and the average age was 15.5 years. Of those responding,
40 (15% of survey responders) had reported having had symptoms
consistent with an mTBI during the football season. Of those
sustaining mTBI based on these symptoms and responding to the
survey, 9 (22.5%) did not report their symptoms to anyone, 18 (45%)
Number of Patients
30
343
Fig. 3. Number of prior concussions sustained by RTP clinic patients.
were cleared in our RTP clinic, 4 (10%) were cleared by a neurologist, 3
(7.5%) were cleared by a pediatrician, 3 (7.5%) were cleared by the
athletic trainer, 1 (2.5%) was cleared by the coach, 1 (2.5%) was not
cleared to RTP and 1 (2.5%) was cleared by an uncategorized provider
listed as an other category on the survey (Fig. 4).
3. Discussion
Current guidelines from American Academy of Neurology (AAN)
[8] and American Academy of Pediatrics (AAP) [9] recommend no
return to play on the day of injury or while symptomatic, but specic
duration of rest (cognitive or physical) is not established. At the time
of institution of our program, the most recent recommendations with
any specics were from the 1997 AAN [11] utilizing the Colorado
Medical Society Guidelines [12]. An mTBI clinic, run under the aegis of
a pediatric trauma center, can evaluate and manage adolescent
athletes suffering from concussive events with a standardized returnto-play algorithm.
The clinic was used for RTP by approximately half of the students
suffering from concussions during the football season. Although some
were seen by other appropriately trained physicians, 10% of students
were cleared by coaches or trainers. Currently, there is no set training
path specically for the assessment of neurologic injury in athletes
nor are there accepted guidelines for the specic RTP management
pathway. Lacking these it is unclear whether unlicensed providers are
appropriate to clear students for RTP after mTBI or are exposed to
liability in doing so [13,14]. We feel that a pediatric trauma center
mTBI clinic and a standardized management RTP algorithm for the
treatment of students suffering from sports-related head trauma can
meet this need until a time when accepted management guidelines
and what constitutes appropriate training are more clearly dened.
This eliminates any potential conict of interest by trainers and
coaches in the management of these injuries.
Substantial barriers to the accuracy of estimating the incidence of
concussion in adolescent youth exist. Many athletes fail to report
concussions because they do not nd them to be serious (60%94%),
feel like concussions are part of game (55%89%), don't want to leave
Headache
25
20
Difficulty
Concentrating
Dizziness
15
Mentally Foggy
10
Noise Sensitivity
Light Sensitivity
Fatigue
Most Common Symptoms
Fig. 2. Most common symptoms at RTP clinic.
Fig. 4. Clearance for RTP.
344
E. Kelleher et al. / Journal of Pediatric Surgery 49 (2014) 341344
the game (41%67%), don't know they had a concussion (36%67%),
and don't want to let their teammates down (up to 32%39%) [15,16].
The combination of these factors has resulted in a signicant and
alarming rate of underreporting. It has been reported that up to 53%
80% of athletes may not report their concussion [1517].
Although small in sample size, our underreported rate for potential
mTBI, at 22.5%, is lower than previous reports. This may result from
increased concussion coverage in the scientic, medical, and popular
media, increased knowledge and awareness of concussion symptoms
among athletes and athletic trainers, and possible increased awareness of the consequences associated with concussions [18,19]. This
suggests that a community education and awareness program
initiated by a regional pediatric trauma center, integrated with the
provision of care in an mTBI clinic can both result in a greater
recognition of injuries and reduce the problem of underreporting.
These observational data offer a proof-of-concept report supporting the implementation and impact of a regional pediatric
trauma center mTBI clinic on the management of concussion within
a pilot program.
The algorithm used in this pilot program was based on grade,
history of concussion, symptoms and physical exam. The algorithm
recommends a specic asymptomatic period prior to being cleared for
a graded RTP as suggested by the 1997 AAN guidelines [11]. It is
unclear if this additional rest period is warranted, especially given the
recommendation of a graded RTP before full contact. Current
guidelines do not utilize grade of concussion in RTP clearance and it
is uncertain if this element is important in an algorithm. A randomized
multicenter trial with varying algorithms should be investigated to
determine an appropriate and safe algorithm that could be consistently utilized by providers in an effort to further streamline RTP and
decrease health care costs.
