Professional Documents
Culture Documents
Gen I To Urinary
Uploaded by
Mohamed Rikarz Ahamed RikarzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gen I To Urinary
Uploaded by
Mohamed Rikarz Ahamed RikarzCopyright:
Available Formats
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 67-year-old male presents after having a urine tract infection treated and has read in a magazine that maybe
Test Analysis
it would be worth checking a PSA.
When should his PSA be checked?
(Please select 1 option)
Check in three days
Check in one week
Check in two weeks
Check on this occasion
No need to check PSA
Submit answer
Skip question
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 67-year-old male presents after having a urine tract infection treated and has read in a magazine that maybe
Answer Statistics
it would be worth checking a PSA.
When should his PSA be checked?
Test Analysis
(Please select 1 option)
Check in three days
Incorrect answer selected
Check in one week
Check in two weeks
This is the correct answer
Check on this occasion
No need to check PSA
PSA concentrations can rise with problems of false positives after catheterisation and particularly urine tract
infections.
Therefore, if one has decided to check a PSA then it is recommended that this should be measured at least
two weeks after a treated UTI.
Score:
Please bear in mind that this is a controversial area and one where the guidelines are not completely clear.
Total Answered:
You would expect some prostatic symptoms in patients with prostatic carcinoma, but most of these will actually
have BPH rather than carcinoma. Many men will come requesting a PSA and it can be useful in those patients
with a family history, young age etc.
Feedback
Rate this question
In practice it would probably be worth checking it in a male presenting with a UTI, as such a diagnosis is fairly
rare in this age group. It is important to allow the infection to clear first however, to reduce the risk of a false
positive result.
Leave question feedback
Question Navigator
Next question
Related Articles (BMJ)
Go to summary
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 56-year-old man who has presented with chest pain, has a PSA of 45 ng/ml (normal less than 4).
Test Analysis
Which of the following statements is correct with respect to this patient's management?
(Please select 1 option)
An elevated PSA is a definitive test for prostate cancer
High selenium intake is related to prostate cancer
Prostate cancer is more aggressive with increasing age
Prostate cancer is typically squamous call carcinoma
The most commonly used pathological grading system is the Gleason score
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 56-year-old man who has presented with chest pain, has a PSA of 45 ng/ml (normal less than 4).
Answer Statistics
Which of the following statements is correct with respect to this patient's management?
Test Analysis
(Please select 1 option)
An elevated PSA is a definitive test for prostate cancer
Incorrect answer selected
High selenium intake is related to prostate cancer
Prostate cancer is more aggressive with increasing age
Prostate cancer is typically squamous call carcinoma
The most commonly used pathological grading system is the Gleason score
This is the correct answer
Prostate-specific antigen (PSA) may be elevated in prostatitis, benign prostatic hyperplasia and prostate
cancer.
High intake of animal fats is related to prostate cancer, as well as low intake of selenium.
As a rule, prostate cancer is more aggressive in younger men.
Score:
Prostate cancer is an adenocarcinoma.
Total Answered:
The Gleason score is recommended by the American College of Pathologists. The most well differentiated
Feedback
tumours have a Gleason score of 2, and the most poorly differentiated a Gleason score of 10.
Rate this question
Next question
Go to summary
Leave question feedback
Related Articles (BMJ)
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 46-year-old homosexual HIV positive man presents with a two week history of weakness of his right arm and
Answer Statistics
leg.
Examination reveals right hemiparesis and left cerebellar signs. CT scan shows white matter lesions in the left
cerebellar region and left temporoparietal area. There is no midline shift or surrounding oedema.
Test Analysis
Which one of the following is most likely to be found in his cerebrospinal fluid (CSF)?
(Please select 1 option)
Positive cytomegalovirus (CMV) PCR
Incorrect answer selected
Positive Epstein-Barr virus (EBV) PCR
Positive herpes simplex virus (HSV) PCR
Positive human herpes virus (HHV) 8 PCR
Positive JC PCR
This is the correct answer
Multifocal lesions in left cerebellar and temporoparietal white matter areas without any mass effect or
surrounding oedema are most likely to be due to progressive multifocal leucoencephalopathy (PML).
Score:
JC virus causes PML in immunocompromised patients especially when the CD4 count is below 100 cells/mm 3 .
Total Answered:
CMV polymerase chain reaction (PCR) may be found in CMV encephalitis. It is clinically not a typical feature of
CMV encephalitis.
Feedback
Positive EBV PCR indicates primary brain lymphoma where CT scan often shows significant mass effect with
surrounding oedema.
Rate this question
HSV PCR may be found in HSV encephalitis which commonly affects temporal lobes in patients with good CD4
count.
Leave question feedback
Question Navigator
HHV 8 PCR is usually associated with Kaposi's sarcoma.
