Professional Documents
Culture Documents
1.emollients Prescribing Guideline Sept 2013
Uploaded by
kyle31Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1.emollients Prescribing Guideline Sept 2013
Uploaded by
kyle31Copyright:
Available Formats
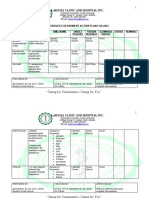
Southwark Clinical Commissioning Group
Lambeth Clinical Commissioning Group
Emollient Prescribing Guideline for Primary and Secondary Care
This guideline has been developed for use in the management of patients with a diagnosed dermatological condition or skin integrity is at risk through xerosis or
pruritus. Its application must be guided by professional judgement. Those people without a diagnosed dermatological condition requesting a general skin moisturiser
may purchase these over the counter.
The list of preferred products has been added to the Guys, Kings, Lewisham and St. Thomass Joint Medicines Formulary.
Consistency/
Formulation
Very Greasy
ointment
Greasy ointment
Preferred Products
Active Constituents
(LP = Liquid Paraffin, WSP = White Soft Paraffin, EW = Emulsifying Wax, WP = White Paraffin, LLP
= Light Liquid Paraffin, YSP = Yellow Soft Paraffin)
(Excipients listed are associated rarely with sensitisation as listed in BNF65/ MIMs online)
White soft paraffin LP 50% + WSP 50%
in liquid paraffin
(50:50)
WSP 50% + EW 30% + LP 20%
Emulsifying
Excipients: cetostearyl alcohol
ointment
Zeroderm ointment LP 40% + WSP 30% + EW
Excipients: cetearyl alcohol, polysorbate 60
Hydromol ointment YSP 30% + EW 30% + LP 40%
Excipients: cetostearyl alcohol
Creams / gels
Lotion
Advice, Restrictions and/or Similar
product
Cost per 500ml/g
(Drug Tariff + MIMs online;
August 2013)
For very dry skin and/ or acute flares. Low
risk of sensitivity.
2.36
Good for night-time, very dry skin or scaly
patches requiring softening.
Same as above
SIMILAR TO: Epaderm Ointment
Same as above
SIMILAR TO: Epaderm Ointment
SIMILAR TO: Oilatum cream and
Diprobase Cream
2.49
4.10
4.82
ZeroAQS
LP 6% + WSP 15% + macrogol cetostearyl ether 1.8%
Aquamax
WSP 20% + LP 8%
Zerocream
LP 12.6%+WSP 14.5%, anhydrous lanolin 1%
Doublebase gel
Isopropyl Myristate 15% + LP 15%
5.83
Cetraben cream
WSP 13.2% + LLP 10.5% + EW
5.99
E45 lotion
WSP 10% + LLP 4%, hypoallergenic anhydrous lanolin 1%
QV Skin lotion
WSP 5% + LP
Excipients: cetostearyl alcohol, chlorocresol
3.99
Excipients: cetostearyl alcohol, polysorbate 60, phenoxyethanol
Excipients: cetyl alcohol, hydroxybenzoates (parabens)
SIMILAR TO: E45 cream
(note this contains hypoallergenic anhydrous lanolin)
Excipients: triethanolamine, phenoxyethanol
Excipients: cetostearyl alcohol, phenoxyethanol, hydroxybenzoates (parabens)
Excipients: benzyl alcohol, isopropyl palmitate, hydroxybenzoates (parabens)
Excipients: cetostearyl Alcohol, hydroxybenzoates (parabens)
3.29
Lighter formulation suitable for
application to hairy areas, skin folds, face
or scalp
(ACBS: see BNF drug monograph)
Same as above
This document was developed by clinicians of NHS Lambeth CCG, NHS Southwark CCG, Departments of Dermatology and Pharmacy GSTFT & KCH.
