Professional Documents
Culture Documents
CTNeoBC Pooled Analysis
Uploaded by
tabaresgonzaloCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CTNeoBC Pooled Analysis
Uploaded by
tabaresgonzaloCopyright:
Available Formats
Articles
Pathological complete response and long-term clinical
benet in breast cancer: the CTNeoBC pooled analysis
Patricia Cortazar, Lijun Zhang, Michael Untch, Keyur Mehta, Joseph P Costantino, Norman Wolmark, Herv Bonnefoi, David Cameron,
Luca Gianni, Pinuccia Valagussa, Sandra M Swain, Tatiana Prowell, Sibylle Loibl, D Lawrence Wickerham, Jan Bogaerts, Jose Baselga,
Charles Perou, Gideon Blumenthal, Jens Blohmer, Eleftherios P Mamounas, Jonas Bergh, Vladimir Semiglazov, Robert Justice, Holger Eidtmann,
Soonmyung Paik, Martine Piccart, Rajeshwari Sridhara, Peter A Fasching, Leen Slaets, Shenghui Tang, Bernd Gerber, Charles E Geyer Jr,
Richard Pazdur, Nina Ditsch, Priya Rastogi, Wolfgang Eiermann, Gunter von Minckwitz
Summary
Lancet 2014; 384: 16472
Published Online
February 14, 2014
http://dx.doi.org/10.1016/
S0140-6736(13)62422-8
See Comment page 115
US Food and Drug
Administration, Silver Spring,
MD, USA (P Cortazar MD,
L Zhang PhD, T Prowell MD,
G Blumenthal MD, R Justice MD,
R Sridhara PhD, S Tang PhD,
R Pazdur MD); HELIOS Klinikum,
Berlin, Germany
(Prof M Untch MD); German
Breast Group, Neu-Isenburg,
Germany (K Mehta MBA,
Prof S Liobl MD,
Prof G von Minckwitz MD);
National Surgical Adjuvant
Breast and Bowel Project,
Pittsburgh, PA, USA
(J P Costantino DrPH,
N Wolmark MD,
D L Wickerham MD, S Paik MD,
P Rastogi MD); Institut
Bergoni INSERM U916 and
Universit Bordeaux Segalen,
Bordeaux, France
(Prof H Bonnefoi MD);
Edinburgh Cancer Research
Centre, University of
Edinburgh and NHS Lothian,
UK (Prof D Cameron MD);
San Raaele Scientic
Institute, Milan, Italy
(Prof L Gianni MD); Fondazione
Michelangelo, Milan, Italy
(P Valagussa BS); Medstar
Washington Hospital Center,
Washington, DC, USA
(S M Swain MD); EORTC
Headquarters, Brussels,
Belgium (J Bogaerts PhD,
L Slaets PhD); Memorial
Sloan-Kettering Cancer Center,
New York, NY, USA
(Prof J Baselga MD); Lineberger
Comprehensive Cancer Center,
Chapel Hill, NC, USA
(C Perou PhD); St Gertrauden
Hospital, Berlin, Germany
(Prof J Blohmer MD); MD
Anderson Cancer Center
Orlando, Orlando, FL, USA
(E P Mamounas MD);
164
Background Pathological complete response has been proposed as a surrogate endpoint for prediction of long-term
clinical benet, such as disease-free survival, event-free survival (EFS), and overall survival (OS). We had four key
objectives: to establish the association between pathological complete response and EFS and OS, to establish the
denition of pathological complete response that correlates best with long-term outcome, to identify the breast cancer
subtypes in which pathological complete response is best correlated with long-term outcome, and to assess whether an
increase in frequency of pathological complete response between treatment groups predicts improved EFS and OS.
Methods We searched PubMed, Embase, and Medline for clinical trials of neoadjuvant treatment of breast cancer. To
be eligible, studies had to meet three inclusion criteria: include at least 200 patients with primary breast cancer
treated with preoperative chemotherapy followed by surgery; have available data for pathological complete response,
EFS, and OS; and have a median follow-up of at least 3 years. We compared the three most commonly used denitions
of pathological complete responseypT0 ypN0, ypT0/is ypN0, and ypT0/isfor their association with EFS and OS
in a responder analysis. We assessed the association between pathological complete response and EFS and OS in
various subgroups. Finally, we did a trial-level analysis to assess whether pathological complete response could be
used as a surrogate endpoint for EFS or OS.
Findings We obtained data from 12 identied international trials and 11 955 patients were included in our responder
analysis. Eradication of tumour from both breast and lymph nodes (ypT0 ypN0 or ypT0/is ypN0) was better associated
with improved EFS (ypT0 ypN0: hazard ratio [HR] 044, 95% CI 039051; ypT0/is ypN0: 048, 043054) and OS
(036, 030044; 036, 031042) than was tumour eradication from the breast alone (ypT0/is; EFS: HR 060, 95% CI
055066; OS 051, 045058). We used the ypT0/is ypN0 denition for all subsequent analyses. The association
between pathological complete response and long-term outcomes was strongest in patients with triple-negative breast
cancer (EFS: HR 024, 95% CI 018033; OS: 016, 011025) and in those with HER2-positive, hormone-receptornegative tumours who received trastuzumab (EFS: 015, 009027; OS: 008, 003, 022). In the trial-level analysis, we
recorded little association between increases in frequency of pathological complete response and EFS (R=003, 95% CI
000025) and OS (R=024, 000070).
Interpretation Patients who attain pathological complete response dened as ypT0 ypN0 or ypT0/is ypN0 have
improved survival. The prognostic value is greatest in aggressive tumour subtypes. Our pooled analysis could not
validate pathological complete response as a surrogate endpoint for improved EFS and OS.
Funding US Food and Drug Administration.
Introduction
New agents to treat breast cancer have historically been
approved rst in the metastatic setting, with approval for
use in early-stage breast cancer following many years
later on the basis of results of large randomised adjuvant
trials with long follow-up. Neoadjuvant treatment
systemic therapy delivered before denitive breast cancer
surgerywas once reserved to reduce the size and extent
of locally advanced tumours, but is now being used more
widely. In addition to increasing the likelihood of tumour
control and the potential for curability in early breast
cancer, neoadjuvant trials allow rapid assessment of drug
ecacy and could expedite development and approval of
treatments for early breast cancer.1 Pathological complete
response has been proposed as a surrogate endpoint for
prediction of long-term clinical benet, such as diseasefree survival and overall survival (OS).25
Although pathological complete response has been the
most commonly used endpoint in neoadjuvant trials, it
has been variably dened, which has made reporting and
interpretation of data challenging. One way to optimise
the denition of pathological complete response, enable
the interpretation of data, and investigate the association
between pathological complete response and long-term
outcome is via a pooled analysis of neoadjuvant trials. To
obtain the requisite number of trials for this pooled
www.thelancet.com Vol 384 July 12, 2014
Articles
analysis, the US Food and Drug Administration established an international working group known as Collaborative Trials in Neoadjuvant Breast Cancer (CTNeoBC)
with investigators who had done neoadjuvant trials for
which long-term data are available.
