Professional Documents
Culture Documents
Postobstructive Pulmonary Edema After Biopsy of A Nasopharyngeal Mass.
Uploaded by
viannikkkyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postobstructive Pulmonary Edema After Biopsy of A Nasopharyngeal Mass.
Uploaded by
viannikkkyCopyright:
Available Formats
Respiratory Medicine Case Reports 16 (2015) 166e168
Contents lists available at ScienceDirect
Respiratory Medicine Case Reports
journal homepage: www.elsevier.com/locate/rmcr
Case report
Postobstructive pulmonary edema after biopsy of a nasopharyngeal
mass
Keyur Kamlesh Mehta a, Sabina Qureshi Ahmad a, *, Vikas Shah b, Haesoon Lee a
a
b
SUNY Downstate Medical Center, 450 Clarkson Avenue, Box 49, Brooklyn, NY 11203, United States
SUNY Downstate, Pediatric Intensivist Kings County Hospital Center, 451 Clarkson Avenue, Brooklyn, NY 11203, United States
a r t i c l e i n f o
a b s t r a c t
Article history:
Received 19 October 2015
Accepted 26 October 2015
We describe a case of 17 year-old male with a nasopharyngeal rhabdomyosarcoma who developed
postobstructive pulmonary edema (POPE) after removing the endotracheal tube following biopsy. He
developed mufed voice, rhinorrhea, dysphagia, odynophagia, and difculty breathing through nose and
weight loss of 20 pounds in the preceding 2 months. A nasopharyngoscopy revealed a eshy nasopharyngeal mass compressing the soft and hard palate. Head and neck MRI revealed a large mass in the
nasopharynx extending into the bilateral choana and oropharynx. Biopsy of the mass was taken under
general anesthesia with endotracheal intubation. Immediately after extubation he developed oxygen
desaturation, which did not improve with bag mask ventilation with 100% of oxygen, but improved after
a dose of succinylcholine. He was re-intubated and pink, frothy uid was suctioned from the endotracheal tube. Chest radiograph (CXR) was suggestive of an acute pulmonary edema. He improved with
mechanical ventilation and intravenous furosemide. His pulmonary edema resolved over the next 24 h.
POPE is a rare but serious complication associated with upper airway obstruction. The pathophysiology
of POPE involves hemodynamic changes occurring in the lung and the heart during forceful inspiration
against a closed airway due to an acute or chronic airway obstruction. This case illustrates the importance of considering the development of POPE with general anesthesia, laryngospasm and removal of
endotracheal tube to make prompt diagnosis and to initiate appropriate management.
2015 The Authors. Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND
license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Keywords:
POPE (postobstructive pulmonary edema)
Pulmonary edema
Nasopharyngeal tumor
Rhabdomyosarcoma
1. Introduction
Postobstructive pulmonary edema (POPE) is a rare but serious
complication associated with upper airway obstruction. The pathophysiology of POPE involves hemodynamic changes occurring in
the lung and the heart during forceful inspiration against a closed
airway due to an acute or chronic airway obstruction. We describe a
case of 17 year-old male with a large nasopharyngeal mass who
developed POPE after biopsy of the mass. This case illustrates the
importance of considering the development of POPE with general
Abbreviations: MRI, magnetic resonance imaging; CXR, chest radiograph; FiO2,
fraction of inspired oxygen; POPE, postobstructive pulmonary edema; NPPE,
negative pressure pulmonary edema; LV, left ventricle; RV, right ventricle; ARDS,
acute respiratory distress syndrome; PEEP, positive end expiratory pressure; CPAP,
Continuous positive airway pressure.
* Corresponding author.
E-mail addresses: keyur.mehta87@gmail.com (K.K. Mehta), sabinaqahmad@
yahoo.com (S.Q. Ahmad), Vikas.Shah@nychhc.org (V. Shah), Haesoon.lee@
downstate.edu (H. Lee).
anesthesia, laryngospasm, and removal of endotracheal tube to
make prompt diagnosis and to initiate appropriate management.
