Professional Documents
Culture Documents
Il 4 in TB Vaksin
Uploaded by
singgih2008Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Il 4 in TB Vaksin
Uploaded by
singgih2008Copyright:
Available Formats
Review
TRENDS in Immunology
Vol.25 No.9 September 2004
IL-4 in tuberculosis: implications for
vaccine design
Graham A.W. Rook1, Rogelio Hernandez-Pando2, Keertan Dheda1 and
Geok Teng Seah3
1
Centre for Infectious Diseases and International Health, Windeyer Institute for Medical Sciences, Royal Free and
University College Medical School, 46 Cleveland Street, London, UK, W1T 4JF
2
Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Vasco de Quiroga 15, Tlalpan 14000, Mexico City, Mexico
3
Department of Microbiology, National University of Singapore MD4, 5 Science Drive 2, Singapore, 117597
Current attempts to find a vaccine for tuberculosis (TB)
are based on the assumption that it must drive a Th1
response. We review the evidence that progressive disease might not be due to absence of Th1, but rather to
the subversive effect of an unusual Th2-like response,
involving interleukin-4 (IL-4) and IL-4d2. This Th2-like
response can impair bactericidal function and lead to
toxicity of tumour necrosis factor-a (TNF-a) and to pulmonary fibrosis. If this is important, effective vaccines
will need to suppress pre-existing Th2-like activity.
Such vaccines are feasible and are active therapeutically
in mouse TB.
Immunity to tuberculosis (TB) in mice is mediated by Th1
lymphocytes. These cells activate macrophages, increase
release of tumour necrosis factor-a (TNF-a) and enhance
formation of cytotoxic T lymphocytes (CTLs) [1]. The same
cytokines are crucial in humans. Children with defective
receptors for interferon-g (IFN-g) or interleukin-12 (IL-12)
are susceptible to mycobacterial disease [2,3] and TB can
be activated when patients are treated with neutralising
antibodies to TNF-a [4]. However, rapid induction of an
IFN-g response to antigens of Mycobacterium tuberculosis
is an almost universal consequence of exposure to the
infection [5]. Why then, in some individuals, is the disease
not controlled? Here we review the possibility that
Th2-like or regulatory mechanisms undermine the efficacy
of the protective response.
Inappropriate cytokine release in human TB
Before the year 2000, some authors reported that, in
addition to Th1 cytokines, there was also increased expression of IL-4 in TB [6,7]. However, other authors failed to
detect raised IL-4 and the issue remained controversial [8].
New data indicate that these earlier failures are attributable to a series of technical problems (outlined in Box 1).
Now, there is therefore a substantial body of evidence that,
in addition to Th1 cytokines, there is an IL-4 response in
human TB, whether the patients are in Europe [9,10] or
in Africa [11,12], although a survey of the literature
(G.A.W. Rook et al., unpublished) suggests that IL-4 levels
Corresponding author: Graham A.W. Rook (g.rook@ucl.ac.uk).
Available online 26 June 2004
could be higher in patients close to the equator, possibly as
a consequence of simultaneous infection with helminths
[13]. For instance, before bacillus Calmette Guerin (BCG)
vaccination, more healthy Malawians than UK adolescents made IL-5 in response to purified protein derivative
(PPD). There was a tendency for greater IL-5 production
with increasing numbers of helminth infections in the
Malawians (G.F. Black et al., pers. commun.). TB patients
have several IL-4-dependent phenomena, including IgE
antibody to M. tuberculosis [14], increased expression of
DC-specific intercellular adhesion molecule (ICAM)-grabbing non-integrin (DC-SIGN) [15,16], and antibody to
cardiolipin [17]. Similarly, both IL-4 mRNA, and T cells
containing IL-4, are increased in human pulmonary TB,
and correlate significantly with serum IgE, serum soluble
CD30 and the extent of cavitation [9 11,18]. Interestingly,
CD8 T cells also make IL-4 in TB [10,19], and CD8 cells
secreting IL-4 correlated with cavitation in the work of van
Crevel et al. [10]. IL-4 expression can also be detected in
some pulmonary lesions by in situ hybridisation [20].