Next question
Go to summary
10
11
12
13
14
15
16
17
18
19
Related Articles (BMJ)
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 39-year-old Caucasian man with symptomatic HIV disease developed multiple painless umbilicated papular
Test Analysis
lesions on his face.
What is the most likely cause of his skin lesions?
(Please select 1 option)
Cytomegalovirus (CMV)
Epstein Barr virus (EBV)
Human herpes virus (HHV) 8
Human papilloma virus (HPV 16)
Pox virus
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 39-year-old Caucasian man with symptomatic HIV disease developed multiple painless umbilicated papular
Answer Statistics
lesions on his face.
What is the most likely cause of his skin lesions?
Test Analysis
(Please select 1 option)
Cytomegalovirus (CMV)
Incorrect answer selected
Epstein Barr virus (EBV)
Human herpes virus (HHV) 8
Human papilloma virus (HPV 16)
Pox virus
This is the correct answer
Multiple painless umbilicated papular lesions are typical of molluscum contagiosum and are caused by pox
virus.
CMV does not cause painless papular lesions.
Score:
EBV causes Burkitt's lymphoma, non-Hodgkin's lymphoma and primary brain lymphomas.
Total Answered:
HHV 8 is strongly associated with Kaposi's sarcoma.
HPV 16 is associated with squamous cell carcinomas in cervix, penis, anus and oral cavity.
Feedback
Reference:
Rate this question
Ban S, Yoganathan K. Physical signs for the general dental practitioner. Case 51. Molluscum contagiosum.
Dent Update. 2008;35(1):68.
Yoganathan K, et al. Carcinoma of the penis in a HIV positive patient. Genitourin Med. 1995;71(1):41-2.
Next question
Go to summary
Leave question feedback
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Related Articles (BMJ)
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 35-year-old HIV positive African woman presented with weakness of both legs and double incontinence.
Test Analysis
CSF showed increased protein and neutrophils with normal glucose.
What is the most likely cause of her weakness?
(Please select 1 option)
CMV polyradiculomyelopathy
Guillain-Barr syndrome
Herpes virus encephalitis
HIV encephalopathy
Toxoplasma encephalitis
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 35-year-old HIV positive African woman presented with weakness of both legs and double incontinence.
Answer Statistics
CSF showed increased protein and neutrophils with normal glucose.
What is the most likely cause of her weakness?
Test Analysis
(Please select 1 option)
CMV polyradiculomyelopathy
Correct
Guillain-Barr syndrome
Herpes virus encephalitis
HIV encephalopathy
Toxoplasma encephalitis
Symptoms are suggestive of polyradiculomyelopathy (weakness of legs with involvement of sphincters).
Increased neutrophils are found in CMV polyradiculomyelopathy but not in Guillain-Barr syndrome.
HIV encephalopathy usually causes confusion and memory loss. It does not involve sphincters.
Score:
Guillain-Barr syndrome causes polyradiculopathy, explaining all her symptoms, but with normal cell counts
Total Answered:
and raised protein in the CSF.
Herpes simplex encephalitis causes fever, headache, confusion and deteriorating level of consciousness.
Feedback
Rate this question
Next question
Go to summary
Leave question feedback
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 2
Revision Advice
Tags
Learning Journal
Work Smart
A 51-year-old homosexual Caucasian HIV positive man developed multiple violaceous painless lesions on his
Test Analysis
trunk.
Which one of the following is the most likely cause of his skin lesions?
(Please select 1 option)
Cytomegalovirus (CMV)
Human herpes virus 8 (HHV8)
Human herpes virus 10 (HHV 10)
Human papilloma virus 16 (HPV 16)
Pox virus
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 51-year-old homosexual Caucasian HIV positive man developed multiple violaceous painless lesions on his
Answer Statistics
trunk.
Which one of the following is the most likely cause of his skin lesions?
Test Analysis
(Please select 1 option)
Cytomegalovirus (CMV)
Incorrect answer selected
Human herpes virus 8 (HHV8)
This is the correct answer
Human herpes virus 10 (HHV 10)
Human papilloma virus 16 (HPV 16)
Pox virus
Multiple violaceous painless lesions are typical of Kaposi's sarcoma in Caucasians. This is associated with
HHV 8.
CMV and HHV 10 do not cause multiple violaceous painless lesions.
Score:
HPV 16 is an oncogenic virus which causes squamous cell carcinomas.
Total Answered:
Pox virus causes molluscum contagiosum.
Feedback
Next question
Go to summary
Rate this question
Leave question feedback
Related Articles (BMJ)
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 32-year-old African woman with HIV presents with a two week history of greenish, frothy, itchy vaginal
Test Analysis
discharge.
What is the most likely cause of her discharge?
