Professional Documents
Culture Documents
SVT
Uploaded by
kennethfarnumOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SVT
Uploaded by
kennethfarnumCopyright:
Available Formats
582
Heart 1998;79:582587
Ventriculo-atrial time interval measured on
M mode echocardiography: a determining
element in diagnosis, treatment, and prognosis of
fetal supraventricular tachycardia
E Jaeggi, J C Fouron, A Fournier, N van Doesburg, S P Drblik, F Proulx
Fetal Cardiology Unit,
Department of
Paediatrics,
Sainte-Justine
Hospital, University of
Montreal, 3175 Cte
Ste Catherine,
Montreal, Quebec H3T
1C5, Canada
E Jaeggi
J C Fouron
A Fournier
N van Doesburg
S P Drblik
F Proulx
Correspondence to:
Dr Fouron.
email: fouronj@
ere.umontreal.ca
Accepted for publication
18 November 1997
Abstract
ObjectiveTo determine whether M mode
echocardiography can diVerentiate fetal
supraventricular tachycardia according to
the ventriculo-atrial (VA) time interval,
and if the resulting division into short and
long VA intervals holds any relation with
clinical presentation, management, and
fetal outcome.
DesignRetrospective case series.
Subjects23 fetuses with supraventricular tachycardia.
Main outcome measuresA systematic
review of the M mode echocardiograms
(for VA and atrioventricular (AV) interval
measurements), clinical profile, and final
outcome.
Results19 fetuses (82.6%) had supraventricular tachycardia of the short VA type
(mean (SD) VA/AV ratio 0.34 (0.16); heart
rate 231 (29) beats/min). Tachycardia was
sustained in six and intermittent in 13.
Hydrops was present in three (15.7%).
Digoxin, the first drug given in 14, failed
to control tachycardia in five. Three of
these then received sotalol and converted
to sinus rhythm. All fetuses of this group
survived. Postnatally, supraventricular
tachycardia recurred in three, two having
WolV-Parkinson-White syndrome. Four
fetuses (17.4%) had long VA tachycardia
(VA/AV ratio 3.89 (0.82); heart rate 226
(10) beats/min). Initial treatment with
digoxin was ineVective in all, but sotalol
was eVective in two. Heart failure caused
fetal death in one and premature delivery
in one. All three surviving fetuses had
recurrences of supraventricular tachycardia after birth: two had the permanent
form of junctional reciprocating tachycardia and one had atrial ectopic tachycardia.
ConclusionsCareful measurement of
ventriculo-atrial intervals on fetal M
mode echocardiography can be used to
distinguish short from long VA supraventricular tachycardia and may be helpful in
optimising management. Digoxin, when
indicated, may remain the drug of choice
in the short VA type but appears ineVective in the long VA type.
(Heart 1998;79:582587)
Keywords: fetus; supraventricular tachycardia;
ventriculo-atrial interval; digoxin
Supraventricular tachycardia is the most commonly reported type of fetal tachycardia1 2 and
may be associated with cardiac decompensation,
manifested by ascites, pleural eVusion, pericardial eVusion, anasarca, and death.35 It usually
requires aggressive treatment to restore sinus
rhythm, thus eliminating the risk of cardiac failure. The most common mechanism that underlies supraventricular tachycardia in neonates and
older children (excluding sinus tachycardia) is
reentry, accounting for about 90% of all narrow
QRS tachycardia.6 7 In infants, reentry circuits
most often occur through accessory atrioventricular (AV) connections, while reentry within
the AV node is less often observed.810 In typical
reentry supraventricular tachycardia, antegrade
conduction through the AV node is slow, while
retrograde pathways show fast conducting properties. On the ECG, retrograde atrial activation
occurs shortly after the QRS complex and thus
yields a short retrograde pathway tachycardia.7 In
other and less common forms of narrow QRS
tachycardia, the retrograde limb shows slow
conduction properties and results in a long retrograde pathway tachycardia; this is the case in the
permanent form of junctional reciprocating
tachycardia, which is also the most commonly
observed type of long retrograde pathway
tachycardia.11 In atrial ectopic tachycardia there
is no reentry circuit and the P wave always precedes the QRS complex, resulting in a short PR
interval and a long RP interval. This type of
arrhythmia is very uncommon in infancy.12 The
permanent form of junctional reciprocating
tachycardia and atrial ectopic tachycardia are
usually incessant and tend to be unresponsive to
most antiarrhythmic agents.13 Thus the further
diVerentiation of fetal supraventricular tachycardias into those with long and short retrograde
pathways could be useful for optimal treatment.
In this study, we investigated whether careful
measurements
of
atrioventricular
and
ventriculo-atrial (VA) intervals on M mode
echocardiograms recorded during fetal tachycardia could help establish the type of VA interval associated with the tachycardia, and whether
this distinction is relevant to the clinical presentation, management, and outcome of the
aVected fetuses.
Methods
DEFINITIONS
Intrauterine supraventricular tachycardia
was defined by a 1:1 AV conduction relation
with a heart rate of more than 180 beats/min
and little or no beat to beat variation.
583
Fetal supraventricular tachycardia
Supraventricular tachycardia was considered
sustained when observed permanently or when
present for more than 50% of the time
required for the echocardiographic examination (approximately 45 minutes); it was classified as intermittent if the tachycardia lasted
less than 50% of the time. The diagnosis of
congestive heart failure was based on the presence of cardiomegaly and fluid accumulation
in at least one of the pleural, pericardial, or
abdominal cavities. The diagnosis of tachycardia related cardiomyopathy was made when
marked thickening and hyperechogenicity of
the myocardium were associated with poor
contractility. Diagnosis of hydrops fetalis required the presence of fluid collections in at
least two of the abdominal, pleural, or pericardial spaces and/or anasarca.5 In this clinical
situation, it was considered to represent an
advanced state of cardiac failure. After birth,
the diagnosis of the permanent form of
junctional reciprocating tachycardia and atrial
ectopic tachycardia was made according to the
electrocardiographic and clinical criteria reported previously.12 1416
CLINICAL MATERIAL
Figure 1 Measurement of ventriculo-atrial time interval on M mode echocardiography
during fetal supraventricular tachycardia. Examples of a long (panel A) and short (panel
B) ventriculo-atrial time intervals are shown. A, atrium; V, ventricle.