We aimed to investigate the potential of pathological
complete response as a surrogate endpoint for long-term
outcomes. We had four key objectives: to establish the
association between pathological complete response and
event-free survival (EFS) and OS, to establish the denition
of pathological complete response that correlates best with
long-term outcome, to identify the breast cancer subtypes
in which pathological complete response is best correlated
with long-term outcome, and to assess whether an increase
in frequency of pathological complete response predicts
improved EFS and OS. Here, we present initial results
from the CTNeoBC pooled analysis.
Methods
Search strategy and selection criteria
We searched PubMed, Embase, and Medline for reports
of clinical trials of neoadjuvant treatment of breast cancer
published between Jan 1, 1990, and Aug 1, 2011. To be
eligible, studies had to meet three inclusion criteria:
include at least 200 patients with primary breast cancer
treated with preoperative chemotherapy followed by
surgery; have available data for pathological complete
response, EFS, and OS; and have a median follow-up of
at least 3 years.
Investigators from identied trials were invited to
participate in a collaborative analysis and agreed to
provide individual patient data. We excluded data from
all patients randomised to postoperative treatment,
patients in the HER2-negative treatment group of the
NOAH trial (necessary data were unavailable for this
group), and patients who never began assigned
treatment.
occurrence of disease progression resulting in
inoperability, locoregional recurrence (after neoadjuvant
therapy), distant metastases, or death from any cause.
Patients alive without an event as of the analysis cuto
date were censored at last study follow-up date. Overall
survival was calculated from date of randomisation to
death. For patients alive on the data cuto date, survival
was censored at last study follow-up date.
Statistical analysis
In the pooled analysis, we categorised patients who either
did not undergo surgery or who had surgery but for whom
data were missing for pathological complete response as
non-pathological complete responders. We compared the
three denitions of pathological complete response for
their association with EFS and OS. In this responder
analysis, EFS and OS were compared between patients
with and without pathological complete response,
irrespective of treatment assignment, with a log-rank test
stratied by study. We estimated hazard ratios (HRs) and
95% CIs of EFS and OS from stratied Cox regression
models with study as a stratication factor. We also
obtained Kaplan-Meier estimates of EFS and OS by
pathological complete response status. We assessed the
association between pathological complete response and
EFS and OS in various subgroups. We did multivariable
analyses with Cox regression models including baseline
factors (age, tumour stage, nodal status, histological type,
tumour grade, and tumour subtype) and pathological
complete response status. We excluded patients with
missing factors from the multivariable analyses.
www.thelancet.com Vol 384 July 12, 2014
Correspondence to:
Dr Patricia Cortazar,
10903 New Hampshire Avenue,
Building 22, Room 2333,
Silver Spring, MD 209930002,
USA
patricia.cortazar@fda.hhs.gov
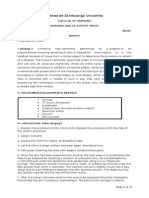
13 856 patients enrolled in 12 neoadjuvant trials
1901 excluded
1667 assigned to adjuvant treatment (904
from ECTO; 763 from NSABP B-18)
99 in the HER2-negative treatment
group of the NOAH trial
1 in the HER2-positive treatment
group of the NOAH trial for whom no
data obtained
134 never began assigned treatment
(60 from GeparTrio; 74 from
GeparQuattro)
Outcome measures
Denitions of pathological complete response varied
across trials. We compared the three most commonly
used pathological complete response denitions to
establish their association with long-term outcome:
ypT0 ypN0 (ie, absence of invasive cancer and in-situ
cancer in the breast and axillary nodes), ypT0/is ypN0
(ie, absence of invasive cancer in the breast and axillary
nodes, irrespective of ductal carcinoma in situ), and
ypT0/is (ie, absence of invasive cancer in the breast irrespective of ductal carcinoma in situ or nodal involvement).
All trials had standard operating procedures for pathological complete response assessments.
The endpoint of choice for adjuvant trials has been
disease-free survival, reecting the fact that patients are
disease free at the time of randomisation. By contrast,
EFS is used in neoadjuvant trials because all patients are
not disease free at randomisation. We calculated EFS as
the interval from randomisation to the earliest
KarolinskaInstitutet and
University Hospital,
Stockholm, Sweden
(Prof J Bergh MD); NN Petrov
Research Institute of Oncology,
St Petersburg, Russia
(Prof V Semiglazov MD);
University Womens Hospital,
Kiel, Germany
(H Eidtmann MD); Jules Bordet
Institute, Brussels, Belgium
(Prof M Piccart MD);
Frauenklinik des
Universittsklinikums,
Erlangen, Germany
(Prof P A Fasching MD);
Universitts Frauenklinik,
Rostock, Germany
(Prof B Gerber MD); Virginia
Commonwealth University
Massey Cancer Center,
Richmond, VA, USA
(C E Geyer Jr MD); and Hospital
of the Ludwig Maximilian
University of Munich, Munich,
Germany (N Ditsch MD,
Prof W Eiermann MD)
11 955 included in responder analysis
2515 excluded
1713 in non-randomised neoadjuvant
groups (451 from ECTO; 285 from
GeparTrioPilot; 760 from NSABP
B-18; 217 from TECHNO)
802 given additional adjuvant taxane
in NSABP B-27
9440 included in the trial-level analysis
Figure 1: Study prole
165
Articles
To explore the potential of pathological complete
response as a surrogate endpoint for EFS or OS in a
trial-level analysis, we quantied the association between
treatment eects on pathological complete response and
EFS and OS using a weighted linear regression model
on a logarithmic scale. We excluded data from patients
in non-randomised groups from this analysis, because
we could not estimate the treatment eect size in these
groups. We also excluded patients in NSABP B-27 who
received additional adjuvant taxane treatment because
the neoadjuvant treatment eect could not be isolated.
We present treatment eects on EFS and OS as
HRs (calculated with Cox proportional hazards models)
and on pathological complete response as odds ratios
(calculated with logistic regression models) within each
randomised comparison. The linear regression model
was weighted by sample size of each randomised comparison. Using a two-stage model to adjust for the
estimation error of treatment eect size estimates,6 we
calculated the coecient of determination (R) and the
associated 95% CI to measure the correlation between
pathological complete response and EFS and OS by
treatment eect. By convention, an HR (experimental vs
control) of less than 1 denotes a favourable result for
EFS and OS in the experimental group, and an odds
ratio (experimental vs control) of more than 1 denotes a
favourable result for pathological complete response.
Thus, a strong negative correlation between log hazard
ratio for EFS or OS and log odds ratio for pathological
complete response would validate pathological complete
response as a surrogate for long-term clinical benet.
All analyses were done with SAS (version 9.2).
Results
We identied 12 international neoadjuvant trials: AGO 1
(n=668),7 ECTO (n=1355),8 EORTC 10994/BIG 1-00
Overall survival
100
80
80
Overall survival (%)
Event-free survival (%)
Event-free survival
100
60
40
HR 048 (95% CI 043054)
20
60
40
HR 036 (95% CI 031042)
20
Pathological complete response
No pathological complete response
0
0
Number at risk
Pathological 2131
complete response
No pathological 9824
complete response
6
9
12
Time since randomisation (years)
15
18
6
9
12
Time since randomisation (years)
15
18
1513
583
337
124
35
2131
1618
640
383
145
43
6169
2674
1523
525
165
9824
7119
3173
1859
659
209
Figure 2: Associations between pathological complete response and event-free survival and overall survival
ypT0/is ypN0 denition of pathological complete response (ie, absence of invasive cancer in the breast and axillary nodes, irrespective of ductal carcinoma in situ).
