Professional Documents
Culture Documents
Regulatory Perspective on Bioequivalence Studies
Uploaded by
bhanu99Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Regulatory Perspective on Bioequivalence Studies
Uploaded by
bhanu99Copyright:
Available Formats
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
BIOEQUIVALENCE STUDIES A REGULATORY PERSPECTIVE
Rudolph Julius D Almeidaab*, Anuradha K Gajjarb
a
Dr. Reddys Laboratories Ltd, Biologics Development Center, Survey No-47, Bachupally,
Qutubullapur, RR District, Andhra Pradesh, India-500090
b
Institute of Pharmacy, Nirma University of Science and Technology,
Sarkhej-Gandhinagar Highway, Ahmedabad - 382 481
Corresponding author
Tel: +91-40-23042004; Fax: + 91-40-23041418
E-mail address: rudolphalmeida@gmail.com
Summary
The concept of bioequivalence is well established in the regulated drug markets. Due to the high
number of studies, significant number bioequivalence related problems are also observed. A
number of studies of marketed drug products which includes the same therapeutic ingredient
from different manufacturers have revealed significant differences in rate and extent of drug
absorption. There are regulatory bodies from different countries which provide standard
requirements for conducting and reporting these bioequivalence studies. The recommendations
of few such regulations for bioequivalence studies are enumerated in this review. As more
number of generic drug makers are pushing for faster approvals, regulatory bodies should be
more vigilant in maintaining the right standards for designing and reporting of these
bioequivalence studies.
Keywords: Bioequivalence studies, bioavailability, regulatory guidelines, pharmacokinetics
Introduction
To demonstrate therapeutic equivalence between two drug products bioequivalence (BE) studies
are considered to be one of the widely and commonly used methods1-3. While using these
studies, the pharmaceutical companies can save lot of time and cost for the development of their
molecules. This is the reason why the bioequivalence have received major importance from the
pharmaceutical companies, contract manufacturing organizations and some institutions. While
planning, designing, conducting, analyzing and reporting of these studies requires lot of
regulatory attention. These bioequivalence studies focus on release characteristics of the
formulation and subsequent absorption into the systemic circulation and acts as an important
element for submission of new or abbreviated drugs or its supplements to the respective
867
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
regulatory authority approvals1. As there are many numbers of generic products are available in
the international markets, it has become a public concern that these products are similar to that of
innovator in terms of safety and efficacy. Therefore a valid statistical evaluation is necessary to
guarantee the safety and efficacy of these products2.
These regulatory guidelines are intended to provide recommendations to pharmaceutical
industries or applicable stakeholders about the planning of these studies. There are various
regulatory recommendations to carry out these bioequivalence studies and depends on country
for which the submission is planned3-14, 52-56. WHO has developed a standard bioequivalence trial
information form (BTIF) and the generic drug products of HIV/AIDS, tuberculosis & malaria are
to be submitted as per this form along with required documents15. The regulatory requirements
for orally administered drug products are well established but for other classes of products,
including biological (biosimilars) and product manufactured by biotechnology, the concept of
bioequivalence remains complex and not established16-19. Only EMEA has a guideline on
developing similar biological medicinal products and other countries would follow soon as
several of these molecules are going off patent in near future20, 21.
This review makes an attempt to establish the differences between the various regulatory
guidelines for bioequivalence studies. The differences are enumerated based on the study design,
type of drug product, subject selection, drug dosing, bioanalytical methodology, moieties to be
measured, sampling schedules and pharmacokinetic parameters.
Study design
The study design should be such that the formulation effects should be distinguished from other
effects3. To measure the pharmacokinetic properties of the active ingredient of the drug a
suitable biological matrix such as blood, plasma and/or serum should be collected for analysis. If
the validated analytical method is not available then the sponsor can opt for conducting a pilot
study with small number of subjects. If the sample size is found to be very high based on the
calculations and assumptions a pilot study can be planned and results can be simulated for the
pivotal bioequivalence study. Most of the regulatory authorities recommend for comparative,
nonreplicate, two periods, two-sequence crossover study designs for the oral drug products,
which includes immediate and modified release formulations1-14. The choice of selecting parallel
(for long half-life drugs), replicate (for highly variable drugs) or nonreplicate design depends on
the statistical recommendations and type of information to be gathered from these studies.
The studies will be carried out using adequate number of healthy subjects in a statistically
powered design. The choice of sample size and the level of statistical significance should be
justified in the protocol. As per Anderson, Liu and Chow, drug switchability would be assured
by assessing bioequivalence within individual subjects2. The subjects should be administered
either test or reference product with specified amount of water under fasting conditions. If the
pharmacokinetics of the drug is affected by presence of food then well designed food-effect
bioequivalence study should be conducted7, 9. The recommendations for food-effect studies may
vary from country to country based on the social and cultural variations but the appropriate
868
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
justification should be provided for the type of food given. These studies are majorly applied for
modified release dosage forms.
As per EMEA, if the Summary of Product Characteristics (SPC) defines food intake based on the
pharmacokinetic properties i.e, increase in bioavailability, to decrease adverse events and/or
improve tolerability fed studies should be planned in addition to the fasting studies. Fluid and
food intake, physical activity, and consumption of certain dietary products must be carefully
restricted during the study course so that these factors will not influence drug absorption or
elimination22.
Type of drug product
Most of the regulatory agencies recommend single dose studies with orally administered drugs
which includes immediate and modified release dosage forms. The sensitivity in assessing the
drug release pattern from these dosage forms is very evident with single dose studies. There are
instances where the regulation asks for conducting the multiple dose studies. These can be
enumerated as, if the
- drug is embedded in modified release dosage form
- drug is following non-linear pharmacokinetics
- sensitivity of the analytical method is poor after single dose administration
- drug demonstrates high intra-subject variability
While designing these multiple dose studies, importance should be given on selection of
appropriate dose and sampling points to demonstrate steady state1-14.
