Professional Documents
Culture Documents
Effect of Anti-Epileptic Drugs in Pregnancy and Teratogenesis
Uploaded by
Nayan ChaudhariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effect of Anti-Epileptic Drugs in Pregnancy and Teratogenesis
Uploaded by
Nayan ChaudhariCopyright:
Available Formats
Indian Journal of Clinical Biochemistry, 2008 / 23 (3) 267-271
EFFECT OF ANTI-EPILEPTIC DRUGS IN PREGNANCY AND TERATOGENESIS
Sowbhagya Lakshmi and Kulkarni Sunanda*
Departments of Biochemistry and *Obstetrics & Gynecology, Bangalore Medical College, Bangalore-560 002.
ABSTRACT
Epilepsy raises special concern in women during pregnancy. Antiepileptic drugs are known to induce major
and minor malformations in the foetus. Aim of the study was to find an association between maternal serum
alpha fetoprotein levels, foetal abnormalities and antiepileptic drugs mediated teratogenicity. Maternal serum
alpha feto protein levels, kidney and liver function tests in age matched normal pregnant women and seizure
free epileptic pregnant women during 12 - 14 weeks of gestation were estimated. Cases were subjected to
ultrasonography at 11th -14th week of pregnancy and again at 20th week of pregnancy. maternal serum alfa feto
protein was assayed by a specific Electro Chemiluminescence Immuno Assay test. There was no significant
difference in kidney and liver function tests in cases as compared to controls. There were elevated levels of
alpha feto protein in cases as compared to controls but this was not statistically significant. No anomalies
were detected in ultrasound reports. Most women had normal full term delivery with healthy children but of low
birth weight. No correlation was seen between maternal serum alfa feto protein levels and antiepileptic drug
leading to teratogenesis.
KEY WORDS
Alpha feto proteins, Antiepileptic drugs, Teratogenic effects, Chemiluminescence.
INTRODUCTION
Epilepsy represents a heterogeneous group of disorders of
neuronal excitability arising from inherited and acquired
disturbances. Prevalence of epilepsy among women in India
is estimated to be 2.5 million (1),52% of them in their
reproductive age group(2). Women experience gender related
physical and social problems and are at the risk of seizures
during labor. A complex interaction between epileptic seizures
during pregnancy, antiepileptic drugs (AED), its adverse
impacts on the developing fetus, congenital malformations are
all being related. The risk of congenital malformation and
teratogenic effect of AED is of great concern.
controversial (5). Some studies show that there is increased
frequency of seizures during pregnancy (6, 7), while others
have shown that there is no increase in seizure frequency
during pregnancy and puerperium (8). Seizure activity or
seizure types do not appear to increase the risk of fetal
malformations (9, 10).A complex congenital malformation are
high in epileptic women who are on medication than among
offspring of untreated patients (8, 11-13).
Address for Correspondence :
Risk increases as the number of anti epileptic drugs increased
due to additive teratogenic effects. The risk of malformation
being higher in women on polytherapy as compared to
monotherapy (14-17). Excess risk was seen in patients using
sodium valproate either as monotherapy or sodium valporate
on poly therapy (13, 18), higher doses implicate with increased
risk. Children exposed to sodium valporate have significantly
lower IQ as compared with those with exposure to other AEDs
(13, 19). Infants born to mother with epilepsy on AEDs in utero
have increased risk of birth defects (10-12).
Prof. Sowbhagya Lakshmi
Govt. Medical College
Shimoga, Karnataka
Mob: 9880484310.
E-mail : sowlakh@rediffmail.com
Major anomalies may affect CNS, CVS and GI systems with
neural tube defects, anencephaly, spina bifida (20, 21),
Chromosomal abnormalities (22, 23) and neurophysiological
effect (19). However, recent studies have shown that there
Many studies have shown that children born to epileptic
mothers have malformations twice as often as children born
to non epileptic mothers (3, 4). The data often varies and is
267
Indian Journal of Clinical Biochemistry, 2008 / 23 (3)
was no significant difference in pregnancy complication in
cases as compared to controls in the incidence of perinatal
mortality, congenital malformations, except low birth weight
babies in cases (18,24,25) Recent reports have also shown
the possibility of AEDs to cause selective developmental
language deficits and Fetal Anti Convulsant Syndrome in
children.(3,19,23, 26-28).