Please direct any queries to LAMCCG.medicinesmanagement@nhs.net or SOUCCG.medicines-management@nhs.net
Approved by: NHS Lambeth CCG and NHS Southwark CCG Joint Prescribing Committee Date: Sept 2013 Review date: Sept 2015 Page 1 of 4
4.08
4.50
5.18
Southwark Clinical Commissioning Group
Lambeth Clinical Commissioning Group
Preparations
containing antimicrobials
Dermol 500 lotion
LP 2.5% + benzalkonium chloride 0.1% + chlorhexidine
dihydrochloride 0.1% + isopropyl myristate 2.5%
Short term use to wash and/ or as a leave
on emollient during skin infection only
6.04
LP 10% + benzalkonium chloride 0.1% + chlorhexidine
dihydrochloride 0.1% + isopropyl myristate 10%
Same as above
6.63
Chlorhexidine gluconate solution 1%, LP + WSP
Same as above
Excipients: cetostearyl alcohol, phenoxyethanol
Dermol cream
Excipients: cetostearyl alcohol, phenoxyethanol
Eczmol cream
(lotion)
Soap substitute
Preparations
containing urea
Spray emollient
7.40
(3.70 = 250ml)
Use any cream or ointment above as a soap substitute in the bath/shower; except 50:50 (since it may not lather well)
Balneum cream
Urea 5% + ceramides 0.1%
Useful where a keratolytic is required e.g.
9.97
hyperkeratosis, ichthyosis, extremely dry
and/ or fissured skin on hands and feet
Aquadrate cream/
Urea 10% + WSP
Same as above
21.85
Hydromol Intensive
(4.37 = 100g)
cream
Emollin
LP 50% + WSP 50%
For very painful/ fragile skin where there
13.04
Excipients: cetostearyl alcohol, polysorbates, propylene glycol
is difficulty with hands on application of
(6.26 = 240ml)
creams / ointments only
Excipients: cetostearyl alcohol
FOR USE IN EXCEPTIONAL/SPECIFIED SITUATIONS ONLY
Bath emollients/
Wash products
Hydromol bath and
shower emollient
LLP 37.8% + isopropyl myristate 13%
4.11
LLP 85.09%
To wash dry scalps/ as soap substitutes
where other emollients are unsuitable/
not tolerated
Note: Risk of slipping in bath.
Same as above
QV Bath oil
Dermol 600 bath
emollient with
antimicrobial
LP 25% + benzalkonium chloride 0.5% + isopropyl myristate
25%
Short term use during skin infection only
Tissue viability - Leg ulcer wash only
7.55 (600ml)
Excipients: hydroxybenzoates (parabens)
Excipients: polysorbate 60
4.66
Acknowledgements: Our thanks go to Dr Catherine Smith (Consultant Dermatologist GSTFT), Dr Emma Wedgeworth (Consultant Paediatric Dermatologist GSTFT), Dr Sarah Walsh (Consultant Dermatologist KCHFT), Karina Jackson
(Consultant Nurse GSTFT), Arlene McGuire (Dermatology Pharmacist GSTFT), Charlotte Bell (Dermatology Pharmacist KCHFT), Dr Naomi Kemp (GPwSI Southwark), Dr Dianne Aitken (GP Lambeth) and Dr Elizabeth Williams (GP
Lambeth) for giving their time & expert advice to produce this document.
References: 1.Primary Care Dermatology Society & British Association of Dermatologists Guidelines for the management of atopic eczema, SKIN Vol 39 Oct 2009; http://www.bad.org.uk/Portals/_Bad/Guidelines/Clinical%20Guidelines/PCDS-
BAD%20Eczema%20reviewed%202010.pdf 2. NICE Clinical Knowledge Summaries; http://cks.nice.org.uk/dermatitis-contact#!prescribinginfosub:3 3. BNF 65 March Sept 2013; http://www.medicinescomplete.com/mc/bnf/current/PHP7454-suitable-quantities-forprescribing.htm; 4. NICE Clinical Guideline 57 Atopic eczema in children December 2007 http://www.nice.org.uk/nicemedia/live/11901/38566/38566.pdf; 5. NHS Choices; http://www.nhs.uk/conditions/emollients/Pages/Introduction.aspx; 6. NHS National Patient
Safety Agency Rapid Response Report 4 Fire hazard with paraffin based skin products on dressings and clothing November 2007; http://www.nrls.npsa.nhs.uk/resources/?entryid45=59876; 7. British Dermatological Nursing Group Best Practice in Emollient Therapy A
Statement for Healthcare Professionals; Dermatological Nursing, 2012, Vol 11, No 4; 8. MHRA Drug Safety Update, Volume 6, issue 8, March 2013: Aqueous cream: may cause skin irritation, particularly in children with eczema, possibly due to sodium lauryl sulfate
content; http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON254804
This document was developed by clinicians of NHS Lambeth CCG, NHS Southwark CCG, Departments of Dermatology and Pharmacy GSTFT & KCH.