2. Case presentation
A 17 year-old African American male with no signicant past
medical history presented to a physician's ofce for an inuenza
vaccination. He reported progressively worsening mufed voice,
rhinorrhea, dysphagia, odynophagia, inability to breathe through
nose and unintentional weight loss of 20 pounds in the preceding 2
months. Physical examination was signicant for rhinorrhea and a
mass in the mouth nearly lling the oral cavity. He was immediately
sent to the otolaryngology clinic for further evaluation. A nasopharyngoscopy demonstrated a eshy nasopharyngeal mass compressing the soft and hard palate displacing them antero-inferiorly
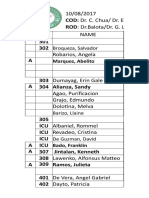
Fig. 1. Further workup included head and neck MRI, which
demonstrated a large mass in the nasopharynx extending into the
bilateral choana and oropharynx Fig. 2. A week later, the patient
was taken to the operating room for biopsy of the mass under
general anesthesia with endotracheal intubation. Immediately after
http://dx.doi.org/10.1016/j.rmcr.2015.10.007
2213-0071/ 2015 The Authors. Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
K.K. Mehta et al. / Respiratory Medicine Case Reports 16 (2015) 166e168
Fig. 1. Arrows show a nasopharyngeal mass displacing the soft and hard palate anteroinferiorly. A mucosal ulcer is seen over the mass.
extubation, he developed oxygen desaturation. His oxygenation did
not improve with bag mask ventilation with 100% of oxygen, but
improved only after a dose of succinylcholine. He was re-intubated
and pink frothy uid was suctioned from the endotracheal tube.
Chest radiograph (CXR) was suggestive of an acute pulmonary
edema Fig. 3. He received 40 mg of furosemide intravenously,
which was repeated twice in the pediatric intensive care unit
(PICU). Serial CXR revealed gradual resolution of pulmonary edema
over the next 24 h. On hospital day #2, he was extubated, placed on
bilevel positive airway pressure (BiPAP) ventilation with the pressure setting of 14/6 cm H2O, inspired oxygen (FiO2) of 40% for 12 h.
Overnight he was weaned to face mask with 30% oxygen, then
weaned to room air the next morning.
3. Discussion
The rst description of postobstructive pulmonary edema
Fig. 2. MRI reconstruction - Arrow shows a nasopharyngeal mass extending from
posterior aspect of nasopharynx to the hypopharynx, signicantly narrowing the
oropharyngeal airway at the tongue base.
167
Fig. 3. Diffuse bilateral air space opacities greater in the upper lung elds suggestive of
pulmonary edema.
(POPE) was on an animal model in 1927, and the rst human cases
were reported in 1973 [1,2]. POPE is considered rare, and most reported cases occurred after the administration of anesthesia. POPE
is thought to occur from hemodynamic changes secondary to
forced inspiration against a closed airway induced by an acute or
chronic airway obstruction. POPE is also called negative pressure
pulmonary edema (NPPE) and its prevalence has been estimated to
be less than 0.1% of cases of administration of general anesthesia
[3]. It usually occurs in young, healthy male patients [4,5].
Numerous clinical conditions with upper airway obstruction have
been associated with POPE, such as laryngospasm, foreign-body
aspiration, endotracheal intubation, upper airway tumor, and
obstructive sleep apnea.
POPE has been categorized into two types. Type I POPE occurs
after forceful inspiration against an acute upper airway obstruction,
while Type II POPE occurs after relief of chronic airway obstruction.
The pathophysiology of Type I POPE involves the hemodynamic
changes occurring in the lung and the left ventricle (LV) during
forceful inspiration against the obstruction. During normal inspiration, pleural and alveolar pressure become more negative than
the atmosphere, effecting air ows from the ambient pressure atmosphere to the low pressure alveoli. The decrease in pleural
pressure increases venous return from peripheral veins to the
intrathoracic vena cava and right atrium.