(Please select 1 option)
Candida albicans infection
Chlamydia infection
Foreign body
Gonorrhoea infection
Trichomonas vaginalis infection
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 32-year-old African woman with HIV presents with a two week history of greenish, frothy, itchy vaginal
Answer Statistics
discharge.
What is the most likely cause of her discharge?
Test Analysis
(Please select 1 option)
Candida albicans infection
Incorrect answer selected
Chlamydia infection
Foreign body
Gonorrhoea infection
Trichomonas vaginalis infection
This is the correct answer
Trichomonas vaginalis causes itchy, frothy, greenish vaginal discharge.
Candida albicans causes a white, curdy, itchy vaginal discharge.
Chlamydia and gonorrhoea do not cause itchy, frothy vaginal discharge and both can be asymptomatic.
Foreign body causes foul smelling vaginal discharge.
Score:
Total Answered:
Further Reading:
British Association of Sexual Health and HIV (BASHH). United Kingdom National Guideline on the Management
of Trichomonas vaginalis (2007).
Next question
Go to summary
Feedback
Rate this question
Leave question feedback
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which of the following is a sign of immunodeficiency in the mouth?
Test Analysis
(Please select 1 option)
Gingivitis
Herpes labialis
Leucoplakia
Oral hairy leucoplakia
Oral wart
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which of the following is a sign of immunodeficiency in the mouth?
Answer Statistics
(Please select 1 option)
Gingivitis
Incorrect answer selected
Test Analysis
Herpes labialis
Leucoplakia
Oral hairy leucoplakia
This is the correct answer
Oral wart
Oral hairy leucoplakia is a sign of immunodefiency. It is due to reactivation of Epstein-Barr virus infection.
Gingivitis is not a sign of immunodefiency.
Leucoplakia is not a sign of immunodefiency but it is a precancerous lesion.
Herpes labialis is due to herpes simplex infection, which causes 'cold sores' in immunocompetent patients and
chronic herpes labialis in immunocompromised patients.
Score:
Oral warts can occur in healthy people. They are due to HPV infection usually due to benign types, 6 and 11.
Total Answered:
Feedback
Next question
Go to summary
Rate this question
Related Articles (BMJ)
Leave question feedback
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following antiretrovirals is likely to cause increased pigmentation of the skin in a black African
Test Analysis
patient?
(Please select 1 option)
Didanosine
Efavirenz
Emtricitabine
Nevirapine
Stavudine
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following antiretrovirals is likely to cause increased pigmentation of the skin in a black African
Answer Statistics
patient?
(Please select 1 option)
Didanosine
Test Analysis
Incorrect answer selected
Efavirenz
Emtricitabine
This is the correct answer
Nevirapine
Stavudine
Emtricitabine causes hyperpigmentation of skin including palmar creases in 8% of black patients.
Didanosine and stavudine cause mitochondrial toxicity, hence peripheral neuropathy, pancreatitis and
hyperlactataemia.
Efavirenz causes CNS toxicity.
Score:
Nevirapine causes acute hepatitis and skin rash.
Total Answered:
Reference:
Rashbaum B. Evaluation of Hyperpigmentation in HIV-Infected Pateients Receiving Emtricitabine. 3rd IAS
Conference on HIV Pathogenesis and Treatment 2005:TuPe2.4C15
Feedback
Rate this question
Next question
Go to summary
Leave question feedback
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 34-year-old homosexual Caucasian man developed jaundice two months after taking a combination of
Test Analysis
antiretroviral drugs.
He admitted that he had had several episodes of unprotected sex with several casual male partners. His liver
function showed raised bilirubin with normal transaminases and alkaline phosphatase.
What is the most likely cause of his jaundice?
(Please select 1 option)
Acute hepatitis B
Alcoholic hepatitis
Atazanavir
Efavirenz
Nevirapine
Score:
Submit answer
Skip question
Go to summary
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 34-year-old homosexual Caucasian man developed jaundice two months after taking a combination of
Answer Statistics
antiretroviral drugs.
He admitted that he had had several episodes of unprotected sex with several casual male partners. His liver
function showed raised bilirubin with normal transaminases and alkaline phosphatase.
Test Analysis
What is the most likely cause of his jaundice?
(Please select 1 option)
Acute hepatitis B
Incorrect answer selected
Alcoholic hepatitis
Atazanavir
This is the correct answer
Efavirenz
Nevirapine
Atazanavir causes hyperbilirubinaemia with normal transaminases and alkaline phosphatase (mimicking
Gilbert's syndrome).
Score:
Acute hepatitis B is unlikely with normal trasaminases and alkaline phosphatase.
Total Answered:
A mild to moderate rise in trasaminases and alkaline phosphatase occurs in alcoholic hepatitis.