There has been increased interest to establish biochemical
mechanisms and genetic factors in teratogenesis. Prenatal
diagnostic tests can identify the fetus with common major
malformations. Alfa Feto Protein (AFP) as a marker, aids in
detecting fetus with neural tube defects. Increase in AFP is
well known in hepatocellular carcinoma. (21), multiple
pregnancy and neural tube defects (29, 30). Low levels of
AFP are associated with molar pregnancy (31) and Downs
syndrome (32).
Teratogenic effect of AED may be mediated by the formation
of free radicals or by antifolate effects. Folic acid
supplementation helps to protect from congenital
malformations (17, 33) including neural tube defects (34).
Indian Registry of Epilepsy and Pregnancy (IREP) have
recommended 5mg folic acid per day throughout the
pregnancy.
AFP is a glycoprotein with molecular weight of 70,000 D formed
in yolk sac and non-differentiated liver cells, secreted to
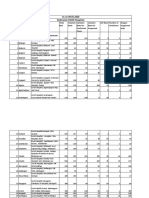
Table 1 : Age wise distribution and obstetric history of
cases and controls
Cases (n=30)
N
AED are known to induce cytochrome P450 enzyme system
in the liver, leading to the formation of rapid hepatic metabolites
of AED which may impair the normal liver functions. Renal
functions normally increases during pregnancy, AEDs may
further add on to aggravate the condition.
The study has been taken, to estimate maternal serum AFP
(MSAFP) levels, liver function tests and kidney function tests
in 12th -14 th week of epileptic pregnant women and controls.
They were subjected to ultrasonography at 11th-14th week of
pregnancy and again at 20th week of pregnancy, to determine
the obstetric and neonatal outcome in epileptic pregnancy as
compared to controls. Reports helps to identify the anomalies,
for timely information regarding AED mediated teratogenicity,
so that major birth defects can be taken care of in early stages.
MATERIALS AND METHODS
The present study was undertaken in the Department of
Biochemistry, Bowring and Lady Curzon Hospital attached to
Bangalore Medical College in collaboration with OBG
department. Thirty epileptic pregnant women below 35 years
of age served as cases and fifty age matched pregnant women
formed the control group, from middle and lower class families.
Both cases and controls were non-smokers, non-alcoholic and
they were on folate supplementation from the day of
confirmation of pregnancy. Folic acid of 0.4 mgs/day for
controls and 5mg/day for cases was prescribed.
Controls(n=50)
N
Age in years
20 25
17
56.67%
31
62%
26 30
11
36.67%
18
36%
> 30
02
6.67%
01
2%
Primigravida
18
60%
29
58%
Gravida 2
11
36.67%
17
34%
Gravida 3
01
3.33%
04
8%
FTND
26
86.67%
44
88%
LSCS
02
6.67%
04
8%
Preterm delivery
01
3.33%
00
IUD
00
01
2%
Abortion
01
3.33%
01
2%
Obstetric History
Outcome of pregnancy
Abbreviations: FTND=Full term normal delivery;
LSCS=Lower segment caesarian section; IUD= Intra uterine death.
268
amniotic fluid and into mothers blood. It reaches maximum in
about 13 14 week of pregnancy and falls continuously (35).
The cases were seizure free for the last one-year but were on
the base line monotherapy except for two cases who were on
drug combination (Table 2). None of them were on sodium
valporate, as its induced risk of teratogenicity is well
established either as monotherapy or as polytherapy.
Gestational age was calculated by counting the number of
complete weeks after last menstrual period. Diabetic and
hypertensive controls and cases were excluded from the study.
Cases and controls of 12 to 14 weeks of gestation were
subjected to various biochemical parameters. Maternal serum
was used to find the levels of glucose, total proteins, albumin,
bilirubin, SGOT, SGPT, alkaline phosphatase, cholesterol, urea
and creatinine. AFP was assayed by chemiluminisence assay
(ECLIA) method, which is a highly innovative detection
technology with enhanced sensitivity and specificity. The
method combines the conventional antigen antibody reaction
on surface of a Magnetic Microbead with Ruthenium complex.