Please direct any queries to LAMCCG.medicinesmanagement@nhs.net or SOUCCG.medicines-management@nhs.net
Approved by: NHS Lambeth CCG and NHS Southwark CCG Joint Prescribing Committee Date: Sept 2013 Review date: Sept 2015 Page 2 of 4
Southwark Clinical Commissioning Group
Lambeth Clinical Commissioning Group
KEY INFORMATION FOR EMOLLIENT PRESCRIBING:
Emollients are essential in the management of diagnosed dermatological conditions but are often underused. When used
correctly, emollients can help maintain and/or restore skin suppleness, prevent dry skin & itching; reduce the number of
flare-ups there-by reducing the need for corticosteroid treatment, in addition to other benefits. They should continue to be
used even after the skin condition has cleared if the clinical condition justifies continued use e.g. evidence of chronic
relapsing eczema.
Assess patient to diagnose a dermatological condition such as eczema, psoriasis or symptomatic xerosis or pruritus caused
by systemic disease that threatens skin integrity e.g. in older patients.
Emollients can be purchased over the counter by patients who do not have a diagnosed dermatological condition or risk to
1
skin integrity. (For diagnostic criteria for atopic eczema refer to the guidelines for the management of atopic eczema ).
2
There is no evidence from controlled trials to support the use of one emollient over another therefore selection is based on
the known physiological properties of emollients, patient acceptability, dryness of the skin, area of skin involved and lowest
acquisition cost.
All primary and secondary care prescribers should where possible select the emollient with the lowest acquisition cost from
the range available in our agreed preferred product list.
Newly diagnosed patients:
Offer the product with the lowest acquisition cost from the above preferred list appropriate to their condition.
Existing patients with a diagnosed dermatological condition prescribed an emollient outside the preferred product list:
Review with a view to trialling a preferred emollient from the list above. If after discussion with the patient, they agree to
switch existing emollient therapy, offer the product with the lowest acquisition cost from the above list by emollient
formulation. If the patient prefers to continue on their existing product this choice should be respected.
Patients who have been reviewed in secondary care and require an emollient outside the preferred product list:
The rationale for the request should be provided to the primary care prescriber in writing and the request respected.
Sufficient quantities should be prescribed to allow liberal application as frequently as required.
The quantity of emollient prescribed will vary depending on:
the size of the person
extent and severity of the dermatological condition
if the emollient is also being used as a soap substitute
As a guide, in generalised eczema, the recommended quantities used are 600 g/week for an adult and 250-500 g/week for a
4
child .
Also offer smaller quantity packs for use at school or work in addition to the main prescription.
This table suggests suitable quantities to be prescribed for an adult for a minimum of twice daily application for one week.
3
For children approximately half this amount is suitable
Area
Face
Both hands
Scalp
Both arms or both
Trunk
Groin & genitalia
affected
legs
Creams and
1530g
2550g
50100g
100200g
400g
1525g
ointments
Lotions
100ml
200ml
200ml
200ml
500ml
100ml
Prescribe up to two different types of emollient to use at different times of day / different body areas / for when condition
severity varies - one of which can be used as a soap substitute as well.
Emollient creams/ointments should be used as soap substitutes for washing as conventional soaps/wash products strip the
skin of natural oils & cause shedding of skin cells.
Locally, emollient bath additives are no longer considered a standard component of 'total emollient therapy' and so
should only be prescribed in the specified circumstances in the preferred list.
The amount of emollient deposited on the skin during bathing/showering is likely to be far lower than with directly applied
emollient creams/ointments. Bath additive emollients will coat the bath and make it greasy and slippery.
If the patient requests a bath additive outside of the preferred list recommended use, any ointment (except 50:50) can be
dissolved in some hot water and added to the bath water as a bath additive and/or use of a cream emollient as a soap
substitute in the bath will offer similar emollient effect.
Aqueous cream is no longer considered suitable as a leave-on emollient or soap substitute for diagnosed dermatological
8
conditions due to its tendency to cause irritant reactions and availability of emollient creams with a lower acquisition cost .