4. Conclusion
A regional pediatric trauma center in conjunction with three
local high schools, was successful in developing a pilot mTBI clinic, to
evaluate and manage adolescent athletes suffering from concussive
events with a standardized return-to-play algorithm. The unreported
mTBI episodes were lower (22.5%) than previously published selfreported mTBI rates suggesting a potential impact of the educational
process involved. The RTP algorithm used was successful in returning
athletes in 16.9 days. This algorithm and data regarding an RTP clinic
can be utilized by other organizations in the establishment of their
own RTP program and justify expanded implementation.
References
[1] McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in
sport 3rd international conference in concussion in sport held in Zurich,
November 2008. Clin J Sport Med 2009;19:185200.
[2] Barkhoudarian G, Hovda DA, Giza CC. The molecular pathophysiology of
concussive brain injury. Clin Sports Med 2011;30:3348.
[3] Leddy JJ, Sandhu H, Sodhi V, et al. Rehabilitation of concussion and postconcussion syndrome. Sports Health 2012;4(2):14754.
[4] Cantu RC, Guskiewicz K, Register-Mihalik JK. A retrospective clinical analysis of
moderate to severe athletic concussions. Phys Med Rehabil 2010;2:108893.
[5] Grady MF. Concussion in the adolescent athlete. Curr Probl Pediatr Adolesc Health
Care 2010;40:15469.
[6] Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of
traumatic brain injury: a brief overview. J Head Trauma Rehabil 2006;21(5):3758.
[7] Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA
1999;282:95863.
[8] Giza CC, Kutcher JS, Ashwald S, et al. Summary of evidence-based guideline
update: evaluation and management of concussion in sports: report of the
guideline development subcommittee on the American Academy of Neurology
[published online ahead of print March 18,2013]. Neurology 2013;80:22507.
http://dx.doi.org/10.1212/WNL.0b013e31828d57dd.
[9] Halstead ME, Walter KD. The Council on Sports Medicine and Fitness: sportrelated concussion in children and adolescents. Pediatrics 2010;126:597615.
[10] Gioia GA. Pediatric assessment and management of concussions. Pediatr Ann
2012;41:198203.
[11] American Academy of Neurology. Practice parameter: the management of
concussion in sports (summary statement). Neurology 1997;48:5815.
[12] Report of the Sports Medicine Committee. Guidelines for the management of
concussion in sports. Colorado Medical Society; 1990 [(Revised May 1991). Class III].
[13] Osborne B. Principles of liability of athletic trainers: managing sports-related
concussion. J Athl Train 2001;36(3):31621.
[14] Williams N, Sas A, Madey J, et al. High school coaches perception of physicians
role in the assessment and management of sports-related concussive injury. Front
Neurol 2012;3:14.
[15] McCrea M, Hammeke T, Olsen F, et al. Unreported concussion in high school
football players: implications for prevention. Clin J Sport Med 2004;14:137.
[16] Broglio SP, Vagnozzi R, Sabin M, et al. Concussion occurrence and knowledge in
Italian football (soccer). J Sports Sci Med 2010;9:41830.
[17] Williamson IJS, Goodman D. Converging evidence for the under-reporting of
concussions in youth ice hockey. B J Sports Med 2006;40:12832.
[18] Daneshvar DH, Nowinski CJ, McKee AC, et al. The epidemiology of sport-related
concussion. Clin Sports Med Jan 2011;30(1):117.
[19] McCrory P. Future advances and areas of future focus in the treatment of sportrelated concussion. Clin Sports Med Jan 2011;30(1):2018.
