Professional Documents
Culture Documents
Varianta 2 Articol Epr
Uploaded by
Georgiana BlagociCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Varianta 2 Articol Epr
Uploaded by
Georgiana BlagociCopyright:
Available Formats
CLINICAL RESEARCH
Clinical evaluations of cast gold alloy, machinable zirconia, and
semiprecious alloy crowns: A multicenter study
Ji-Man Park, DDS, PhD,a Yong-Shin Hong, DDS,b Eun-Jin Park, DDS, PhD,c Seong-Joo Heo, DDS, PhD,d and
Namsik Oh, DDS, PhDe
Computer-aided design and
ABSTRACT
computer-aided manufacture
Statement of problem. Few studies have compared the marginal and internal ts of crowns
(CAD/CAM) technology, which
fabricated from machinable palladium-silver-indium (Pd-Ag-In) semiprecious metal alloy.
uses a computer to design and
Purpose. The purpose of this clinical study was to evaluate and compare the marginal and internal
precisely mill dental prostheses,
ts of machined Pd-Ag-In alloy, zirconia, and cast gold crowns.
has been applied to multiple
Material and methods. A prospective clinical trial was performed on 35 participants and 52
areas of dentistry, including the
abutment teeth at 2 centers. Individuals requiring prosthetic restorations were treated with gold
design and fabrication of simple
alloy or zirconia crowns (2 control groups) or Pd-Ag-In alloy crowns (experimental group). A replica
inlays and crowns, complex
technique was used to evaluate the marginal and internal ts. The buccolingual and mesiodistal
xed and removable dental
cross-sections were measured, and a noninferiority comparison was conducted.
prostheses, implants, and
Results. The mean marginal gaps were 68.2 mm for the gold crowns, 75.4 mm for the zirconia
cement- and screw-retained
crowns, and 76.9 mm for the Pd-Ag-In alloy crowns. In the 5 cross-sections other than the distal
implant-supported
restoracross-section,
the 2-sided 95% condence limits for the differences between the Pd-Ag-In alloy
tions.1-9 In addition, this techcrowns and the 2 control groups were not larger than the 25-mm noninferiority margin. The
nology results in consistent
control groups displayed smaller internal gaps in the line angle and occlusal spaces compared
material properties by addresswith the Pd-Ag-In crown group.
ing the deformation issues that
Conclusion. The marginal gaps of machinable Pd-Ag-In alloy crowns did not meet the
result from the casting and
noninferiority criterion in the distal margin compared with zirconia and gold alloy crowns.
sintering processes and by conNonetheless, all 3 crowns had clinically applicable precision. (J Prosthet Dent 2015;-:---)
trolling the shapes and thicknesses of the prosthesis and the space for cement.10,11
with soldering, which makes it difcult to fabricate longThe increased cost of gold has resulted in the need for
span xed dental prostheses.
a replacement material and the use of a precious metal
To overcome the limitations of cast gold crowns and
alloy that contains less gold. Zirconia, which is widely
the disadvantages of zirconia, machinable metals have
used clinically, has been shown to be robust, biocombeen developed.18 Titanium has been used as the main
patible, esthetically pleasing, and applicable to the CAD/
machinable metal,19,20 but bonding to a ceramic veneer is
CAM systems.12-17 Zirconia units cannot be connected
difcult due to the thick oxide layer.21-23 Thus, instead of
This work was partially supported by the Medical Devices Comparative Clinical and Performance Evaluation Program of the Korea Medical Devices
Industrial Cooperation Association (KMDICA) and the Basic Science Research Program through the National Research Foundation of Korea (NRF),
funded by the Ministry of Science, ICT, and Future Planning (NRF-2013R1A1A1076022).
a
Clinical Associate Professor, Department of Prosthodontics and Dental Research Institute, Seoul National University Gwanak Dental Hospital, Seoul, Korea.
b
Former resident, Department of Prosthodontics, School of Medicine, Ewha Womans University, Seoul, Korea.
c
Professor, Department of Prosthodontics, School of Medicine, Ewha Womans University, Seoul, Korea.
d
Professor, Department of Prosthodontics and Dental Research Institute, Seoul National University, Seoul, Korea.
e
Professor, Department of Dentistry, School of Medicine, Inha University, Incheon, Korea.
THE JOURNAL OF PROSTHETIC DENTISTRY
Volume
Clinical Implications
The marginal and internal ttings of machinable
Pd-Ag-In alloy crowns were comparable to those of
conventional cast and zirconia crowns.
titanium alloy, alloys of platinum group metals have been
used for xed prostheses and implant abutments.
Although the platinum metal alloys have been used in
conventional casting methods, their specic compositions differ from those of the conventional alloys if they
are manufactured for precision milling.24-26 If the weight
ratio of palladium (Pd) and indium (In) is adjusted, the
alloy has a gold-like color, excellent physical properties,
and adequate bond strength with ceramic. The machinable Pd-silver (Ag)-In alloy has a hardness of between
185 and 330 VHN, an elongation of 5%, a modulus of
elasticity of 80 GPa, and a bond strength with ceramic of
38 MPa.27 Moreover, it displays resistance to corrosion
and discoloration that is higher than the criteria for
clinical use.