Emollients containing urea, antimicrobials etc. are not generally recommended as the evidence to support their use is
2
limited ; however they may be useful in a select group of patients (see preferred list).
Colloidal oatmeal containing emollients are borderline substances & may only be prescribed in accordance with the advice
of the Advisory Committee on Borderline Substances (ACBS) for the clinical conditions listed (see current BNF).
This document was developed by clinicians of NHS Lambeth CCG, NHS Southwark CCG, Departments of Dermatology and Pharmacy GSTFT & KCH.
Please direct any queries to LAMCCG.medicinesmanagement@nhs.net or SOUCCG.medicines-management@nhs.net
Approved by: NHS Lambeth CCG and NHS Southwark CCG Joint Prescribing Committee Date: Sept 2013 Review date: Sept 2015 Page 3 of 4
Southwark Clinical Commissioning Group
Lambeth Clinical Commissioning Group
Counselling points for patients/parents/carers
WHAT is an Emollient?
Emollients (sometimes called moisturisers) are creams, ointments and lotions which help to prevent dry skin and
itching by keeping it soft and moist and reduce the number of skin flare ups.
What is the DIFFERENCE between emollients?
The difference between lotions, creams and ointments is their content of oil (lipid) and water. The oil content is
lowest in lotions, intermediate in creams and highest in ointments. The higher the oil content, the greasier and
stickier it feels and the shinier it looks on the skin.
As a general rule, the higher the oil content (the more greasy and thick the emollient), the better and longer it
works but it may be messier to use.
Ointments: greasiest, usually do not contain preservatives (ingredients to help protect the product from
bacteria/germs and increase its shelf-life) therefore are associated with less skin sensitivities, good for
moderate-severe dry skin and night time application.
Creams: less greasy, normally contain preservatives so may cause skin irritation, usually need to be applied more
often than ointments, good for day time application and weeping eczema.
Lotions: good for mildly dry skin, hairy areas of skin, face or weeping eczema; normally contain preservatives so
may cause skin irritation.
WHICH Emollient is best?
There is no best emollient. The type (or types) to use depends on the dryness of the skin, the area of skin
involved and patient preference.
More than one emollient may be required for use at different times of the day or for when the skin condition is
more active.
HOW and WHEN to USE/APPLY an emollient?
Wash & dry hands before applying emollients to reduce the risk of introducing germs to the skin.
If using a tub, remove the required amount of emollient from the tub onto a clean plate/bowl using a
spatula/teaspoon to prevent introduction of germs to the container.
Apply emollients whenever the skin feels dry/ as often as you need. This may be 2-4 times a day or more.
Apply emollients immediately after washing or bathing when skin has been dabbed dry. Emollients can and
should be applied at other times during the day e.g. in extreme weather to provide a barrier from the cold.
Emollients should continue to be used after the skin condition has cleared if the clinical condition justifies
continued use. This will be assessed by your doctor or nurse.
Apply by smoothing them into the skin in the direction the body hair naturally lies, rather than rubbing them
in.
Emollients should be used as a soap substitute, as normal soap tends to dry the skin.
Intensive use of emollients can reduce the need for topical corticosteroids, the quantity and frequency of use of
emollients should be far greater than that of other therapies given.
If a topical corticosteroid is required, emollients should be applied at least 15-30 minutes before or after the
topical corticosteroid.
Paraffin-based emollients are flammable; take care near any open flames or potential causes of ignition such
as cigarettes.
WHERE to go for FURTHER INFORMATION
NHS Choices (http://www.nhs.uk)
National Eczema Society (http://www.eczema.org)
British Skin Foundation (http://www.britishskinfoundation.org.uk/Home.aspx)
National Psoriasis Foundation (http://www.psoriasis.org)
Primary Care Dermatology Society atopic eczema(http://www.pcds.org.uk/clinical-guidance/atopiceczema#management)
British Association of Dermatologists patient information leaflets (http://www.bad.org.uk)
(This is not an exhaustive list)
This document was developed by clinicians of NHS Lambeth CCG, NHS Southwark CCG, Departments of Dermatology and Pharmacy GSTFT & KCH.