You might also like
- Howard County [Md] Public Schools Athletic Director Annual Report to Bd of Ed, Re High School Sports Program p. 15 Concussion Stats by Sport p. 14 Limit on In-season Football Contact Practices to 2 Per WeekDocument15 pagesHoward County [Md] Public Schools Athletic Director Annual Report to Bd of Ed, Re High School Sports Program p. 15 Concussion Stats by Sport p. 14 Limit on In-season Football Contact Practices to 2 Per WeekConcussion_MCPS_MdNo ratings yet
- Symposium Poster 15Document1 pageSymposium Poster 15api-305509371No ratings yet
- Policies and Programs On Concussions For Public Schools and Youth Sport ProgramsDocument19 pagesPolicies and Programs On Concussions For Public Schools and Youth Sport ProgramsConcussion_MCPS_MdNo ratings yet
- 641 MoreInfoH5 81586 PDFDocument4 pages641 MoreInfoH5 81586 PDFImPACTTestNo ratings yet
- Pi Is 1556370715000784Document7 pagesPi Is 1556370715000784Guillermo HuertaNo ratings yet
- 602 MoreInfoH1 30709 PDFDocument4 pages602 MoreInfoH1 30709 PDFImPACTTestNo ratings yet
- Traumatic Brain Injury GuidelinesDocument108 pagesTraumatic Brain Injury GuidelinesMu Z100% (1)
- MD BD of Education Sports Concussion Regulation Approved 05-21-2013 Unofficial COMAR 13A.06.08.01Document4 pagesMD BD of Education Sports Concussion Regulation Approved 05-21-2013 Unofficial COMAR 13A.06.08.01Concussion_MCPS_MdNo ratings yet
- Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and AdolescentsDocument11 pagesAssociation Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and AdolescentsCTV OttawaNo ratings yet
- Football Injuries: A Clinical Guide to In-Season ManagementFrom EverandFootball Injuries: A Clinical Guide to In-Season ManagementKevin W. FarmerNo ratings yet
- Short Review - Morgan ShermanDocument5 pagesShort Review - Morgan Shermanapi-303131314No ratings yet
- Moser Schatz JordanDocument7 pagesMoser Schatz JordanClaudiu_1105No ratings yet
- Lesiones en La AUDLDocument10 pagesLesiones en La AUDLJorge Andres Suarez CameroNo ratings yet
- Journal of Science and Medicine in SportDocument6 pagesJournal of Science and Medicine in SportAlvaro FernandoNo ratings yet
- Rhim 2020Document9 pagesRhim 2020MatkoNo ratings yet
- Athletes' Use of Mental Skills During Sport Injury Rehabilitation - AspDocument10 pagesAthletes' Use of Mental Skills During Sport Injury Rehabilitation - AspKoffi GáborNo ratings yet
- Attr 55 06 563 572 Mills FinalDocument10 pagesAttr 55 06 563 572 Mills FinalMary ErasNo ratings yet
- Concussion Management Protocols: Cynthia Dilaura Devore, M.D., M.A., M.S., F.A.A.PDocument25 pagesConcussion Management Protocols: Cynthia Dilaura Devore, M.D., M.A., M.S., F.A.A.PkitsilcNo ratings yet
- What Are The Health Challenges An Esport Player Faces and How Can They Be Addressed by StakeholdersDocument7 pagesWhat Are The Health Challenges An Esport Player Faces and How Can They Be Addressed by Stakeholders01 Anjali VardaniNo ratings yet
- Question NoDocument4 pagesQuestion Noifsha akhlaqNo ratings yet
- Preparticipation Injury Complaint Is A Risk Factor For Injury: A Prospective Study of The Moscow 2013 IAAF ChampionshipsDocument8 pagesPreparticipation Injury Complaint Is A Risk Factor For Injury: A Prospective Study of The Moscow 2013 IAAF ChampionshipsBagus Indra KusumaNo ratings yet
- Seizures and Cognitive Outcome After Traumatic Brain Injury: A Post Hoc AnalysisDocument9 pagesSeizures and Cognitive Outcome After Traumatic Brain Injury: A Post Hoc AnalysisAlexisBallénNo ratings yet
- Exercise Physiology for the Pediatric and Congenital CardiologistFrom EverandExercise Physiology for the Pediatric and Congenital CardiologistNo ratings yet