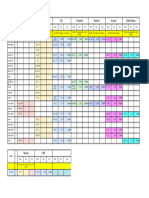
Table 1
All cases of fetal supraventricular tachycardia
seen between 1988 and 1995 at our fetal cardiology unit were systematically reviewed. Atrial
flutter and multifocal tachycardia were excluded from the study. Fetuses who where
already on antiarrhythmic treatment before the
first echocardiographic study were also excluded. Supraventricular tachycardia was
documented in 27 subjects on at least one
Summary of patient characteristics with short and long VA interval
GA at
detection
Max HR
(beats/min)
Pattern of
SVT
Sign of
CHF
Short VA SVT
1
0.55
2
0.52
26
35
240
200
Sustained
Sustained
H
No
3
4
5
6
7
8
9
10*
11
12
13*
14
15
16
17
18
19
0.34
0.22
0.33
0.3
0.44
0.22
0.49
0.32
0.15
0.63
0.44
0.07
0.35
0.33
0.55
0.05
0.16
31
30
31
25
34
31
20
32
38
38
25
36
30
32
28
26
32
288
214
187
192
200
219
218
229
222
230
230
272
214
250
260
232
285
Intermittent
Intermittent
Intermittent
Sustained
Intermittent
Intermittent
Intermittent
Intermittent
Intermittent
Sustained
Intermittent
Sustained
Intermittent
Intermittent
Intermittent
Intermittent
Sustained
No
No
No
No
No
PE
No
No
No
No
No
No
No
No
H,CMP
No
H
Mean (SD)
0.34 (0.16)
30.5 (4.7)
230.6 (29)
Long VA SVT
20
21
3.13
3.33
24
27
234
235
22
23
4.23
4.89
29
34
220
216
Mean (SD)
3.89 (0.82)
28.5 (4.2)
226 (9.7)
Case
VA/AV ratio
Treatment in utero
GA at birth Treatment postnatal
SVT
postnatal
ECG
40
37
S(+)
Propr(+)
Yes/reentry
No
WPW
WPW
40
40
41
40
40
40
40
33
40
38
38
39
39
38
32
39
35
No
No
D(+)
D(), S(+)
No
D(+)
D(+)
No
No
D(+)
No
D(+)
No
D(+)
D(+)
No
S(+)
No
No
No
Yes/reentry
No
No
No
No
No
No
No
No
No
No
No
No
Yes/reentry
Normal
Normal
Normal
Normal
Normal
Normal
Normal
Normal
Normal
WPW
Normal
Normal
RVH
Normal
Normal
Normal
WPW
3/19
D(), S(+)
D(); V(),
delivery
D(+)
D(); S(+)
D(+)
D(+)
No
D(+)
D()
No
No
No
D(+)
D(+)
D(+)
D(+)
D(+), delivery
No
D(), S(+),
delivery
(+) = 17/19
Sustained
Sustained
H,CMP
No
D(), Ad(), S(+) Death iu
D(), S(), delivery 36
Sustained
Sustained
No
CMP
D(), S(+)
D(), delivery
40
35
2/4
(+) = 2/4
37 (2.6)
38.4 (2.5)
3/14
D(), S(),
Yes/PJRT
Flec(), Pf(+)
D(), S(+)
Yes/PJRT
D(), Ad(),
Yes/AET
EC(), Am(+), Pf(+)
3/3
Normal
Normal
Normal
Drug eVects: (), no rhythm control; (+), rhythm control.
*Twin pregnancy; tetralogy of Fallot.
CHF, congestive heart failure; CMP, cardiomyopathy; GA, gestational age in weeks; H, hydrops; HR, maximum heart rate before treatment; iu, in utero; PE, pericardial eVusion, RVH, right ventricular hypertrophy; SVT, supraventricular tachycardia; WPW, WolV-Parkinson-White syndrome; PJRT, permanent form of junctional
reciprocating tachycardia; AET, atrial ectopic tachycardia.
Ad, adenosine; Am, amiodarone; D, digoxin; EC, electroconversion; Flec, flecainide; Pf, propafenone; Propr, propranolol; S, sotalol; V, verapamil.
584
Jaeggi, Fouron, Fournier, et al
two standard deviations above the mean for
gestational age.17
The clinical records of each of these fetuses
was then reviewed for the following variables:
gestational age at detection of supraventricular
tachycardia, maximum heart rate before treatment, presence of congestive heart failure, type
of initial treatment and response, the need for
more than one drug, and recurrence of
supraventricular tachycardia on follow up.
Postnatal evaluation included gestational age at
birth, presence of cardiac malformations, and
an electrocardiographic study during sinus
rhythm and, when present, during episodes of
tachycardia.
According to our management protocol,
antiarrhythmic treatment with maternal digoxin was indicated when congestive heart
failure or sustained supraventricular tachycardia was present. Mothers received loading
doses of 2 mg digoxin over a two day period,
followed by a maintenance dose of 0.5 to
0.75 mg daily, adjusted to maintain maternal
digoxin concentrations near 2 nmol/l. If digoxin appeared to be ineVective after eight days
of treatment, oral sotalol (80 to 160 mg twice a
day) was added in fetuses younger than 35
gestational weeks, or the pregnancy was
electively terminated when the fetus was older.
DATA ANALYSIS
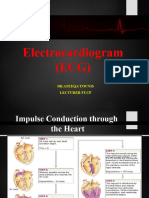
Figure 2 (A) Example of simultaneous M mode echocardiogram and ECG recordings
during a neonatal reentry supraventricular tachycardia. Arrows mark peaks of P waves.