Source and significance of IL-4 in TB
A variety of different cell types can make IL-4 [T cells,
eosinophils, basophils, mast cells, natural killer (NK) cells
and some antigen-presenting cells (APCs)]. Attention has
been focused recently on the neglected observation that
IL-4 can be involved in driving Th1 responses [21] and
CTLs [22]. This can be IL-4 administered externally or
IL-4 from CD11bCD11clo APCs, which are present at an
early stage of Th1 response induction [23]. IL-4 present at
later stages downregulates Th1 responses [21], and this
must be happening in TB, where at least some of the Th2
cytokines are coming from T cells [10,19].
Box 1. Why is assay of interleukin-4 (IL-4) so difficult?
(i) The low concentrations and low mRNA copy numbers at which IL-4
is active [59]
(ii) Short half-life of mRNA encoding IL-4 in clinical samples (an hour
or less) [60]
(iii) The existence of a splice variant of IL-4, which lacks exon 2 [61]
(Box 2)
(iv) Pre-stimulation of cells causes secretion of interferon-g (IFN-g)
and rapid reciprocal downregulation of Th2-cell proliferation, further
depleting an already low copy number cytokine (IL-4)
www.sciencedirect.com 1471-4906/$ - see front matter q 2004 Elsevier Ltd. All rights reserved. doi:10.1016/j.it.2004.06.005
484
Review
TRENDS in Immunology
A further possibility is that IL-4 in TB has a necessary
regulatory or anti-inflammatory role. Under some circumstances, regulatory T cells express IL-4 in addition to
classical regulatory cytokines, such as IL-10 and transforming growth factor-b (TGF-b) [24]. However, the
evidence is against this role for IL-4. In progressive
disease, IL-4 causes increased, rather than diminished,
immunopathology [25]. The presence of specific IgE
antibody [14] and of T cells that release IL-4 in vitro
when driven by TB antigen [11] indicates a genuine
antigen-specific Th2 lymphocyte response.
Nevertheless, the increased IL-4 expression in TB is
different from that seen in the partly Th2-mediated
disorder, allergic asthma [26]. In the latter disease, the
increase is mostly due to IL-4 itself, rather than to the
splice variant. By contrast, in TB patients, levels of mRNA
encoding IL-4d2, an inhibitory splice variant, were found
to rise as well [26] (Box 2). Therefore, we refer to this small
IL-4 component in TB as Th2-like.
Bovine TB
Infection of cattle with Mycobacterium bovis (a strain
derived from the human M. tuberculosis) generates both
IFN-g and IL-4 responsiveness to PPD and to ESAT-6
(early secreted antigenic target-6 kDa) [27]. Similarly, the
extent of lung pathology correlates with the production of
IL-4 by peripheral blood mononuclear cells in vitro in
response to PPD [28]. Interestingly, when cattle were
immunised with a DNA vaccine, and then 3 weeks and
6 weeks later, vaccinated again with the protein encoded
by the DNA vaccine emulsified in oil, they were more
susceptible than non-immunised controls. This increased
susceptibility correlated with an increased IL-4 response
to subsequent challenge [28].
Mouse models
Because the increased expression of IL-4 in human
(and bovine) TB is no longer in dispute, the relevant
mouse models are those in which, as in humans, IL-4
production is observed during the progressive phase of the
disease. Studies of Th1 and Th2 cytokine expression reveal
that in some, but not all, murine models of TB there are at
Box 2. Interleukin-4d2 (IL-4d2): a neglected cytokine
IL-4d2 is a splice variant of IL-4 that lacks exon 2 (48 base pairs)
[61,62]
IL-4d2 mRNA is found in primates, rabbits and woodchucks but not
in rats or mice [63]
Recombinant IL-4d2 functions as a natural antagonist of IL-4 [61,62]
Final proof that the IL-4d2 protein is produced in vivo has not yet
been obtained
Because antibodies used in flow cytometry or ELISA assays can
bind either, or both, existing work on IL-4 in humans using these
assays could be uninterpretable
IL-4d2 is easily distinguished by RT PCR [64], however, most
published work uses primers that will amplify both cytokines
IL-4d2 might be the dominant form of IL-4 mRNA in human lungs,
and associated with fibrosis [39]. Possibly an agonist on fibroblasts
IL-4d2 rises little in atopic asthma, in which mRNA encoding IL-4
itself rises 1000x more [26]
IL-4d2 mRNA does rise to a variable extent in tuberculosis [9] and in
contacts
www.sciencedirect.com
Vol.25 No.9 September 2004
first high IFN-g levels, followed later, in the progressive
phase, by a superimposed IL-4 response [29,30]. Confusion
about this point arose from the study of the effects of IL-4
gene knockout in mouse strains C57Bl 129SvJ [31] and
C57Bl [32], in which IL-4 secretion is not characteristic of
the infection. These are elegant studies, however, C57Bl
mice develop progressively increasing lung granulomas
and eventually drown in Th1 cells, without the switch to
Th2 cytokine production that is seen in Balb/c mice and,
albeit to a lesser extent, in humans.