Please direct any queries to LAMCCG.medicinesmanagement@nhs.net or SOUCCG.medicines-management@nhs.net
Approved by: NHS Lambeth CCG and NHS Southwark CCG Joint Prescribing Committee Date: Sept 2013 Review date: Sept 2015 Page 4 of 4
You might also like
- Pharmaceutical PreparationsDocument40 pagesPharmaceutical PreparationsAreej Hamid50% (2)
- Emollient Guide Adults and Children June 2018Document4 pagesEmollient Guide Adults and Children June 2018Shinichi Ferry RoferdiNo ratings yet
- Homemade Beauty Products: Easy DIY Recipes & Holistic Solutions for Glowing Skin and Beautiful HairFrom EverandHomemade Beauty Products: Easy DIY Recipes & Holistic Solutions for Glowing Skin and Beautiful HairNo ratings yet
- Cosmetics Help Treat Acne VulgarisDocument7 pagesCosmetics Help Treat Acne VulgarisJihanNo ratings yet
- Formulating With Cationic EmulsifiersDocument16 pagesFormulating With Cationic EmulsifiersherfuentesNo ratings yet
- Dermatological Therapy GuideDocument46 pagesDermatological Therapy GuideKevin BlackNo ratings yet
- OintmentsDocument74 pagesOintmentsJezreel JavierNo ratings yet
- Kuliah Dermato Terapi 2013Document46 pagesKuliah Dermato Terapi 2013Vania EssiandaNo ratings yet
- Dermocalm LotionDocument5 pagesDermocalm LotionSai KrishnaNo ratings yet
- Unit V Lecture on Parenteral Products Formulation and PackagingDocument29 pagesUnit V Lecture on Parenteral Products Formulation and PackagingHamid Hussain HamidNo ratings yet
- Dermatopharmatology: Aldilanoviatri Timpengajarfarmakoterapi Fkhub 2 0 1 8Document64 pagesDermatopharmatology: Aldilanoviatri Timpengajarfarmakoterapi Fkhub 2 0 1 8Nadiya ShiyamahNo ratings yet
- Emoderm CreamDocument4 pagesEmoderm CreamSM ZuhailNo ratings yet
- Efficacy Evaluation of Different Cream Formulations On Healthy Skin PropertiesDocument8 pagesEfficacy Evaluation of Different Cream Formulations On Healthy Skin Propertieslab.kalibrasi BBPOM di SurabayaNo ratings yet
- PCT 212 Week 15-16Document13 pagesPCT 212 Week 15-16Oluwaseun OladipupoNo ratings yet
- Bepanthen Plus Cream Treats Skin InfectionsDocument3 pagesBepanthen Plus Cream Treats Skin InfectionsWaqar AhmedNo ratings yet
- Cosmetics 05 00011Document21 pagesCosmetics 05 00011Alexandra AlomanNo ratings yet
- Topical FormulationsDocument8 pagesTopical FormulationsjaimurugeshNo ratings yet
- Coco Scalpoint PDFDocument4 pagesCoco Scalpoint PDFBaluNo ratings yet
- Topical Drug Delivery Systems: DR Khalid Sheikh Department of Pharmaceutics Room 419 EmailDocument36 pagesTopical Drug Delivery Systems: DR Khalid Sheikh Department of Pharmaceutics Room 419 Emailchegu BusinessNo ratings yet
- Come Do GenicDocument7 pagesCome Do GenicdokterasadNo ratings yet
- Treating Skin Diseases NaturallyDocument26 pagesTreating Skin Diseases NaturallyM Dicky HidayatullahNo ratings yet
- Inolex PCAsia SkinLight Jan13Document4 pagesInolex PCAsia SkinLight Jan13Violeta StoynovaNo ratings yet
- Typing Jaaaabs 2nd PartDocument9 pagesTyping Jaaaabs 2nd PartXyries Blues IlagaNo ratings yet
- Cele TequeDocument14 pagesCele TequeJoycee PerezNo ratings yet
- Astringents & Bleaching AgentsDocument40 pagesAstringents & Bleaching AgentssujataNo ratings yet
- Skin Moisturizing Effects of Panthenol Based FormulationsDocument10 pagesSkin Moisturizing Effects of Panthenol Based FormulationsYudha Amandangi SyahputeraNo ratings yet