- SuggsfinallitreviewDocument7 pagesSuggsfinallitreviewapi-426365553No ratings yet
- GBCRDocument43 pagesGBCRapi-609515775No ratings yet
- Milewski 2014Document5 pagesMilewski 2014Ádám GusztafikNo ratings yet
- Injuries, Risk Factors and Prevention Initiatives in Youth SportDocument27 pagesInjuries, Risk Factors and Prevention Initiatives in Youth SportDonny KurniawanNo ratings yet
- Manuscript NNRDocument23 pagesManuscript NNRNidya YunazNo ratings yet
- Portfolio Project: EDUC 765: Trends and Issues in Instructional DesignDocument25 pagesPortfolio Project: EDUC 765: Trends and Issues in Instructional Designapi-334077930No ratings yet
- Sports PhysicalsDocument18 pagesSports PhysicalsAndika Laksmana Kurniadi100% (1)
- Concussion Rates in Youth Soccer on the RiseDocument5 pagesConcussion Rates in Youth Soccer on the RiseLuvanor SantanaNo ratings yet
- Effects of Exercise On Quality of Life in Stroke Survivors: A Meta-AnalysisDocument12 pagesEffects of Exercise On Quality of Life in Stroke Survivors: A Meta-AnalysisNoor KameliaNo ratings yet
- Pre-Participation Physical ExamDocument2 pagesPre-Participation Physical ExamTeoNo ratings yet
- Adolescent perceptions of health-related quality of life one year after concussionDocument8 pagesAdolescent perceptions of health-related quality of life one year after concussioncheree iadevaiaNo ratings yet
- Final Cat 2Document20 pagesFinal Cat 2api-458845384No ratings yet
- An Intensive Virtual Reality Program Improves Functional Balance and Mobility of Adolescents With Cerebral PalsyDocument9 pagesAn Intensive Virtual Reality Program Improves Functional Balance and Mobility of Adolescents With Cerebral PalsyStephGrenNo ratings yet
- Chronic WhiplashDocument7 pagesChronic WhiplashsoylahijadeunvampiroNo ratings yet
- Incidence and Risk Factors For Injuries in Girls' High School Volleyball: A Study of 2072 PlayersDocument8 pagesIncidence and Risk Factors For Injuries in Girls' High School Volleyball: A Study of 2072 Playersgonzalo osorioNo ratings yet
- Spinal Cord Injury 1Document20 pagesSpinal Cord Injury 1sampathNo ratings yet
- Exercise-Based Injury Prevention in Child and Adolescent Sport - Systematic ReviewDocument16 pagesExercise-Based Injury Prevention in Child and Adolescent Sport - Systematic Reviewanon_418581607No ratings yet
- 435 MoreInfoG6 49020 PDFDocument4 pages435 MoreInfoG6 49020 PDFImPACTTestNo ratings yet
- Paper BrazilDocument6 pagesPaper BrazilMariela RojasNo ratings yet
- Pilot Evaluation of A Novel Clinical Test of Reaction Time in National Collegiate Athletic Association Division I Football PlayersDocument6 pagesPilot Evaluation of A Novel Clinical Test of Reaction Time in National Collegiate Athletic Association Division I Football PlayersAli Berkay TolalıNo ratings yet
- Functional Strength Training Versus Movement Performance Therapy For Upper Limb Motor Recovery Early After Stroke: A RCTDocument8 pagesFunctional Strength Training Versus Movement Performance Therapy For Upper Limb Motor Recovery Early After Stroke: A RCTانجمن بدنسازی ایرانNo ratings yet
- Fugl-Meyer Assessment of Sensorimotor Function After StrokeDocument27 pagesFugl-Meyer Assessment of Sensorimotor Function After StrokeBasith HalimNo ratings yet
- 482 MoreInfoG4 74924 PDFDocument4 pages482 MoreInfoG4 74924 PDFImPACTTestNo ratings yet
- The Therapeutic Effects of Exercise Training On Elderly Patients With DementiaDocument23 pagesThe Therapeutic Effects of Exercise Training On Elderly Patients With DementiamarshaNo ratings yet
- Mapping of Research Gaps in Sports Medicine in Kenya Through The Application of Evidence EDITED Ver 2Document8 pagesMapping of Research Gaps in Sports Medicine in Kenya Through The Application of Evidence EDITED Ver 2Safari AgureNo ratings yet