Feedback
Efavirenz can cause acute hepatitis with raised levels of transaminases.
Rate this question
Nevirapine causes acute hepatitis where transaminases are raised several-fold.
Leave question feedback
Next question
Go to summary
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 47-year-old Portuguese former intravenous drug abuser presented with a two week history of right
Test Analysis
hemiparesis.
He was found to have hepatitis B and C infection. His absolute lymphocyte count was 0.6 109/L. CT of the
head showed multiple ring-enhanced lesions.
What would be your next best course of action?
(Please select 1 option)
Manage him conservatively with physiotherapy
Refer him to a neurosurgeon for urgent brain biopsy
Refer him to a stroke specialist
Request an HIV antibody test
Start thrombolysis treatment
Score:
Submit answer
Skip question
Go to summary
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Sign Out
Help
Group Learning 3
Mock Tests
Revision Advice
Tags
Learning Journal
Work Smart
A 47-year-old Portuguese former intravenous drug abuser presented with a two week history of right
Answer Statistics
hemiparesis.
He was found to have hepatitis B and C infection. His absolute lymphocyte count was 0.6 109/L. CT of the
head showed multiple ring-enhanced lesions.
Test Analysis
What would be your next best course of action?
(Please select 1 option)
Manage him conservatively with physiotherapy
Incorrect answer selected
Refer him to a neurosurgeon for urgent brain biopsy
Refer him to a stroke specialist
Request an HIV antibody test
This is the correct answer
Start thrombolysis treatment
This man was already infected with two blood-borne viruses (hepatitis B and C). His absolute lymphocyte count
was low. CT scan showed multiple ring-enhanced lesions, which were suggestive of cerebral toxoplasmosis.
Score:
Therefore, testing HIV is the next best course of action. Finding multiple ring-enhanced lesions on CT scan
needs further investigations.
Total Answered:
Managing conservatively with physiotherapy is not an appropriate course of action.
Feedback
CT scan is not typical of brain tumour, hence referring him for urgent brain biopsy is not the best course of
action.
Rate this question
Thrombolysis treatment should not be started, as the CT scan was not typical of ischaemic stroke.
Leave question feedback
Reference:
Question Navigator
Yoganathan K. A 'brain tumor' in an intravenous drug abuser. Int J Gen Med. 2009;2:73-5.
Next question
Go to summary
10
11
12
13
14
15
16
17
18
19
Related Articles (BMJ)
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 34-year-old Thai lady presented with a left hemiparesis of two weeks duration.
Test Analysis
HIV antibody test was positive. CT scan of the head showed multiple ring-enhanced lesions.
What is the most likely cause of her weakness?
(Please select 1 option)
Amoebic brain abscesses
Cerebral toxoplasmosis
Herpes simplex encephalitis
Primary brain lymphoma
Progressive multifocal leucoencephalopathy
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 34-year-old Thai lady presented with a left hemiparesis of two weeks duration.
Answer Statistics
HIV antibody test was positive. CT scan of the head showed multiple ring-enhanced lesions.
What is the most likely cause of her weakness?
Test Analysis
(Please select 1 option)
Amoebic brain abscesses
Cerebral toxoplasmosis
Incorrect answer selected
This is the correct answer
Herpes simplex encephalitis
Primary brain lymphoma
Progressive multifocal leucoencephalopathy
Cerebral toxoplasmosis is the most likely diagnosis. Multiple ring-enhanced lesions are commonly seen in
patients with cerebral toxoplasmosis, though solitary ring enhanced lesions are seen in 25% of patients on CT
scan. MRI scan is more sensitive in identifying small lesions than CT scan.
Score:
Amoebic brain abscesses are not the most likely cause in this patient.
Total Answered:
Multiple ring-enhanced lesions are not seen in patients with herpes simplex encephalitis.
Primary brain lymphoma causes a significant mass effect with surrounding oedema.
Feedback
Progressive multifocal leucoencephalopathy causes multifocal white matter lesions without any mass effect or
surrounding oedema.
Rate this question
Reference:
Leave question feedback
Yoganathan K. A 'brain tumor' in an intravenous drug abuser. Int J Gen Med. 2009;2:73-5.
Next question
Related Articles (BMJ)
Question Navigator
Go to summary
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following is an oncogenic virus?
Test Analysis
(Please select 1 option)
Hepatitis A
Human papilloma virus 6 (HPV 6)
Human papilloma virus 11 (HPV 11)
Human papilloma virus 16 (HPV 16)
Varicella zoster virus (VZV)
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following is an oncogenic virus?
Answer Statistics
(Please select 1 option)
Hepatitis A
Incorrect answer selected
Test Analysis
Human papilloma virus 6 (HPV 6)
Human papilloma virus 11 (HPV 11)
Human papilloma virus 16 (HPV 16)
This is the correct answer
Varicella zoster virus (VZV)
HPV 16 is oncogenic and causes squamous cell carcinomas in the oral cavity, cervix, anus and penis.