- Topical FormulationsDocument5 pagesTopical FormulationsSandeep GargNo ratings yet
- Bepanthen Ointment Professional Information PDFDocument3 pagesBepanthen Ointment Professional Information PDFmulugeta ayeleNo ratings yet
- Steroid Potency ChartDocument3 pagesSteroid Potency ChartGee Thanabhorn100% (3)
- Adaferin cream detailsDocument6 pagesAdaferin cream detailsddandan_2No ratings yet
- Lanolin 6ppDocument6 pagesLanolin 6ppicrao100% (1)
- Module 23 HiquinDocument27 pagesModule 23 HiquinHasan AliraqiNo ratings yet
- Topical Formulation DevelopmentDocument5 pagesTopical Formulation DevelopmentjaimurugeshNo ratings yet
- Review of Artificial Tears and Ocular Lubricants For The Treatment of Dry EyeDocument10 pagesReview of Artificial Tears and Ocular Lubricants For The Treatment of Dry Eyearyati yayaNo ratings yet
- Materi KrimDocument20 pagesMateri Krimsiti salma haniyyahNo ratings yet
- Quiz answer skin care products pricesDocument3 pagesQuiz answer skin care products pricesadeNo ratings yet
- Product Leaflet Verstatil RangeDocument7 pagesProduct Leaflet Verstatil RangegowestcreativeNo ratings yet
- Ointment Cream and GelsDocument79 pagesOintment Cream and GelsGwyneth Cartalla100% (2)
- Advanced Chemical Peels - Notes of InterstDocument4 pagesAdvanced Chemical Peels - Notes of Interstgeraffe100% (3)
- Emulsions 2019Document37 pagesEmulsions 2019Ayman WaddadNo ratings yet
- Allergies To Cosmetic IngredientsDocument1 pageAllergies To Cosmetic IngredientsHelNo ratings yet
- Topical Corticosteroids: A Guide to Potency, Application, and DosingDocument59 pagesTopical Corticosteroids: A Guide to Potency, Application, and DosingdrbhaveshpNo ratings yet
- 47-Drug Acting On Skin and MucousDocument3 pages47-Drug Acting On Skin and MucousMuhammad Sarmad MalikNo ratings yet
- Formulation and evaluation of clotrimazole and ichthammol ointmentDocument10 pagesFormulation and evaluation of clotrimazole and ichthammol ointmentDindaNo ratings yet
- 1,4-DIOXANE: FOUND IN: Products That Create Suds (Such As Shampoo, LiquidDocument7 pages1,4-DIOXANE: FOUND IN: Products That Create Suds (Such As Shampoo, Liquidranni94No ratings yet
- Arlamol PS15E - 0314 PCDS256v2 PDFDocument2 pagesArlamol PS15E - 0314 PCDS256v2 PDFsimmiNo ratings yet
- International Journal of Pharmacy and Pharmaceutical SciencesDocument9 pagesInternational Journal of Pharmacy and Pharmaceutical SciencesEslam Mohamed HamedNo ratings yet
- Adrmg CapecitabineDocument9 pagesAdrmg CapecitabineLauraNo ratings yet
- Prinsip Obat-Obat KulitDocument21 pagesPrinsip Obat-Obat Kulitnathanielfarrel96No ratings yet
- Hydromol Bath Shower EmollientDocument4 pagesHydromol Bath Shower Emollientyussf.hsNo ratings yet
- Topical Drugs Therapy in DermatologyDocument43 pagesTopical Drugs Therapy in DermatologyhudaNo ratings yet
- Lightening efficacy of tamarind fruit extract cleansing lotionDocument7 pagesLightening efficacy of tamarind fruit extract cleansing lotionarryandi01No ratings yet
- Mr. Saran Kumar Das Ms. Deepika U M.Pharm Department of PharmaceuticsDocument36 pagesMr. Saran Kumar Das Ms. Deepika U M.Pharm Department of PharmaceuticsChilaNo ratings yet
- Final HODocument15 pagesFinal HOMoonrich Dayle BallestraNo ratings yet
- High-Performance Liquid Chromatographic Determination of Arbutin in Skin-Whitening Creams and Medicinal Plant ExtractsDocument10 pagesHigh-Performance Liquid Chromatographic Determination of Arbutin in Skin-Whitening Creams and Medicinal Plant ExtractsSahera Nurhidayah NasutionNo ratings yet