HR=hazard ratio.
Overall survival
100
80
80
Overall survival (%)
Event-free survival (%)
Event-free survival
100
60
40
ypT0 ypN0 (n=1554); HR 044 (95% CI 039051)
ypT0/is ypN0 (n=2131); HR 048 (95% CI 043054)
ypT0/is (n=2598); HR 060 (95% CI 055066)
20
60
40
ypT0 ypN0 (n=1554); HR 036 (95% CI 030044)
ypT0/is ypN0 (n=2131); HR 036 (95% CI 031042)
ypT0/is (n=2598); HR 051 (95% CI 045058)
20
0
0
10
15
Time since randomisation (years)
20
10
15
Time since randomisation (years)
20
Figure 3: Associations between three denitions of pathological complete response and event-free survival and overall survival
We compared event-free survival and overall survival between patients who did and did not achieve a pathological complete response according to one of three
denitions. Patients who did not achieve a pathological complete response are not shown. Number of patients who achieved a pathological complete response is listed
for each pathological complete response denition. Patients could achieve pathological complete response according to more than one denition. ypT0 ypN0=absence
of invasive cancer and in-situ cancer in the breast and axillary nodes. ypT0/is ypN0=absence of invasive cancer in the breast and axillary nodes, irrespective of ductal
carcinoma in situ. ypT0/is=absence of invasive cancer in the breast, irrespective of ductal carcinoma in situ or nodal involvement. HR=hazard ratio.
166
www.thelancet.com Vol 384 July 12, 2014
Articles
(n=1856),9 GeparDuo (n=907),10 GeparQuattro (n=1495),11,12
GeparTrio (n=2072),13,14 GeparTrio-Pilot (n=285),15 NOAH
(n=334),16 NSABP B-18 (n=1523),17,18 NSABP B-27 (n=2411),18,19
PREPARE (n=733),20,21 and TECHNO (n=217; appendix).22
No major trial was excluded from the pooled analysis. All
were randomised controlled trials except for TECHNO,22
which was a single-group study previously included in the
pooled analysis of the German neoadjuvant trials.23
In each trial, heterogeneous populations of patients
were enrolled and randomised comparisons of
See Online for appendix
Percentage of patients
achieving pathological
complete response
(95% CI)
Clinical tumour stage
T1 (n=785)
T2 (n=7328)
T3 (n=2493)
T4ac (n=781)
T4d (n=482)
Clinical nodal status
Negative (n=6320)
Positive (n=5487)
Histological type
Ductal (n=8567)
Lobular (n=1221)
Mixed (n=475)
Tumour grade
1 (n=426)
2 (n=4392)
3 (n=3217)
Clinical tumour subtype
Hormone-receptor-positive, HER2-negative, grade 1/2 (n=1986)
Hormone-receptor-positive, HER2-negative, grade 3 (n=630)
HER2-positive, hormone-receptor-positive, trastuzumab (n=385)
HER2-positive, hormone-receptor-positive, no trastuzumab (n=701)
HER2-positive, hormone-receptor-negative, trastuzumab (n=364)
HER2-positive, hormone-receptor-negative, no trastuzumab (n=471)
Triple negative (n=1157)
183 (157212)
199 (190209)
130 (117143)
145 (121171)
160 (128196)
188 (179198)
169 (159179)
155 (147163)
78 (6394)
227 (190268)
78 (54107)
123 (113133)
258 (243274)
75 (6387)
162 (134193)
309 (263358)
183 (155213)
503 (450555)
302 (260345)
336 (309364)
0
10
20
30
40
Pathological complete response (%)
50
60
HR (95% CI)
Clinical tumour stage
T1 (n=785)
T2 (n=7328)
T3 (n=2493)
T4ac (n=781)
T4d (n=482)
Clinical nodal status
Negative (n=6320)
Positive (n=5487)
Histological type
Ductal (n=8567)
Lobular (n=1221)
Mixed (n=475)
Tumour grade
1 (n=426)
2 (n=4392)
3 (n=3217)
Clinical tumour subtype
Hormone-receptor-positive, HER2-negative, grade 1/2 (n=1986)
Hormone-receptor-positive, HER2-negative, grade 3 (n=630)
HER2-positive, hormone-receptor-positive, trastuzumab (n=385)
HER2-positive, hormone-receptor-positive, no trastuzumab (n=701)
HER2-positive, hormone-receptor-negative, trastuzumab (n=364)
HER2-positive, hormone-receptor-negative, no trastuzumab (n=471)
Triple negative (n=1157)
064 (039105)
034 (027042)
032 (023045)
047 (028078)
046 (027079)
039 (031049)
035 (028043)
040 (032049)
093 (050170)
030 (014065)
048 (012196)
055 (040075)
029 (022037)
047 (021107)
029 (013065)
056 (023137)
057 (031104)
008 (003022)
029 (017050)
016 (011025)
01
02
04
06
Overall survival better with
pathological complete response
15
Overall survival better without
pathological complete response
Figure 4: Percentage of patients achieving pathological complete response (A) and HRs for overall survival (B), by subgroup
Information about clinical tumour stage available for 11 869 patients, about clinical nodal status for 11 807 patients, about histological type for 10 263 patients,
about tumour grade for 8035 patients, and about clinical tumour subtype for 5694 patients. ypT0/is ypN0 denition of pathological complete response used. No
multiplicity adjustment was made. HR=hazard ratio.
www.thelancet.com Vol 384 July 12, 2014
167
Articles
anthracycline-based and taxane-based regimens were
done, with the exception of the NOAH16 and TECHNO22
trials, which were limited to patients with HER2positive locally advanced or inammatory breast cancer.
Patients in the NOAH16 trial were randomly assigned to
preoperative
chemotherapy
with
or
without
trastuzumab, and those in the TECHNO22 trial received
trastuzumab and chemotherapy followed by 1 year of
adjuvant trastuzumab. In the GeparQuattro trial,11,12
patients with HER2-positive tumours received trastuzumab concomitantly with chemotherapy. Overall, 1087
(55%) of 1989 patients with HER2-positive tumours
included in the pooled analysis did not receive 1 year of
adjuvant trastuzumab because they were treated before
adjuvant trastuzumab trials were reported. All
Hormone-receptor-positive,
HER2-negative
patients with hormone-receptor-positive tumours were
supposed to receive at least 5 years of endocrine therapy.
Breast cancer subtype was established by clinicopathological criteria, such as hormone-receptor status,
HER2 overexpression, and histological grade as
assessed by local pathologists. The Ki-67 labelling index
had not been routinely assessed in the included studies.
11 955 patients were included in our pooled responder
analysis (gure 1). Baseline characteristics are shown in
the appendix. Median age was 49 years (IQR 4357).
7328 patients (61%) had T2 tumours, 482 (4%) had
inammatory breast cancer (ie, T4d tumours), and
5487 (46%) had clinically involved lymph nodes.