With an acute upper airway obstruction, the patient takes
forceful inspiration against the obstruction, known as Muller's
maneuver [6]. The intrapleural pressure decreases markedly and
venous return increases due to the increased pressure gradient
from the peripheral veins to the central veins leading to increased
right ventricular (RV) output, pulmonary blood ow and RV pressure. Buda AJ et al. examined the hemodynamic events of Muller
maneuver and found pleural pressure surrounding the LV, peripheral arterial pressure and LV ejection fraction were decreased,
despite an increased LV volume. They concluded that the negative
intrathoracic pressure affected LV function by increasing LV transmural pressure and afterload [7]. The impaired LV function also
increased the pulmonary capillary back pressure. When the
transcapillary pressure, the pressure gradient between the pulmonary capillary to the interstitium increases above 18 cm H2O,
capillary transudation occurs. Once the microvascular ltrate in the
peri-microvascular compartment exceeds a certain limit, it inundates the adjacent alveoli causing alveolar edema [8]. Pulmonary
vascular congestion, chronic hypoxia and hypercapnea cause systemic uid retention further favoring pulmonary capillary uid
168
K.K. Mehta et al. / Respiratory Medicine Case Reports 16 (2015) 166e168
transudation and development of pulmonary edema [9,10]. Pathogenesis of POPE can represent either a form of hydrostatic edema
as in congestive heart failure or an increased permeability edema as
in acute respiratory distress syndrome (ARDS). Limited studies of
protein composition of the edema uid indicate that it is a hydrostatic edema. Alveolar exudate protein was less than 65% of the
serum protein, which is a cutoff point between hydrostatic versus
permeability edema [11,12]. When the factors favoring uid
movement from the capillary to the interstitium is reversed, pulmonary edema rapidly resolves. Rapid resolution of edema in POPE
suggests an intact alveolar capillary membrane, unlike that in
ARDS, in which edema resolution is delayed.
Our patient had partial obstruction of the nasopharynx and oral
airway due to a tumor, which turned out to be rhabdomyosarcoma
on pathology. His baseline serum bicarbonate was 31mEq suggesting metabolic compensation for chronic hypercapnea secondary to an upper airway obstruction. After extubation, maintenance
of airway patency was probably compromised from the residual
effect of anesthesia, leading to airway occlusion. However,
obstruction from laryngospasm after extubation is also a possibility.
In chronic airway obstruction it is believed that there is a moderate
level of auto PEEP (positive end expiratory pressure) produced by
the obstructing lesion which increases end expiratory lung volume.
With removal of the obstruction there is a sudden removal of PEEP
which leads to interstitial uid transudation and pulmonary edema
[13,14].
Diagnosis of POPE requires a high index of suspicion. Persistent
tachypnea, oxygen desaturation, pink frothy bronchial secretions,
bradycardia, and rales on auscultation indicate likely pulmonary
edema. The diagnosis is established by CXR. A chest computed tomography (CT) is not necessary for the diagnosis of POPE.
POPE usually resolves within 12e24 h if prompt diagnosis and
proper management are initiated. Most cases have been treated
with PEEP and diuretics; however the role of diuretic is not clear
[15]. Continuous positive airway pressure (CPAP) or bilevel positive
airway pressure (BiPAP) is an alternative to intubation. Recent data
suggest that noninvasive respiratory support such as BiPAP may be
an important tool to prevent or treat acute respiratory failure while
avoiding intubation. The aims of noninvasive respiratory support in
the management of POPE include reducing the work of breathing,
increasing alveolar recruitment with better oxygenation, and
reducing left ventricular after load, increasing cardiac output and
improving hemodynamics [16].
POPE resolves by itself once the airway obstruction is removed.
Passage of time brings about resolution of edema, not from diuretics or corticosteroids. Early relief of upper airway obstruction
should decrease the incidence of POPE. Preventative measures have
been suggested, such as the use of intra-operative muscle relaxants,
topical or spray lidocaine, corticosteroids, and early or delayed
extubation to reduce the risk of laryngospasm. Other preventive
measures that have also been suggested are to clear the airway of
the retained blood or secretions by suctioning the oropharynx and
extubating the patient in either a very deep or very light level of
anesthesia, when the risk of laryngospasm is less. Prophylactic
CPAP may be the most effective preventive measure for the patients
at-risk [17,18].