- Natural herbal cosmetic cream from Aloe vera, Cucumis sativus and Daucus carotaDocument6 pagesNatural herbal cosmetic cream from Aloe vera, Cucumis sativus and Daucus carotafebriantiNo ratings yet
- Dermal FillersDocument13 pagesDermal FillersAhmed Badawy100% (1)
- Natural Emulsifiers and Preservative Factsheet FINALDocument8 pagesNatural Emulsifiers and Preservative Factsheet FINALFrederick HeisenbergNo ratings yet
- JCN 11 E34Document8 pagesJCN 11 E34kakarafnieNo ratings yet
- ECR2014Document9 pagesECR2014kyle31No ratings yet
- Medical LatinDocument14 pagesMedical Latinjadephoebe0% (1)
- Gari BayDocument18 pagesGari Baykyle31No ratings yet
- Modified Alvarado Scoring SystemDocument5 pagesModified Alvarado Scoring Systemkyle31No ratings yet
- Blepharitis PPPDocument31 pagesBlepharitis PPPkyle31No ratings yet
- Blood Pressure Health EnglishDocument14 pagesBlood Pressure Health EnglishRajeshNo ratings yet
- Acs PatientinformationDocument8 pagesAcs PatientinformationAtmiHadjiNo ratings yet
- 6Document13 pages6kyle31No ratings yet
- Faq 177Document3 pagesFaq 177kyle31No ratings yet
- Eye EmergenciesDocument18 pagesEye EmergenciesdrDre91No ratings yet
- PF Normal Postpartum Adjustment and PMADs Understanding The Difference 0Document52 pagesPF Normal Postpartum Adjustment and PMADs Understanding The Difference 0kyle31No ratings yet
- 20Document4 pages20kyle31No ratings yet
- Abdominal Pain PDFDocument8 pagesAbdominal Pain PDFYa Ya MieLg AriezNo ratings yet
- TorchDocument8 pagesTorchfeti_08No ratings yet
- Anatomical Causes Bad Obstetric HistoryDocument3 pagesAnatomical Causes Bad Obstetric Historykyle31No ratings yet
- Toxoplasma Gondii in Woman With Bad Obstetric History and Infertility: A Five Years StudyDocument4 pagesToxoplasma Gondii in Woman With Bad Obstetric History and Infertility: A Five Years Studykyle31No ratings yet
- Karyotyping and Counseling in Bad Obstetric History and InfertilityDocument6 pagesKaryotyping and Counseling in Bad Obstetric History and Infertilitykyle31No ratings yet
- QA73 InadeqLactationDocument7 pagesQA73 InadeqLactationkyle31No ratings yet
- DIAGRAM Cutaneus Bacterial InfectionDocument1 pageDIAGRAM Cutaneus Bacterial Infectionkyle31No ratings yet
- Keberhasilan Penanganan DM Pragestasional Dengan Komplikasi BeratDocument4 pagesKeberhasilan Penanganan DM Pragestasional Dengan Komplikasi BeratWiguna Fuuzzy WuuzzyNo ratings yet
- Policy Directive: Children and Infants With Fever - Acute ManagementDocument26 pagesPolicy Directive: Children and Infants With Fever - Acute Managementkyle31No ratings yet
- Acne Vulgaris (FDA)Document17 pagesAcne Vulgaris (FDA)Doar SiregarNo ratings yet
- 20Document4 pages20kyle31No ratings yet
- 1201 10Document8 pages1201 10kyle31No ratings yet
- 2041Document5 pages2041kyle31No ratings yet
- 136 Drugs Cognitive ImpairmentDocument9 pages136 Drugs Cognitive Impairmentkyle31No ratings yet
- Approach To Skin Lesions - Learn PediatricsDocument13 pagesApproach To Skin Lesions - Learn Pediatricskyle31No ratings yet
- Common Skin Infections PDFDocument26 pagesCommon Skin Infections PDFkyle31No ratings yet
- Care Plan Handbook TemplateDocument34 pagesCare Plan Handbook TemplateBreanna Hopkins100% (1)