For long-term success, prostheses made of a variety of
materials require appropriate marginal and internal
adaptation. Inappropriate margins may cause restoration
failure due to the accumulation of plaque and secondary
caries, and the excess or lack of space for the cement can
result in fracture, detachment, or incomplete placement.28,29 Many in vitro and in vivo studies have been
conducted on marginal and internal gaps.30-44 Although
a consensus has not yet been reached, a marginal gap of
100 to 120 mm and an internal gap of 140 to 150 mm are
recommended as the clinical upper limits for complete
crowns.38-40
A representative method for identifying the in vivo
marginal and internal ts is the replica technique, which
was described by Molin et al in 1993.45 This technique,
which duplicates the relationship of the inner space of a
crown and an abutment on a model with the registration
material, has a number of advantages. A crown does not
need to be sectioned, and the number of measurement
sites can be decided without restriction. In addition,
repeated measurements are possible. Consequently, this
method has been frequently used in in vitro and in vivo
studies.4,46-54
Most studies of the marginal accuracy of crowns have
examined CAD/CAM prostheses or compared cast alloy
crowns and CAD/CAM crowns.55-59 Few comparative
studies of the ts of Pd-Ag-In semiprecious metal
crowns, CAD/CAM zirconia crowns, and/or cast gold
alloy crowns have been conducted. Thus, in this study,
prostheses fabricated with gold alloy, zirconia, and PdAg-In alloy were provided for study participants, and
their marginal and internal ts were compared. The
THE JOURNAL OF PROSTHETIC DENTISTRY
Issue
primary null hypothesis was that the marginal t of the
semiprecious metal alloy crown was statistically noninferior to that of the zirconia and cast gold crowns. The
secondary null hypothesis was that the internal t of the
Pd-Ag-In alloy crown did not differ statistically from
those of the control groups.
MATERIAL AND METHODS
This study was approved by the Institutional Review
Board of Inha University and Ewha Womans University
Hospitals. The study participants were adults ranging
from 20 to 81 years of age who voluntarily consented to
enroll in this clinical trial. Individuals under the age of 20,
pregnant women or women suspected of being pregnant,
individuals with alcohol addiction or mental illness, and
individuals with abnormal clinical ndings that a study
supervisor or investigator considered inappropriate for
this study were excluded.
Prosthesis materials were gold alloy (DeguDent LTG;
DeguDent GmbH), zirconia (Lava; 3M ESPE), and blocktype Pd-Ag-In alloy (Innovium; Ceragem Biosys Co). The
gold alloy and zirconia were fabricated as controls, and
the Pd-Ag-In alloy was the experimental material. The
crown that was selected among the 3 by the participant
was cemented for the denitive prosthesis.
To determine the necessary number of participants,
differences in the marginal gaps of the matched pairs
were set as the primary evaluation variable. When the
actual differences and standard deviations of the differences in the marginal gaps of the Pd-Ag-In alloy crown
compared with the gold alloy and zirconia crowns of the 2
control groups were set to 0 mm and 63.7 mm, respectively,
the number of required participants was estimated to be
52 from a noninferiority test with a noninferiority margin
of 25 mm, a 1-sided alpha level of .025 and a power
of 80%.60,61 Fifty-two teeth (31 molars, 11 premolars,
2 canines, and 8 anterior teeth; 20 teeth in the maxilla and
32 in the mandible) in 35 participants (16 men and 19
women; average age, 46.7 years) who needed metal or
ceramic complete crown restorations because of tooth
damage such as dental caries or tooth fractures were
enrolled.
A denitive cast was produced for the tooth to be
treated according to the conventional restoration process
through tooth preparation and impression making. The
preparation design was for a ceramic restoration with
rounded line angles. The design of an equally placed
gingival nish line was the chamfer for the most part and
the deep chamfer for the esthetic areas. The denitive
stone cast underwent the die process and was then
scanned with a 3-dimensional model scanner (Dental
Wings 7Series; Dental Wings Inc) to generate a virtual
model. The gold alloy crown was fabricated by the conventional waxing, investment, wax elimination, and
Park et al
2015
Figure 1. Fabrication process of 3 types of crowns under same conditions. A, After preparing tooth, impression was made with elastomeric impression
material. B, Abutment tooth was scanned with desktop scanner after cast sectioning. C, Wax pattern was made by skilled technician and scanned to
make shape of crowns identical. D, Crown was fabricated by superimposing wax pattern scan on abutment with double scan technique.
casting processes. For the fabrication of the zirconia and
Pd-Ag-In alloy crowns, a double scanning method was
used. The waxing that was made for the cast gold crown
was scanned 3 dimensionally, and the scan was superimposed on the existing cast and applied as the contour
and morphology of the Pd-Ag-In alloy crown.62,63 This
method was used to exclude variables other than the
marginal and internal t. For crowns in the esthetic area,
a veneering ceramic was applied on the labial surface
with a conventional layering technique. The marginal
and internal cement space parameters and the minimum
core thickness of both the Lava and Innovium crowns
were set in the CAD program at 35 mm, 70 mm, and 0.5
mm, respectively (Fig. 1). Based on the completed design,
the Innovium alloy and Lava zirconia blocks were processed and nished with a milling machine (Dento Mc5AX; Digiworks), and the Lava zirconia blocks were
processed with a Lava CNC 500 (3M).
The replica technique was used to examine the marginal and internal t.41 The 3 types of completed crowns
were evaluated separately on the abutment tooth. The
proximal contact, margin, and occlusion were evaluated.
After an initial adjustment, the intaglio surface of the
Park et al
crown was lled with a silicone registration material (Fit
Checker II; GC Corp), and the crown was placed on the
prepared tooth. The patient was instructed to clench their
teeth on a gauze wrapped stick placed on the occlusal
surface. After 2 minutes for polymerization, the crown
was removed from the oral cavity, and the registration
material was assessed for bubbles or tears. Subsequently,
the intaglio was lled with a polyvinyl siloxane impression material (Examixne; GC Corp), and the base was
supplemented with a putty silicone (Exaex; GC Corp)
and stabilized, which yielded a replica (Fig. 2). Among
the 3 types of complete crowns, the crown that was
selected by the patient was delivered with resin-modied
glass ionomer cement (FujiCEM; GC Corp).