BE studies are waived for solutions on the assumption that release of the drug substance from the
drug product is self-evident and that the solutions do not contain any excipients that significantly
affects drug absorption11. If the application is for the generic drug then the test product should be
compared with the corresponding dosage form of the reference product. The choice of selecting
the strength, dosage and formulation of the reference product should be justified in the protocol3.
The test product should be manufactured under GMP conditions, the batch records and
comparative in-vitro dissolution profiles should be maintained. While selecting a highly variable
drug (HVD), due to its poor formulation characteristics the test drug may not show bioequivalent
to that of reference drug8, 23.
Subject selection
The subject selection is purely based on the power function of the parametric statistical test
procedure applied. A major objective of subject selection criteria is a reduction in
pharmacokinetic variability attributed to subjects characteristics. A written informed consent
should be obtained from all the subjects participating in the BE studies. Sponsor should also take
care of adequate sample size to accommodate the dropouts because replacing the subjects may
complicate the statistical analysis1. Agencies like CDSCO, India recommends to replace a
subject withdrawn/drop out from the study once it has begun provided the substitute must follow
the same protocol and controlled conditions. If for any reason other than adverse event (AE) or
869
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
serious adverse event (SAE) the subject withdraws the results of all samples that were measured
must be included in the report10. If subjects drop out of the study for personal reasons, the
subject's blood samples do not have to be assayed5. Japans National Institute of Health allows
the addition of subjects to increase the power of a failed BE study. However, the add-on subjects
cannot be less than half the number in the original study13, 24.
Most of the regulatory agencies recommend minimum number of subjects to be enrolled but the
decision lies with the sponsor. The general recommendation is to enroll normal healthy subjects
of either sex, preferably non-smokers and non-alcoholics. The sponsor should also consider the
appropriate demographic profile to minimize the inter-subject variability. If there are safety
concerns as in the case of cytotoxic or antiretroviral or specific population (patients) and gender
(females in case of oral contraceptives) should be selected25, 26. Other factors such as age, body
size, nutritional status, tobacco use, disease states, concurrent drug use, and substance abuse
must be considered to identify a suitable subject population in which the product formulations
will be the only significant determinants of bioequivalence22.
Drug dosing
In the bioequivalence studies of a generic product, a highest approved strength of the innovator
product will be used unless there are safety concerns preventing the use of this strength1, 3. The
dose administered should not be more than the recommended labeling instructions. For a single
dose study US FDA recommends, test and reference products should not vary more than 5% in
their potencies. The drug should be administered with sufficient fluid after at least 10 hours of
fasting which is continued for at least 4 hours post-dose. To minimize the carry over effect a
sufficient washout period should be scheduled between treatments1. Appropriate restrictions on
fluid intake and physical activities should be maintained and all vital signs and adverse events
are monitored post-dose.
To reduce the gastrointestinal side effects some drugs are given with food. Studies of such drugs
should include studies with standard meals. The nature of the test meal to be administered-in the
part of the study where the formulation is given in the presence of food-should be determined
based on the physicochemical and pharmacokinetic characteristics of the drug and its
formulation. The appropriate choice of the meal's timing and its contents should be chosen
carefully7, 9.
Sampling schedules
The samples using appropriate biological matrix (blood, plasma, serum or urine) would be
collected at different time periods from the participating subjects. The selection of these time
points mainly depends on the pharmacokinetic behavior of the drug in the body16, 17, 38. Based on
the in-vitro dissolution data using deconvolution method can help to determine the accurate
sampling time points. Generally the biological matrix of choice is plasma or serum and if the
measurement with these neither are nor reliable then urine may be analyzed. The trapezoidal rule
is used on these sampling time points to estimate the area under the plasma concentration-time
curve. After a single dose of administration, a rule of thumb is that blood samples are drawn at
870
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
several times during the absorption phase of the drug, then several times near the peak and at
relatively fewer times in the elimination phase. Usually, 10-15 total sampling times are
employed27-29. There are various designs published related to selection of appropriate sampling
time points for individual and population pharmacokinetic studies. Increase in sampling time
points may lead to concerns in ethical practices as this may lead to higher volume of blood draw,
inconvenience due to number of vein punctures and compensation to the participating subjects17.
Moieties to be measured
In many cases the evaluation of bioequivalence would be based on the measured concentration of
the parent compound3. The concentration-time profile of the parent compound is more sensitive
to changes in formulation performance than a metabolite, which majorly reflects metabolism,
distribution and elimination1. If the concentration of active compound is too low in the biological
matrix and results in high variability or metabolite contributes significantly to safety and/or
efficacy in those cases active or inactive metabolites of the compound can be measured. To
understand the clinical pharmacology characteristics of a new drug it is always advisable to study
the metabolite but this is still debated as it comes to the BE studies30, 31. If the metabolite
significantly contributes to the total activity of an active substance and the pharmacokinetic
system is nonlinear then both the parent and metabolite plasma concentrations should be
measured separately. Eventually there are no specific regulatory guidelines which explain the
requirements of submitting the metabolite data, but recommends that the sponsor should consult
with the respective regulatory agency while preparing the protocol16. The complete statistical
evaluation should be performed to the parent compound and the metabolite data can be used as a
supportive evidence for comparing the therapeutic outcome32.