Vertical lines mark mechanical ventricular and atrial events. The ECG shows a short RP
supraventricular tachycardia of 260 beats/min with 1:1 AV conduction, an RP interval of
95 ms, and a PR interval of 135 ms, leading to an electrical RP/PR ratio of 0.7. The M
mode echocardiogram indicates a corresponding short VA tachycardia with a VA interval of
80 ms, an AV interval of 150 ms, and a mechanical VA/AV ratio of 0.53. (B) Electrocardiographic demonstration of pre-excitation (WolV-Parkinson-White syndrome) after
termination of the supraventricular tachycardia in the same neonate (case 19). IVS,
interventricular septum; LA, left atrium; MV, mitral valve; RV, right ventricle.
echocardiogram. Four cases were excluded for
one of the reasons mentioned.
PROCEDURES
Fetal echocardiographic imaging and M mode
examinations were performed with 3.5 and 5.0
MHz transducers using either an HP Sonos
100 (Hewlett-Packard, Palo Alto, California,
USA) or an Acuson Computed Sonographic
machine model 128XP/10c (Acuson, Mountain View, California, USA). The M mode
tracings of the 23 remaining fetuses recorded
before any drug treatment were reviewed
blindly by an experienced echocardiographer
(EJ) not aware of the clinical history and the
outcome of the patients.
Guided by bidimensional real time imaging,
it was always possible to direct the M mode
ultrasound beam simultaneously through the
atrial and ventricular walls. VA and AV
intervals, analogous to the RP and PR intervals
of the extrauterine electrocardiogram, were
measured at peak atrial and ventricular systolic
wall motions. A long VA tachycardia was
defined by a VA/AV ratio above 1. The cardiothoracic ratio was obtained on the four
chamber view by dividing the cardiac by the
thoracic circumferences. Cardiomegaly was
defined as a cardiothoracic ratio greater than
Patients were divided into two groups based on
the presence of short or long VA intervals during fetal tachycardia. The Student t test was
used to compare means, while the Fisher exact
test was used to analyse categorical variables.
Statistical significance was set at p = 0.05.
Results
M mode echocardiograms allowed the identification of 19 fetuses with a short VA interval,
with a mean (SD) VA/AV ratio of 0.34 (0.16),
and four with a long VA interval, with a mean
VA/AV ratio of 3.89 (0.82) (p < 0.003). The
intra- and interobserver variabilities on 40
measurements
were
13.1(14.1)%
and
16.6(13.9)% for VA, and 7.5(5.3)% and
10.2(6.6)% for AV, respectively. Figure 1 shows
an example of the M mode echocardiograms
recorded from each group. The clinical presentation, management, and outcome are presented in table 1.
CLINICAL PRESENTATION
The two groups of fetuses did not diVer
significantly in mean gestational age at detection of supraventricular tachycardia (30.5
(4.7) v 28.5 (4.2) weeks for the short and long
VA interval groups, respectively) and heart
rate before medical treatment (230.6 (29) v
226 (10) beats/min). The initial ultrasound
examinations showed an intermittent tachycardia in 13 of the 19 fetuses (68%) with a
short VA interval. Supraventricular tachycardia
with a short VA interval led to hydrops in three
cases, with cardiomyopathy in one. One
cardiac malformation was observed in the
short VA group. In contrast, all four fetuses
with long VA intervals showed the same pattern
of sustained tachycardia. This diVerence was
Fetal supraventricular tachycardia
585
Figure 3 (A) Electrocardiogram of one of the neonates with permanent form of junctional reciprocating tachycardia: limb leads I, II, III, aVR, aVL, aVF
in full standardisation; narrow QRS tachycardia at 180 beats/min with l:l AV relation; long RP, short PR; negative P waves in II, III, and aVF. (B) Atrial
ectopic tachycardia: limb leads I, II, III, aVR, aVL, aVF in full standardisation, narrow QRS tachycardia at 180 beats/min with l:l AV relation; long RP,
short PR; abnormal P wave morphology and axis.
statistically significant (p < 0.003). Two
fetuses in this group showed evidence of
tachycardia induced cardiomyopathy.
FETAL MANAGEMENT AND OUTCOME
Short VA group
Drug treatment was indicated in 14 of the 19
fetuses in the short VA group. Digoxin, always
the first drug given, successfully controlled
tachyarrhythmia in nine fetuses (64%), while it
failed to convert the tachycardia in five (cases
1, 2, 4, 9, and 19). In three instances (cases 1,
4, and 19) conversion to sinus rhythm was
achieved before delivery by adding sotalol.
Case 9 presented with intermittent supraventricular tachycardia, which persisted despite
digoxin treatment but never showed signs of
cardiac failure.
In four cases from this group, pregnancy had
to be terminated prematurely, twice (cases 10
and 17) for maternal reasons. Patient 19 had to
be delivered despite conversion to sinus rhythm
with sotalol because of evidence of restrictive
foramen ovale causing hypodevelopment of the
left ventricle. Fetus 2 was at 35 weeks gestation
at the time of diagnosis and was the only case
delivered prematurely for lack of response to
antiarrhythmic treatment.
In this group, drug treatment was considered
unjustified in five fetuses, either because of the
intermittent nature of the tachycardia (cases 7,
10, 11, and 18) or because the diagnosis was
made close to term and the fetus delivered
before treatment (case 12). No patient in this
group presented signs of congestive heart
failure at birth.
After birth, eight infants with short VA
remained on digoxin treatment for up to 12
months, while propranolol was given in one
and sotalol in two. Recurrence of supraventricular tachycardia occurred in three infants
(cases 1, 6, and 19), two of whom had
WolV-Parkinson-White syndrome. Surface
ECGs showed WolV-Parkinson-White in four
of the 19 patients with short VA supraventricular tachycardia (21%). All patients survived.