The molar was sectioned twice, and the premolar and
canine were sectioned once from the center in the buccolingual direction to obtain cross-sections to visualize the
gaps between the crown and the tooth. In the mesiodistal
direction, all teeth were cut from the center. Four regions
were selected as reference points for the measurements of
the marginal and internal gaps. For the measurement of
the gaps in each sectioned part, images were made with a
stereoscopic microscope (SZX7; Olympus Corp) at 30
THE JOURNAL OF PROSTHETIC DENTISTRY
Volume
Issue
Figure 2. Replica technique procedure to measure internal t of crowns. A, Internal gaps of crowns in 3 groups were made with silicone registration
material under same condition. B, Replica was prepared by stabilizing volume of registration material with silicone material with different color.
magnication, and images were analyzed with image
analysis software (ImageJ version 1.45 software; US National Institutes of Health). A laboratory technician, who
did not participate in the clinical process, performed the
measurement (Fig. 3). The dental laboratory processes
were evaluated by comparing the t on a cast, shape
reproducibility, level of oxide layer formation, bubbles
during the opaque application, properties and deformation
level of the surface, deformation level after ceramic
veneering, and satisfaction with ceramic shades relative to
each material.
Measurements from the replica specimen were
analyzed with statistical software (SAS v9.2; SAS Institute, Inc). Comparisons of the noninferiority of the
margins between the experimental group with crowns
that were prepared by milling the Pd-Ag-In alloy block
and the control groups of the cast and zirconia crowns
were performed as the primary end point. If the upper
limit of the 95% condence interval (CI) of the gap difference between the 2 groups was less than the prespecied noninferiority margin of 25 mm, the Pd-Ag-In
alloy group was considered noninferior to the gold or
zirconia group at a 1-sided alpha level of .025. The same
method and criteria were applied for the values of 6
sections from different locations. The results of the survey
of the evaluations of the laboratory procedure were
analyzed by obtaining the average ranking from the
rankings for each of the respective items.
Pd-Ag-In alloy crowns and the 2 control groups did not
exceed the noninferiority margin of 25 mm. However, in
the distal section, the marginal gap was larger in the PdAg-In alloy group (84.5 mm) than those in the gold group
(67.9 mm, P=.002) and the zirconia group (69.8 mm,
P=.01). The difference in the marginal gap between the
experimental group and the gold group was 16.6 mm
(95% condence limits [CL]: 6.3, 26.9 mm) and that between the experimental group and the zirconia group
was 14.7 mm (95% CL: 3.4, 26 mm). Thus, the criterion for
noninferiority was not met in the distal sections (Fig. 4).
At the axial wall, the gap difference between the gold
alloy and the Pd-Ag-In alloy crowns was 11.9 mm (95%
CL: 2.4, 26.2 mm). At the mesiobuccal section, the gap
differences were 26 mm (95% CL: 10.2, 41.7 mm) between
the gold and Pd-Ag-In crowns and 18.8 mm (95% CL:
1.9, 35.7 mm) between the zirconia and Pd-Ag-In alloy
crowns. These differences did not meet the noninferiority
criteria. However, in the remaining 4 sections, the upper
limit of the CL did not exceed the noninferiority margin
(Fig. 5). For the line angle and occlusal space, the size of
the internal gaps of the experimental group did not meet
the noninferiority criteria in comparison with the gold
alloy and zirconia crowns in all of the sections (Figs. 6-8).
In the evaluations of the fabrication procedures of the
crowns in the dental laboratory, the zirconia crown displayed the best overall results for all of the items,
including the model t and bubble formation during the
opaque application (Table 2).
RESULTS
The average marginal gap measured on the silicone
replica of the cast gold crowns was 68.2 m m, 75.4 mm for
the zirconia crowns, and 76.9 mm for the Pd-Ag-In alloy
crowns. The average internal gaps at the margin, axial
wall, line angle, and occlusal space are shown in
Table 1. In the 5 sections other than the distal section of
the margin, the differences in the gaps between the
THE JOURNAL OF PROSTHETIC DENTISTRY
DISCUSSION
In an in vitro study that compared the t of different
crowns fabricated with the CAD/CAM system under the
same conditions, Gonzalo et al35 reported that, in 3-unit
partial xed dental prostheses made of Lava, Procera zirconia, InCeram zirconia, and metal ceramic, the rst 3
groups showed smaller marginal gaps than metal ceramic.
Park et al
2015
Mp - Mz
Distal
Mesial
Distolingual
Distobuccal
Mesiolingual
30.0
Location
Figure 4. Two-sided 95% CI of gap differences at margin. Blue dotted
line denotes noninferiority margin (25 mm). MP, machined group of PdAg-In alloy; MZ, machined group of zirconia.
In addition, Baig et al55 reported that the marginal gaps
were 66.4 mm for the Cercon system and 36.6 mm for the
IPS Empress II system, both made with the CAD/CAM
method, and 37.1 mm for a cast complete metal crown. In
an in vivo study that was conducted on 19 participants,
Park et al
5.0
5.0
15.0
Mp - Gold
25.0
Mp - Mz
35.0
Distal
Mp - Gold
20.0
15.0
Mesial
10.0
Distolingual
0.0
25.0
Distobuccal
10.0
35.0
Mesiolingual
20.0
45.0
Mesiobuccal
Two-Sided 95% CI of Gap Difference
at Axial Wall (m)
30.0
Mesiobuccal
Two-Sided 95% CI of Gap Difference
at Margin (m)
Figure 3. Cross-section view of each area to measure marginal and internal gaps in silicone replica after mesiodistal and buccolingual sectioning (30
magnication). A, Margin. B, Axial wall. C, Line angle. D, Occlusal space.
Location
Figure 5. Two-sided 95% CI of gap differences at axial wall.