Bioanalytical methodology
Bioequivalence determination is purely dependent on the use of adequate analytical method used
for the analysis of parent or metabolite33, 35. The reliability of the method used can be established
by using different validation techniques. The validation demonstrates that the method used is
appropriate for the intended purpose, i.e, qualitative, semi-quantitative or quantitative
determination of drugs in the pharmaceutical formulations. US FDA has published a separate
guideline on Bioanalytical Method Validation to assist sponsors in validating the bioanalytical
methods34. Most of the regulatory bodies recommend that the methods used must be accurate,
precise, specific, sensitive and reproducible. The analyst can modify the existing method as per
the requirements but should be validated to ensure the performance. The validation procedures
should be carried out using the same biological matrix for e.g. plasma to plasma or serum to
serum. The stability procedures of samples should be studied and should reflect situations likely
to be encountered during sample collection and analysis. It is recommended to select sufficient
number of (~6 to 8) standards to correlate the relationship between concentration and response of
the drug to be studied.
Enantioselective bioanalytical methods:
During the drug development process the sponsor always choose to submit the data on racemic
drugs instead of their constituent enantiomers. If the enantiomers differ in their
871
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
pharmacodynamic and pharmacokinetic properties as a result of stereo selective interaction with
the biological molecules, the analyst should develop suitable method to identify the single safe
and effective isomer36-38. Presently there is no regulatory precedence to address stereochemical
aspects in bioequivalence studies, but there are only a few examples in the literature whereby the
investigators have employed stereoselective assays in the bioequivalence testing of racemic
drugs 39-41. US FDA recommends measurement of individual enantiomer for bioavailability
studies and for BE, measurement of racemates using an achiral assay would suffice. EMEA
recommends BE studies of chiral active substance should be supported with enantiomeric
bioanalytical methods. Japan has not issued any specific guideline on chiral drug development
but recommends approaches mentioned in US FDA and EMEA guidelines.
Pharmacokinetic & Statistical analysis
The major concern in bioequivalence studies is to quantify the difference between the
bioavailability of test and reference products and to ensure that they are not clinically different3.
Generally majority of the regulatory bodies require both pharmacokinetic and statistical
information on test and reference formulations under investigation42-49. The pharmacokinetic
parameters obtained from plasma concentrations (e.g. Cmax and AUC) should be subjected to
logarithmic transformation before analysis. The observed AUC (0-), Cmax or Tmax from the
blood or plasma concentration-time is preferred because they provide the essential information
about the pharmacokinetic characteristics in assessment of bioequivalence and are model
independent and easy to calculate2. Various rules were proposed by FDA from 1977 to 1992 for
testing the bioequivalence in terms of average bioavailability for specific drugs where the AUC
and Cmax were the primary measures. Out of the several, only 20 rule was acceptable by FDA
for evaluation of average bioequivalence but sometime it may lead to inconsistent conclusions.
Therefore the acceptable statistical method used for estimation of bioequivalence would be based
on the 90% confidence interval (CI) for the parameters under consideration i.e. Cmax and AUC
and should be in the limit of 80 to 125%. Except EMEA, no other regulatory agency has
suggested the acceptance limits for narrow therapeutic or highly variable drug products.
Interestingly, The Danish Medicines Agency considers that the bioequivalence acceptance limits
for immunosuppressives must be within 90-111% as they are narrow therapeutic index drugs50.
Most of the BE studies are designed to evaluate the average bioequivalence and therefore there
are no specific recommendations for individual and population studies51. Considerable amount of
debate is in progress for accepting the individual BE requirements proposed by FDA. The
individual BE approach offers flexible equivalence criteria based on the individual therapeutic
window and the variability of the reference drug product which is referred as subject to
formulation interaction2, 16, 42. As there are several issues related to this concept, regulatory
authorities need to explore before implementing as a guideline. FDA clearly states that if the
predose concentration is more than 5% of Cmax, then the subject should be dropped from all the
BE study evaluation1. There are no other regulatory except FDA which describes handling the
data if there is vomiting reported for immediate and modified release dosage forms. There are
several tests published for the detection of outlying data but there are no specific
recommendations mentioned in the regulatory guidelines. Therefore reporting and handling of
missing values and outliers should be described in the protocol. Few of the regulatory
recommendations while designing and conducting a standard BE study are tabulated in Table 1,
872
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
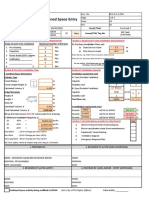
Table 1: Regulatory agency recommendations for bioequivalence study designs
Details
Regulatory Agency recommendations
US FDA
EMEA
TPD
ANVISA
Number of
Minimum 12
Not less than 12
Minimum 12
Based on adequate
subjects
statistical power
CDSCO
Not less than 16
Design
Non replicate,
Crossover, two
treatment, two
period, two sequence
Crossover, two
treatment, two
period, two
sequence
Crossover, Two
period
Non replicate,
crossover, two
treatment, two
period, two sequence
Crossover, two
treatment, two
period, two
sequence
Food effect study
Fast and fed studies
are required for
immediate and
modified release
dosage forms
Fasted studies for
immediate release
and both fasted
and fed studies
for modified
release dosage
forms
Fasted studies for
immediate release
and both fasted
and fed studies
for modified
release dosage
forms
Fasted studies for
immediate release
and both fasted and
fed studies for
modified release
dosage forms
Fasted studies for
immediate release
and both fasted
and fed studies for
modified release
dosage forms
Fasting status
Fasted for at least 10
hrs before drug
administration
Fasting for at
least during the
night prior to
dosing
Fasted for 10 hrs
before dosing
Fasted for at least 8
hrs before drug
administration
Fasted for at least
10 hrs before drug
administration
Water intake
Allowed water as
desired except for 1
hour before and after
dosing.