The mean follow up for this group was 3.6
(2.4) years. Figure 2A shows an example of
simultaneous M mode and ECG recordings
during reentry tachycardia in a neonate with
WolV-Parkinson-White syndrome. This figure
shows the similarity between time interval
measurements on ECG and M mode echocardiographic recordings; after conversion to sinus
rhythm this patient showed a pre-excitation
wave (WolV-Parkinson-White syndrome) (fig
2B).
Long VA group
All four fetuses with long VA tachycardia
required drug treatment. Digoxin, which was
the drug of choice for all fetal supraventricular
tachycardias before this study, failed to convert
the tachycardia in all four of these cases. Compared with the short VA group, this lack of
response was significant (p < 0.04). One fetus
(case 23) was electively delivered by caesarean
section without further medication because of
signs of progressive cardiomyopathy. Sotalol
was added in the remaining three cases and two
of them (cases 20 and 22) converted to sinus
rhythm. One of the sotalol responders (case 20)
died in utero at 26 weeks gestation because of
persistent severe secondary cardiomyopathy
with generalised hydrops. This fetus had failed
to respond to direct fetal administration of
adenosine two weeks earlier. Necropsy examination revealed no congenital malformation.
The diVerence in the incidence of tachycardia
related cardiomyopathy in the long VA group
compared with the short VA group (2/4 v 1/19)
did not reach statistical significance (p < 0.06).
All three surviving neonates from this group
had recurrent episodes of supraventricular
tachycardia (p < 0.01), requiring the administration of various antiarrhythmic drugs (table
1). The permanent form of junctional reciprocating tachycardia was diagnosed in two (cases
586
Jaeggi, Fouron, Fournier, et al
21 and 22) (fig 3A), and an atrial ectopic
tachycardia in the other patient (case 23) (fig
3B). In all cases, digoxin was ineVective in preventing recurrence of tachycardia, while
propafenone (two cases) or sotalol (one case)
succeeded. After a mean follow up of 2.5 (1.9)
years, only one child with the permanent form
of junctional reciprocating tachycardia (case
22) could be weaned from treatment (at 1.5
years).
Discussion
Up to now, fetal M mode echocardiography has
been used to analyse the relative chronology of
atrial and ventricular mechanical systoles,
allowing rapid determination of atrioventricular conduction patterns.1822 The reliable identification of fetal arrhythmias such as atrial or
ventricular ectopia, atrial flutter, supraventricular tachycardia, and partial or complete
atrioventricular block has thus been possible.
In extrauterine life, surface ECG, transoesophageal electrocardiograms and, more
invasively, electrophysiological studies, allow
the division of narrow QRS supraventricular
tachycardias into two groups, based on the
duration of the RP interval.7 Our present study
shows that the same analysis can be performed
in utero using M mode echocardiography. As
can be seen from the results, the values of the
VA/AV ratio in the two groups of fetuses were
quite disparate, averaging 0.34 (0.16) for the
short VA group and 3.84 (0.82) for the long VA
group. This large diVerence between the two
ratios decreases the risk of erroneous
classification of the type of tachycardia, allowing for the fact that the peak of ventricular
contraction can occasionally be diYcult to
identify with precision on M mode.
A long VA supraventricular tachycardia was
found in four of our patients (17%), and was
associated with an increased risk of morbidity
and mortality. Of these fetuses, two developed
arrhythmia related cardiomyopathy, one died
in utero at 26 weeks gestation, and the other
had to be delivered prematurely. None of the
long VA patients responded to maternal
digoxin administration, though maternal sotalol proved eVective in controlling the supraventricular tachycardia in utero in two of the three
cases where it was used. In the same group,
adenosine was unsuccessful when given directly into the umbilical vein of one fetus (case
20), and intravenously to a neonate (case 23).
After birth, all surviving long VA infants had
recurrences of supraventricular tachycardia in
the first months of life despite prophylaxis with
digoxin.
In contrast, prenatal conversion to sinus
rhythm was observed in 17 of the 19 cases with
short VA interval, either spontaneously (five
cases) or after administration of digoxin alone
(nine cases), or in combination with sotalol
(three cases). The fact, however, that five
fetuses in this group did not respond to digoxin
suggests that in some cases other elements
besides the VA/AV measurements may have to
be taken into account if treatment fails. Only
one tachycardia related cardiomyopathy was
observed in this group (case 17). The postnatal
recurrence risk of supraventricular tachycardia
was substantially less in the short VA group
than in the long VA group (15.7% v 100%;
p < 0.01).
Since the completion of this study our management protocol for fetal supraventricular
tachycardia has been redesigned. Once the
diagnosis of supraventricular tachycardia has
been established, eVorts are now made to
measure the VA and AV intervals on M mode
echocardiograms before giving any drugs. In
the presence of a short VA interval, a reentry
mechanism with slow anterograde and fast retrograde conduction is the most likely diagnosis
and the conventional protocol is applied, with
digoxin as the drug of first choice. In cases
where conversion to sinus rhythm is not
achieved with digoxin and adenosine,2327 there
is no consensus in medical reports on alternative drugs. In the past, we have mainly used
sotalol, a class III antiarrhythmic agent with
some non-selective adrenergic blocking
activity. The favourable response previously
reported on the immature myocardium,28 and
the positive results that we and others2931 have
obtained, encourage us to continue with this
drug. Potential proarrhythmic eVects of sotalol
reported in adults and also in paediatric
patients32 remain a source of concern, and this
excludes its use as the drug of first choice in
uncomplicated short VA supraventricular
tachycardia.
There have been no controlled trials to
document the superiority of a specific antiarrhythmic drug for long VA supraventricular
tachycardias, which are usually sustained and
unresponsive to most antiarrhythmic drugs.