Reich et al50 reported that the marginal gaps of the Lava
and Cerec systems were both approximately 65 mm, which
was not signicantly different from the 54 mm for the
metal ceramic crown. Wettstein et al51 reported that, when
the Cercon zirconia framework and conventional metal
ceramic framework were selectively fabricated for 25 participants, the internal ts of the zirconia framework were
cervical, 189.6 mm; axial, 140.5 mm; occlusal cusp tip, 121.3
THE JOURNAL OF PROSTHETIC DENTISTRY
Volume
15.0
5.0
5.0
Distal
Mesial
Distolingual
Distobuccal
Mesiolingual
15.0
Location
Figure 6. Two-sided 95% CI of gap differences at line angles.
55.0
35.0
*
15.0
5.0
25.0
Distal
Mesial
25.0
Distolingual
35.0
75.0
Distobuccal
45.0
Mp - Mz
Mesiolingual
Mp - Mz
55.0
Issue
Mp - Gold
95.0
Mesiobuccal
Mp - Gold
65.0
Two-Sided 95% CI of Gap Difference
at Occlusal Space (m)
75.0
Mesiobuccal
Two-Sided 95% CI of Gap Difference
at Line Angle (m)
Location
Figure 7. Two-sided 95% CI of gap differences at occlusal spaces.
mm, and centro-occlusal, 192.0 mm; these values were
signicantly greater than those of the metal ceramic
framework, which were 118.6 mm, 95.7 mm, 122.5 mm, and
153.1 mm. Thus, in most studies, the crowns fabricated
with the CAD/CAM method were comparable with metal
ceramic or complete-metal crowns that were made by
casting and had marginal and internal ts that were within
the clinically acceptable range.21,38,44,52 In addition, Tan
et al59 compared the vertical margin openings of titanium
crowns that were designed by CAD software, milled titanium crowns that were waxed followed by double scanning with a 3-dimensional scanner, and cast high noble
crowns. The marginal discrepancies were 79 mm, 73 mm,
and 24 mm, respectively. In addition, the CAD/CAM
method with and without double scanning did not show
signicantly different marginal gaps.
In this in vivo study, the rst null hypothesis was
rejected because the crown that was fabricated by
milling the Pd-Ag-In alloy block showed a marginal t
on the distal cross-section of the crown that was inferior to that of the cast crowns and zirconia crowns.
However, the marginal gap of the Pd-Ag-In alloy crown
was not statistically inferior to those of the control
groups on all of the cross-sections except for the distal
section. The average marginal gaps of the cast crowns
(68.2 mm), zirconia crowns (75.4 mm), and Pd-Ag-In
alloy crowns (76.9 mm) were generally greater
compared with the results of previous in vivo studies.55-58
In contrast, other in vivo studies have reported larger
marginal gaps than those found in our study.50,51 In
addition, the marginal gap (84.5 mm) of the distal section
was statistically inferior to the 120 mm that was proposed as the clinically acceptable gap by Hung et al,38
indicating that the Pd-Ag-In alloy crown had a clinically
applicable t. The differences in the internal gaps at the
axial wall between the Pd-Ag-In group and the control
groups exceeded the noninferiority margin at the mesial
section (100.8 mm) and mesiobuccal section (103.1 mm).
THE JOURNAL OF PROSTHETIC DENTISTRY
However, similar to the marginal gap, all of the internal
gaps obtained in this study showed values less than 140 to
150 mm.
For the line angle and occlusal space, the second null
hypothesis was rejected because the Pd-Ag-In alloy
crown showed larger internal gaps in all of the cross
sections compared with the control groups. Both the PdAg-In alloy and zirconia crowns had signicantly greater
internal gaps in the occlusal space compared with the
cast crowns. This was likely a result of the characteristics
of the CAD/CAM fabrication method, such as the limited
size of the milling tool and tool compensation.64 In
addition, some crowns have their internal spacer parameters set to be bigger in the CAD system to avoid
early contact on the sharp edge of a preparation and to
reduce the marginal gap. Therefore, the gap might
become larger in the CAD process compared with a cast
restoration.56,65
The larger gap in the line angle and the occlusal space
of the Pd-Ag-In alloy crown compared with the zirconia
crown from the same CAD/CAM method was thought to
result from differences in the gaps that might have
occurred as a result of the parameters set during milling
because of the difference between zirconia, which has
volume reduction during the sintering process, and the
Pd-Ag-In alloy, which has no volume change. For the
general procedures for crowns in the dental laboratory
evaluations, the zirconia crowns appeared to be the
easiest to fabricate. However, this was thought to be
because of skill differences, and the fabrication and
placement of the gold or Pd-Ag-In alloy crowns was not
exceptionally difcult.
The methods that are used to evaluate the t of a
crown include direct visualization under a microscope,
visualization by the attachment of the crown to a die that
is followed by sectioning, evaluation after impression
making, and evaluation with an explorer and the naked
eye.66,67 This in vivo study used the replica technique
Park et al
2015
A deep chamfer nish line was prepared for the labial
or buccal side of the incisors, canines, and premolars,
while a conventional chamfer margin was prepared for
the remaining margin. Syu et al68 suggested that the type
of nish line does not affect the marginal gap. In addition, the preparation design may not result in signicant
differences between the t of the cast crowns and CAD/
CAM crowns.69,70
The analysis in this clinical study indicated that the
marginal and internal ts of the crowns fabricated by
milling machining Pd-Ag-In semiprecious metal alloys
were comparable with those of the conventionally used
cast crowns and zirconia crowns. Although the Pd-Ag-In
crowns did not meet the noninferiority criterion
compared with the existing materials for the line angle
and occlusal space, their values were within the clinically
acceptable range. Furthermore, most areas of the marginal and axial locations met the noninferiority criterion.