240 mL water will
be allowed during
dosing.
Abstain from
alcohol for 24 hrs
At least 150 mL
with dose.
250 mL water
permitted upto 2
hrs of dosing.
150 mL water
with the dose.
Not specified
To be standardized
and mentioned in
the protocol.
Should not have a
history of alcohol
Should be
mentioned in the
To be mentioned in
the protocol
During the study
and at least 48 hrs
Alcohol intake
873
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
before each study
abuse.
period and until after
the last sample from
each period is
collected.
protocol.
before its
commencement
Meals
Meals allowed no
less than 4 hours
after dosing
Not specified
Meals after 4 hrs
of dosing
Not specified
Meals 4 hrs after
dosing
Sampling schedule
Sampling at least
three or more
terminal half lives of
the drug
Till adequate
estimation of
Cmax and AUC
At least three
times the terminal
half-life of the
drug.
Equal to or higher
than 3-5 times the
elimination half-life
of the drug or
metabolite
At least 3
elimination halflives
Washout period
Washout period at
least 5 elimination
half-lives
Washout period at
least 3
elimination halflives
Not less than 10
times the mean
terminal half-life
of the drug
Washout period at
least 7 elimination
half-lives
Washout period
5 elimination halflives
Number of
samples
12 to 18 samples,
including a predose
sample, be collected
per subject per dose.
Adequate
estimation of
Cmax & AUC
12 to 18 samples
should be
collected per
subject per dose
Predose and other
Adequate
sampling time points estimation of total
to be mentioned in
AUC
protocol
Steady state
studies
Not required
Required, if the
formulation is
prolonged release
or transdermal.
Required, if AUC
ratio is less than
80%
Not recommended
Required on case
to case basis
Observed AUC
% of AUC to be
observed >88%
> 80%
> 80%
Not specified
Not specified
874
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
Metabolite
analysis
Required for drugs
which form
metabolite before or
during absorption
phase
Required for
prodrugs or
metabolite has
significant
efficacy
None
Required, if
metabolite is active
Not specified
Statistical
approach
Pharmacokinetic
parameters
Average BE
Average BE
Average BE
Average BE
Average BE
AUCt, AUCinf,
Cmax
AUCt, AUCinf,
Cmax
AUCt, Cmax
AUCt, AUCinf,
Cmax, Tmax
AUCt, AUCinf,
Cmax, Tmax
Bioequivalence
criteria
90% CI between 80125.00%
90% CI between
80-125.00%
90% CI between
80-125.00%
90% CI between 80125.00%
90% CI between
80-125.00%
BE criteria for
HVD
Not specified
Cmax 75-133%
for HVD
Cmax-Add on
Not specified
Not specified
studies are
recommended
EMEA: European Medicines Agency
ANVISA: National Health Surveillance Agency
US FDA: United States Food & Drug Administration
TPD: Therapeutic Products Directorate
CDSCO: Central Drugs Standard Control Organization
875
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
Conclusions
As technology advances and regulations tighten, the competition to get new drugs on to the
market has never been easy. The next few years look to be a critical time for the pharmaceutical
industry as there is more number of challenges in generic portfolios. The development pipeline
looks increasingly sparse, so equipping pharmaceutical business with cutting edge technologies
and efficient strategies for drug development and reformulation will be the best way to keep
profits high. The US FDA is also aiming to create an online database of bioequivalence study
guidelines. This would be helpful to acquire information on designing bioequivalence studies for
various types of drug products57. There are lot of other online forums available which discuss
various scientific issues and requirements related to bioequivalence studies. Therefore countries
should make an attempt to further strengthen their regulations clubbed with scientific discussions
in providing safe and affordable drugs to the patients.
References
1. Guidance for Industry: Bioavailability and bioequivalence for orally administered drug products.
General Considerations, Food and Drug Administration (FDA), Centre for Drug Evaluation and
Research, March 2003.
2. Chow SC, Liu J. Design and analysis of bioavailability and bioequivalence studies. Edition: 2
2000
3. Committee for Proprietary Medicinal Products (CPMP), Note for guidance on the Investigation
of bioavailability and bioequivalence (CPMP/EWP/QWP/1401/98), The European Agency for
the Evaluation of Medicinal Products, Evaluation of Medicines for Human Use, January 2002.
4. GCP inspectors working group. Reflection paper on advice to applicants/sponsors/
CROs of bioequivalence studies, European medicines agency inspections, September 2008
5. Health Products and Food Branch, guidance for industry, Conduct and Analysis of
Bioavailability and Bioequivalence Studies - Part A: Oral Dosage Formulations Used for
Systemic Effects, 1992.
6. Health Products and Food Branch Guidance for Industry, Conduct and Analysis of
Bioavailability and Bioequivalence Studies - Part B: Oral Modified Release Formulations, 1996.
7. Health Products and Food Branch, Guidance for industry, Bioequivalence Requirements:
Comparative Bioavailability Studies Conducted in the Fed State, 2005
8. Health Products and Food Branch, Guidance for industry, Bioequivalence requirements: critical
dose drugs, 2006
9. Guidance for Industry: Food-effect Bioavailability and fed bioequivalence studies, Food and
Drug Administration (FDA), Centre for Drug Evaluation and Research. 2002.
10. Guidelines for bioavailability and bioequivalence studies. Central drugs standard control
organization, Directorate General Health Services, Ministry oh Health & Family Welfare,
Government of India, New Delhi. March 2005.
11. Food and Drug Administration. Code of Federal Regulations. Title 21, Part 320: Bioavailability
and Bioequivalence Requirements, 2003.