3572 (30%) patients had hormone-receptor-negative
breast cancer, and 1989 (17%) had HER2-positive
Hormone-receptor-positive,
HER2-negative, grade 1/2
Hormone-receptor-positive,
HER2-negative, grade 3
Event-free survival (%)
100
80
60
40
20
HR 049 (95% CI 033071)
HR 063 (95% CI 038104)
HR 027 (95% CI 014050)
0
0
Number at risk
pCR 270 244 224 184 113 69 21
No pCR 2491 2226 1978 1616 1017 658 247
6
84
2
20
2
1
HER2-positive
148 134 123 102 55 33 10
1838 1653 1493 1236 790 517 198
5
68
2
15
2
1
HER2-positive, hormone-receptor-positive
102 92 83 71 49 30
528 458 376 290 173 111
9
38
1
14
0
5
HER2-positive, hormone-receptor-negative
Event-free survival (%)
100
80
60
40
20
HR 039 (95% CI 031050)
HR 058 (95% CI 042082)
HR 025 (95% CI 018034)
0
0
Number at risk
pCR 586 527 454 371 212 120 37
No pCR 1403 1157 918 713 436 269 106
4
33
2
3
1
1
2
3
4
5
6
7
Time since randomisation (years)
247 224 194 157 91 50
839 723 617 484 306 198
17
79
2
24
2
3
1
1
2
3
4
5
6
7
Time since randomisation (years)
325 293 250 205 115 65
510 392 269 200 111 59
19
22
2
6
Triple negative
pCR
No pCR
Event-free survival (%)
100
80
60
40
20
HR 024 (95% CI 018033)
0
0
1
2
3
4
5
6
7
Time since randomisation (years)
Number at risk
pCR 389 349 310 250 166 88 29 11
No pCR 768 604 429 317 198 125 50 13
1
1
Figure 5: Association between pCR and event-free survival, by breast cancer subtype
pCR=pathological complete response. HR=hazard ratio.
168
www.thelancet.com Vol 384 July 12, 2014
Articles
tumours. Tumour testing for HER2 was not necessary in
the earlier trials, so information about HER2-receptor
status was not available for four trials (AGO-1,7 NSABP
B-18,17 NSABP B-27,19 and ECTO8). Overall median followup for EFS was 540 years (95% CI 533544) and for
OS was 537 years (531543).
Overall frequency of pathological complete response
was low, and the frequency decreased with increasingly
stringent denitions: 22% (95% CI 2122) of patients
achieved ypT0/is, 18% (1719) achieved ypT0/is ypN0,
and 13% (1214) achieved ypT0 ypN0. Overall, patients
who achieved a pathological complete response had
longer EFS and OS than did patients with residual
invasive cancer (gures 2, 3). Eradication of tumour
from both the breast and axillary lymph nodes (ypT0
pN0 and ypT0/is ypN0) was better associated with
improved EFS and OS than was eradication of invasive
tumour from the breast alone (ypT0/is; gure 3).
Associations with EFS and OS were similar for ypT0
ypN0 and ypT0/is ypN0 (gure 3). Additionally,
associations were consistent when we adjusted for
baseline factors using multivariable Cox models. We
used the ypT0/is ypN0 denition for all subsequent
analyses.
As expected, frequency of pathological complete
responses in patients with low-grade, hormone-receptorpositive tumours was low, and more than doubled in
the high-grade hormone-receptor-positive subgroup
(gure 4A). The more aggressive subtypestriplenegative and HER2-positive tumourshad increased
frequencies of pathological complete response
(gure 4A). Within the HER2-positive population, pathological complete response was more common for
hormone-receptor-negative tumours than for hormonereceptor-positive tumours, and with the addition of
trastuzumab (gure 4A).
The pathological complete response was positively
associated with EFS (HR 049, 95% CI 033071) and
OS (043, 023071) in the overall hormone-receptorpositive, HER2-negative population. The association
between pathological complete response and long-term
outcome was stronger in patients with high-grade
tumours than in those with low-grade tumours
(gures 4B, 5). Additionally, pathological complete
response was associated with long-term outcome in the
HER2-positive subgroup irrespective of hormonereceptor status (EFS: HR 039, 95% CI 031050;
OS: 034, 024047). The strength of the association
increased in the hormone-receptor-negative subgroup
(EFS: 025, 018034; OS: 019, 012031). The most
favourable outcomes after pathological complete response
were recorded in patients with HER2-positive, hormonereceptor-negative tumours who received trastuzumab
(EFS: 015, 009027; OS: 008, 003022), and in the
triple-negative subgroup (gures 4B, 5).
We analysed the association between the eect of
treatments on pathological complete response and longterm outcomes in ten randomised comparisons, excluding
non-randomised neoadjuvant groups and patients given
additional adjuvant taxane (gure 1). At a trial level, we
recorded little association between increases in frequency
of pathological complete response and the treatments
eect on EFS or OS (gure 6). The coecient of
determination (R) between improvement in pathological
complete response and EFS was 003 (95% CI 000025),
and that between improvement in pathological complete
response and OS was 024 (000070).
We also investigated the trial-level association between
pathological complete response and long-term outcome
by tumour subtype. We excluded patients with lowgrade, hormone-receptor-positive tumours because of
low frequency of pathological complete response. The
Overall survival
Event-free survival
12
12
B
Hazard ratio for overall survival
Hazard ratio for event-free survival
A
10
C
08
F
E
G
I
06
B
10
H
08
C
E
A
10
12
16
20
24
30
Odds ratio for pathological complete response
36
G
I
06
08
08
10
12
16
20
24
30
Odds ratio for pathological complete response
36
Figure 6: Trial-level correlation between treatment eect on pathological complete response and event-free survival or overall survival
Each circle corresponds to one randomised comparison and the size of the circle represents the sample size. A=GeparQuattro (epirubicin plus cyclophosphamide
followed by docetaxel then capecitabine vs epirubicin plus cyclophosphamide followed by docetaxel). B=GeparDuo. C=GeparQuattro (epirubicin plus
cyclophosphamide followed by docetaxel and capecitabine vs epirubicin plus cyclophosphamide followed by docetaxel). D=EORTC 10994/BIG 1-00. E=PREPARE.
F=NSABP B-27. G=responders in GeparTrio. H=non-responders in GeparTrio. I=AGO 1. J=NOAH.
www.thelancet.com Vol 384 July 12, 2014
169
Articles
results of the analyses by breast cancer subtype were
consistent with ndings in the overall population: no
correlation between improvement in frequency of
pathological complete response and the treatments
eect on EFS or OS was recorded (appendix).
Discussion
In our pooled analysis, we recorded that eradication of
tumours from both breast and lymph nodes (ypT0 ypN0
or ypT0/is ypN0 pathological complete response) had a
stronger association with improved EFS and OS than did
eradication of tumour from the breast alone (ypT0/is).
The strongest association between pathological complete response and long-term outcome was in patients
with aggressive breast cancer subtypes (triple negative;
hormone-receptor-positive, high-grade, and HER2-negative; and HER2-positive and hormone-receptor-negative).
Nevertheless, an increase in frequency of pathological
complete response between treatment groups did not
predict improved EFS and OS.