However, because this study had a small sample size and
a short period for crown placement, long-term clinical
studies that involve a larger sample are required. In
addition, studies on possible events in the oral cavity,
such as antagonistic tooth wear or fracture, chipping of
the ceramic veneer, and methods of fabricating more
precise crowns through improvements of the CAD/CAM
technique are necessary.
CONCLUSIONS
Within the limitations of this in vivo study, the following
conclusions may be drawn.
1. The average standard deviation marginal gaps
were 68.2 24.8 mm for the cast gold crowns, 75.4
28.8 mm for the zirconia crowns, and 76.9 27.0
mm for the Pd-Ag-In alloy crowns. The Pd-Ag-In
alloy crowns met the noninferiority criterion in all
the areas, except for the distal cross-section,
compared with the control groups.
2. For the line angle and occlusal space, the Pd-Ag-In
alloy crowns were inferior to the control groups for
the internal gaps.
Figure 8. Representative silicone replicas of internal gaps of crowns
evaluated. A, Gold alloy group. B, Zirconia group. C, Pd-Ag-In alloy group.
(30 magnication).
which duplicated the state of the abutment because
directly cutting the patients tooth was not possible.45 No
signicant differences have been reported between the die
sectioning method and replica technique, and these results
were not affected by the type of silicone registration material.53,54 Although the replica was prepared using the
maximum clenching force of a patient, the replica may not
have reected the precise positions, possibly increasing
the standard deviation of the occlusal space.
Park et al
REFERENCES
1. Fasbinder DJ. Clinical performance of chairside CAD/CAM restorations. J Am
Dent Assoc 2006;137:22S-31S.
2. Mormann WH, Brandestini M, Lutz F, Barbakow F. Chairside computeraided direct ceramic inlays. Quintessence Int 1989;20:329-39.
3. Bindl A, Mormann WH. Fit of all-ceramic posterior xed partial denture
frameworks in vitro. Int J Periodontics Restorative Dent 2007;27:567-75.
4. Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ. Marginal t
of alumina-and zirconia-based xed partial dentures produced by a CAD/
CAM system. Oper Dent 2001;26:367-74.
5. Williams RJ, Bibb R, Eggbeer D. CAD/CAM in the fabrication of removable
partial denture frameworks: a virtual method of surveying 3D scanned dental
casts. Quint J Dent Technol 2004;2:268-76.
6. Sun Y, Lu P, Wang Y. Study on CAD&RP for removable complete denture.
Comput Methods Programs Biomed 2009;93:266-72.
7. Williams RJ, Bibb R, Eggbeer D, Collis J. Use of CAD/CAM technology to
fabricate a removable partial denture framework. J Prosthet Dent 2006;96:
96-9.
THE JOURNAL OF PROSTHETIC DENTISTRY
8. Andersson M, Razzoog ME, Oden A, Hegenbarth EA, Lang BR. Procera: a
new way to achieve an all-ceramic crown. Quintessence Int 1998;29:285-96.
9. Kapos T, Evans C. CAD/CAM technology for implant abutments, crowns,
and superstructures. Int J Oral Maxillofac Implants 2014;29 Suppl:117-36.
10. Luthardt RG, Sandkuhl O, Herold V, Walter MH. Accuracy of mechanical
digitizing with a CAD/CAM system for xed restorations. Int J Prosthodont
2001;14:146-51.
11. McLaren EA, Terry DA. CAD/CAM systems, materials, and clinical guidelines
for all-ceramic crowns and xed partial dentures. Compend Contin Educ
Dent 2002;23:637-41. 44, 46 passim; quiz 54.
12. Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials
1999;20:1-25.
13. Tinschert J, Zwez D, Marx R, Anusavice KJ. Structural reliability of alumina-,
feldspar-, leucite-, mica- and zirconia-based ceramics. J Dent 2000;28:529-35.
14. Ardlin BI. Transformation-toughened zirconia for dental inlays, crowns and
bridges: chemical stability and effect of low-temperature aging on exural
strength and surface structure. Dent Mater 2002;18:590-5.
15. Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness
and microstructure of a selection of all-ceramic materials. Part II. Zirconiabased dental ceramics. Dent Mater 2004;20:449-56.
16. Raigrodski AJ. Contemporary materials and technologies for all-ceramic xed
partial dentures: a review of the literature. J Prosthet Dent 2004;92:557-62.
17. Tinschert J, Natt G, Hassenpug S, Spiekermann H. Status of current CAD/
CAM technology in dental medicine. Int J Comput Dent 2004;7:25-45.
18. Lee DH, Lee BJ, Kim SH, Lee KB. Shear bond strength of porcelain to a new
millable alloy and a conventional castable alloy. J Prosthet Dent 2015;113:
329-35.
19. Abduo. Fit of CAD/CAM implant frameworks: a comprehensive review.
J Oral Implantol 2014 Dec;40(6):758-66.
20. Kapos T, Ashy LM, Gallucci GO, Weber HP, Wismeijer D. Computer-aided
design and computer-assisted manufacturing in prosthetic implant dentistry.
Int J Oral Maxillofac Implants 2009;24:110-7.
21. Boening KW, Walter MH, Reppel PD. Non-cast titanium restorations in xed
prosthodontics. J Oral Rehabil 1992;19:281-7.
22. Gilbert JL, Covey DA, Lautenschlager EP. Bond characteristics of porcelain
fused to milled titanium. Dent Mater 1994;10:134-40.
23. Walter M, Boning K, Reppel PD. Clinical performance of machined titanium
restorations. J Dent 1994;22:346-8.
24. Goodacre CJ. Palladium-silver alloys: a review of the literature. J Prosthet
Dent 1989;62:34-7.
25. Huget EF, Civjan S. Status report on palladium-silver-based crown and
bridge alloys. J Am Dent Assoc 1974;89:383-5.