12. Guide for relative bioavailability/bioequivalence tests of drug products. ANVISA Resolution RE n 896, of May 29, 2003
876
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
13. Clinical pharmacokinetic studies of pharmaceuticals. Ministry of Health, Labour, and Welfare,
Japan, 1 June 2001
14. Guidelines for the design and evaluation of oral prolonged release dosage forms, Ministry of
health and welfare, Japan, March 11, 1988
15. Information for Applicants: Guidelines: Generics Annex 7, Presentation of BE Trial Information
(BTIF): World Health Organization, Aug 2005.
16. Rani S. Bioequivalence: issues and perspectives. Indian J Pharmacol 2007; 39 (5):218-225.
17. Cedar L. Elements of successful bioequivalence studies. CanBiotech newsletter 2003;2:13-15
18. Nation RL, Sansom LN. Bioequivalence requirements for generic products. Pharmacol Ther
1994;62:41-55.
19. Patnaik R, Lesko LJ, Chan K, Williams RL. Bioequivalence assessment of generic drugs. An
American point of view. Eur J Drug Metab Pharmacokinet 1996;21:159-64
20. Stavchansky S. Pharmaceutical equivalence of biological drug products. J Pharm Pharm Sci
2001;4:77-137
21. Committee for Medicinal Products for Human (CHMP). Guideline on similar biological
medicinal products (CHMP/437/04), 2005.
22. Henderson JD, Dighe SV, Williams RL. Subject Selection and Management in Bioequivalence
Studies. Clin Research and Regulatory Affairs 1992;9(2):71-87.
23. Midha KK, Rawson MJ, Hubbard JW. The bioequivalence of highly variable drugs and drug
products. Int J Clin Pharmacol Ther 2005;43:485-98.
24. Haidar SH, Davit B, Chen ML, et al. Bioequivalence approaches for highly variable drugs and
drug products. Pharm Res 2008:25(1):237-41
25. Guideline for the study and evaluation of gender differences in clinical evaluation of drugs. U.S.
Food and Drug Administration. Fed Regist 1993; 58: 39406-16.
26. Harris RZ, Benet LZ, Schwartz JB. Gender effects in pharmacokinetics and pharmacodynamics.
Drugs 1995;50:222-39.
27. Choi L, Caffo B, Rohde C. Optimal Sampling Times in Bioequivalence Studies Using a
Simulated Annealing Algorithm. Johns Hopkins University, Dept. of Biostatistics Working
Papers 2004. Working Paper 59.
28. Jackson AJ. Evaluation of a limited sampling method to determine the bioequivalence of highly
variable drugs with long half-lives. Biopharm Drug Dispos 2001;22:179-90.
29. Hui Kong F, Gonin R. Optimal sampling times in bioequivalence tests. J Biopharm Stat 2000;
10(1):3144
30. Jackson AJ, Robbie G, Marroum P. Metabolites and bioequivalence: Past and present. Clin
Pharmacokinet 2004; 43 (10):655-672.
31. Chen ML, Jackson AJ. The role of metabolites in bioequivalency assessment: I: Linear
pharmacokinetics without first-pass effect. Pharm Res 1991;8:25-32
32. Bioequivalence requirements guidelines. Kingdom of Saudi Arabia, Saudi food and drug
authority, drug sector draft May 2005.
33. ICH Harmonised Tripartite guideline: Validation of analytical procedures: text and methodology
Q2 (R1), Current Step 4 version, Parent Guideline dated 27 October 1994 (Complementary
Guideline on Methodology dated 6 November 1996 incorporated in November 2005).
34. Guidance for Industry, Bioanalytical Method Validation, U.S. Department of Health and Human
Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for
Veterinary Medicine (CVM), May 2001.
877
Pharmacologyonline 2: 867-878 (2009)
Newsletter
DAlmeida et al.
35. Guide for validation of analytical and bioanalytical methods. ANVISA Resolution - RE n. 899,
of May 29, 2003
36. Health Products and Food Branch, Guidance for industry, Stereo chemical Issues in Chiral Drug
Development, 2000
37. Department of Health and Human Services, Food and Drug Administration. FDAs policy
statement for the development of new stereoisomeric drugs. Federal Register 1992: 57: 22249
38. CPMP Working Parties on Safety and Efficacy of Medicinal Product, Commission of the
European Communities, Note for Guidance: Investigation of Chiral active substances III/3501/91
last revised June 1997.
39. Srinivas NR. Role of Stereoselective Assays in Bioequivalence Studies of Racemic Drugs: Have
We Reached a Consensus? J Clin Pharmacol 2004; 44:115-119.
40. Srinivas NR, Barbhaiya RH, Midha KK. Enantiomeric Drug Development: Issues,
Considerations, and Regulatory Requirements. J Pharm Sciences 2001;90 (9):1205-1215.
41. Shimazawa R, Nagai N, Toyoshima S, Okuda H. Present state of new chiral drug development
and review in Japan. Journal of Health Science 2008;54 (1):24-29.
42. Guidance for Industry. Statistical Approaches to Establishing Bioequivalence, U.S. Department
of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and
Research (CDER), January 2001
43. Anderson S, Hauck WW. Consideration of individual bioequivalence. J Pharmacokinet
Biopharm 1990;18:259-73
44. Chen ML. Individual bioequivalence: A regulatory update. J Biopharm Stat 1997;7:5-11.
45. Average, Population and Individual approaches to establishing bioequivalence. 1999
46. Rani S, Pargal A. Bioequivalence: An overview of statistical concepts. Indian J Pharmacol
2004;36:209-16
47. Guide for planning and carrying out the statistical stage of studies of relative
bioavailability/bioequivalence. ANVISA Resolution - RE n. 898, of May 29, 2003
48. Tsang YC, Hems J, Spino J. Use of AUC 0-72 in bioequivalence assessment for drugs with a long
half-life. Pharm Res 1996;13:S477.