Standardisation of the denition of pathological complete response would allow planning and interpretation
of future neoadjuvant clinical trials intended to support
drug approval. We propose that pathological complete
response is dened as either ypT0/is ypN0 or ypT0 ypN0
in future trials. However, ypT0 ypN0 is a more stringent
denition and its use could lead to reduced frequencies
of pathological complete response. Presence or absence
of ductal carcinoma in situ did not aect long-term
outcome in our analysis. Additionally, a retrospective
analysis24,25 of a database including more than
2000 patients treated with neoadjuvant chemotherapy
showed that residual ductal carcinoma in situ in patients
with complete eradication of the invasive cancer from the
breast and lymph nodes did not adversely aect survival.
By contrast, a German pooled analysis26 of seven
neoadjuvant trials showed that patients without ductal
carcinoma in situ had longer survival than did patients
with residual ductal carcinoma in situ when all invasive
disease was eradicated.
Several other groups have reported improved longterm outcomes in patients with pathological complete
response compared with those with residual tumour at
the time of surgery.17,19,23,24,26 Our pooled analysis
conrmed this nding in various tumour subtypes and
in groups divided by other baseline characteristics. The
strength of the association increased with trastuzumab
treatment, which emphasises the importance of targeted
therapy. The association between pathological complete
response and long-term outcome was weakest for
hormone-receptor-positive and low-grade tumours, and
for HER2-positive and hormone-receptor-positive
tumours. The German pooled analysis23,26 similarly
showed that the association between pathological
complete response and long-term outcome was strongest
in patients with aggressive breast cancer subtypes.
However, pathological complete response was not
170
prognostic in patients with luminal A or luminal B and
HER2-positive breast cancer.
The dierence between patient-level analyses and triallevel analyses is a common source of confusion. Patientlevel analyses, sometimes referred to as responder
analyses, compare the clinical outcome of patients with
and without pathological complete response, irrespective
of the treatment group. These analyses are meaningful
as they predict improved survival for patients who attain
pathological complete response. Because these responder
analyses are independent of the treatment group, they
are not useful for comparisons of treatments at a trial
level. The CTNeoBC pooled analysis is the rst large
analysis in which primary source data has been used to
assess the association between pathological complete
response and EFS and OS at a trial level.
We propose four potential explanations for the
nding that an increase in frequency of pathological
complete response between treatment groups did not
predict improved EFS and OS. First, in most of the
included trials, women with heterogeneous breast
cancer tumour subtypes were enrolled, which would be
expected to obscure the association between pathological complete response and survival if subtypes
respond dierently to the same treatment, or if dierent
absolute improvements in frequency of pathological
complete response are necessary to meaningfully aect
long-term outcomes. Second, a neoadjuvant therapy
targeted to a specic tumour subtype (trastuzumab)
was used in only three trials (GeparQuattro,12 NOAH,16
and TECHNO22), and trastuzumab used as an adjunct
to chemotherapy in only the NOAH study. As a result,
absolute dierences in the frequency of pathological
complete response between chemotherapy groups in
the included trials were generally low (111%), but were
as high as 20% for the NOAH trial, comparing
trastuzumab plus chemotherapy with chemotherapy
alone (ypT0/is ypN0: 35% vs 15%; odds ratio 304,
95% CI 164582). Similarly, the dierence in the
proportion of patients achieving EFS at 5 years between
treatment groups in the NOAH study was 13%,
although postoperative trastuzumab in the experimental
group could have partly contributed to the treatment
eect. Fourth, factors unrelated to primary tumour
response could have had a role. In the HER2-positive
subgroup, we noted that the addition of one trial with
increased treatment eects (NOAH) decreased the
slope of the curve, suggesting a trial-level correlation
between frequency of pathological complete response
and long-term outcome could be identied in future
trials with more homogeneous populations and
incorporation of targeted therapies. Future trials of
subtype-specic populations with dierences in
frequency of pathological complete response between
treatment groups that are larger than are those in the
trials we included could predict improvement in EFS or
OS in early-stage breast cancer.
www.thelancet.com Vol 384 July 12, 2014
Articles
The importance of individual-level association should
not be overlooked; it oers insight into the natural
history of an individuals disease and is thus useful to
counsel patients. Trial-level association is useful to
predict population treatment benets. As previously
suggested,6,27 an acceptable surrogate endpoint should be
correlated with outcome at both the individual and trial
levels. Our pooled analysis could not establish a triallevel correlation between pathological complete response
and long-term outcome. In view of the substantial
improvements in survival for individual patients who
attain pathological complete response, we believe that if a
novel agent produces a marked absolute increase in
frequency of pathological complete response compared
with standard therapy alone in the intention-to-treat
population, that agent could also be reasonably likely to
result in long-term improvements in EFS or OS.28 In our
future analyses (with genomic assays to better characterise subgroups and including additional anti-HER2
trials), we will investigate the importance of pathological
complete response in dened subsets and assess other
promising surrogate endpoints.
Contributors
PC, MU, JPC, NW, LG, PV, SL, DLW, EPM, RJ, SP, CEG Jr, PR, and GvM
designed the study. PC, LZ, KM, JPC, HB, DC, PV, JBo, and GvM
collected and analysed data. All authors interpreted data and wrote the
report.
Declaration of interests
DC is a consultant for Genentech, GlaxoSmithKline, and Roche. LG has
received a grant or research support from Roche. SMS is an unpaid
consultant for Genentech, and research grants, and her institution has
received received grants from Genentech, Roche, Sano-Aventis, Puma,
and BMS. CP is a paid consultant for Sano-Aventis. JBl has received
nancial support from Amgen, Roche, and Sano-Aventis. JBe has
received grants or research support from Amgen, Bayer, Roche, and
Sano-Aventis. HE is a paid consultant for Amgen, Novartis, and Roche;
and has received nancial support from Amgen, GlaxoSmithKline,
Novartis, and Roche. MP is a board member for Pharmamar and is a
paid consultant for Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim,
Roche, and Sano. PAF has received nancial support from Novartis,
Pzer, Roche, and Sano-Aventis. BG is a paid consultant for
AstraZeneca and has received honoraria from AstraZeneca and
GlaxoSmithKline. WE is a paid consultant for Roche, Sano-Aventis, and
Genomic Health; and has received speakers honoraria from Genomic
Health, Novartis, Roche, and Sano-Aventis. GvM is a paid consultant
for Roche and Sano-Aventis; and has received nancial support from
Amgen, Roche, and Sano-Aventis. The other authors declare that they
have no competing interests.
Acknowledgments
This project was partly funded by the US Food and Drug Administration.
We thank Janet Woodcock, who provided nancial support for the
CTNeoBC pooled analysis; all the patients, Breast Cancer Cooperative
Groups, investigators, pathologists, and statisticians who participated in
the neoadjuvant trials; and Jo Anne Zujewski for her help.
References
1
Prowell TM, Pazdur R. Pathological complete response and
accelerated drug approval in early breast cancer. N Engl J Med 2012;
366: 243841.
2
Bonadonna G, Valagussa P, Brambilla C, Ferrari L. Preoperative
chemotherapy in operable breast cancer. Lancet 1993; 341: 1485.