Antiepileptic Drugs in Pregnancy
Table 2 : Particulars regarding onset of seizures and AED Protocol
Age of Onset
< 5 years
Number
Percentage
08
26.67%
5-10 years
18
60%
11-20 years
04
13.33%
AED protocol
Drugs
Dosage
Carbamazepine(CBZ)
14
400mg/day
Phenytoin
07
200mg/day
Phenobarbital (PB)
07
120mg/day
PB+CBZ
28
93.33%
02
6.67%
6mg/day(PB)+
400mg/day(CBZ)
ECLIA is a process in which highly reactive species are
generated from stable precursors at the surface of an
electrode. Congenital abnormalities were assessed by detailed
ultrasonography targeting foetal organogenesis, between 11th
-14th week of pregnancy and again at 20th week of pregnancy.
Neonatologists service was taken to detect congenital
abnormalities.
Students t test was used to find the statistical significance.
The protocol of the study was to refer women to amniocentesis
for estimation of amniotic fluid AFP levels, chromosomal study
and 3 D ECHO in the following conditions-1. When the MSAFP
levels were more than normal levels? 2. When skeletal and
soft tissue anomalies were detected? 3. When the heart
chambers and the out flow track of fetus was abnormal. This
is to narrow down the group of women of high risk, for further
higher invasive diagnostic tests, so that AED mediated
teratogenesis can be detected early which aids in effective
management by counseling the parents for selective
termination and to confirm the diagnosis on the aborted fetus.
RESULTS AND DISCUSSION
The results obtained in the present study are presented in
Tables 1-5. Epidemiological study has shown 2.5 million
women with epilepsy in India (1). The findings of the
complications during pregnancy and its outcome are
controversial. Some studies have shown increase in seizures
during pregnancy with epilepsy(6,7) while some studies have
shown no increase in seizure during pregnancy and perpeurim
(8).Chances of risk with AEDs are more, the risk being higher
with polytherapy as compared to monotherapy (14-17). Sodium
valporate either as monotherapy or as poly therapy increases
the risk of foetal malformations (13, 18). Recent studies have
shown no significant difference between cases and controls
in pregnancy complications and perinatal mortality
(18, 24, 25).
There was no significant difference in liver function tests and
kidney function tests in cases as compared to controls (Table
3 and 4). There was increase in MSAFP levels in cases as
compared to controls but not statistically significant and its
levels were found to be independent of the type of AED used.
No congenital abnormalities were seen in the newborn. There
were no complications either during pregnancy or during labor
with no difference in neonatal outcome in cases as compared
with controls (Table 1) except low birth weight babies in cases
(Table 5) in accordance to the finding of others (18, 24, 25).
The beneficial effect may be due to folic acid supplementation
(5mg/day) through out pregnancy. Folic acid is needed for
DNA replication. It is an important vitamin involved in one
carbon transfer and has a major role in amino acid, purine
and pyrimidine metabolism. Any interference in this metabolism
may affect normal development especially in rapidly
proliferative embryonic tissues including post transcriptional
modification. Folic acid is known to reduce the incidence of
neural tube defects (34), congenital defect can be reduced by
perioconceptual folate supplementation (16, 33, 34). Low birth
weight in children may be due to intrauterine growth retardation
by AED.
Most of the patients (93.33%) in this study were on base line
monotherapy (Table 2), the children born to cases were normal,
without any congenital malformations in agreement with other
studies. Monotherapy was found to reduce the overall
prevalence of malformation, as the additive teratogenic effects
of AED (polytherapy) are considerably reduced (14-17).
Teratogenic effect of AED may be mediated by the formation
of free radicals or by antifolate effects. The relationship
Table 3 : Liver function tests of cases and control
Group
Total Protein
Cases (n=30)
5.680.36*
Controls (n=50)
6.410.34
Albumin
Bilirubin
SGOT
3.140.36*
0.60.16*
20.63.38*
3.50.45
0.40.14
25.5454
SGPT
Alk.Phosphatase
22.562.8*
125.66 21.33*
22.264.7
117.021.89
Results are expressed as mean SD; *Not Significant
269
Indian Journal of Clinical Biochemistry, 2008 / 23 (3)
Table 4 : Plasma levels of sugar, urea, creatinine, cholesterol and MSAFP levels in cases and controls
Group
Sugar
Urea
Creatinine
Cholesterol
MSAFP
Cases (n=30)
87.485.5*
25.225.5*
0.710.15*
164.06.9*
29.958.7**
Controls (n=50)
83.027.15
22.764.2
0.60.17
163.017.5
25.725.19
Results are expressed as mean SD; * Not Significant ** P < 0.1
between AFP levels, epileptic pregnancy and congenital
malformations is therefore unclear.