49. Midha KK, Rawson MJ, Hubbard JW. Prescribability and switchability of highly variable drugs
and drug products. J Control Release 1999;62:33-40
50. Bioequivalence and labelling of medicinal products with regard to generic substitution. The
Danish Medicines Agency, 13 July 2005, updated 17 January 2006.
51. Chen ML, Patnaik R, Hauck WW, et al. An individual bioequivalence criterion: regulatory
considerations Statistics in Medicine 2000; 19(20):2821-4242
52. Meredith PA. Generic drugs: Therapeutic equivalence. Drug Saf 1996; 15:233-42
53. ASEAN guidelines for the conduct of bioavailability and bioequivalence studies. Final draft : 21
July 2004.
54. Malaysian guidelines for the conduct of bioavailability and bioequivalence studies. Ministry of
health, Malaysia supported by seminar on clinical trials and bioequivalence studies, 14
September 2000.
55. South Korean guidelines for Minimum Requirements for bioequivalence test, Dec 2005.
56. Submission of BA/BE Dossiers: Ministry Of Health Of The Turkish Republic Pharmaceutical
General Directorate, Jan 2006
57. Guidance for Industry. Bioequivalence Recommendations for Specific Products. U.S.
Department of Health and Human Services, Food and Drug Administration, Center for Drug
Evaluation and Research (CDER), May 2007.
878
You might also like
- Bid ProcessDocument85 pagesBid ProcessRobiatol Adawiah Mohammad ShamsidiNo ratings yet
- Altered Pharmacokinetics in Liver DiseasesDocument30 pagesAltered Pharmacokinetics in Liver DiseasesNailaAns100% (1)
- Chapter 2 New Drug and DevelopmentDocument152 pagesChapter 2 New Drug and DevelopmentMeriam JuanNo ratings yet
- Introspective Hypnosis Class - 052017 - Antonio Sangio (2745)Document62 pagesIntrospective Hypnosis Class - 052017 - Antonio Sangio (2745)sandra100% (4)
- Guidelines On Bio Similar SDocument201 pagesGuidelines On Bio Similar Sbhanu99No ratings yet
- 1 Introduction - BiopharmaceuticsDocument32 pages1 Introduction - BiopharmaceuticsLouie Fernand LegaspiNo ratings yet
- Root Cause Analysis and Corrective Actions To Prevent Recurrence (PDFDrive)Document46 pagesRoot Cause Analysis and Corrective Actions To Prevent Recurrence (PDFDrive)bhanu99No ratings yet
- Pharmacokinetics GuideDocument59 pagesPharmacokinetics GuideirrelevantNo ratings yet
- Ice-Cream ProductionDocument65 pagesIce-Cream ProductionMujtaba HaseebNo ratings yet
- The Crime of Galileo - de Santillana, Giorgio, 1902Document372 pagesThe Crime of Galileo - de Santillana, Giorgio, 1902Ivo da Costa100% (2)
- Bioavailability & Bioequivalence studies guideDocument45 pagesBioavailability & Bioequivalence studies guideHussein Talal Kenaan100% (2)
- BioassayDocument38 pagesBioassayMuhammad Masoom AkhtarNo ratings yet
- Formulation and DevelopmentDocument38 pagesFormulation and Developmentapi-3810976100% (2)
- Targeted Drug Delivery Systems - BRAINDocument51 pagesTargeted Drug Delivery Systems - BRAINsunil100% (6)
- Drug DesignDocument12 pagesDrug DesignAlok KumarNo ratings yet
- Concept and Design of Rate Controlled Drug DeliveryDocument57 pagesConcept and Design of Rate Controlled Drug Deliveryufahad88% (8)
- ICH-Guidelines SummaryDocument34 pagesICH-Guidelines SummarySamiksha More100% (1)
- Introduction To BiopharmaceuticsDocument27 pagesIntroduction To BiopharmaceuticsAmina Akther Mim 1821179649No ratings yet
- Biopharmaceutics and PharmacokineticsDocument38 pagesBiopharmaceutics and Pharmacokineticsmj.vinoth@gmail.comNo ratings yet
- BioavailabilityDocument35 pagesBioavailabilityDr. Bharat JainNo ratings yet
- Comparisonofweldingeconomy Kehlnaht 12551752Document10 pagesComparisonofweldingeconomy Kehlnaht 12551752Asebaho BadrNo ratings yet
- Optimization in Pharmaceutics & ProcessingDocument75 pagesOptimization in Pharmaceutics & ProcessingAbdul Muheem100% (1)
- Analytical Quality by DesignDocument17 pagesAnalytical Quality by DesignDimitris PapamatthaiakisNo ratings yet
- PPTDocument48 pagesPPTMukesh KumarNo ratings yet
- Bioavailability and BioequivalenceDocument82 pagesBioavailability and Bioequivalenceكسلان اكتب اسمي100% (1)
- Application of PK in Clinical SitutionDocument42 pagesApplication of PK in Clinical Situtionsafia mehmood100% (1)
- Nonclinical Safety Assessment: A Guide to International Pharmaceutical RegulationsFrom EverandNonclinical Safety Assessment: A Guide to International Pharmaceutical RegulationsWilliam J. BrockNo ratings yet
- Flutter Layout Cheat SheetDocument11 pagesFlutter Layout Cheat SheetJarrett Yew0% (1)
- Eco Schools Action PlanDocument1 pageEco Schools Action PlanJohnty GreentoesNo ratings yet