Hepatitis A is not an oncogenic virus, as it does not cause chronic infection or cancer.
HPV 6 and 11 typically cause the majority of benign warts.
VZV causes chicken pox and herpes zoster.
Score:
References:
1. British Association for Sexual Health and HIV (BASHH). United Kingdom National Guideline on the
Management of Anogenital Warts, 2007.
2. Yoganathan K, et al. Carcinoma of the penis in a HIV positive patient. Genitourin Med. 1995;71(1):41-2.
Total Answered:
Feedback
Rate this question
Next question
Go to summary
Leave question feedback
Related Articles (BMJ)
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 28-year-old man with HIV presents with a five day history of feeling unwell. He is a heavy smoker.
Test Analysis
A chest radiograph showed right upper lobe consolidation. His CD4 count was 468 cells/mm 3. HIV RNA level
was 90,678 copies/ml. He is not on any antiretroviral treatment.
What is the most likely diagnosis?
(Please select 1 option)
Bronchial carcinoma
Invasive pulmonary aspergillosis
Pulmonary tuberculosis
Pneumocystis jiroveci pneumonia (PCP)
Streptococcal pneumonia
Score:
Submit answer
Skip question
Go to summary
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Community
Work Hard
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 28-year-old man with HIV presents with a five day history of feeling unwell. He is a heavy smoker.
Answer Statistics
A chest radiograph showed right upper lobe consolidation. His CD4 count was 468 cells/mm 3. HIV RNA level
was 90,678 copies/ml. He is not on any antiretroviral treatment.
Test Analysis
What is the most likely diagnosis?
(Please select 1 option)
Bronchial carcinoma
Incorrect answer selected
Invasive pulmonary aspergillosis
Pulmonary tuberculosis
Pneumocystis jiroveci pneumonia (PCP)
Streptococcal pneumonia
This is the correct answer
This is typical of community-acquired pneumonia. One should think of common infections rather than any
opportunistic infections in HIV patients with good CD4 counts. (More than 400 cells/mm 3 is not
immunocompromised.)
Score:
It is not a typical history for bronchial carcinoma as the history was short and radiographic changes were not
typical of bronchial carcinoma.
Total Answered:
Invasive pulmonary aspergillosis is unlikely in a patient with good CD4 count. Pulmonary tuberculosis typically
Feedback
causes cavitating lesions in a patient with a good CD4 count.
Rate this question
PCP commonly occurs in patients with CD4 count of less than 200 cells/mm 3 and chest radiograph shows
bilateral infiltrates from the hila without any effusion or lymphadenopathy.
Leave question feedback
The history is too short for tuberculosis, and apart from HIV there aren't any other risk factors for this.
Question Navigator
Next question
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
Go to summary
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 31-year-old African man presented with a history of fever, night sweats, shortness of breath and weight loss
Test Analysis
for two months.
His chest radiograph showed a moderately severe left pleural effusion only. He consented to an HIV test which
was positive.
What is the most likely cause of pleural effusion?
(Please select 1 option)
Hodgkin's lymphoma
Pleural tuberculosis
Pneumocystis jirovecii pneumonia (PCP)
Pulmonary aspergillosis
Pulmonary Kaposi's sarcoma
Score:
Submit answer
Skip question
Go to summary
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 31-year-old African man presented with a history of fever, night sweats, shortness of breath and weight loss
Answer Statistics
for two months.
His chest radiograph showed a moderately severe left pleural effusion only. He consented to an HIV test which
was positive.
Test Analysis
What is the most likely cause of pleural effusion?
(Please select 1 option)
Hodgkin's lymphoma
Pleural tuberculosis
Incorrect answer selected
This is the correct answer
Pneumocystis jirovecii pneumonia (PCP)
Pulmonary aspergillosis
Pulmonary Kaposi's sarcoma
Pleural tuberculosis is the most likely cause in an HIV positive African man with a two month history of weight
loss. His pleural effusion is due to pleural tuberculosis (extra pulmonary tuberculosis).
Hodgkin's lymphoma can cause pleural effusion due to pleural involvement but it is often associated with
mediastinal mass. His chest radiographshowed only pleural effusion. Non-Hodgkin's lymphoma (not Hodgkin's
lymphoma) is commonly associated with these patients.
PCP does not cause pleural effusion. It typically causes bilateral reticular shadows from the hila without any
hilar lymph node enlargement or pleural effusion.
Pulmonary aspergillosis shows infiltrative lesions but it does not typically cause pleural effusion.