Class III agents are potential drugs of first
choice. Because of the known side eVects of
amiodarone on thyroid function and its long
half life, sotalol could be considered as a
suitable alternativealone if cardiac failure is
absent, or in combination with digoxin if there
is circulatory decompensation. Other types of
antiarrhythmic drug, such as class IC antiarrhythmic agents, have been used with
success in a limited number of cases of
unresponsive fetal supraventricular tachycardia.33 34
Because of the relative rarity of long VA
supraventricular tachycardia in the paediatric
age group, it is not surprising that only four
fetuses could be identified with this type of
arrhythmia. This small number of cases does not
allow us to draw definitive conclusions. Further
studies are obviously needed to reach a clear
consensus on the best way to approach the long
VA fetal supraventricular tachycardia. Only a
multicentre investigational protocol will help
achieve this goal in the shortest period of time.
1 Kleinman CS, Copel JA, Weinstein EM, et al. In utero diagnosis and treatment of fetal supraventricular tachycardia.
Semin Perinatol 1985;9:11329.
2 Van Engelen AD, Weijtens O, Brenner JI, et al. Management, outcome and follow-up of fetal tachycardia. J Am
Coll Cardiol 1994;24:13715.
3 Bergmans MGM, Jonker GJ, Kock HC. Fetal supraventricular tachycardia: review of the literature. Obstet Gynecol
Surv 1985;40:618.
4 Owen J, Colvin EV, Davis RO. Fetal death after successful
conversion of fetal supraventricular tachycardia with
digoxin and verapamil. Am J Obstet Gynecol 1988;158:
116970.
Fetal supraventricular tachycardia
5 Skoll MA, Sharland GK, Allan LD. Is the ultrasound definition of fluid collections in non-immune hydrops fetalis
helpful in defining the underlying cause or predicting outcome? Ultrasound Obstet Gynecol 1991;1:30912.
6 Kleinman CS, Copel JA. Electrophysiological principles and
fetal antiarrhythmic therapy. Ultrasound Obstet Gynecol
1991;1:28697.
7 Josephson ME. Supraventricular tachycardias. In: Clinical
cardiac electrophysiology: techniques and interpretation, 2nd ed.
Philadelphia: Lea and Febinger, 1993:181274.
8 Ko JK, Deal BJ, Strasburger JF, et al. Supraventricular
tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol 1992;69:102832.
9 Benson DW, Dunnigan A, Benditt DG, et al. Transoesophageal study of infant supraventricular tachycardia: electrophysiologic characteristics. Am J Cardiol 1983;52:10026.
10 Weidling SN, Saul JP, Walsh EP. EYcacy and risks of medical therapy for supraventricular tachycardia in neonates
and infants. Am Heart J 1996;131:6672.
11 Ludomirsky A, Garson A. Supraventricular tachycardia. In:
Gillette PC, Garson A, eds. Pediatric arrhythmias: electrophysiology and pacing. Philadelphia: WB Saunders, 1990:
380426.
12 Mehta AV, Sanchez GR, Sacks EJ, et al. Ectopic automatic
tachycardia in children: clinical characteristics, management and follow-up. J Am Coll Cardiol 1988;11:37985.
13 Sung RJ. Sustained supraventricular tachycardia. Pace 1983;
6:130626.
14 Coumel P, Cabrol C, Fabiato A, et al. Tachycardie
permanente par rhythm rciproque. Arch Mal Coeur 1967;
60:183064.
15 Critelli G, Gallagher JJ, Monda V, et al. Anatomic and
electro-physiologic substrate of the permanent form of
junctional reciprocating tachycardia. J Am Coll Cardiol
1984;4:60110.
16 Gillette PC, Garson A. Electrophysiologic and pharmacologic characteristics of autonomic ectopic atrial tachycardia. Circulation 1977;56:5715.
17 Paladini D, Chita SK, Allan LD. Prenatal measurement of
cardiothoracic ratio in evaluation of heart disease. Arch Dis
Child 1990;65:203.
18 Allan LD, Anderson RH, Sullivan ID, et al. Evaluation of
fetal arrhythmias by echocardiography. Br Heart J 1983;50:
2405.
19 Kleinman CS, Donnerstein RL, JaVe CC, et al. Fetal
echocardiography: a tool for evaluation of in utero cardiac
arrhythmias and monitoring of in utero therapy. Analysis of
71 patients. Am J Cardiol 1983;51:23743.
587
20 Silverman NH, Enderlein MA, Stanger P, et al. Recognition
of fetal arrhythmias by echocardiography. J Clin Ultrasound
1985;13:25563.
21 Reed KL, Sahn DJ, Marx GR, et al. Cardiac Doppler flows
during fetal arrhythmias: physiologic consequences. Obstet
Gynecol 1987;70:16.
22 Strasburger JF, Huhta JC, Carpenter RJ, et al. Doppler
echocardiography in the diagnosis and management of persistent fetal arrhythmias. J Am Coll Cardiol 1986;7:1386
91.
23 DiMarco JP, Sellers TD, Lerman BB, et al. Diagnostic and
therapeutic use of adenosine in patients with supraventricular tachyarrhythmias. J Am Coll Cardiol 1985;6:417
25.
24 Clarke B, Till J, Rowland E, et al. Rapid and safe
termination of supraventricular tachycardia in children
with adenosine. Lancet 1987;i:299301.
25 McIntosh-Yellin NL, Drew BJ, Scheinman MM. Safety and
eYcacy of central intravenous bolus administration of
adenosine for termination of supraventricular tachycardia.
J Am Coll Cardiol 1993;22:7415.
26 Ralston MA, Knilans TK, Hannon DW, et al. Use of adenosine for the diagnosis and the treatment of tachyarrhythmias in pediatric patients. J Pediatr 1994;124:13943.
27 Kohl T, Tercanli S, Kececioglu D, et al. Direct fetal administration of adenosine for the termination of sustained
supraventricular tachycardia. Obstet Gynecol 1995;85:873
4.
28 Houyel L, Fournier A, Ducharme G, et al. Electrophysiologic eVects of sotalol on the immature mammalian heart.
J Cardiovasc Pharmacol 1992;19:1349.