Epilepsy raises special concern in women especially during
pregnancy. AED are known to induce major and minor
malformation in the fetus. The study was aimed in detecting
AED mediated teratogenesis. No congenital abnormalities
were seen in the newborn except they were low birth weight.
The beneficial effect may be due to folic acid supplementation,
which plays a major role in nucleic acid metabolism.
Table 5 : Birth weight of new born children of
cases & controls
Birth Weight
Cases(n=30)
REFERENCES
1.
Sridaran R, Murthy BN. Prevalence and pattern of epilepsy
in India. Epilepsia 1999; 40:631-6.
2.
World population Prospects: The 2004 Revision and world
urbanization Prospects.
3.
Gaily E, Kanota-Sorsa E, Hillesmaa V. Normal intelligence
in children with prenatal exposure to carbamazepine.
Neurology 2004; 62:28-32.
4.
Meador KJ, Zupang ML. Neurodeveopmental outcome of
children born to mothers with epilepsy. Cleve Clin J Med
2004; 71:38-41.
5.
Marrow JJ, Graig JJ. Antiepileptic drugs in pregnancy.
Current safety and other issues. Exp Opin Pharmacother
2003; 4: 445-56.
6.
Knight AH, Rhind EG. Epilepsy and pregnancy. A study of
153 pregnancies in 59 patients. Epilepsia 1975; 16: 99-110.
7.
Yerby MS. Pregnancy and epilepsy. Epilepsia 1991; 32:
51-9.
8.
Costa Al, Lopes-Cendes I, Guerreiro CA. Seizure frequency
during pregnancy and the puerperium. Inter J Gynaecol
Obstet 2005; 88:148-9.
9.
Batino D, Binclli S, Caccamo ML. Malformations in the
offsprings of 305 epileptic women, a prospective study. Acta.
Neurol Scand 1992; 85: 204 07.
Controls(n=50)
< 2.5 kg
26
86.67%
05
10%
2.5 3 kg
03
10%
27
54%
3 3.5 kg
16
32%
The study was on small number of epileptic patients on
baseline monotherapy. Further research must be aimed in
multivariate analysis of risk factors on large population. Several
other factors unrelated to AEDs such as consanguinity, genetic
factors, socioeconomic status and nutritional factors have to
be correlated before coming to conclusion. Epidemiological
data along with retrospective study of data of epileptic pregnant
women is essential to correlate the effect of monotherapy/
polytherapy, dosage of drugs to congenital malformations.
Large population study and long term prospective follow up
for neurological development of the children is needed before
coming to any conclusion. Estimation of Red cell folate along
with the measure of proportions of unbound AED to bound
AED in different AED regime is our plan for future study to
elucidate the role of drugs and its dosage in implicating fetal
anomalies.
10. Kaneko S, Battino D, Andermann E, Wada K, Kan R, Takeda
A, Nakane Y,et al. Congenital malformations due to
antiepileptic drugs. Epilepsy Res 1999; 33:145-58.
11. Prolifka JE, Friedman JMJ. Medical genetics, Clinical
teratology in the age of genomics. C M A J 2002; 167:
265-73.
12. Holmes LB, Wyszynski DF, Lieberman E.The AED pregnancy
register, 6 year experience. Arch Neuro 2004; l61:163-7.
13. Artama MA, Raudaskoski T, Isojarvi JIT, Raitanen J, Auvinen
A. Antileptic drug use of women with epilepsy and congenital
malformation of offspring. Neurology 2005; 64:1874-8.
14. Samreen EB, VanDuijn CM, Christiaens GC, Hofman A, Dick
Lindhout. Antiepileptic drug regimens and major congenital
abnormalities in the offspring. Ann Neurol 1999; 46: 739-46.
15. Meischenguiser R, DGiano CH, Ferraro SM. Oxcarbazepine
in pregnancy, Clinical experience in Argentina. Epilepsy
Behav 2004; 5:163-7.
270
Antiepileptic Drugs in Pregnancy
16. OBrien MD, Gilmour-White SK. Management of epilepsy in
women. Postgrad Med J 2005; 81:278-85.
17. Perucca E. Birth defects af ter prenatal exposure to
antiepileptic drugs. Lancet Neurol 2005; 4: 781-6.
18. Marrow J, Russel A, Gutthrie E, Parson L, Robertson I,
Woddell R, Irwin B. Malformation risks of antiepileptic drugs
in pregnancy. A prospective study from U.K Epilepsy and
pregnancy register. J N N P 2006; 77:193-8.