3
Cameron DA, Anderson ED, Levack P, et al. Primary systemic
therapy for operable breast cancer10-year survival data after
chemotherapy and hormone therapy. Br J Cancer 1997;
76: 1099105.
www.thelancet.com Vol 384 July 12, 2014
10
11
12
13
14
15
16
17
18
19
20
Liedtke C, Mazouni C, Hess KR, et al. Response to neoadjuvant
therapy and long-term survival in patients with triple-negative
breast cancer. J Clin Oncol 2008; 26: 127581.
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative
chemotherapy for women with operable breast cancer.
Cochrane Database Syst Rev 2007; 2: CD005002.
Burzykowski T. An ordinal surrogate for a survival true endpoint.
In: Burzykowski T, Molengerghs G, Buyse M, eds. The evaluation
of surrogate endpoints. New York, NY: Springer, 2005.
Untch M, Mbus V, Kuhn W, et al. Intensive dose-dense compared
with conventionally scheduled preoperative chemotherapy for
high-risk primary breast cancer. J Clin Oncol 2009; 27: 293845.
Gianni L, Baselga J, Eiermann W, et al. Phase III trial evaluating the
addition of paclitaxel to doxorubicin followed by cyclophosphamide,
methotrexate, and uorouracil, as adjuvant or primary systemic
therapy: European Cooperative Trial in Operable Breast Cancer.
J Clin Oncol 2009; 27: 247481.
Bonnefoi H, Piccart M, Bogaerts J, et al, on behalf of the EORTC
10994/BIG 1-00 Study Investigators. TP53 status for prediction of
sensitivity to taxane versus non-taxane neoadjuvant chemotherapy
in breast cancer (EORTC 10994/BIG 1-00): a randomised phase 3
trial. Lancet Oncol 2011; 12: 52739.
von Minckwitz G, Raab G, Caputo A, et al. Doxorubicin with
cyclophosphamide followed by docetaxel every 21 days compared
with doxorubicin and docetaxel every 14 days as preoperative
treatment in operable breast cancer: the GEPARDUO study of the
German Breast Group. J Clin Oncol 2005; 23: 267685.
von Minckwitz G, Rezai M, Loibl S, et al. Capecitabine in addition
to anthracycline- and taxane-based neoadjuvant treatment in
patients with primary breast cancer: phase III GeparQuattro study.
J Clin Oncol 2010; 28: 201523.
Untch M, Rezai M, Loibl S, et al. Neoadjuvant treatment with
trastuzumab in HER2-positive breast cancer: results from the
GeparQuattro study. J Clin Oncol 2010; 28: 202431.
von Minckwitz G, Kmmel S, Vogel P, et al, and the German Breast
Group. Neoadjuvant vinorelbine-capecitabine versus docetaxeldoxorubicin-cyclophosphamide in early nonresponsive breast
cancer: phase III randomized GeparTrio trial. J Natl Cancer Inst
2008; 100: 54251.
von Minckwitz G, Kmmel S, Vogel P, et al, and the German Breast
Group. Intensied neoadjuvant chemotherapy in early-responding
breast cancer: phase III randomized GeparTrio study.
J Natl Cancer Inst 2008; 100: 55262.
von Minckwitz G, Blohmer JU, Raab G, et al, and the German
Breast Group. In vivo chemosensitivity-adapted preoperative
chemotherapy in patients with early-stage breast cancer:
the GEPARTRIO pilot study. Ann Oncol 2005; 16: 5663.
Gianni L, Eiermann W, Semiglazov V, et al. Neoadjuvant
chemotherapy with trastuzumab followed by adjuvant trastuzumab
versus neoadjuvant chemotherapy alone, in patients with
HER2-positive locally advanced breast cancer (the NOAH trial):
a randomised controlled superiority trial with a parallel
HER2-negative cohort. Lancet 2010; 375: 37784.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative
chemotherapy in patients with operable breast cancer: nine-year
results from National Surgical Adjuvant Breast and Bowel Project
B-18. J Natl Cancer Inst Monogr 2001; 30: 96102.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy:
updates of National Surgical Adjuvant Breast and Bowel Project
Protocols B-18 and B-27. J Clin Oncol 2008; 26: 77885.
Bear HD, Anderson S, Brown A, et al, and the National Surgical
Adjuvant Breast and Bowel Project Protocol B-27. The eect on
tumor response of adding sequential preoperative docetaxel to
preoperative doxorubicin and cyclophosphamide: preliminary
results from National Surgical Adjuvant Breast and Bowel Project
Protocol B-27. J Clin Oncol 2003; 21: 416574.
Untch M, Fasching PA, Konecny GE, et al, and the
Arbeitsgemeinschaft Gynkologische Onkologie PREPARE
investigators. PREPARE trial: a randomized phase III trial
comparing preoperative, dose-dense, dose-intensied chemotherapy
with epirubicin, paclitaxel and CMF versus a standard-dosed
epirubicin/cyclophosphamide followed by paclitaxel darbepoetin
alfa in primary breast cancerresults at the time of surgery.
Ann Oncol 2011; 22: 198898.
171
Articles
21
22
23
24
172
Untch M, von Minckwitz G, Konecny GE, et al, and the
Arbeitsgemeinschaft Gynkologische Onkologie PREPARE
investigators. PREPARE trial: a randomized phase III trial
comparing preoperative, dose-dense, dose-intensied chemotherapy
with epirubicin, paclitaxel, and CMF versus a standard-dosed
epirubicin-cyclophosphamide followed by paclitaxel with or without
darbepoetin alfa in primary breast canceroutcome on prognosis.
Ann Oncol 2011; 22: 19992006.
Untch M, Fasching PA, Konecny GE, et al. Pathologic complete
response after neoadjuvant chemotherapy plus trastuzumab predicts
favorable survival in human epidermal growth factor receptor
2-overexpressing breast cancer: results from the TECHNO trial of the
AGO and GBG study groups. J Clin Oncol 2011; 29: 335157.
von Minckwitz G, Untch M, Nesch E, et al. Impact of treatment
characteristics on response of dierent breast cancer phenotypes:
pooled analysis of the German neo-adjuvant chemotherapy trials.
Breast Cancer Res Treat 2011; 125: 14556.
Feldman LD, Hortobagyi GN, Buzdar AU, Ames FC,
Blumenschein GR. Pathological assessment of response to induction
chemotherapy in breast cancer. Cancer Res 1986; 46: 257881.
25
26
27
28
Mazouni C, Peintinger F, Wan-Kau S, et al. Residual ductal
carcinoma in situ in patients with complete eradication of invasive
breast cancer after neoadjuvant chemotherapy does not adversely
aect patient outcome. J Clin Oncol 2007; 25: 265055.
von Minckwitz G, Untch M, Blohmer JU, et al. Denition and
impact of pathologic complete response on prognosis after
neoadjuvant chemotherapy in various intrinsic breast cancer
subtypes. J Clin Oncol 2012; 30: 1796804.
Buyse M, Burzykowski T, Michiels S, Carroll K. Individual- and
trial-level surrogacy in colorectal cancer. Stat Methods Med Res
2008; 17: 46775.