Score:
Total Answered:
Feedback
Rate this question
Leave question feedback
Pulmonary Kaposi's sarcoma can cause pleural effusion by involving the pleura, but it often causes coarse
irregular nodular lesions in the lungs.
Reference:
el-Gadi SM, et al. Kaposi sarcoma presenting as severe haemoptysis. Genitourin Med. 1997;73(6):575-6.
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Next question
Go to summary
Revision Notes
Related Articles (BMJ)
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following is an AIDS defining illness?
Test Analysis
(Please select 1 option)
Anal canal warts
Extra genital molluscum contagiosum
Multidermatomal shingles
Oesophageal candidiasis
Oral candidiasis
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following is an AIDS defining illness?
Answer Statistics
(Please select 1 option)
Anal canal warts
Incorrect answer selected
Test Analysis
Extra genital molluscum contagiosum
Multidermatomal shingles
Oesophageal candidiasis
This is the correct answer
Oral candidiasis
Any opportunistic infections or opportunistic malignancies are AIDS defining illnesses.
Oesophageal candidiasis is an AIDS defining illness but oral candidiasis is not.
Anal warts are not an opportunistic infection.
Extra genital molluscum contagiosum is also not an opportunistic infection but frequently occurs in symptomatic
HIV positive patients.
Score:
Multidermatomal shingles is not an opportunistic infection but if it occurs in a young person HIV infection needs
to be excluded.
Total Answered:
Feedback
Next question
Go to summary
Rate this question
Leave question feedback
Related Articles (BMJ)
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following cutaneous lesions is associated with HIV infection?
Test Analysis
(Please select 1 option)
Leucoplakia
Lichen planus
Lichen sclerosus
Plasma cell balanitis
Psoriasis
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following cutaneous lesions is associated with HIV infection?
Answer Statistics
(Please select 1 option)
Leucoplakia
Incorrect answer selected
Test Analysis
Lichen planus
Lichen sclerosus
Plasma cell balanitis
Psoriasis
This is the correct answer
It occurs in 2-4% of healthy people. If pre-existing psoriasis flares up for no apparent reason or middle-aged
people develop psoriasis for the first time, one should exclude underlying HIV infection in those patients.
Leucoplakia is a pre-cancerous lesion whereas oral hairy leucoplakia is a sign of immunodefiency in an HIV
positive patient.
Lichen planus, lichen sclerosus and plasma cell balanitis are not associated with HIV infection.
Score:
Total Answered:
Next question
Go to summary
Feedback
Related Articles (BMJ)
Rate this question
Leave question feedback
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 36-year-old Caucasian woman was successfully treated for Pneumocystis jirovecii pneumonia (PCP).
Test Analysis
She was re-admitted with acute breathlessness with left-sided chest pain ten days after her discharge from the
hospital. Examination revealed that she was hypoxic and found to have diminished breath sounds on the left
side of chest.
What is the most likely cause of her recent admission?
(Please select 1 option)
Acute myocardial infarction
Acute pericarditis
Acute pulmonary embolism
Left lobar pneumonia
Pneumothorax
Score:
Submit answer
Skip question
Go to summary
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
A 36-year-old Caucasian woman was successfully treated for Pneumocystis jirovecii pneumonia (PCP).
She was re-admitted with acute breathlessness with left-sided chest pain ten days after her discharge from the
hospital. Examination revealed that she was hypoxic and found to have diminished breath sounds on the left
side of chest.
Answer Statistics
Test Analysis
What is the most likely cause of her recent admission?
(Please select 1 option)
Acute myocardial infarction
Incorrect answer selected
Acute pericarditis
Acute pulmonary embolism
Left lobar pneumonia
Pneumothorax
This is the correct answer
Pneumothorax is a well-known complication of PCP. An acute history of chest pain with breathlessness and
diminished breath sounds is typical of pneumothorax.
Score:
Diminished breath sounds are not a feature of acute myocardial infarction or acute pericarditis.
Total Answered:
Acute pulmonary embolism should be considered due to her recent admission but diminished breath sounds
are not a feature.
Feedback
There are no signs of consolidation to consider lobar pneumonia.
Rate this question
Leave question feedback
Next question
Go to summary
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following drugs is associated with hypersensitivity reactions?
Test Analysis
(Please select 1 option)
Atazanavir
Lamivudine
Nevirapine
Tenofovir
Zidovudine
Submit answer
Skip question
Go to summary
Score:
Total Answered:
Question Navigator
1
10
11
12
13
14
15
16
17
18
19
Tags
Tag
Tag
Hide Question
2014 BMJ Publishing Group Ltd . All rights reserved.
Contact . Corporate . Terms and conditions & Privacy policy
My Profile
Exam Revision
Work Smart
Scores
Work Hard
Community
Mock Tests
Sign Out
Help
Group Learning 3
Revision Advice
Tags
Learning Journal
Work Smart
Which one of the following drugs is associated with hypersensitivity reactions?