Acknowledgments
There are no sponsors for this case report and there is no potential conict of interest, real or perceived; this includes a
description of the role of the study sponsor(s), if any, in: (1) study
design; (2) the collection, analysis, and interpretation of data; (3)
the writing of the report; and (4) the decision to submit the paper
for publication.
The rst author is Keyur K. Mehta and the corresponding author
is Sabina Q. Ahmad, and no honorarium, grant, or other form of
payment was given to anyone to produce the manuscript.
References
[1] R.L. Moore, C.A.L. Binger, The response to respiratory resistance: a comparison
of the effects produced by partial obstruction in the inspiratory and expiratory
phases of respiration, J. Exp. Med. 45 (1927) 1065e1080.
[2] C.E. Oswalt, G.A. Gates, F.M.G. Holmstrom, Pulmonary edema as a complication of acute airway obstruction, JAMA 238 (1977) 1833e1835.
[3] K. Deepika, C.A. Kenaan, A.M. Barrocas, J.J. Fonseca, G.B. Bikazi, Negative
pressure pulmonary edema after acute upper airway obstruction, J. Clin.
Anesth. 9 (1997) 403e408.
[4] A.F. Anderson, D. Alfrey, A.B. Lipscomb Jr., Acute pulmonary edema, an unusual complication following arthroscopy: a report of three cases, Arthroscopy
6 (1990) 235e237.
[5] J.R. Holmes, R.N. Hensinger, E.W. Wojtys, Postoperative pulmonary edema in
young, athletic adults, Am. J. Sports Med. 19 (1991) 365e371.
[6] C.D. Cook, J. Mead, Maximum and minimum airway pressures at various lung
volumes in normal children and adults, Fed. Proc. 19 (1960) 377.
[7] A.J. Buda, M.R. Pinsky, N.B. Ingels Jr., et al., Effect of intrathoracic pressure on
left ventricular performance, N. Engl. J. Med. 301 (1979) 453e459.
[8] T.A. Zumsteg, A.M. Havill, M.H. Gee, Relationships among lung extravascular
uid compartments with alveolar ooding, J. Appl. Physiol. Respir. Environ.
Exerc. Physiol. 53 (1982) 267e271.
[9] S.A. Lang, P.G. Duncan, D.A.E. Shepard, et al., Pulmonary edema associated
with airway obstruction, Can. J. Anesth. 37 (1990) 210e218.
[10] M.H. Kollef, J. Pluss, Noncardiogenic pulmonary edema following upper
airway obstruction, Medicine 70 (1991) 91e98.
[11] R.D. Freemont, R.H. Kallet, M.A. Matthay, L.B. Ware, Postobstructive pulmonary edema. A case for hydrostatic mechanisms, Chest 131 (2007)
1742e1746.
[12] A. Feins, R.F. Grossman, J.G. Jones, et al., The value of edema uid protein
measurement in patients with pulmonary edema, Am. J. Med. 67 (1979)
32e38.
[13] S.A. Lang, P.G. Duncan, D.A. Shephard, et al., Pulmonary oedema associated
with airway obstruction, Can. J. Anaesth. 37 (2) (1990) 210e218.
[14] T.N. Gufn, G. Harel, A. Sanders, F.E. Lucente, M. Nash, Acute postobstructive
pulmonary edema, Otolaryngol. Head. Neck Surg. 112 (1995) 235e237.
[15] M.S. Koh, A.A. Hsu, P. Eng, Negative pressure pulmonary oedema in the
medical intensive care unit, Intensive Care Med. 29 (2003) 1601e1604.
[16] S. Jaber, G. Chanques, B. Jung, Postoperative noninvasive ventilation, Anesthesiology 112 (2010) 453e461.
[17] S.M. Bagshaw, A. Delaney, C. Farrell, J. Drummond, P.G. Brindley, Best evidence
in critical care medicine. Steroids to prevent post-extubation airway
obstruction in adult critically ill patients, Can. J. Anaesth. 55 (2008) 382e385.