- PAR-Q Physical Activity Readiness QuestionnaireDocument3 pagesPAR-Q Physical Activity Readiness QuestionnaireMhervin BisisNo ratings yet
- Body Mass IndexDocument3 pagesBody Mass IndexSunnyVermaNo ratings yet
- (Đề thi có 4 trang) : Thời gian làm bài: 60 phút, không kể thời gian giao đềDocument4 pages(Đề thi có 4 trang) : Thời gian làm bài: 60 phút, không kể thời gian giao đềNguyễn HoaNo ratings yet
- Cor-Ban 27 LDocument2 pagesCor-Ban 27 LMahammadNo ratings yet
- CureDocument338 pagesCureThiago Cavalli Azambuja100% (1)
- 23 Nov 2022Document1 page23 Nov 2022Tahir ShahNo ratings yet
- Safety Practice in Sports and ExerciseDocument32 pagesSafety Practice in Sports and ExercisePrincess Reiann LopezNo ratings yet
- MAPEH 1 (2nd Quarter Complete)Document60 pagesMAPEH 1 (2nd Quarter Complete)Roselyn GutasNo ratings yet
- SOCIAL SERVICES aCTION PLAN FOR 2022Document6 pagesSOCIAL SERVICES aCTION PLAN FOR 2022Rocel Cañete Ordoyo-GabrielNo ratings yet
- Drug Study (GBS)Document16 pagesDrug Study (GBS)Mary Rose Verzosa LuisNo ratings yet
- Click To Download June2020 Edition PDFDocument30 pagesClick To Download June2020 Edition PDFJomon JohnyNo ratings yet
- Two Step TSTDocument2 pagesTwo Step TSTBrianHoNo ratings yet
- Development of Protein Rich Flavored BarDocument6 pagesDevelopment of Protein Rich Flavored BarIJRASETPublicationsNo ratings yet
- DMSCO Log Book Vol.40 1962Document73 pagesDMSCO Log Book Vol.40 1962Des Moines University Archives and Rare Book RoomNo ratings yet
- Level 1 Q& A Og - KoncptDocument14 pagesLevel 1 Q& A Og - KoncptadiNo ratings yet
- Bias and Confounding: Nayana FernandoDocument31 pagesBias and Confounding: Nayana FernandoanojNo ratings yet
- Tenecteplasa Vs AlteplasaDocument9 pagesTenecteplasa Vs AlteplasaJefferson Duque MartinezNo ratings yet
- Pi 021 2 Aide Memoire On GMP GCPDocument10 pagesPi 021 2 Aide Memoire On GMP GCPIsmail MathakiyaNo ratings yet
- INITIAL DATA BASE Form For Family 1Document5 pagesINITIAL DATA BASE Form For Family 1Reignallienn Inocencio MartinNo ratings yet
- Glaucoma Management and Target IOPDocument24 pagesGlaucoma Management and Target IOPElfi RisalmaNo ratings yet
- Chitoglucan New OverviewDocument6 pagesChitoglucan New OverviewmjmorcelliNo ratings yet
- Psych Drug StudyDocument5 pagesPsych Drug StudyLorina Lynne Apelacio100% (4)
- Pathology MBBSDocument12 pagesPathology MBBSDinah Penserga100% (1)
- A 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaDocument5 pagesA 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaYUSUF MUSANo ratings yet
- Course Content Related To Chronic Wounds in Nursing Degree Programs in SpainDocument2 pagesCourse Content Related To Chronic Wounds in Nursing Degree Programs in SpainMikey MadRatNo ratings yet
- Wilfredo Mallari Resume Safety Supervisor UpdatedDocument1 pageWilfredo Mallari Resume Safety Supervisor Updatedwilly mallariNo ratings yet
- Enhancing Your Skills in Stroke Quality Improvement and Data AnalysisDocument50 pagesEnhancing Your Skills in Stroke Quality Improvement and Data AnalysisRaisha Klinik Vaksinasi YogyakartaNo ratings yet
- Food Contact Materials FDA NSF and Other StandardsDocument3 pagesFood Contact Materials FDA NSF and Other StandardsMuhammad Brilian Syifa HabibiNo ratings yet
- Balantidium ColiDocument7 pagesBalantidium ColiOmar GhoneimNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)