US Center for Drug Evaluation and Research. Guidance for
industry: pathologic complete response in neoadjuvant treatment of
high-risk early-stage breast cancer: use as an endpoint to support
accelerated approval. May, 2012. http://www.fda.gov/downloads/
Drugs/GuidanceComplianceRegulatoryInformation/Guidances/
UCM305501.pdf (accessed Jan 22, 2014).
www.thelancet.com Vol 384 July 12, 2014
You might also like
- Damon Torque and Bracket Placement GuideDocument2 pagesDamon Torque and Bracket Placement GuideMarlina Adrini Turnodihardjo57% (7)
- Bi-Rads 6 EdDocument69 pagesBi-Rads 6 EdFernando Jaramillo100% (1)
- BB4 San Genital FemelDocument430 pagesBB4 San Genital FemelLoredana Milea Ex Lefter0% (1)
- Healthcare Financing in IndiADocument86 pagesHealthcare Financing in IndiAGeet Sheil67% (3)
- DLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsDocument4 pagesDLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsMa. Reina Gail T. Lizaso100% (5)
- Arthritis astrology signs and planetsDocument5 pagesArthritis astrology signs and planetsJatinder SandhuNo ratings yet
- Mini Project - Final Report: Object Oriented Programming (CSC238)Document23 pagesMini Project - Final Report: Object Oriented Programming (CSC238)Wan adlinaNo ratings yet
- De Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?Document3 pagesDe Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?jenmercadoNo ratings yet
- TraztuzumabDocument8 pagesTraztuzumabArlina Wiyata GamaNo ratings yet
- Ni Hms 574605Document17 pagesNi Hms 574605circe5690No ratings yet
- surgery of primary in de novo metastatic caDocument28 pagessurgery of primary in de novo metastatic caMariajanNo ratings yet
- Oup Accepted Manuscript 2017 PDFDocument8 pagesOup Accepted Manuscript 2017 PDFatikha apriliaNo ratings yet
- Impact of Time From Completion of Neoadjuvant Chemotherapy To Surgery On Survival Outcomes in Breast Cancer PatientsDocument7 pagesImpact of Time From Completion of Neoadjuvant Chemotherapy To Surgery On Survival Outcomes in Breast Cancer PatientsPani lookyeeNo ratings yet
- Sabcs 2014 AllabstractsDocument1,508 pagesSabcs 2014 Allabstractsrajesh4189No ratings yet
- Breast CADocument8 pagesBreast CAjchowkingNo ratings yet
- Hormone Replacement Therapy in Cancer SurvivorsDocument13 pagesHormone Replacement Therapy in Cancer Survivorsiulia bNo ratings yet
- Sciencedirect: Original ResearchDocument8 pagesSciencedirect: Original ResearchThiamNo ratings yet
- Ojog 2015031717082632Document6 pagesOjog 2015031717082632SarlitaIndahPermatasariNo ratings yet
- THR-morbid ObesityDocument5 pagesTHR-morbid ObesityMohan DesaiNo ratings yet
- Prospektive Cohort Study of Risk Factors For Breast Cancer in Post Menopausal WomenDocument9 pagesProspektive Cohort Study of Risk Factors For Breast Cancer in Post Menopausal WomenAdi KaswadiNo ratings yet
- CLEOPATRA Biomarker Analysis - ProtocolDocument117 pagesCLEOPATRA Biomarker Analysis - ProtocolweilinmdNo ratings yet
- Yeo Et AlDocument10 pagesYeo Et AlAna MoraisNo ratings yet
- Running Head: INTEGRATIVE REVIEW 1Document13 pagesRunning Head: INTEGRATIVE REVIEW 1api-400244160No ratings yet
- Homocysteine As A Biomarker For Predicting Disease-Free Survival in Breast Cancer PDFDocument8 pagesHomocysteine As A Biomarker For Predicting Disease-Free Survival in Breast Cancer PDFNelson Carvas JrNo ratings yet
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDocument6 pagesNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanNo ratings yet
- Breast Cancer Follow-Up Literature Review and DiscussionDocument8 pagesBreast Cancer Follow-Up Literature Review and DiscussionaflsjnfvjNo ratings yet
- Cancer Treatment Reviews: Systematic or Meta-Analysis StudiesDocument14 pagesCancer Treatment Reviews: Systematic or Meta-Analysis StudieselmismoNo ratings yet
- PIIS0015028207002786 Phytoestrogens in Clinical PracticeDocument7 pagesPIIS0015028207002786 Phytoestrogens in Clinical PracticeGeorge CarpNo ratings yet
- Jco 2003 04Document8 pagesJco 2003 04fatimaramos31No ratings yet
- Conventional Dose ChemotherapyDocument8 pagesConventional Dose ChemotherapyOnic AugustineNo ratings yet
- Jurnal Breast CancerDocument8 pagesJurnal Breast CancerRudy AmoyeeNo ratings yet
- Predictors of Positive Chest Radiography in Non-Traumatic Chest Pain in The Emergency DepartmentDocument5 pagesPredictors of Positive Chest Radiography in Non-Traumatic Chest Pain in The Emergency DepartmentHario Tri HendrokoNo ratings yet
- Critical Appraisal For RCT & Meta AnalisisDocument8 pagesCritical Appraisal For RCT & Meta AnalisisHanniNo ratings yet
- Pelvic Pain in EndometriosisDocument7 pagesPelvic Pain in Endometriosism_tonydharmawanNo ratings yet
- Iranian Decision Making abdominal painDocument7 pagesIranian Decision Making abdominal painghaffari.eli5912No ratings yet
- NMAHP Research Unit, 2. Leicester Royal Infirmary: Hagen S, Stark D, Campbell PDocument2 pagesNMAHP Research Unit, 2. Leicester Royal Infirmary: Hagen S, Stark D, Campbell PMarkoNo ratings yet
- ContentServer 5 PDFDocument10 pagesContentServer 5 PDFkikiNo ratings yet
- Perez Et Al 2014 Trastuzumab Plus Adjuvant Chemotherapy For Human Epidermal Growth Factor Receptor 2 Positive BreastDocument10 pagesPerez Et Al 2014 Trastuzumab Plus Adjuvant Chemotherapy For Human Epidermal Growth Factor Receptor 2 Positive BreastDaniel Del RíoNo ratings yet
- Ovario Poliquitico ArticuloDocument6 pagesOvario Poliquitico ArticuloDaniela CristanchoNo ratings yet
- Document PDFDocument7 pagesDocument PDFharzalinaNo ratings yet
- Breast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsDocument11 pagesBreast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsAn'umillah Arini ZidnaNo ratings yet
- Aqy 028Document9 pagesAqy 028Yohanes AdinugrohoNo ratings yet
- NutritionsDocument9 pagesNutritionsPutra EkaNo ratings yet
- 247 FullDocument10 pages247 FullMeidianty TandiNo ratings yet
- Lower Risk of Hip Fracture with Higher Fruit and Vegetable IntakeDocument4 pagesLower Risk of Hip Fracture with Higher Fruit and Vegetable IntakerocksurNo ratings yet
- Kemoterapi THT 5Document8 pagesKemoterapi THT 5Niko Nofian NugrohoNo ratings yet