26. Kansu G, Aydin AK. Evaluation of the biocompatibility of various dental
alloys: Part 2eAllergenical potentials. Eur J Prosthodont Restor Dent 1996;4:
155-61.
27. Hong JT, Shin SY. A comparative study on the bond strength of porcelain to
the millingable Pd-Ag alloy. J Adv Prosthodont 2014;6:372-8.
28. Sorensen JA. A rationale for comparison of plaque-retaining properties of
crown systems. J Prosthet Dent 1989;62:264-9.
29. Sorensen SE, Larsen IB, Jorgensen KD. Gingival and alveolar bone reaction
to marginal t of subgingival crown margins. Scand J Dent Res 1986;94:
109-14.
30. Assif D, Rimer Y, Aviv I. The ow of zinc phosphate cement under a fullcoverage restoration and its effect on marginal adaptation according to the
location of cement application. Quintessence Int 1987;18:765-74.
31. Bader JD, Rozier RG, McFall WT Jr, Ramsey DL. Effect of crown margins on
periodontal conditions in regularly attending patients. J Prosthet Dent
1991;65:75-9.
32. Belser UC, MacEntee MI, Richter WA. Fit of three porcelain-fused-to-metal
marginal designs in vivo: a scanning electron microscope study. J Prosthet
Dent 1985;53:24-9.
33. Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in vivo crown
margin discrepancies on periodontal health. J Prosthet Dent 1991;65:357-64.
34. Fusayama T, Ide K, Hosoda H. Relief of resistance of cement of full cast
crowns. J Prosthet Dent 1964;14:95-106.
35. Gonzalo E, Suarez MJ, Serrano B, Lozano JF. Marginal t of Zirconia posterior xed partial dentures. Int J Prosthodont 2008;21:398-9.
36. Grasso JE, Nalbandian J, Sanford C, Bailit H. Effect of restoration quality on
periodontal health. J Prosthet Dent 1985;53:14-9.
37. Grey NJ, Piddock V, Wilson MA. In vitro comparison of conventional crowns
and a new all-ceramic system. J Dent 1993;21:47-51.
38. Hung SH, Hung KS, Eick JD, Chappell RP. Marginal t of porcelain-fusedto-metal and two types of ceramic crown. J Prosthet Dent 1990;63:26-31.
39. McLean JW, von Fraunhofer JA. The estimation of cement lm thickness by
an in vivo technique. Br Dent J 1971;131:107-11.
40. Palomo F, Peden J. Periodontal considerations of restorative procedures.
J Prosthet Dent 1976;36:387-94.
41. Passon C, Lambert RH, Lambert RL, Newman S. The effect of multiple layers
of die-spacer on crown retention. Oper Dent 1992;17:42-9.
42. Schwartz NL, Whitsett LD, Berry TG, Stewart JL. Unserviceable crowns and
xed partial dentures: life-span and causes for loss of serviceability. J Am
Dent Assoc 1970;81:1395-401.
THE JOURNAL OF PROSTHETIC DENTISTRY
Volume
Issue
43. Walton JN, Gardner FM, Agar JR. A survey of crown and xed partial denture
failures: length of service and reasons for replacement. J Prosthet Dent
1986;56:416-21.
44. Christensen GJ. Marginal t of gold inlay castings. J Prosthet Dent 1966;16:
297-305.
45. Molin M, Karlsson S. The t of gold inlays and three ceramic inlay systems. A
clinical and in vitro study. Acta Odontol Scand 1993;51:201-6.
46. Boening KW, Wolf BH, Schmidt AE, Kastner K, Walter MH. Clinical t of
Procera AllCeram crowns. J Prosthet Dent 2000;84:419-24.
47. Coli P, Karlsson S. Fit of a new pressure-sintered zirconium dioxide coping.
Int J Prosthodont 2004;17:59-64.
48. Kohorst P, Brinkmann H, Dittmer MP, Borchers L, Stiesch M. Inuence of
the veneering process on the marginal t of zirconia xed dental prostheses.
J Oral Rehabil 2010;37:283-91.
49. Reich S, Kappe K, Teschner H, Schmitt J. Clinical t of four-unit zirconia
posterior xed dental prostheses. Eur J Oral Sci 2008;116:579-84.
50. Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical t of all-ceramic
three-unit xed partial dentures, generated with three different CAD/CAM
systems. Eur J Oral Sci 2005;113:174-9.
51. Wettstein F, Sailer I, Roos M, Hammerle CH. Clinical study of the internal
gaps of zirconia and metal frameworks for xed partial dentures. Eur J Oral
Sci 2008;116:272-9.
52. Fransson B, Oilo G, Gjeitanger R. The t of metal-ceramic crowns, a clinical
study. Dent Mater 1985;1:197-9.
53. Rahme HY, Tehini GE, Adib SM, Ardo AS, Rifai KT. In vitro evaluation of the
replica technique in the measurement of the t of Procera crowns.
J Contemp Dent Pract 2008;9:25-32.
54. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal
t of cast crownsevalidation of the silicone replica method. J Oral Rehabil
2008;35:116-22.
55. Baig MR, Tan KB, Nicholls JI. Evaluation of the marginal t of a zirconia
ceramic computer-aided machined (CAM) crown system. J Prosthet Dent
2010;104:216-27.
56. Bindl A, Mormann WH. Marginal and internal t of all-ceramic CAD/CAM
crown-copings on chamfer preparations. J Oral Rehabil 2005;32:441-7.
57. Hertlein GHS, Frank S, Suttor D. Marginal t of CAD/CAM manufactured all
ceramic prosthesis. J Dent Res 2001;80:42-4.
58. May KB, Russell MM, Razzoog ME, Lang BR. Precision of t: the Procera
AllCeram crown. J Prosthet Dent 1998;80:394-404.