29 Meden H, Neeb U. Transplazentare Kardioversion bei
fetaler supraventrikulrer Tachykardie mit Sotalol. Z
Geburtsh Perinatol 1990;194:1824.
30 Colin A, Chabaud JJ, Ponsoit J, et al. Les tachycardies
supraventriculaires foetales et leur traitement. Arch Fr Pediatr 1989;46:33540.
31 Maragns P, Tipple M, Fournier A. EVectiveness of oral
sotalol for treatment of pediatric arrhythmias. Am J Cardiol
1992;69:7514.
32 Pfammatter JP, Paul T, Lehmann C, et al. EYcacy and
proarrhythmia of oral sotalol in pediatric patients. J Am
Coll Cardiol 1995;26:10027.
33 Allan LD, Chita KS, Sharland GK, et al. Flecainide in the
treatment of fetal tachycardias. Br Heart J 1991;65:468.
34 Meijboom EJ, van Engelen AD, van de Beek EW, et al. Fetal
arrhythmias. Curr Opin Cardiol 1994;9:97102.
You might also like
- Interpreting ECGs A Practical Approach 1st EdDocument769 pagesInterpreting ECGs A Practical Approach 1st EdArtem Trunov100% (2)
- Understanding 12-lead ECGDocument7 pagesUnderstanding 12-lead ECGccbrown7No ratings yet
- Test Bank ECGs Made Easy 5th Edition Barbara J AehlertDocument10 pagesTest Bank ECGs Made Easy 5th Edition Barbara J AehlertErnest67% (3)
- Cardio Pulmonary Final FrontierDocument10 pagesCardio Pulmonary Final Frontierdina sharafNo ratings yet
- Corporate Finance Instructor's ManualDocument541 pagesCorporate Finance Instructor's ManualJohn MathiasNo ratings yet
- ECG Made Easy - J HamptonDocument78 pagesECG Made Easy - J Hamptonkabal321100% (1)
- Wallenberg Syndrome: Publication DetailsDocument9 pagesWallenberg Syndrome: Publication DetailsHuang Jen Liang100% (1)
- Contoh Soal Residen CardioDocument13 pagesContoh Soal Residen CardioLusyAlwiNo ratings yet
- Tetralogy of FallotDocument22 pagesTetralogy of FallotHusna Aje100% (1)
- DefibrillationDocument13 pagesDefibrillationKristine VedadNo ratings yet
- Titman CH 05Document115 pagesTitman CH 05YenyensmileNo ratings yet
- Fetal DisritmiaDocument18 pagesFetal DisritmiaSebastian ChandraNo ratings yet
- Tachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDDocument21 pagesTachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDEmilio Emmanué Escobar CruzNo ratings yet
- Emergency Diagnosis and Management of Pediatric Arrhythmias 2010Document22 pagesEmergency Diagnosis and Management of Pediatric Arrhythmias 2010Jose Maria Julian RoggenNo ratings yet
- Arritmia FetalesDocument9 pagesArritmia FetalesPaulina VillarroelNo ratings yet
- Anesthetic Challenges and Successful Management of Uncorrected Tetralogy of Fallot (Tof) in PregnancyDocument3 pagesAnesthetic Challenges and Successful Management of Uncorrected Tetralogy of Fallot (Tof) in PregnancyIJAR JOURNALNo ratings yet
- SVT Mayo 2008Document12 pagesSVT Mayo 2008muhanasNo ratings yet
- Permanent Junctional Reciprocating Tachycardia in Children - A Multicenter Experience 2014Document26 pagesPermanent Junctional Reciprocating Tachycardia in Children - A Multicenter Experience 2014Võ Từ NhấtNo ratings yet
- Therapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticDocument8 pagesTherapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticNITACORDEIRONo ratings yet
- In-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisDocument15 pagesIn-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisAnonymous OU6w8lX9No ratings yet
- 1echocardiography and The NeonatologistDocument4 pages1echocardiography and The NeonatologistAbuAlezzAhmedNo ratings yet
- MECHANISMSDocument2 pagesMECHANISMSfinandaNo ratings yet
- Establishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratoryDocument15 pagesEstablishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratorySamuelNo ratings yet
- Modi Fied Blalock Taussig Shunt: A Not-So-Simple Palliative ProcedureDocument7 pagesModi Fied Blalock Taussig Shunt: A Not-So-Simple Palliative ProcedureJakler NicheleNo ratings yet
- RVOT Stenting in TOF PatientDocument31 pagesRVOT Stenting in TOF PatientHannaTashiaClaudiaNo ratings yet
- Zuva MuzachimDocument6 pagesZuva MuzachimZuva MuzachimNo ratings yet
- Tetralogy of FallotDocument24 pagesTetralogy of FallotjustinahorroNo ratings yet
- 1326 FTPDocument1 page1326 FTPabraryeniNo ratings yet
- Diagnosis and Management of Paroxysmal Supraventricular TachycardiaDocument10 pagesDiagnosis and Management of Paroxysmal Supraventricular TachycardiaRomán Wagner Thomas Esteli ChávezNo ratings yet
- Supraventricular TachycardiDocument8 pagesSupraventricular TachycardiHairunisa 0049No ratings yet
- Reentry Mechanism and Case Report of AVRT AblationDocument2 pagesReentry Mechanism and Case Report of AVRT AblationNanank Akhiruddin SyamsaNo ratings yet
- Cardiac Arrhythmias in The Pregnant Woman and The Foetus: Arrhythmia ManagementDocument5 pagesCardiac Arrhythmias in The Pregnant Woman and The Foetus: Arrhythmia ManagementRendyNo ratings yet