- Bowen Therapy and Concussion ResolutionDocument10 pagesBowen Therapy and Concussion ResolutionMichaelNo ratings yet
- A Review of Return To Plau Issues and Sports Related ConcussionDocument8 pagesA Review of Return To Plau Issues and Sports Related ConcussionMarco FerreiraNo ratings yet
- Alli Gokeller - Principles of Motor Learning in ACL RehabDocument13 pagesAlli Gokeller - Principles of Motor Learning in ACL RehabAdmirNo ratings yet
- All Things Sports:: Controversies & Clinical AdvancesDocument6 pagesAll Things Sports:: Controversies & Clinical AdvancesNidhin JoseNo ratings yet
- Narrative Report-Concussion MovieDocument2 pagesNarrative Report-Concussion MovieAsdfg QwertyNo ratings yet
- Simon, 2021. Calidad de Vida Relacionada Con La Salud en Ex Deportistas Comparados Con Deportistas No Universitarios Un Seguimiento de 5 AñosDocument8 pagesSimon, 2021. Calidad de Vida Relacionada Con La Salud en Ex Deportistas Comparados Con Deportistas No Universitarios Un Seguimiento de 5 AñosIván Lázaro IllatopaNo ratings yet
- Prognosis of Six-Month Functioning After Moderate To Severe Traumatic Brain Injury: A Systematic Review of Prospective Cohort StudiesDocument12 pagesPrognosis of Six-Month Functioning After Moderate To Severe Traumatic Brain Injury: A Systematic Review of Prospective Cohort StudiesYan Sheng HoNo ratings yet
- 16Document10 pages16TaniaZayuriRosalesOrtizNo ratings yet
- Psychological Features and Outcomes of The Back School Treatment in Patients With Chronic Non-Specific Low Back Pain. A Randomized Controlled Study.Document9 pagesPsychological Features and Outcomes of The Back School Treatment in Patients With Chronic Non-Specific Low Back Pain. A Randomized Controlled Study.pau_59No ratings yet
- 13A.06.08.01 MSDE Proposed Concussion Regulation, Redlined With Comments by ParentDocument6 pages13A.06.08.01 MSDE Proposed Concussion Regulation, Redlined With Comments by ParentConcussion_MCPS_MdNo ratings yet
- Incidencia de Lesiones en El LCA en Atletas AdolescentesDocument11 pagesIncidencia de Lesiones en El LCA en Atletas AdolescentesAna Paula TorresNo ratings yet
- Ritzer An Epidemiologic Comparison of Acute and Overuse Injuries in High School SportsInjury EpidemiologyDocument11 pagesRitzer An Epidemiologic Comparison of Acute and Overuse Injuries in High School SportsInjury EpidemiologyRahmati UnsamNo ratings yet
- ESENER 2019 Policy Brief ENDocument64 pagesESENER 2019 Policy Brief ENBegoña MartinezNo ratings yet
- Psychosocial Work Factors and Stress DisordersDocument10 pagesPsychosocial Work Factors and Stress DisordersBegoña MartinezNo ratings yet
- The Effectiveness of Mindfulness Based Programs In.4Document9 pagesThe Effectiveness of Mindfulness Based Programs In.4Begoña MartinezNo ratings yet
- Amigurumi White Rabbit Free Crochet Pattern - AmigurumiDocument18 pagesAmigurumi White Rabbit Free Crochet Pattern - AmigurumiBegoña Martinez0% (1)
- Preventing Psychosocial Risks at Work: An Evaluation Study of Labour Inspectorate InterventionsDocument8 pagesPreventing Psychosocial Risks at Work: An Evaluation Study of Labour Inspectorate InterventionsBegoña MartinezNo ratings yet
- Tryptophan-Rich Diet Is Negatively Associated Withdepression and Positively Linked To Social CognitionDocument7 pagesTryptophan-Rich Diet Is Negatively Associated Withdepression and Positively Linked To Social CognitionBegoña MartinezNo ratings yet
- International Journal of Nursing Studies: ReviewDocument14 pagesInternational Journal of Nursing Studies: ReviewBegoña MartinezNo ratings yet