The Th2 response is cause rather than effect
Is the IL-4 response in TB an irrelevant consequence of
the infection, or is it significantly involved in reducing
protection and increasing immunopathology? Simple
experiments where mice were pre-immunised, so that
they had small Th2 responses to one or several components
of M. tuberculosis before infection, have shown that
pre-existing Th2 activity leads to increased severity of
infection and to death [33,34]. Wangoo et al. demonstrated
that a pre-existing Th2 response to a single 16 amino
acid epitope expressed within the challenge strain of
M. tuberculosis was sufficient to undermine the efficacy of
the dominant Th1 response, and to aggravate weight loss
and lung fibrosis [35]. Further studies in Balb/c mice with
knocked out IL-4 genes proved that the absence of IL-4 led
to diminished bacterial growth, and confirmed that IL-4 is
directly involved in TNF-a-mediated immunopathology
and fibrosis in this strain [25] (see later). Interestingly,
although other authors have not studied IL-4 knockout
Balb/c mice, it was found that STAT6 (signal transducer
and activator of transcription 6) knockout Balb/c respond
normally to aerosol infection with M. tuberculosis [36].
This implies that the relevant functions of IL-4 (fibrosis
and enhanced toxicity of TNF-a) might be signaled
through insulin receptor substrate-2 (IRS-2) or IRS-1
rather than via STAT6 [37].
Fibrosis is a major cause of lung dysfunction in TB
Fibrosis in TB is a major cause of permanent respiratory
dysfunction, however, it has never been satisfactorily
explained. The dominant cytokine in TB, IFN-g, opposes
fibrosis in humans and in mice [38]. Interestingly, in
human diseases characterised by pulmonary fibrosis,
there is usually marked expression of type 2 cytokines
[systemic sclerosis, idiopathic pulmonary fibrosis, radiationinduced pulmonary fibrosis, chronic lung allograft rejection (reviewed in Ref. [38])]. These observations have led to
the type 2 cytokine hypothesis of fibrosis [38]. Fibrosis
in human TB might therefore be related to the presence
of the Th2-like response (Figure 1). Interestingly, pulmonary fibrosis in systemic sclerosis is associated with
CD8 cells secreting IL-4 and IL-4d2 [39], reminiscent of the
CD8 cells expressing either IL-4 or IL-4d2 noted previously
in human TB [10,19].
TNF-a is a crucial protective molecule but it is toxic in TB
when IL-4 is present
TNF-a-mediated immunopathology is the other phenomenon associated with IL-4 in the mouse models. In IL-4
gene knockout tuberculous Balb/c mice, there is not only
Review
M. tuberculosis
TRENDS in Immunology
Th1
FAILED Th1-MEDIATED
IMMUNITY
BACTERIAL
PROLIFERATION
Environmental
mycobacteria
BCG?
PROPHYLACTIC
VACCINE
Th2-like
IL-4
IL-13
IL-5
(IL- 42)
IMMUNOPATHOLOGY
(+TNF-)
FIBROSIS
APOPTOSIS
THERAPEUTIC
VACCINE
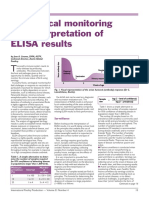
TRENDS in Immunology
Figure 1. The roles of the subversive Th2-like component of the immune response
in progressive human tuberculosis. This might be primed by bacillus Calmette
Guerin (BCG) vaccination or by environmental mycobacteria but it is then
enhanced following exposure to Mycobacterium tuberculosis. A vaccine, even
if prophylactic, might need to eliminate any pre-existing Th2 component.