[18] A.G. Galvis, J.E. Stool, C.D. Bluestone, Pulmonary edema following relief of
upper airway obstruction, Ann. Otol. Rhinol. Laryngol. 89 (1980) 124e128.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Acute and Chronic SinusitisDocument38 pagesAcute and Chronic SinusitisBellaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Gomes Wses 15Document6 pagesGomes Wses 15Rara Aulia IINo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- VTE0113Document91 pagesVTE0113Karen PinemNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Gomes Wses 15Document6 pagesGomes Wses 15Rara Aulia IINo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- TreatmentDocument9 pagesTreatmentviannikkkyNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Fibroadenoma PDFDocument2 pagesFibroadenoma PDFAthika Dwi Sofiana100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Raw Milk For The HealthDocument7 pagesRaw Milk For The HealthviannikkkyNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- VTE0113Document91 pagesVTE0113Karen PinemNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Typhoid Fever and It Association With Environmental Factors in The Dhaka Metropolitan Area of Bangladesh A Spatial and Time-Series ApproachDocument14 pagesTyphoid Fever and It Association With Environmental Factors in The Dhaka Metropolitan Area of Bangladesh A Spatial and Time-Series ApproachviannikkkyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- A Novel Paradigm For Heart Failure With Preserved Ejection FractionDocument9 pagesA Novel Paradigm For Heart Failure With Preserved Ejection FractionviannikkkyNo ratings yet
- Patof HfpefDocument13 pagesPatof HfpefviannikkkyNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Topical Tranexamic Acid Versus Autotransfusion After Total KneeDocument4 pagesTopical Tranexamic Acid Versus Autotransfusion After Total KneeviannikkkyNo ratings yet
- MergedDocument13 pagesMergedviannikkkyNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- A Qualitative Study Thypoid in MadagascarDocument7 pagesA Qualitative Study Thypoid in MadagascarviannikkkyNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Ekstraksi Forceps Vacuum Mahasiswa Fkui TK ViDocument19 pagesEkstraksi Forceps Vacuum Mahasiswa Fkui TK ViCiiezz BunciiezzNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Serious Asthma Events With FluticasoneDocument9 pagesSerious Asthma Events With FluticasoneviannikkkyNo ratings yet
- Glycemic Control and Cardiovascular OutcomesDocument10 pagesGlycemic Control and Cardiovascular OutcomesGrace KahonoNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Gestational Trop Ho Blastic NeoplasiaDocument9 pagesGestational Trop Ho Blastic NeoplasiaviannikkkyNo ratings yet
- Kritall APRASIALDocument7 pagesKritall APRASIALHaidar ShiddiqNo ratings yet
- Typhoid Fever and It Association With Environmental Factors in The Dhaka Metropolitan Area of Bangladesh A Spatial and Time-Series ApproachDocument14 pagesTyphoid Fever and It Association With Environmental Factors in The Dhaka Metropolitan Area of Bangladesh A Spatial and Time-Series ApproachviannikkkyNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Handbook: For Clinical Management of DengueDocument124 pagesHandbook: For Clinical Management of DengueraattaiNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Kritall APRASIALDocument7 pagesKritall APRASIALHaidar ShiddiqNo ratings yet
- A Qualitative Study Thypoid in MadagascarDocument7 pagesA Qualitative Study Thypoid in MadagascarviannikkkyNo ratings yet
- CA CervixDocument43 pagesCA CervixSabrina Indri WardaniNo ratings yet
- Obstetrics and Gynecology New Treatment Guidelines - 2008Document56 pagesObstetrics and Gynecology New Treatment Guidelines - 2008aminskiNo ratings yet
- Randomized Trialof Labour Induction in WomenDocument10 pagesRandomized Trialof Labour Induction in WomenviannikkkyNo ratings yet