- Occupational Stress Among Health Workers of A University HospitalDocument6 pagesOccupational Stress Among Health Workers of A University HospitalBegoña MartinezNo ratings yet
- 1 s2.0 S1556086415317809 MainDocument7 pages1 s2.0 S1556086415317809 MainBegoña MartinezNo ratings yet
- Better Safe Than Sorry: Methods For Risk Assessment of Psychosocial HazardsDocument18 pagesBetter Safe Than Sorry: Methods For Risk Assessment of Psychosocial HazardsBegoña MartinezNo ratings yet
- A Review of Mushrooms in Human Nutrition and HealthDocument14 pagesA Review of Mushrooms in Human Nutrition and HealthBegoña MartinezNo ratings yet
- Research in Developmental Disabilities: Matilde Taddei, Sara BulgheroniDocument6 pagesResearch in Developmental Disabilities: Matilde Taddei, Sara BulgheroniBegoña MartinezNo ratings yet
- Regulation ofN-Methyl-D-aspartic Acid (NMDA) Receptors Bymetabotropic Glutamate Receptor 7Document11 pagesRegulation ofN-Methyl-D-aspartic Acid (NMDA) Receptors Bymetabotropic Glutamate Receptor 7Begoña MartinezNo ratings yet
- International Journal of Nursing Studies: Constanze Leineweber, Staffan Marklund, Gunnar Aronsson, Klas GustafssonDocument9 pagesInternational Journal of Nursing Studies: Constanze Leineweber, Staffan Marklund, Gunnar Aronsson, Klas GustafssonBegoña MartinezNo ratings yet
- Misuse of Statistical Tests Inarchives of ClinicalNeuropsychologypublicationsDocument7 pagesMisuse of Statistical Tests Inarchives of ClinicalNeuropsychologypublicationsBegoña MartinezNo ratings yet
- 1 s2.0 S0887617704001209 MainDocument6 pages1 s2.0 S0887617704001209 MainBegoña MartinezNo ratings yet
- Confounding Obscures Our View, Effect Modification Is Part of RealityDocument2 pagesConfounding Obscures Our View, Effect Modification Is Part of RealityBegoña MartinezNo ratings yet
- 1 s2.0 S1059131116301595 MainDocument8 pages1 s2.0 S1059131116301595 MainLuisa FernandaNo ratings yet
- A Motion To Exclude and The Fixed' Versus Flexible' Battery in Forensic' Neuropsychology: Challenges To The Practice of Clinical NeuropsychologyDocument7 pagesA Motion To Exclude and The Fixed' Versus Flexible' Battery in Forensic' Neuropsychology: Challenges To The Practice of Clinical NeuropsychologyBegoña MartinezNo ratings yet
- Forensic Neuropsychology: Are We There Yet?: Jim HomDocument19 pagesForensic Neuropsychology: Are We There Yet?: Jim HomBegoña MartinezNo ratings yet
- Karate Form 1 Hand PositionsDocument7 pagesKarate Form 1 Hand PositionsBegoña MartinezNo ratings yet
- FBI (Frontal Behabioral InventoryDocument2 pagesFBI (Frontal Behabioral InventoryBegoña Martinez100% (1)
- National Academy of Neuropsychology: President's Address The Future of NeuropsychologyDocument12 pagesNational Academy of Neuropsychology: President's Address The Future of NeuropsychologyBegoña MartinezNo ratings yet
- Neuropsychologia: Andrew H. Bell, Janet H. BultitudeDocument9 pagesNeuropsychologia: Andrew H. Bell, Janet H. BultitudeBegoña MartinezNo ratings yet
- Baremos NeuronormaDocument21 pagesBaremos NeuronormaDebbieNo ratings yet
- Karate Form 1 Hand PositionsDocument7 pagesKarate Form 1 Hand PositionsBegoña MartinezNo ratings yet
- Montreal Cognitive Assessment Basic English FINAL VERSION 4 June 2014Document2 pagesMontreal Cognitive Assessment Basic English FINAL VERSION 4 June 2014Begoña Martinez100% (1)
- MoCA B Instructions FinalDocument5 pagesMoCA B Instructions FinalsequoyahNo ratings yet
- Crochet Project Planner Download 1Document1 pageCrochet Project Planner Download 1Begoña MartinezNo ratings yet
- MoCA-Test-English - 7 - 3 June - 13 PDFDocument1 pageMoCA-Test-English - 7 - 3 June - 13 PDFBegoña Martinez100% (2)