Abbreviations: IL-4, interleukin-4; TNF-a, tumour necrosis factor-a.
diminished bacterial proliferation, but also a complete
absence of TNF-a-mediated toxicity following TNF-a
challenge [25]. This observation can explain the paradoxical role of TNF-a in TB. TNF-a is crucial for protection
against TB in animals [40] and in humans [4]. Nevertheless, in progressive human disease, as in progressive
TB in the Balb/c mouse [25], it is toxic (Figure 1), and drugs
that shorten the half-life of the mRNA encoding TNF-a
lead to weight gain and symptomatic relief [41]. Because
IL-4 levels are raised in progressive human disease, it is
likely that, as in mice, IL-4 is involved in the toxicity of
TNF-a. Examples of interactions between IL-4 and TNF-a
in other diseases, and possible mechanisms for proinflammatory interactions between these cytokines, are
described in Box 3.
Most existing prophylactic TB vaccine candidates fail as
therapeutic vaccines
Most known vaccine candidates (i.e. effective as prophylactic vaccines in mice) are ineffective as therapeutic
vaccines [42,43]. This is also true of BCG and of various
preparations of M. tuberculosis itself [43]. The history of
this observation goes back to Robert Koch, who observed
necrosis in tuberculous guinea-pigs given injections of
Old Tuberculin (the Koch Phenomenon), and then
repeated the experiment, with the same result, in humans
(reviewed in Ref. [44]). The role of TNF-a in the immunopathology triggered by BCG in tuberculous mice was
highlighted again recently [43].
Vaccines that downregulate IL-4 are active
therapeutically in murine TB
Interestingly, there are two preparations that are exceptions to the rule that protective vaccines are not therapeutic. One is a DNA vaccine based on heat-shock
protein 65 (hsp65) of Mycobacterium leprae, which, in
contrast to a different construct used in an aerosol
model [45], will treat ongoing TB after intravenous
infection, and while doing so, dramatically reduces IL-4
www.sciencedirect.com
Vol.25 No.9 September 2004
485
Box 3. Interleukin-4 (IL-4), decreased immunity and
increased immunopathology in tuberculosis (TB)
There are several reasons why immunity to TB might be particularly
susceptible to detrimental effects of IL-4, even when Th1 cytokines,
such as interferon-g, dominate.
Further examples of immunopathology attributable to Th1 1 Th2 1
tumour necrosis factor-a (TNF-a)
In Trichinella spiralis infection, immunopathology in the gut is
attributable to TNF-a in a mixed Th1 Th2 response. No immunopathology in IL-4 knockout mice [65]
The mixed Th1/Th2 granulomata of Schistosomiasis are exquisitely sensitive to systemic cytokine release triggered by lipopolysaccharide (LPS) [66,67]
Possible mechanisms of increased toxicity of TNF-a in mixed
Th1 1 Th2 lesions
Induction of cortisol-resistance in T cells exposed simultaneously
to Th1 and Th2 cytokines [68]
Synergistic induction of vascular cell adhesion molecule-1
(VCAM-1) on endothelial cells leading to increased recruitment of
inflammatory cells [69]
Downregulation of TRAF-2 (TNF receptor-associated factor-2)
biases functions of TNF-a away from activation and towards cell
death, which was observed in CD30 T cells incubated with TB
antigen [50]
Why is expression of IL-4 detrimental to immunity to TB?
Inappropriate type of macrophage activation [57]
Decreased expression of, and signalling through, Toll-like receptor 2
(TLR2) [56]
Downregulated inducible nitric oxide synthase (iNOS) [55];
iNOS might be fundamental to the induction and maintenance of
latency [70]
ELISPOT T-cell numbers [46]. In the same experiment, a
BCG vaccine run in parallel neither treated the disease
nor reduced IL-4 production [46]. The other exception,
heat killed Mycobacterium vaccae, is also active as an
immunotherapeutic in mice, in which it strikingly reduces
IL-4 expression when administered 60 days after intrapulmonary infection [30]. Its major mode of action is not
the induction of Th1, but rather, suppression of Th2 by
driving CD4CD45RBlow regulatory T cells [47]. Thus,
although these are only correlations, effective therapy
might relate to downregulation of IL-4 (Figure 1).
Efficacy of BCG vaccine varies in different geographical
areas
BCG vaccine is a deletional mutant of M. bovis derived by
repeated in vitro culture. Like M. bovis itself [27], BCG
primes not only Th1 but also IL-4 responses both in cattle
[48] and in mice [49]. Most workers fail to notice this
induction of IL-4, because it is far weaker that the
concomitant induction of IFN-g, and as discussed earlier,
more difficult to measure. Moreover, we do not know if
BCG induces an IL-4 response in humans, but it is likely to
because peripheral blood mononuclear cells from healthy
BCG-vaccinated donors release IL-4 in response to antigens of M. tuberculosis [50]. Not only does BCG not downregulate Th2 responses in murine TB [46], but BCG itself
evokes IL-4-secreting cells [49].