Answer Statistics
(Please select 1 option)
Atazanavir
Incorrect answer selected
Test Analysis
Lamivudine
Nevirapine
This is the correct answer
Tenofovir
Zidovudine
Nevirapine can cause acute hepatitis and skin rash as a part of hypersensitive reaction especially when the
CD4 count is over 250 cells/ml in women and over 400 cells/ml in men. Nevirapine should not be prescribed in
those conditions.
Atazanavir causes hyperbilirubinaemia and rarely renal stones.
Lamivudine does not cause hypersensitivity reaction.
Score:
Tenofovir causes proximal tubular damage.
Total Answered:
Zidovudine causes bone marrow suppression.
Reference:
Feedback
Danino S, et al. Urolithiasis in an HIV infected patient - a link with atazanavir? HIV Med 2007;8(Suppl 1):45.
Rate this question
Leave question feedback
Go to summary
Question Navigator
Related Articles (BMJ)
10
11
12
13
14
15
16
17
18
19
Revision Notes
Any revision notes recorded
here will be automatically
added to a list, and can be
viewed in full on the summary
page.
You might also like
- Hypoxemic Respiratory FailureDocument70 pagesHypoxemic Respiratory FailureMohamed Rikarz Ahamed RikarzNo ratings yet
- Medical exam questions on diseases, conditions and clinical findingsDocument11 pagesMedical exam questions on diseases, conditions and clinical findingsMohamed Rikarz Ahamed RikarzNo ratings yet
- Den 4Document4 pagesDen 4Daniela Montalbán FiestasNo ratings yet
- A Study of Dengue Fever in Pregnancy and Its Maternal and Fetal PrognosisDocument4 pagesA Study of Dengue Fever in Pregnancy and Its Maternal and Fetal PrognosissharenNo ratings yet
- 12 Kasper Notes 2020 OphthalmologyDocument33 pages12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzNo ratings yet
- Symptomatic Dengue Infection During Pregnancy PDFDocument8 pagesSymptomatic Dengue Infection During Pregnancy PDFImanuel Far-FarNo ratings yet
- Maternal and Perinatal Outcomes of Dengue in Portsudan, Eastern SudanDocument4 pagesMaternal and Perinatal Outcomes of Dengue in Portsudan, Eastern SudanMohamed Rikarz Ahamed RikarzNo ratings yet
- Medical exam questions on diseases, conditions and clinical findingsDocument11 pagesMedical exam questions on diseases, conditions and clinical findingsMohamed Rikarz Ahamed RikarzNo ratings yet
- 12 Kasper Notes 2020 OphthalmologyDocument33 pages12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue 208Document3 pagesDengue 208Mohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue 201Document6 pagesDengue 201Mohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue 208Document3 pagesDengue 208Mohamed Rikarz Ahamed RikarzNo ratings yet
- Suspect DHF With Warning SignsDocument2 pagesSuspect DHF With Warning SignsMohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue Infections During PregnancyDocument7 pagesDengue Infections During PregnancyImanuel Far-FarNo ratings yet
- All in One Golden CPSP QuestionsDocument570 pagesAll in One Golden CPSP QuestionsQuranSunnat100% (2)
- Cir 27Document3 pagesCir 27Mohamed Rikarz Ahamed RikarzNo ratings yet
- Rheumatology Notes For ReadingDocument8 pagesRheumatology Notes For ReadingMohamed Rikarz Ahamed RikarzNo ratings yet
- Hemodynamic Changes in Hypotensive Shock: Lcs LumDocument2 pagesHemodynamic Changes in Hypotensive Shock: Lcs LumMohamed Rikarz Ahamed RikarzNo ratings yet
- May 2017 Mrcp1Document9 pagesMay 2017 Mrcp1Mohamed Rikarz Ahamed RikarzNo ratings yet
- Microbiology SBA For MRCOG Part 1Document42 pagesMicrobiology SBA For MRCOG Part 1Mohamed Rikarz Ahamed Rikarz100% (1)
- Results of The Selection Examination in Surgery - .January/February, 2017Document1 pageResults of The Selection Examination in Surgery - .January/February, 2017Mohamed Rikarz Ahamed RikarzNo ratings yet
- Basic SciencesDocument117 pagesBasic SciencesMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of Colombo: 2017/SEIMDIFM - 003Document1 pagePostgraduate Institute of Medicine University of Colombo: 2017/SEIMDIFM - 003Mohamed Rikarz Ahamed RikarzNo ratings yet