19. Vinten J, Adab N, Kini U, Gorry J, Gregg J, Baker GA.
Neurophysiological effects of exposure to anti convulsant
medication in utero. Neurol 2005; 64:949-54.
20. Rosa FW. Spina bifida in infants of women treated with
carbamezapine during pregnancy. N Engl J Med 1991;
324:674-7.
21. King PB, Lie RT, Iegene LM. Spina bifida and cleft lip among
newborn of Norwegian women with epilepsy. Changes
related to the use of anticonvulsant. Am J Public Health 1996;
86:1454-6.
22. Simpson JL, Baum LD, Marder R, Elias S, Ober C, Martin
AO. Maternal serum AFP screening : Low and high values
for detection of genetic abnormalities. Am J Obstet Gynaecol
1986; 155: 593-7.
23. Thomas SV, Indrani L, Devi GC, Jacob S, Beegum J, Jacob
P, Kesavadas K, Radhakrishnan K, Sarma PS. Pregnancy
in women with epilepsy, preliminary results of Kerala registry
of epilepsy and pregnancy. Neurol India 2001; 49:60-6.
24. Goel P, Devi L, Saha PK, Takkar N, Haria A, Dua D. Maternal
and perinatal outcome in pregnancy with epilepsy. Internet
J Gynaecol Obst 2006;5: 2-12.
25. Viinikainen K, Heinonen S, Eriksson K, Kalviainen R.
Community-based, prospective, controlled study of obstetric
and neonatal outcome of 179 pregnancies in women with
epilepsy. Epilepsia 2006; 47:186-92.
26. Wide K, Winbladh B, Kallen B. Major malformations in infants
exposed to antiepileptic drugs in utero, with emphasis on
carbamazepine and valproic acid: A nationwide, populationbased register study. Acta Paediatr 2004; 93: 174-6.
27. Alsdorf R, Wyszynski D F. Teratogenicity of Sodium
Valproate. Expert Opinion on Drug Safety 2005; 2:345-53.
28. Wyszynski DF, Nambisan M, Surve T, Alsdorf RM, Smith
CR. Antiepileptic drug Pregnancy registry .Increased rate of
major malformations in offspring exposed to valproate during
pregnancy. Neurology 2005; 64:961-5.
29. Cuckle H, Wald N, Stevenson JD, May HM, Ferguson-Smith
MA, Ward AM, et al. Maternal serum alpha-fetoprotein
screening for open neural tube defects in twin pregnancies.
Prenatal diagnosis 1990; 10: 71-7.
30. Thomas SV. Management of epilepsy and pregnancy. J
Postgraduate Med 2006; 52:57-64.
31. Kaur M, Verma IC. Serum AFP screening in high-risk
pregnancies. Ind J Pead 1995; 62: 10107.
32. Burton BK. Outcome of pregnancy in patients with
unexplained increased and decreased levels of maternal
serum AFP. Obstet Gynaecol 1988; 72:709-13.
33. De Wals P, Tairou F, VanAllen MI, SH Uh, Lowry RB.
Reduction in neural tube defects after folic acid fortification
in Canada. N Eng J Med 2007; 35:135-42.
34. Shaw G M, Schaffer D, Ellen MV, Kimberly Morland, John
AH. Periconceptional vitamin dietary folate and the
occurrence neural tube defects.Epidemiology 1995; 6:
219-26.
35. Brewer TA, Tanks ES. Yolk sac tumor and AFP in first year
life. Urology 1993; 42, 79 80.