- JSSCPT Physiotherapy HandbookDocument59 pagesJSSCPT Physiotherapy HandbookAbhishek N100% (2)
- Death by Explosion of Paint ThinnerDocument3 pagesDeath by Explosion of Paint ThinnermkumNo ratings yet
- Journal of EnterologyDocument139 pagesJournal of EnterologyLenuţa SzakacsNo ratings yet
- Hospital Safe From DisastersDocument26 pagesHospital Safe From DisastersRicardo limpinNo ratings yet
- Deep Neck Space InfectionsDocument48 pagesDeep Neck Space InfectionshaneiyahNo ratings yet
- Articol Protetica StomatologieDocument5 pagesArticol Protetica StomatologieStefana NanuNo ratings yet
- Workplace BreastfeedingDocument12 pagesWorkplace Breastfeedingjonas_luceroNo ratings yet
- Multix Swing DatasheetDocument8 pagesMultix Swing Datasheetatmroo975% (4)
- Cardiac Troponin T Is Not Increased in PatientsDocument5 pagesCardiac Troponin T Is Not Increased in PatientsAnanda Putri ImsezNo ratings yet
- Gangrenous AppendicitisDocument5 pagesGangrenous Appendicitisamal.fathullahNo ratings yet
- CCT in Anaesthetics - Assessment Blueprint Aug 2010 V1.3Document14 pagesCCT in Anaesthetics - Assessment Blueprint Aug 2010 V1.3sherif11110% (1)
- Myroides Odoratum Osteomyelitis in A Diabetic Patient Case Report and Review On A Rare PathogenDocument4 pagesMyroides Odoratum Osteomyelitis in A Diabetic Patient Case Report and Review On A Rare PathogenHerald Scholarly Open AccessNo ratings yet
- Antenatally Diagnosed HydronephrosisDocument71 pagesAntenatally Diagnosed HydronephrosisrajarshikNo ratings yet
- Hospital Patient Data in HCU RoomDocument108 pagesHospital Patient Data in HCU RoomSri Ratna FitriadewiNo ratings yet
- Viva Questions 1Document15 pagesViva Questions 1Reeba Mary PrinceNo ratings yet
- NDTDocument9 pagesNDTKhaing Hsu WaiNo ratings yet
- Day Case Open Appendectomy: A Safe and Cost-Effective ProcedureDocument9 pagesDay Case Open Appendectomy: A Safe and Cost-Effective ProcedureAcademecian groupNo ratings yet
- Alex Shulgin Playboy ArticleDocument13 pagesAlex Shulgin Playboy ArticleDevon BalsavageNo ratings yet
- Book Review Aunt Minnie 4th EditionDocument1 pageBook Review Aunt Minnie 4th EditiontvrbNo ratings yet
- Karen Horney (Rubio, Retiban)Document38 pagesKaren Horney (Rubio, Retiban)Princess Joy Ann RetibanNo ratings yet
- What It Takes To Be A Doctor?Document11 pagesWhat It Takes To Be A Doctor?Marion YaoNo ratings yet
- Bair Hugger 505 OM-EnGDocument14 pagesBair Hugger 505 OM-EnGCarl AzzopardiNo ratings yet
- RH Isoimmunization (PritDocument23 pagesRH Isoimmunization (PritmaezuNo ratings yet
- Terminologies: Dr.N.Govindrajkumar MDS Professor Dept of Oral Pathology Vishnu Dental CollegeDocument23 pagesTerminologies: Dr.N.Govindrajkumar MDS Professor Dept of Oral Pathology Vishnu Dental CollegeeshwarirajNo ratings yet
- Dry Mouth SolutionsDocument4 pagesDry Mouth SolutionsbryanabauerNo ratings yet
- 1 FluidsDocument17 pages1 FluidsMae CalunsagNo ratings yet
- Immediate Care of The NewbornDocument12 pagesImmediate Care of The NewbornLucilyn EbuengaNo ratings yet
- Telemedicine Projects in West Bengal: A Presentation by Kunal YadavDocument12 pagesTelemedicine Projects in West Bengal: A Presentation by Kunal Yadavaasan shinaNo ratings yet
- DR Fazeela Abbasi - Skin SpecialistDocument2 pagesDR Fazeela Abbasi - Skin SpecialistnicechitchatNo ratings yet
- Medical Sales RepDocument2 pagesMedical Sales Repapi-78904483No ratings yet
![Howard County [Md] Public Schools
Athletic Director Annual Report to Bd of Ed,
Re High School Sports Program
p. 15 Concussion Stats by Sport
p. 14 Limit on In-season Football Contact Practices to 2 Per Week](https://imgv2-2-f.scribdassets.com/img/document/124077961/149x198/5a472ee067/1360115263?v=1)