- Ancient EgyptDocument18 pagesAncient EgyptMohamed Rikarz Ahamed RikarzNo ratings yet
- PGIM Ophthalmology Selection Results 2017Document1 pagePGIM Ophthalmology Selection Results 2017Mohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Nstitute of Med C E University of Colombo: LT S T III A Il, 2016Document1 pagePostgraduate Nstitute of Med C E University of Colombo: LT S T III A Il, 2016Mohamed Rikarz Ahamed RikarzNo ratings yet
- 643 PDFDocument1 page643 PDFMohamed Rikarz Ahamed RikarzNo ratings yet
- 642Document1 page642Mohamed Rikarz Ahamed RikarzNo ratings yet
- Answers To Questions For Volume 11, Number 4: The Surgical Approach To Postpartum HaemorrhageDocument6 pagesAnswers To Questions For Volume 11, Number 4: The Surgical Approach To Postpartum HaemorrhageMohamed Rikarz Ahamed RikarzNo ratings yet
- Physiological Changes in Pregnancy: Candice K Silversides, Jack M ColmanDocument12 pagesPhysiological Changes in Pregnancy: Candice K Silversides, Jack M ColmanrinimeimeiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- RSIA Rizki Bunda Slow Moving Drug ListDocument4 pagesRSIA Rizki Bunda Slow Moving Drug Listzolla verbiantiNo ratings yet
- Price Master ListDocument38 pagesPrice Master ListSolideo Gloria50% (2)
- Preventive MedicineDocument17 pagesPreventive MedicinersimranjitNo ratings yet
- Homeopathy For Memory and ConcentrationDocument5 pagesHomeopathy For Memory and Concentrationshashi_gadadNo ratings yet
- Jurnal MeiristaDocument8 pagesJurnal Meiristameirista deviNo ratings yet
- Special Neonatal ConditionsDocument37 pagesSpecial Neonatal ConditionsSanthosh.S.UNo ratings yet
- TBCP GuideDocument20 pagesTBCP GuideJustin CreekNo ratings yet
- Pelvic TB: Genital Tract InfectionDocument11 pagesPelvic TB: Genital Tract InfectionAmalia Zulfa AmandaNo ratings yet
- 1Document3 pages1EslamAlmassriNo ratings yet
- Drug inventory and sales reportDocument6 pagesDrug inventory and sales reportifrs inanta1No ratings yet
- AzithromycinDocument1 pageAzithromycinjennelyn losantaNo ratings yet
- Inggris IndonesiaDocument26 pagesInggris IndonesialaudyaFebNo ratings yet
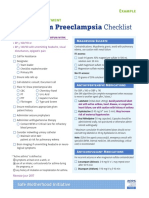
- Postpartum Preeclampsia Checklist: Emergency Department ExampleDocument1 pagePostpartum Preeclampsia Checklist: Emergency Department ExamplewijeNo ratings yet
- 100Document15 pages100Samar FakhryNo ratings yet
- GENERICSKING TRADING INC PRICE LISTDocument10 pagesGENERICSKING TRADING INC PRICE LISTCrystal NgNo ratings yet
- CroupDocument20 pagesCroupFariezuan HamidNo ratings yet
- IMCI NewDocument81 pagesIMCI NewBianca de GuzmanNo ratings yet
- Acute Respiratory InfectionsDocument18 pagesAcute Respiratory InfectionsEmilyRose17No ratings yet
- Subiecte Morfopatologie MacroDocument3 pagesSubiecte Morfopatologie MacroRebeca PetreaNo ratings yet
- AnalgesicsDocument4 pagesAnalgesicsshairaorquetaNo ratings yet
- I II III IV V: Description Examples ScheduleDocument1 pageI II III IV V: Description Examples ScheduleAndre PrayogoNo ratings yet
- Clinical Reasoning, Assessment, and RecordingDocument19 pagesClinical Reasoning, Assessment, and RecordingChristyl JoNo ratings yet
- List of Basic Essential Medicines Ministry of Health Seychelles 2010Document14 pagesList of Basic Essential Medicines Ministry of Health Seychelles 2010portosinNo ratings yet
- Certificate of VaccinationDocument5 pagesCertificate of VaccinationDiana LicupaNo ratings yet
- Metformin in PCOSDocument5 pagesMetformin in PCOSbalaramNo ratings yet
- TOACSDocument18 pagesTOACSarjumandNo ratings yet
- 100QforCIP 30QforDiagnosticReviewDocument29 pages100QforCIP 30QforDiagnosticReviewpamgelNo ratings yet
- Notes on Medicine SubdivisionsDocument35 pagesNotes on Medicine SubdivisionsTush Rame100% (1)
- Kunjungan Bpjs 2019Document92 pagesKunjungan Bpjs 2019Puskesmas RambipujiNo ratings yet
- Azithromycin WarningsDocument4 pagesAzithromycin WarningsChristian Angelo LeonorNo ratings yet