- Managing Palpitations and Arrhythmias During Pregnancy: Dawn L Adamson, Catherine Nelson-PiercyDocument7 pagesManaging Palpitations and Arrhythmias During Pregnancy: Dawn L Adamson, Catherine Nelson-PiercyFlo ArdyansyahNo ratings yet
- Auricchio & Cols. (1999)Document6 pagesAuricchio & Cols. (1999)Luba D'AndreaNo ratings yet
- Debo Ode 2018Document23 pagesDebo Ode 2018MaluNo ratings yet
- Hollamby Mitchell s5001226 Case 1 DtgaDocument13 pagesHollamby Mitchell s5001226 Case 1 Dtgaapi-299009880No ratings yet
- Prehospital and Emergency Department Care of Atrial FibrillationDocument8 pagesPrehospital and Emergency Department Care of Atrial FibrillationindahkurNo ratings yet
- Ecocardiografia Monitoreo Hemodinamico en Critico..Document12 pagesEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNo ratings yet
- Case 1 - Widuri - His Bundle Pacing in TAVBDocument17 pagesCase 1 - Widuri - His Bundle Pacing in TAVBW Wita SNo ratings yet
- Case Report: Middle Aortic Syndrome Treated by Implantation of An Advanta V12 Large Diameter StentDocument3 pagesCase Report: Middle Aortic Syndrome Treated by Implantation of An Advanta V12 Large Diameter StentLenardR.ApazaNo ratings yet
- Smith 2013 SMIIDocument9 pagesSmith 2013 SMIIGryseldaGryGryNo ratings yet
- JP Journals 10055 0097Document2 pagesJP Journals 10055 0097William KamarullahNo ratings yet
- Trabajo de InglesDocument11 pagesTrabajo de InglesMario A. AbreuNo ratings yet
- Normabeat FlecainideDocument34 pagesNormabeat FlecainideAmit KinareNo ratings yet
- Article 1Document4 pagesArticle 1Fakhar Mahmood ShahidNo ratings yet
- Common Types of Supraventricular Tachycardia - Diagnosis and Management - AAFPDocument9 pagesCommon Types of Supraventricular Tachycardia - Diagnosis and Management - AAFPMohamad MostafaNo ratings yet
- T Wave Alternans For Ventricular Arrhythmia Risk StratificationDocument5 pagesT Wave Alternans For Ventricular Arrhythmia Risk StratificationSalim VelaniNo ratings yet
- AV Bloc Induces TDPDocument13 pagesAV Bloc Induces TDPMirza AlfiansyahNo ratings yet
- Qara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationDocument7 pagesQara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationQara Syifa FNo ratings yet
- Co GenitalDocument5 pagesCo GenitalRana Abd AlmugeethNo ratings yet
- Congenital HDDocument19 pagesCongenital HDNikhil YadavNo ratings yet
- Maternal Heart Disease Outcomes in PregnancyDocument70 pagesMaternal Heart Disease Outcomes in PregnancySergiu HelciugNo ratings yet
- Ijmps - The Value of Holter Monitoring PDFDocument6 pagesIjmps - The Value of Holter Monitoring PDFAnonymous Y0wU6InINo ratings yet
- Anesthetic Management of An Atrial Septal Defect in Adult-Case ReportDocument3 pagesAnesthetic Management of An Atrial Septal Defect in Adult-Case ReportNikhil YadavNo ratings yet
- Cardiac Rhythms (Ecg) Name: Melody A. Boado Subject: Medsurg Year and Section: BSNDocument15 pagesCardiac Rhythms (Ecg) Name: Melody A. Boado Subject: Medsurg Year and Section: BSNMelody BoadoNo ratings yet
- Intensive Care Unit Arrhythmias: S.M. HollenbergDocument13 pagesIntensive Care Unit Arrhythmias: S.M. HollenbergEvita FebriyantiNo ratings yet
- Wide Qrs Tachy 2Document6 pagesWide Qrs Tachy 2Mohit TandonNo ratings yet
- Vijayalakshmi 2008Document7 pagesVijayalakshmi 2008Rakesh DashNo ratings yet
- Arrhythmias After TOF SurgeryDocument6 pagesArrhythmias After TOF SurgeryElizabeth Joan SalimNo ratings yet
- Early and Late Postoperative Tachyarrhythmias in Children and Young Adults Undergoing Congenital Heart Disease SurgeryDocument13 pagesEarly and Late Postoperative Tachyarrhythmias in Children and Young Adults Undergoing Congenital Heart Disease SurgeryYar ZepolNo ratings yet
- Primary Midgut VolvulusDocument2 pagesPrimary Midgut VolvulusNihal S KiranNo ratings yet
- ArrhythmiaDocument12 pagesArrhythmiamohamedsmnNo ratings yet
- Biology Project TheoryDocument16 pagesBiology Project TheoryAntra ashraNo ratings yet
- SEHGAL 2016 - A New Look at Bronchopulmonary Dysplasia - Post Capillary Pathophysiology and Cardiac DysfunctionDocument8 pagesSEHGAL 2016 - A New Look at Bronchopulmonary Dysplasia - Post Capillary Pathophysiology and Cardiac DysfunctionRafael JustinoNo ratings yet
- Uptodte TSVDocument215 pagesUptodte TSVcrilala23No ratings yet
- Medical Emergency Oral Q.docx26.docx8Document44 pagesMedical Emergency Oral Q.docx26.docx8Simina ÎntunericNo ratings yet
- Down Syndrome: Case ReportsDocument4 pagesDown Syndrome: Case ReportsPedro CardosoNo ratings yet
- WikiDocument1 pageWikikennethfarnumNo ratings yet
- WikiDocument1 pageWikikennethfarnumNo ratings yet
- M02 Titman 2544318 11 FinMgt C02Document57 pagesM02 Titman 2544318 11 FinMgt C02kennethfarnumNo ratings yet
- Chap 001Document21 pagesChap 001ajaw267No ratings yet