- Ventilation Plan For Confined Space EntryDocument9 pagesVentilation Plan For Confined Space EntryMohamad Nazmi Mohamad Rafian100% (1)
- Bio PharmaceuticsDocument48 pagesBio PharmaceuticsRajan Kashyap100% (2)
- Quality by Design For ANDAs - MR TabletsDocument161 pagesQuality by Design For ANDAs - MR TabletsShilpa Kotian100% (1)
- Medicine Price Surveys, Analyses and Comparisons: Evidence and Methodology GuidanceFrom EverandMedicine Price Surveys, Analyses and Comparisons: Evidence and Methodology GuidanceSabine VoglerNo ratings yet
- Biopharmaceutics and Pharmacokinetics in Drug ResearchDocument20 pagesBiopharmaceutics and Pharmacokinetics in Drug Researchlenanazarova1969No ratings yet
- Direct Compression TabletDocument61 pagesDirect Compression TabletMitul Shah100% (1)
- Preclinical Trials PDFDocument2 pagesPreclinical Trials PDFFiroz TPNo ratings yet
- Preclinical Research PDFDocument4 pagesPreclinical Research PDFEleyra Llanos Parra100% (1)
- Regulatory Perspective on Bioequivalence StudiesDocument12 pagesRegulatory Perspective on Bioequivalence Studiesbhanu99100% (2)
- Controlled Drug Delivery SystemDocument43 pagesControlled Drug Delivery Systemsukanya100% (1)
- Prodrug Design: Perspectives, Approaches and Applications in Medicinal ChemistryFrom EverandProdrug Design: Perspectives, Approaches and Applications in Medicinal ChemistryRating: 3 out of 5 stars3/5 (1)
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Molecular Biological Markers for Toxicology and Risk AssessmentFrom EverandMolecular Biological Markers for Toxicology and Risk AssessmentNo ratings yet
- BP 181212054815Document74 pagesBP 181212054815Ahmad AinurofiqNo ratings yet
- Tier1-Cvs, Cns and Respiratory Safety Pharmacology, Herg Assay Tier2-Gi, Renal and Other StudiesDocument30 pagesTier1-Cvs, Cns and Respiratory Safety Pharmacology, Herg Assay Tier2-Gi, Renal and Other StudiesCHETHAN K SNo ratings yet
- ToxicokineticsDocument17 pagesToxicokineticsAshwin Ben JamesNo ratings yet
- Qsar Parameters: Sharad P Patange M.Pharm 1 Year Pharmacology School of Pharmacy S.R.T.M.U.NandedDocument23 pagesQsar Parameters: Sharad P Patange M.Pharm 1 Year Pharmacology School of Pharmacy S.R.T.M.U.NandedGatwech DechNo ratings yet
- GRDDSDocument31 pagesGRDDSMuhammad Azam TahirNo ratings yet
- Clinical PharmacokineticsDocument5 pagesClinical Pharmacokineticsfarha naazNo ratings yet
- Compartment ModellingDocument46 pagesCompartment ModellingBio DataNo ratings yet
- Session 1-1 William Potter PDFDocument21 pagesSession 1-1 William Potter PDFDrAmit Verma100% (1)
- Trends in Drug ResearchDocument186 pagesTrends in Drug ResearchEvsevios HadjicostasNo ratings yet
- DRUG DesignDocument19 pagesDRUG DesignAmit SharmaNo ratings yet
- Saquinavir Sodgganga PDFDocument104 pagesSaquinavir Sodgganga PDFSiva PrasadNo ratings yet
- Chemical TESTS For TabletsDocument6 pagesChemical TESTS For TabletsFahad Naeem100% (1)
- Bioavailability and BoequivalenceDocument47 pagesBioavailability and BoequivalenceSilvyNo ratings yet
- BioassayDocument4 pagesBioassayAddictedto Nonsense50% (2)
- Nonlinear Pharmacokinetics 1Document34 pagesNonlinear Pharmacokinetics 1donndisaster100% (1)
- Biological assays measure effects on living systemsDocument19 pagesBiological assays measure effects on living systemsSubhash DhungelNo ratings yet
- Use and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewDocument114 pagesUse and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewMuthu Venkatesh100% (1)
- 5 Biopharmaceutic Considerations of A Drug DesignDocument89 pages5 Biopharmaceutic Considerations of A Drug DesignImDanaBananaaaNo ratings yet
- Bio-Relevant Dissolution MediaDocument30 pagesBio-Relevant Dissolution Mediavinay_anand50% (2)
- Bioassay or Biological AssayDocument9 pagesBioassay or Biological AssayOladayo SiyanbolaNo ratings yet
- Design of Dosage FormsDocument17 pagesDesign of Dosage FormsMuhammad HilmiNo ratings yet
- Types of Research TrialDocument2 pagesTypes of Research TrialGems GlasgowNo ratings yet
- FDA Guidance For Industry S7a Safety Pharmacology Studies For Human Pharmaceuticals PDFDocument14 pagesFDA Guidance For Industry S7a Safety Pharmacology Studies For Human Pharmaceuticals PDFbmartindoyle6396No ratings yet
- (PTSM-I) : Pharmacological & Toxicological Screening Methods-IDocument44 pages(PTSM-I) : Pharmacological & Toxicological Screening Methods-INeha RoyNo ratings yet
- Rate Controlled Drug DeliveryDocument22 pagesRate Controlled Drug DeliveryVee shNo ratings yet