If this IL-4 component to the response evoked by BCG is
detrimental, then one would expect the efficacy of BCG to
486
Review
TRENDS in Immunology
be variable, particularly in areas close to the equator [51]
where the Th2 response to M. tuberculosis is likely to be
particularly high [13]. Similarly, repeat BCG vaccination
might be hazardous in the same environments because it
might boost the IL-4, rather than the IFN-g? component.
Repeat BCG vaccination of cattle reduced the protective
efficacy of a single vaccination, and the effects of repeat
vaccination in humans are variable, as reviewed in a paper
on cattle [48].
IL-4 and IL-4d2 in contacts of TB patients
Is expression of IL-4, or of the potential antagonist IL-4d2,
increased in latent TB, and if so, how does this differ from
what happens in those in whom the disease progresses?
Recent studies have focused on healthy individuals in
The Gambia and Ethiopia, whose peripheral blood mononuclear cells give IFN-g responses to the TB-specific
antigen, ESAT-6. These people have latent TB and it has
emerged that they have significantly raised levels of
mRNA encoding IL-4d2 in their unstimulated peripheral
blood mononuclear cells [52,53]. In The Gambia, expression of IL-4 is also increased [53]. These findings fuel
speculation that the balance of the agonist (IL-4) and
potential antagonist (IL-4d2) might be relevant to whether
or not the disease progresses, and current studies are
addressing this question. Crucial questions include whether
IL-4d2 is present only as mRNA or also active protein, and
which cell types are expressing these mRNAs in the
latently infected contacts [52]. These experiments are
currently in progress. Meanwhile, a study of healthcare
workers in Portugal has revealed that those individuals
whose peripheral blood mononuclear cells synthesised
IL-4 in response to M. tuberculosis in vitro went on to
develop overt TB within 2 4 years [54]. The methods used,
however, will not have distinguished between IL-4 and
IL-4d2. Further work will be required to discover whether it
is high IL-4, rather than IL-4d2, that predisposes to disease.
Conclusions
A Th1 response to M. tuberculosis develops rapidly following exposure and diagnostic methods detect this Th1
activity [5]. Why, then, does the disease progress? And why
do the Th1-inducing vaccine candidates that have been
tried as therapeutic vaccines cause necrosis and make the
disease worse? We have reviewed evidence that the Th1
response fails because a smaller Th2 response (IL-4, partially opposed by the antagonist, IL-4d2) is undermining its
efficacy and driving immunopathology in synergy with
TNF-a. We have also considered the more conventional
views of the role of IL-4 in TB, which are that it is needed to
drive CTLs, that it has a useful anti-inflammatory role, or
that it is merely a late consequence of progressive disease.
We have shown that recent findings make all of these
views very difficult to sustain.
IL-4, with its ability to downregulate inducible nitric
oxide synthase (iNOS) [55], Toll-like receptor 2 (TLR2) [56]
and macrophage activation [57], is potentially an early
player in the events that determine whether the infection
becomes latent or progressive. Recent studies of contacts
with latent disease [52], and of healthcare workers who
subsequently developed the disease [53,54], lend support
www.sciencedirect.com
Vol.25 No.9 September 2004
to this possibility. Now that we can distinguish IL-4 from
the antagonist IL-4d2, the role of IL-4 can be more precisely delineated. If this role is important, effective vaccines against TB might need to concentrate on elimination
of the IL-4 response, rather than on boosting the Th1
response, which develops spontaneously as a consequence
of infection (Figure 1). This principle might be equally
applicable to pre-exposure vaccines, post-exposure vaccines and therapeutic vaccines, because in each case a preexisting IL-4 response will exist, whether induced by BCG
vaccination, exposure to M. tuberculosis or cross-reactive
organisms in the environment.
How might such vaccines be achieved? The components
of M. tuberculosis responsible for driving the IL-4-secreting
T cells could be identified. It has been shown, using IL-4
ELISPOTs, that ESAT-6 and peptides derived from it do
not do so [58]. The components that do drive IL-4 can be
identified by ELISPOT or by monitoring their ability to
drive expression of IL-4 mRNA in vitro. Such antigens are
present in crude sonicated M. tuberculosis [50]. IL-4driving components could be combined with adjuvants
capable of converting the response to Th1 or of driving a
regulatory T-cell response.