- WikiDocument1 pageWikikennethfarnumNo ratings yet
- Bui Kim Yen - PTDTCKDocument436 pagesBui Kim Yen - PTDTCKkennethfarnumNo ratings yet
- Capitulo 4Document151 pagesCapitulo 4radizryddleNo ratings yet
- WikiDocument1 pageWikikennethfarnumNo ratings yet
- Titman CH 03Document124 pagesTitman CH 03YenyensmileNo ratings yet
- Chap 1Document49 pagesChap 1Andre ShieldsNo ratings yet
- A Healthy BreakfastDocument19 pagesA Healthy BreakfastkennethfarnumNo ratings yet
- Testing Behavioral Asset Pricing Models On Russian Financial MarketDocument4 pagesTesting Behavioral Asset Pricing Models On Russian Financial MarketkennethfarnumNo ratings yet
- 37213Document29 pages37213William SonyoNo ratings yet
- Collier ThesisDocument38 pagesCollier ThesiskennethfarnumNo ratings yet
- Medical Management of Missed Abortion A.9Document4 pagesMedical Management of Missed Abortion A.9kennethfarnumNo ratings yet
- Divine It ReportDocument13 pagesDivine It ReportkennethfarnumNo ratings yet
- Care of Transexual PersonDocument7 pagesCare of Transexual PersonkennethfarnumNo ratings yet
- Calendar 433Document12 pagesCalendar 433kennethfarnumNo ratings yet
- Calendar 323Document12 pagesCalendar 323kennethfarnumNo ratings yet
- Calendar 366Document12 pagesCalendar 366kennethfarnumNo ratings yet
- Calendar 2589Document12 pagesCalendar 2589kennethfarnumNo ratings yet
- Calendar 2114Document12 pagesCalendar 2114kennethfarnumNo ratings yet
- Calendar 2544Document12 pagesCalendar 2544kennethfarnumNo ratings yet
- Calendar 554Document12 pagesCalendar 554kennethfarnumNo ratings yet
- Calendar 111Document12 pagesCalendar 111kennethfarnumNo ratings yet
- Calendar 212Document12 pagesCalendar 212kennethfarnumNo ratings yet
- Calendar 455Document12 pagesCalendar 455kennethfarnumNo ratings yet
- Left Anterior Fascicular Block (LAFB) ECG Review - Criteria and ExamplesDocument1 pageLeft Anterior Fascicular Block (LAFB) ECG Review - Criteria and ExamplesWiwik Puji LestariNo ratings yet
- Bls (BHD) : Dr. Rusdian Nurmadi, Mked (An), SpanDocument74 pagesBls (BHD) : Dr. Rusdian Nurmadi, Mked (An), SpanDedi Iskandar4549No ratings yet
- Ventricular Arrhythmia - VT: Braghmandaru A.BDocument113 pagesVentricular Arrhythmia - VT: Braghmandaru A.BFaisol SiddiqNo ratings yet
- Bullous ImpetigoDocument4 pagesBullous Impetigorostikawaty.A.sudirjaNo ratings yet
- Pacemaker learning essentialsDocument46 pagesPacemaker learning essentialsDeepak BhatNo ratings yet
- Cardiopulmonary ResuscitationDocument42 pagesCardiopulmonary ResuscitationDe EnNo ratings yet
- Arrhythmia Drugs Test QuestionsDocument7 pagesArrhythmia Drugs Test QuestionsDrishya BioplannetNo ratings yet
- S8 Defibrillator/monitor: - Share With The WorldDocument19 pagesS8 Defibrillator/monitor: - Share With The WorldKarl MamarilNo ratings yet
- Oral Contributions: JACC March 9, 2010 ABSTRACTS: Cardiac Arrhythmias A1Document217 pagesOral Contributions: JACC March 9, 2010 ABSTRACTS: Cardiac Arrhythmias A1Apner Calvin SuNo ratings yet
- THE NORMAL ELECTROCARDIOGRAM: DIAGNOSING MEDICAL PROBLEMS WITH AN ECGDocument63 pagesTHE NORMAL ELECTROCARDIOGRAM: DIAGNOSING MEDICAL PROBLEMS WITH AN ECGPuravin Crishan VeerasamyNo ratings yet
- TurkJEmergMed22275 5543957 - 013223 2Document8 pagesTurkJEmergMed22275 5543957 - 013223 2Ria Junita AyuNo ratings yet
- Or-DR Tally FinalDocument1 pageOr-DR Tally FinalMarvinNo ratings yet
- Anaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Document16 pagesAnaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Suresh KumarNo ratings yet
- 321 Lecture ECGDocument38 pages321 Lecture ECGCea Mikee Mitch BartolomeNo ratings yet
- Cardiac Channelopathies: ECG Review of Brugada, Long QT, Short QT, and CPVT SyndromesDocument37 pagesCardiac Channelopathies: ECG Review of Brugada, Long QT, Short QT, and CPVT SyndromesCarissa CkNo ratings yet
- Atrial Fibrillation: Racheal James Heart Rhythm Specialist Nurse UHWDocument37 pagesAtrial Fibrillation: Racheal James Heart Rhythm Specialist Nurse UHWAman ChaudharyNo ratings yet
- ECG Analysis of AF SuppressionDocument5 pagesECG Analysis of AF SuppressionAbid KhanNo ratings yet
- Ecg 2Document106 pagesEcg 2hammad992No ratings yet
- 439 3 Electrophysiology & ECG BasicsDocument34 pages439 3 Electrophysiology & ECG Basicssrisairampoly0% (1)
- Preventive Maintenance Checks for DefibrillatorsDocument26 pagesPreventive Maintenance Checks for DefibrillatorsArifah AzwaniNo ratings yet
- ECG InterpretationDocument3 pagesECG InterpretationBIANCA ROMELLE STEPHANIE PAYOTNo ratings yet
- Chapter 13: The Heart and Heart DiseaseDocument3 pagesChapter 13: The Heart and Heart Diseasetrbrown2011No ratings yet
- کتێبی وێنەی پزیشکی (KakaLea)Document159 pagesکتێبی وێنەی پزیشکی (KakaLea)be No.1No ratings yet
- Sgarbossa CrtiteriaDocument4 pagesSgarbossa Crtiteriaanisah astiraniNo ratings yet