59. Tan PL, Gratton DG, Diaz-Arnold AM, Holmes DC. An in vitro comparison
of vertical marginal gaps of CAD/CAM titanium and conventional cast restorations. J Prosthodont 2008;17:378-83.
60. Kokubo Y, Tsumita M, Kano T, Sakurai S, Fukushima S. Clinical marginal and
internal gaps of zirconia all-ceramic crowns. J Prosthodont Res 2011;55:40-3.
61. Chow SC, Shao J, Wang H. Sample size calculations in clinical research. 2nd
ed. Boca Raton, FL: Chapman and Hall/CRC; 2007.
62. Beuer F, Stimmelmayr M, Gueth JF, Edelhoff D, Naumann M. In vitro performance of full-contour zirconia single crowns. Dent Mater 2012;28:449-56.
63. Kollar A, Huber S, Mericske E, Mericske-Stern R. Zirconia for teeth and
implants: a case series. Int J Periodontics Restorative Dent 2008;28:479-87.
64. Sturdevant JR, Bayne SC, Heymann HO. Margin gap size of ceramic inlays
using second-generation CAD/CAM equipment. J Esthet Dent 1999;11:
206-14.
65. Bornemann G, Lemelson S, Luthardt R. Innovative method for the analysis
of the internal 3D tting accuracy of Cerec-3 crowns. Int J Comput Dent
2002;5:177-82.
66. Sorensen JA. A standardized method for determination of crown margin delity. J Prosthet Dent 1990;64:18-24.
67. Holmes JR, Bayne SC, Holland GA, Sulik WD. Considerations in measurement of marginal t. J Prosthet Dent 1989;62:405-8.
68. Syu JZ, Byrne G, Laub LW, Land MF. Inuence of nish-line geometry on
the t of crowns. Int J Prosthodont 1993;6:25-30.
69. Tsitrou EA, Northeast SE, van Noort R. Evaluation of the marginal t of three
margin designs of resin composite crowns using CAD/CAM. J Dent 2007;35:
68-73.
70. Ayad MF. Effect of the crown preparation margin and die type on the marginal accuracy of ber-reinforced composite crowns. J Contemp Dent Pract
2008;9:9-16.
Corresponding author:
Dr Namsik Oh
Inha University, 7-206
#3 Shinhung-dong, Jung-gu
Incheon, 400-711
REPUBLIC OF KOREA
Email: onsdo@inha.ac.kr
Acknowledgments
The authors thank Dr Kyoung-Ae Kong for performing statistical analyses in this
study.
Copyright 2015 by the Editorial Council for The Journal of Prosthetic Dentistry.
Park et al
You might also like
- Mandibular Expansion AppliancesDocument9 pagesMandibular Expansion AppliancesGeorgiana BlagociNo ratings yet
- 3M Oral Care Impression Procedure GuideDocument123 pages3M Oral Care Impression Procedure GuideGeorgiana BlagociNo ratings yet
- Piis0889540617303475 PDFDocument2 pagesPiis0889540617303475 PDFModit GuptaNo ratings yet
- Evaluation of Two Different Bonding Materials For Orthodontic Retention TreatmentDocument22 pagesEvaluation of Two Different Bonding Materials For Orthodontic Retention TreatmentGeorgiana BlagociNo ratings yet
- Paradigm Shift in The Treatment of Class-II Malocclusions in Children and AdolescentsDocument31 pagesParadigm Shift in The Treatment of Class-II Malocclusions in Children and AdolescentsGeorgiana BlagociNo ratings yet
- Denture StomatitisDocument5 pagesDenture Stomatitissarah wilderNo ratings yet
- Methods of Data Collection in Qualitative Research: Interviews and Focus GroupsDocument6 pagesMethods of Data Collection in Qualitative Research: Interviews and Focus GroupsGeorgiana BlagociNo ratings yet
- Background: Surveys Are Becoming of Frequent Use in The Field of Healthcare and Health-RelatedDocument10 pagesBackground: Surveys Are Becoming of Frequent Use in The Field of Healthcare and Health-RelatedGeorgiana BlagociNo ratings yet
- Clinical Manifestation, DiagnosisDocument13 pagesClinical Manifestation, DiagnosisGeorgiana BlagociNo ratings yet
- Denture StomatitisDocument5 pagesDenture Stomatitissarah wilderNo ratings yet
- The Novel Coronavirus SARSDocument8 pagesThe Novel Coronavirus SARSGeorgiana BlagociNo ratings yet
- Errors in Survey Research and Their Threat To Validity and ReliabilityDocument9 pagesErrors in Survey Research and Their Threat To Validity and ReliabilityGeorgiana BlagociNo ratings yet
- Lista SindroameDocument1 pageLista SindroameGeorgiana BlagociNo ratings yet
- Errors in Survey Research and Their Threat To Validity and ReliabilityDocument9 pagesErrors in Survey Research and Their Threat To Validity and ReliabilityGeorgiana BlagociNo ratings yet
- Vesiculobullous LesionsDocument37 pagesVesiculobullous LesionsGeorgiana BlagociNo ratings yet
- Autoimmune Vesiculo Bullous LesionsDocument31 pagesAutoimmune Vesiculo Bullous LesionsGeorgiana BlagociNo ratings yet
- Winter2016microscopes PDFDocument8 pagesWinter2016microscopes PDFGeorgiana BlagociNo ratings yet
- EndodonticsDocument206 pagesEndodonticssomebody_ma90% (10)
- Color Atlas of EndoDocument203 pagesColor Atlas of Endooana_en100% (23)
- 1-Zirconia An Up-Date Review Litrature - Docx Virayesh AkharDocument15 pages1-Zirconia An Up-Date Review Litrature - Docx Virayesh AkharteertheshNo ratings yet