271
You might also like
- All India Institute of Medical Sciences, Nagpur Result NotificationDocument4 pagesAll India Institute of Medical Sciences, Nagpur Result NotificationNayan ChaudhariNo ratings yet
- 1150 Medical (Only PG DM - MCH) Latest 26 - 02 - 20Document2 pages1150 Medical (Only PG DM - MCH) Latest 26 - 02 - 20Nayan ChaudhariNo ratings yet
- Notification 16 - 01 - 20Document3 pagesNotification 16 - 01 - 20Nayan Chaudhari100% (1)
- Organization: U.S. Food and Drug Administration (FDA)Document2 pagesOrganization: U.S. Food and Drug Administration (FDA)Nayan ChaudhariNo ratings yet
- Notification 16 - 01 - 20Document3 pagesNotification 16 - 01 - 20Nayan Chaudhari100% (1)
- 1 Short Report 1: Vivax Malaria Resistant To Chloroquine: Case Reports From BombayDocument2 pages1 Short Report 1: Vivax Malaria Resistant To Chloroquine: Case Reports From BombayNayan ChaudhariNo ratings yet
- Faculty Advertisement 4 202001 1Document7 pagesFaculty Advertisement 4 202001 1Akshay DateyNo ratings yet
- Notes On Economics ChecklistDocument10 pagesNotes On Economics ChecklistNayan ChaudhariNo ratings yet
- Name Conversion: Folder Name OCR LanguageDocument1 pageName Conversion: Folder Name OCR LanguageNayan ChaudhariNo ratings yet
- All India Institute of Medical Sciences, Nagpur Result NotificationDocument4 pagesAll India Institute of Medical Sciences, Nagpur Result NotificationNayan ChaudhariNo ratings yet
- Report GovtDocument5 pagesReport GovtNayan ChaudhariNo ratings yet
- Introduction To TheoryDocument8 pagesIntroduction To TheoryNayan ChaudhariNo ratings yet
- Youanewowec? Here Are The Next StepsDocument3 pagesYouanewowec? Here Are The Next StepsNayan ChaudhariNo ratings yet
- Pharmacoeconomics PHAR 773 Winter Quarter, 2004Document3 pagesPharmacoeconomics PHAR 773 Winter Quarter, 2004Nayan ChaudhariNo ratings yet
- JBI - Critical Appraisal - Checklist - For - Randomized - Clinical - Trial 2017Document9 pagesJBI - Critical Appraisal - Checklist - For - Randomized - Clinical - Trial 2017M Vecdi GecinNo ratings yet
- D Mer Bond Resp Once SheetDocument2 pagesD Mer Bond Resp Once SheetNayan ChaudhariNo ratings yet
- Article 4Document11 pagesArticle 4Nayan ChaudhariNo ratings yet
- AbstractFilePath 2 PDFDocument3 pagesAbstractFilePath 2 PDFNayan ChaudhariNo ratings yet
- Glossary of Clinical Trials TermsDocument7 pagesGlossary of Clinical Trials TermsNayan ChaudhariNo ratings yet
- Fellowship in OncotherapeutDocument3 pagesFellowship in OncotherapeutNayan ChaudhariNo ratings yet
- WIPO Patent PrimerDocument38 pagesWIPO Patent PrimerSrinivasan ShanmugamNo ratings yet
- Admission Notice For Govt Sponsored Teachers of The North-Eastern StatesDocument1 pageAdmission Notice For Govt Sponsored Teachers of The North-Eastern StatesNayan ChaudhariNo ratings yet
- Guideline On Good Pharmacovigilance Practices (GVP) Module IX - Signal Management (Rev. 1)Document25 pagesGuideline On Good Pharmacovigilance Practices (GVP) Module IX - Signal Management (Rev. 1)Salló TivadarNo ratings yet
- Socio-Economic Status Scales Updated For 2017: Educational ForumDocument4 pagesSocio-Economic Status Scales Updated For 2017: Educational ForumNayan ChaudhariNo ratings yet
- GR 2008 Medical BondDocument5 pagesGR 2008 Medical BondKishore Rambhau SonkusareNo ratings yet
- Theorem BayesDocument4 pagesTheorem BayesNayan ChaudhariNo ratings yet
- Fellowship in OncotherapeuticsDocument4 pagesFellowship in OncotherapeuticsDrPallavi DNo ratings yet
- New Challenges in Pharmacovigilance - 1 PDFDocument1 pageNew Challenges in Pharmacovigilance - 1 PDFNayan ChaudhariNo ratings yet
- Manual of Drug Safety and PharmacovigilanceDocument1 pageManual of Drug Safety and PharmacovigilanceNayan ChaudhariNo ratings yet
- Postexposure Treatment of Rabies Infection: Can It Be Done Without Immunoglobulin?Document4 pagesPostexposure Treatment of Rabies Infection: Can It Be Done Without Immunoglobulin?Nayan ChaudhariNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- QUES2-1 Stir Not The World's DoomDocument49 pagesQUES2-1 Stir Not The World's DoomNicholas LouieNo ratings yet