- Formulation and in Vitro Evaluation of Mucoadhesive Tablets of Ofloxacin Using Natural GumsDocument6 pagesFormulation and in Vitro Evaluation of Mucoadhesive Tablets of Ofloxacin Using Natural Gumsabdi100% (1)
- Pharamcokinetics: Course In-Charge: Nimra Waheed Course Name: Biopharmaceutics and Pharmacokinetics Course Code: 613-TDocument21 pagesPharamcokinetics: Course In-Charge: Nimra Waheed Course Name: Biopharmaceutics and Pharmacokinetics Course Code: 613-TNeha GulfamNo ratings yet
- ImmobtrypsinspinDocument3 pagesImmobtrypsinspinbhanu99No ratings yet
- Thermo Scientific - LIMSWikiDocument5 pagesThermo Scientific - LIMSWikibhanu99No ratings yet
- ANVISA Guide Validates Analytical MethodsDocument15 pagesANVISA Guide Validates Analytical MethodsVinod Venkiteswaran Kalyanraman100% (1)
- Scada Indian GuidelineDocument37 pagesScada Indian Guidelinebhanu99No ratings yet
- Guidance For IndustryDocument18 pagesGuidance For IndustryDavid HarlowNo ratings yet
- What Are Web ApplicationsDocument6 pagesWhat Are Web Applicationsbhanu99No ratings yet
- Tunning ParametersDocument9 pagesTunning Parametersbhanu99No ratings yet
- ANVISA Guide Validates Analytical MethodsDocument15 pagesANVISA Guide Validates Analytical MethodsVinod Venkiteswaran Kalyanraman100% (1)
- ANVISA Guide Validates Analytical MethodsDocument15 pagesANVISA Guide Validates Analytical MethodsVinod Venkiteswaran Kalyanraman100% (1)
- 21 CFR Part 11 - 1997 - 2003Document38 pages21 CFR Part 11 - 1997 - 2003bhanu99No ratings yet
- EGA Handbook On Biosimilar MedicinesDocument28 pagesEGA Handbook On Biosimilar Medicinesbhanu99No ratings yet
- 21 CFR Part 11 - 1997 - 2003-1Document7 pages21 CFR Part 11 - 1997 - 2003-1bhanu99No ratings yet
- 3 To 8 Decoder in NGSPICEDocument14 pages3 To 8 Decoder in NGSPICEJaydip FadaduNo ratings yet
- Win Top Prizes in Investizo's SuperTrader ContestDocument3 pagesWin Top Prizes in Investizo's SuperTrader ContestJafrid NassifNo ratings yet
- Geometric Design of Highways for Optimal Traffic FlowDocument123 pagesGeometric Design of Highways for Optimal Traffic FlowGadisa TeferaNo ratings yet
- Power and Energy Meters: Model No. Remarks Sl. WH WH W Va Var 1. ET3021 ET4021Document1 pagePower and Energy Meters: Model No. Remarks Sl. WH WH W Va Var 1. ET3021 ET4021Ram KumarNo ratings yet
- Curios AllianceDocument32 pagesCurios AllianceyesterowNo ratings yet
- 08 - Truck Driver's Dhobi SinkDocument3 pages08 - Truck Driver's Dhobi SinkfebousNo ratings yet
- SNS Bank XS0382843802Document7 pagesSNS Bank XS0382843802Southey CapitalNo ratings yet
- Worksheet Chapter 50 Introduction To Ecology The Scope of EcologyDocument2 pagesWorksheet Chapter 50 Introduction To Ecology The Scope of EcologyFernando CastilloNo ratings yet
- Assignment 2Document2 pagesAssignment 2shivam souravNo ratings yet
- Temp Gradient For Warping Stress in Rigid PavementDocument9 pagesTemp Gradient For Warping Stress in Rigid PavementAmul KotharkarNo ratings yet
- Drilling RisersDocument13 pagesDrilling Risersadvantage025No ratings yet
- Research Associate in The DFG Graduate Program - Collective Decision-Making - (12 Positions) - 28 Subsection 3 HMBHGDocument3 pagesResearch Associate in The DFG Graduate Program - Collective Decision-Making - (12 Positions) - 28 Subsection 3 HMBHGFiya ShahNo ratings yet
- Sap - HR Standard Operating Procedure: Facility To Reset Password of ESSDocument6 pagesSap - HR Standard Operating Procedure: Facility To Reset Password of ESSPriyadharshanNo ratings yet
- 2017 NEC Table of ContentsDocument124 pages2017 NEC Table of ContentsFaheem PP13No ratings yet
- Hypac C 766 C 778Document4 pagesHypac C 766 C 778Dave100% (1)
- Gr07 S DanceDocument17 pagesGr07 S DanceMaliNo ratings yet
- List of British StandardsDocument6 pagesList of British StandardsPankajNo ratings yet
- Reynaers Product Overview CURTAIN WALLDocument80 pagesReynaers Product Overview CURTAIN WALLyantoNo ratings yet
- E-Governance in KeralaDocument10 pagesE-Governance in KeralaRahmath SafeenaNo ratings yet
- A Study On Consumer Preference Towards Skincare With Special Reference To Himalaya Herbal Products in Nilambur at Malappuram District of KeralaDocument4 pagesA Study On Consumer Preference Towards Skincare With Special Reference To Himalaya Herbal Products in Nilambur at Malappuram District of Keralaarcherselevators50% (2)
- Ethics UNAM IsakDocument74 pagesEthics UNAM IsakIsak Isak IsakNo ratings yet
- #1 Introduction To C LanguageDocument6 pages#1 Introduction To C LanguageAtul SharmaNo ratings yet