To be a pathogen, an organism can either fail to evoke
the protective response or it can drive the protective
mechanisms and then deliberately sabotage them. Recent
data suggest that this might be how M. tuberculosis operates. If this proves to be correct, radically new approaches
to vaccine design will be needed, and this train of thought
will deserve to be extended into the fields of HIV and
certain parasitic diseases.
References
1 Flynn, J.L. (2004) Immunology of tuberculosis and implications in
vaccine development. Tuberculosis (Edinb.) 84, 93 101
2 Newport, M. et al. (1996) A mutation in the interferon-g receptor gene
and susceptibility to mycobacterial infection. N. Engl. J. Med. 335,
1941 1949
3 de Jong, R. et al. (1998) Severe mycobacterial and Salmonella
infections in interleukin-12 receptor-deficient patients. Science 280,
1435 1438
4 Keane, J. et al. (2001) Tuberculosis associated with infliximab,
a tumor necrosis factor a-neutralizing agent. N. Engl. J. Med. 345,
1098 1104
5 Lalvani, A. et al. (2001) Enhanced contact tracing and spatial tracking
of Mycobacterium tuberculosis infection by enumeration of antigenspecific T cells. Lancet 357, 2017 2021
6 Schauf, V. et al. (1993) Cytokine gene activation and modified
responsiveness to interleukin-2 in the blood of tuberculosis patients.
J. Infect. Dis. 168, 1056 1059
7 Sanchez, F.O. et al. (1994) Immune responsiveness and lymphokine
production in patients with tuberculosis and healthy controls. Infect.
Immun. 62, 5673 5678
8 Lin, Y. et al. (1996) Absence of a prominent Th2 cytokine response
in human tuberculosis. Infect. Immun. 64, 1351 1356
9 Seah, G.T. et al. (2000) Type 2 cytokine gene activation and its
relationship to extent of disease in patients with tuberculosis. J. Infect.
Dis. 181, 385 389
10 van Crevel, R. et al. (2000) Increased production of interleukin 4 by
CD4 and CD8 T cells from patients with tuberculosis is related to the
presence of pulmonary cavities. J. Infect. Dis. 181, 1194 1197
11 Marchant, A. et al. (2001) Polarization of PPD-specific T-Cell response
of patients with tuberculosis from Th0 to Th1 profile after successful
antimycobacterial therapy or in vitro conditioning with interferon-a or
interleukin-12. Am. J. Respir. Cell Mol. Biol. 24, 187 194
Review
TRENDS in Immunology
12 Lienhardt, C. et al. (2002) Active tuberculosis in Africa is associated
with reduced Th1 and increased Th2 activity in vivo. Eur. J. Immunol.
32, 1605 1613
13 Malhotra, I. et al. (1999) Helminth- and bacillus Calmette Guerininduced immunity in children sensitized in utero to filariasis and
schistosomiasis. J. Immunol. 162, 6843 6848
14 Yong, A.J. et al. (1989) Total and anti-mycobacterial IgE levels in
serum from patients with tuberculosis and leprosy. Tubercle 70,
273 279
15 Relloso, M. et al. (2002) DC-SIGN (CD209) expression is IL-4
dependent and is negatively regulated by IFN, TGF-b, and antiinflammatory agents. J. Immunol. 168, 2634 2643
16 Tailleux, L. et al. (2003) DC-SIGN is the major Mycobacterium
tuberculosis receptor on human dendritic cells. J. Exp. Med. 197,
121 127
17 Fischer, K. et al. (2002) IL-4 and T cells are required for the generation
of IgG1 isotype antibodies against cardiolipin. J. Immunol. 168,
2689 2694
18 Suzuki, N. et al. (2001) Can Mycobacterium tuberculosis infection
prevent asthma and other allergic disorders? Int. Arch. Allergy
Immunol. 124, 113 116
19 Smith, S.M. et al. (2002) Decreased IFN-g and increased IL-4
production by human CD8 T cells in response to Mycobacterium
tuberculosis in tuberculosis patients. Tuberculosis (Edinb.) 82, 7 13
20 Fenhalls, G. et al. (2000) In situ production of g interferon,
interleukin-4, and tumor necrosis factor a mRNA in human lung
tuberculous granulomas. Infect. Immun. 68, 2827 2836
21 Biedermann, T. et al. (2001) IL-4 instructs TH1 responses and
resistance to Leishmania major in susceptible BALB/c mice. Nat.