- Pharmaceutical CareDocument114 pagesPharmaceutical CareRisdaFitriaNo ratings yet
- Nursing Care Plan: Student's Name: ID: Course Name: SettingDocument3 pagesNursing Care Plan: Student's Name: ID: Course Name: SettingnjoodNo ratings yet
- Giardia M.SC PDFDocument18 pagesGiardia M.SC PDFRahul ChaudharyNo ratings yet
- Sociology PresentationDocument31 pagesSociology PresentationNirbhay SinghNo ratings yet
- Introduction To Antiviral Drugs For Influenza: David Shay Influenza Branch Centers For Disease Control & PreventionDocument36 pagesIntroduction To Antiviral Drugs For Influenza: David Shay Influenza Branch Centers For Disease Control & PreventionAmal AljabriNo ratings yet
- Apraxia of Speech and Grammatical Language Impairment in Children With Autism Procedural Deficit HypothesisDocument6 pagesApraxia of Speech and Grammatical Language Impairment in Children With Autism Procedural Deficit HypothesisEditor IJTSRDNo ratings yet
- Artikel Bahasa Inggris Tentang Kesehatan LingkunganDocument2 pagesArtikel Bahasa Inggris Tentang Kesehatan LingkunganYolanda SefraniNo ratings yet
- Rhinitis MedicamentosaDocument22 pagesRhinitis MedicamentosaDanti NurdindayantiNo ratings yet
- A Biological Profile For Diagnosis and Outcome of COVID-19 PatientsDocument10 pagesA Biological Profile For Diagnosis and Outcome of COVID-19 PatientsAristidesNo ratings yet
- A Review On Herbal Drugs Used in The Treatment of COVID-19.Document15 pagesA Review On Herbal Drugs Used in The Treatment of COVID-19.Samiksha SarafNo ratings yet
- List COVID Facilities State OdishaDocument3 pagesList COVID Facilities State OdishadrjyotivetNo ratings yet
- CholestyramineDocument1 pageCholestyramineKatie McPeekNo ratings yet
- Pakpak LawinDocument16 pagesPakpak Lawinmaylene estoque0% (1)
- Spine Magnetic Resonance Image Segmentation Using Deep Learning TechniquesDocument6 pagesSpine Magnetic Resonance Image Segmentation Using Deep Learning TechniquesSandeep VermaNo ratings yet
- A Review of Fluid and Hydration in Competitive TennisDocument11 pagesA Review of Fluid and Hydration in Competitive TennisSilvio DantasNo ratings yet
- The Role of Neuroglia in AutismDocument30 pagesThe Role of Neuroglia in AutismWesley M.SantosNo ratings yet
- Warming Center New HavenDocument3 pagesWarming Center New HavenHelen BennettNo ratings yet
- Obg FormatDocument17 pagesObg Formatarchana vermaNo ratings yet
- Conoco Bentone Grease MSDSDocument6 pagesConoco Bentone Grease MSDSJas SumNo ratings yet
- US Army Medical Pharmacology IDocument202 pagesUS Army Medical Pharmacology ISpace_Hulker100% (2)
- Bee Empowerment Leslie WilsonDocument6 pagesBee Empowerment Leslie Wilsonchakravartys1327100% (1)
- Export Act 1963Document27 pagesExport Act 1963Anonymous OPix6Tyk5INo ratings yet
- Natural Medicine IODINE by Sue Visser.4810627Document3 pagesNatural Medicine IODINE by Sue Visser.4810627relativelabs2075No ratings yet
- The Importance of Mineral Elements For Humans, Domestic Animals and Plants: A ReviewDocument3 pagesThe Importance of Mineral Elements For Humans, Domestic Animals and Plants: A ReviewMaricel Canlas MacatoNo ratings yet
- 2018 - ICRU 83 - BaliDocument86 pages2018 - ICRU 83 - BalisanggamNo ratings yet
- Impaction in Dairy Animals: Ashwani KumarDocument6 pagesImpaction in Dairy Animals: Ashwani KumarGiriNo ratings yet
- Case Taking ProformaDocument7 pagesCase Taking ProformaDr Dushyant Kamal Dhari50% (2)
- Newport International Journal of Scientific and Experimental Sciences (Nijses) Volume 3 Issue 2 2023Document8 pagesNewport International Journal of Scientific and Experimental Sciences (Nijses) Volume 3 Issue 2 2023KIU PUBLICATION AND EXTENSIONNo ratings yet
- Hex A Chloro But A DieneDocument15 pagesHex A Chloro But A DieneAfraNo ratings yet