- Yao 2011Document10 pagesYao 2011Jemma ArakelyanNo ratings yet
- Breast Cancer and Physical Activity Literature ReviewDocument6 pagesBreast Cancer and Physical Activity Literature Reviewgvzph2vhNo ratings yet
- Screening Latent TB in Adult PDFDocument212 pagesScreening Latent TB in Adult PDFListiana Masyita DewiNo ratings yet
- Hormonal Contraceptives and Hormone Replacement Therapy As A Possible Risk Factor For Breast CancerDocument6 pagesHormonal Contraceptives and Hormone Replacement Therapy As A Possible Risk Factor For Breast CancerIdman GushaendriNo ratings yet
- Armen I 2020Document2 pagesArmen I 2020paolaNo ratings yet
- Fiber and HemmerhoidsDocument8 pagesFiber and HemmerhoidsHendry RamadhanNo ratings yet
- Kartika Erma Sundari AB212073 - CompressedDocument33 pagesKartika Erma Sundari AB212073 - Compressedrizky ardikaNo ratings yet
- Cleopatra2015 PDFDocument17 pagesCleopatra2015 PDFAndersson SaenzNo ratings yet
- Jurnal LeoDocument7 pagesJurnal LeoyunielsyaNo ratings yet
- Nejmoa 1606220Document10 pagesNejmoa 1606220Jay TiwariNo ratings yet
- V 04 P 0577Document8 pagesV 04 P 0577Sucipto HartonoNo ratings yet
- Blood 2012 LudwigDocument43 pagesBlood 2012 LudwigRaquel LopesNo ratings yet
- Beaumont 2011 Patient Reported Outcomes in Phase III Study of Everolimus Vs PlaceboDocument11 pagesBeaumont 2011 Patient Reported Outcomes in Phase III Study of Everolimus Vs PlaceboIzaty HamidNo ratings yet
- Cummings Et Al-2014-The Journal of PathologyDocument9 pagesCummings Et Al-2014-The Journal of Pathologyalicia1990No ratings yet
- Ebn - MSDDocument6 pagesEbn - MSDIrene NecesitoNo ratings yet
- World Congress Integrative Medicine & Health 2017: Part TwoDocument65 pagesWorld Congress Integrative Medicine & Health 2017: Part TwoGabrielAbarcaNo ratings yet
- Nej Mo A 1209978Document10 pagesNej Mo A 1209978MayMaryMasieMacyNo ratings yet
- Fiber TreatmentDocument8 pagesFiber TreatmentLana AdilaNo ratings yet
- Thursday, 13 June 2013 347: Scientific AbstractsDocument2 pagesThursday, 13 June 2013 347: Scientific Abstractstika_876267153No ratings yet
- Art:10 1186/bcr1744Document23 pagesArt:10 1186/bcr1744Preda LoredanaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 17: OncologyFrom EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyNo ratings yet
- POSITIVEDocument12 pagesPOSITIVEtabaresgonzaloNo ratings yet
- Chronic Pelvic Pain in Women. A Review 2021 PDFDocument11 pagesChronic Pelvic Pain in Women. A Review 2021 PDFRicardo Robles AlfaroNo ratings yet
- EBCTCGDocument31 pagesEBCTCGapi-26302710No ratings yet
- DNA PaperDocument18 pagesDNA PaperDavid LeNo ratings yet
- Cuz Ick 2016Document6 pagesCuz Ick 2016tabaresgonzaloNo ratings yet
- POSITIVEDocument12 pagesPOSITIVEtabaresgonzaloNo ratings yet
- Nejm MacDocument8 pagesNejm MactabaresgonzaloNo ratings yet
- Committee Opinion No 682 Microarrays And.55Document7 pagesCommittee Opinion No 682 Microarrays And.55tabaresgonzaloNo ratings yet
- Atlas of - Breast - Disease PDFDocument91 pagesAtlas of - Breast - Disease PDFPanagiotis KorkokiosNo ratings yet
- Date & Time Topics Subtopics Skills Lab: Prepared By: Rey Stephen T. Buenavista, RNDocument3 pagesDate & Time Topics Subtopics Skills Lab: Prepared By: Rey Stephen T. Buenavista, RNRS BuenavistaNo ratings yet
- Antipsychotic Agents: Conventional vs AtypicalDocument18 pagesAntipsychotic Agents: Conventional vs AtypicalmengakuNo ratings yet
- TERRUR 1st VerDocument16 pagesTERRUR 1st VerJerome JeremiasNo ratings yet
- The 38 Bach RemediesDocument20 pagesThe 38 Bach RemediesSriram Bharat100% (1)
- Clinical Manifestations, Diagnosis, and Surgery of Inferior Oblique Muscle EctopiaDocument5 pagesClinical Manifestations, Diagnosis, and Surgery of Inferior Oblique Muscle EctopiaMuhammad Imam NoorNo ratings yet
- Maternal and Child PreboardDocument17 pagesMaternal and Child PreboardMichelle GambolNo ratings yet
- CBTDocument21 pagesCBTsavvy_as_98No ratings yet
- Diuretics in States of Volume Overload Core Curriculum 2022Document13 pagesDiuretics in States of Volume Overload Core Curriculum 2022Fercho MedNo ratings yet
- Contact AllergyDocument39 pagesContact AllergylintangNo ratings yet
- 108 Names of DhanvantariDocument7 pages108 Names of DhanvantaricantuscantusNo ratings yet
- Ngos in WayanadDocument51 pagesNgos in Wayanadnivia008No ratings yet
- (Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingDocument7 pages(Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingRia DeviNo ratings yet
- CV Sef Disciplina Victor Lorin PurcareaDocument8 pagesCV Sef Disciplina Victor Lorin PurcareaMircea LeonardNo ratings yet
- 05 - SPSF3 04 B2 PDFDocument20 pages05 - SPSF3 04 B2 PDFCikgu RoshailaNo ratings yet
- Cor Pulmonale PresentationDocument17 pagesCor Pulmonale Presentationandi reskifaisNo ratings yet
- Beggs Stage 1 - Ortho / Orthodontic Courses by Indian Dental AcademyDocument33 pagesBeggs Stage 1 - Ortho / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- IM Injuction: Definition of Intramuscular InjectionDocument8 pagesIM Injuction: Definition of Intramuscular InjectiondhanasundariNo ratings yet
- (ANES) Mon 01 Epidural For Labor Analgesia (A2021)Document3 pages(ANES) Mon 01 Epidural For Labor Analgesia (A2021)Miguel SantosNo ratings yet
- Ateneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyDocument4 pagesAteneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyHaifi HunNo ratings yet
- Staff Nurse Interview Questions 2Document3 pagesStaff Nurse Interview Questions 2daciana_ilie100% (2)
- Transcultural NursingDocument13 pagesTranscultural NursingHassen ZabalaNo ratings yet
- Rheumatoid Arthritis: Pathophysiology PathophysiologyDocument34 pagesRheumatoid Arthritis: Pathophysiology PathophysiologyOmair RiazNo ratings yet
- Closed Tibia and Fibula Fracture Case PresentationDocument30 pagesClosed Tibia and Fibula Fracture Case Presentationzhafran_darwisNo ratings yet
- The Abc of Handover: E.D. Registrar A: Areas AllocationDocument1 pageThe Abc of Handover: E.D. Registrar A: Areas AllocationDiahNiatiNo ratings yet
- List of Empanelled Hospitals/Diagnostic Centres, and Cghs RatesDocument53 pagesList of Empanelled Hospitals/Diagnostic Centres, and Cghs RatesArputNo ratings yet