- A Cluster-Randomized Trial To Reduce Cesarean Delivery Rates in QuebecDocument12 pagesA Cluster-Randomized Trial To Reduce Cesarean Delivery Rates in QuebecviannikkkyNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Female Reproductive HealthDocument276 pagesFemale Reproductive HealthviannikkkyNo ratings yet
- Hepatocellular CarcinomaDocument16 pagesHepatocellular CarcinomaviannikkkyNo ratings yet
- History Taking Form in Gynecology Obstetrics - CompressDocument8 pagesHistory Taking Form in Gynecology Obstetrics - CompresskeightNo ratings yet
- Colic Surgery Recent Upda - 2023 - Veterinary Clinics of North America EquineDocument14 pagesColic Surgery Recent Upda - 2023 - Veterinary Clinics of North America EquinediazsunshineNo ratings yet
- 3.muscle TestDocument10 pages3.muscle TestSummer PookieNo ratings yet
- StaphylococcusDocument28 pagesStaphylococcusAliyah SajaNo ratings yet
- Pricelist 13 Juli 2020Document21 pagesPricelist 13 Juli 2020Achmad Sya'idNo ratings yet
- Stabilis-Monographie-Doxorubicin Hydrochloride Liposome PegDocument9 pagesStabilis-Monographie-Doxorubicin Hydrochloride Liposome PegSepti Marta SariNo ratings yet
- Pulmonaryrehabilitation 180412172759Document44 pagesPulmonaryrehabilitation 180412172759IvanNo ratings yet
- Chapter 7-Brief Psychodynamic Therapy: BackgroundDocument54 pagesChapter 7-Brief Psychodynamic Therapy: BackgroundKarenHNo ratings yet
- Journal of Interventional Medicine: Yanli Wang, Guohao Huang, Tian Jiang, Xinwei HanDocument5 pagesJournal of Interventional Medicine: Yanli Wang, Guohao Huang, Tian Jiang, Xinwei HanDzulRizkaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- DRUGS (Topotecan)Document2 pagesDRUGS (Topotecan)BARRISTERFLOWERSEAURCHIN6No ratings yet
- Chist de Septum PellucidumDocument3 pagesChist de Septum PellucidumdansarariuNo ratings yet
- 3rd Year Syllabus-202Document24 pages3rd Year Syllabus-202Sahal ShaikhNo ratings yet
- List of PM&DC Recognized JournalsDocument14 pagesList of PM&DC Recognized JournalsSanaa AhmedNo ratings yet
- MNT For Rheumatic DiseaseDocument107 pagesMNT For Rheumatic DiseasejwhssanNo ratings yet
- Tarun Kumar ReportDocument1 pageTarun Kumar Reportnavdeep madheshiyaNo ratings yet
- Respiratory SystemDocument7 pagesRespiratory SystemNgọc Mai Khanh NguyễnNo ratings yet
- Access Corporate Fact SheetDocument2 pagesAccess Corporate Fact SheetMattNo ratings yet
- Epidemology TestDocument12 pagesEpidemology TestS.100% (1)
- Hyperemesis GravidarumDocument16 pagesHyperemesis GravidarumArra MayNo ratings yet
- Health Teaching Plan For Dengue Hemorrhagic FeverDocument3 pagesHealth Teaching Plan For Dengue Hemorrhagic Fevershiramu100% (5)
- Perioperative Nursing 1Document2 pagesPerioperative Nursing 1Rosie Cuasito100% (2)
- Utility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonDocument6 pagesUtility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonAmanda AlmaNo ratings yet
- Makerere AR 67th Graduation Day2 22ndfeb2017Document40 pagesMakerere AR 67th Graduation Day2 22ndfeb2017The Independent Magazine100% (2)
- Polyphenols, and Physical PerformanceDocument7 pagesPolyphenols, and Physical PerformancezoliteamlavylitesNo ratings yet
- Government College of Nursing JodhpurDocument7 pagesGovernment College of Nursing JodhpurNaresh JeengarNo ratings yet
- Congenital DiseaseDocument39 pagesCongenital DiseaseRavi SharmaNo ratings yet
- Immunological Tolerance, Pregnancy, and Preeclampsia: The Roles of Semen Microbes and The FatherDocument39 pagesImmunological Tolerance, Pregnancy, and Preeclampsia: The Roles of Semen Microbes and The FatherAnanda Yuliastri DewiNo ratings yet
- Fundamental Concepts of PharmacologyDocument5 pagesFundamental Concepts of PharmacologyphoebeNo ratings yet
- Neuroblastoma RadiopediaDocument8 pagesNeuroblastoma Radiopediaroni pahleviNo ratings yet
- Census FormatDocument35 pagesCensus Formatkolintang1No ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)