- 1-Zirconia An Up-Date Review Litrature - Docx Virayesh AkharDocument15 pages1-Zirconia An Up-Date Review Litrature - Docx Virayesh AkharteertheshNo ratings yet
- Manifest Symptomatology of Depression in AdultsDocument92 pagesManifest Symptomatology of Depression in AdultsGeorgiana BlagociNo ratings yet
- Biological Theories of DepressionDocument41 pagesBiological Theories of DepressionGeorgiana BlagociNo ratings yet
- Aesthetic Clasp Design For Removable Partial Dentures A Litewrature ReviewDocument5 pagesAesthetic Clasp Design For Removable Partial Dentures A Litewrature Reviewpablogdv956100% (1)
- Pain Management SHORTENEDDocument2 pagesPain Management SHORTENEDIngerul20022No ratings yet
- 608671Document11 pages608671Georgiana BlagociNo ratings yet
- Autoimmune Vesiculo Bullous LesionsDocument31 pagesAutoimmune Vesiculo Bullous LesionsGeorgiana BlagociNo ratings yet
- An IV 2013-2014Document16 pagesAn IV 2013-2014Georgiana BlagociNo ratings yet
- Study Skills HandoutDocument2 pagesStudy Skills HandoutGeorgiana BlagociNo ratings yet
- Standards For The Dental TeamDocument98 pagesStandards For The Dental TeamTy ChiewNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Characterization of Chemically Treated Limonia Acidissima Wood Apple Shell Powder Physicochemical Thermal and Morphological PropertiesDocument12 pagesCharacterization of Chemically Treated Limonia Acidissima Wood Apple Shell Powder Physicochemical Thermal and Morphological PropertiesSharath P CNo ratings yet
- SHC Polyrex 100 Electric Motor Synthetic Grease - MobilDocument2 pagesSHC Polyrex 100 Electric Motor Synthetic Grease - MobilAnibal RiosNo ratings yet
- Machine Guarding PDFDocument133 pagesMachine Guarding PDFbrsharmaNo ratings yet
- 6 - Geomembrane Lifetime Prediction PDFDocument27 pages6 - Geomembrane Lifetime Prediction PDF齐左No ratings yet
- On Wire IndustryDocument47 pagesOn Wire IndustryAjit SharmaNo ratings yet
- ME136P-2 Experiment 1.2 AporaDocument7 pagesME136P-2 Experiment 1.2 AporaErol Josef AporaNo ratings yet
- Catalog Aer Condiționat Split Inverter SAMSUNG-2014Document17 pagesCatalog Aer Condiționat Split Inverter SAMSUNG-2014georgianconstantinNo ratings yet
- Datasheet SKHI 22A PDFDocument12 pagesDatasheet SKHI 22A PDFGlauber GoncalvesNo ratings yet
- Plant Commissioning & Start Up ProcedureDocument18 pagesPlant Commissioning & Start Up Procedureaamirapi100% (7)
- Iso 2528Document8 pagesIso 2528nisa nurhidayatiNo ratings yet
- 5-3 CLEAL Porousfine PP (English) JH-35302116Document2 pages5-3 CLEAL Porousfine PP (English) JH-35302116Milimas Tirta SolusiNo ratings yet
- DielectricResonatortype A4Document2 pagesDielectricResonatortype A4denivaldo2009No ratings yet
- ReddyheaterDocument268 pagesReddyheaterstraffer1No ratings yet
- The World of Chemistry Video Guide SetDocument10 pagesThe World of Chemistry Video Guide SetrkvNo ratings yet
- Chapter 11 - Industry and ManufacturingDocument36 pagesChapter 11 - Industry and ManufacturingNolan NelsonNo ratings yet
- C10129004 PDFDocument20 pagesC10129004 PDFChristopherNo ratings yet
- Standard BS 1042 - Part 1 - 1964Document116 pagesStandard BS 1042 - Part 1 - 1964MPChethan100% (2)
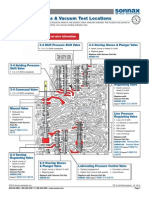
- 722 6 VacTestLocationsDocument4 pages722 6 VacTestLocationsUrszula WalczewskaNo ratings yet
- Borgianni, de Filippis - Gasification Process of Wastes Containing PVCDocument7 pagesBorgianni, de Filippis - Gasification Process of Wastes Containing PVCJorge VeraNo ratings yet
- MIL-F-5509D - Fittings, Flared Tube, Fluid ConnectionDocument18 pagesMIL-F-5509D - Fittings, Flared Tube, Fluid ConnectionthomasNo ratings yet
- Gates: Conventional Flap GateDocument8 pagesGates: Conventional Flap GateprasenjitsayantanNo ratings yet
- Physics Planning Practice 4Document4 pagesPhysics Planning Practice 4Michael LeungNo ratings yet
- Vice President Operations in Somerville NJ Resume Vasu MohanDocument3 pagesVice President Operations in Somerville NJ Resume Vasu MohanVasumohanNo ratings yet
- Parker FittingsDocument62 pagesParker FittingsIacob Cozonac100% (1)
- Cantilever Calculation ToolDocument10 pagesCantilever Calculation ToolEnoch Twumasi50% (2)
- 6 Big Losses in Manufacturing-2Document3 pages6 Big Losses in Manufacturing-2izzudinrozNo ratings yet
- Emissivity TableDocument13 pagesEmissivity TableUtubesNo ratings yet
- Codigos FordDocument66 pagesCodigos FordavffNo ratings yet
- Chapter 11: Transformation in AlloysDocument48 pagesChapter 11: Transformation in AlloysbadaboyNo ratings yet
- Zinc Oxide Powder & DispersionDocument5 pagesZinc Oxide Powder & DispersionAfdilah IrawatiNo ratings yet