Immunol. 2, 1054 1060
22 Miethke, T. et al. (1988) Interleukin 4 (BSF-1) induces growth in
resting murine CD8 T cells triggered via cross-linking of T3 cell surface
structures. Eur. J. Immunol. 18, 767 772
23 Stager, S. et al. (2003) Natural antibodies and complement are
endogenous adjuvants for vaccine-induced CD8 T-cell responses.
Nat. Med. 9, 1287 1292
24 Seddon, B. and Mason, D. (1999) Regulatory T cells in the control of
autoimmunity: the essential role of transforming growth factor b and
interleukin 4 in the prevention of autoimmune thyroiditis in rats by
peripheral CD4CD45RC2 cells and CD4CD82 thymocytes. J. Exp.
Med. 189, 279 288
25 Hernandez-Pando, R. et al. (2004) Pulmonary tuberculosis in Balb/c
mice with non-functional IL-4 genes; changes in the inflammatory
effects of TNF-a in the regulation of fibrosis. Eur. J. Immunol. 34,
174 183
26 Seah, G.T. et al. (2001) Interleukin-4 and its alternatively spliced
variant (IL-4d2) in atopic asthmatics. Am. J. Respir. Crit. Care Med.
164, 1016 1018
27 Rhodes, S.G. et al. (2000) Distinct response kinetics of g interferon
and interleukin-4 in bovine tuberculosis. Infect. Immun. 68,
5393 5400
28 Wedlock, D.N. et al. (2003) Vaccination with DNA vaccines encoding
MPB70 or MPB83 or a MPB70 DNA prime-protein boost does not
protect cattle against bovine tuberculosis. Tuberculosis (Edinb.) 83,
339 349
29 Hernandez-Pando, R. et al. (1996) Correlation between the kinetics of
Th1/Th2 cells and pathology in a murine model of experimental
pulmonary tuberculosis. Immunology 89, 26 33
30 Hernandez-Pando, R. et al. (2000) Interactions between hormonemediated and vaccine-mediated immunotherapy for pulmonary
tuberculosis in Balb/c mice. Immunology 100, 391 398
31 North, R.J. (1998) Mice incapable of making IL-4 or IL-10 display
normal resistance to infection with Mycobacterium tuberculosis. Clin.
Exp. Immunol. 113, 55 58
32 Turner, J. et al. (2001) The progression of chronic tuberculosis in
the mouse does not require the participation of B lymphocytes or
interleukin-4. Exp. Gerontol. 36, 537 545
33 Lindblad, E.B. et al. (1997) Adjuvant modulation of immune responses
to tuberculosis subunit vaccines. Infect. Immun. 65, 623 629
34 Hernandez-Pando, R. et al. (1997) Pathogenesis of tuberculosis in mice
exposed to low and high doses of an environmental mycobacterial
saprophyte. Infect. Immun. 65, 3317 3327
www.sciencedirect.com
Vol.25 No.9 September 2004
487
35 Wangoo, A. et al. (2001) Contribution of Th1 and Th2 Cells to
protection and pathology in experimental models of granulomatous
lung disease. J. Immunol. 166, 3432 3439
36 Jung, Y.J. et al. (2002) Evidence inconsistent with a negative influence
of T helper 2 cells on protection afforded by a dominant T helper 1
response against Mycobacterium tuberculosis lung infection in mice.
Infect. Immun. 70, 6436 6443
37 Paul, W.E. (1997) Interleukin 4: signalling mechanisms and control of
T cell differentiation. Ciba Found. Symp. 204, 208 216
38 Lee, C.G. et al. (2001) Interleukin-13 induces tissue fibrosis by
selectively stimulating and activating transforming growth factor b1.
J. Exp. Med. 194, 809 821
39 Atamas, S.P. et al. (1999) Production of Type 2 cytokines by CD8 lung
cells is associated with greater decline in pulmonary function in
patients with systemic sclerosis. Arthritis Rheum. 42, 1168 1179
40 Flynn, J.L. et al. (1995) Tumor necrosis factor-a is required in the
protective immune response against Mycobacterium tuberculosis in
mice. Immunity 2, 561 572
41 Klausner, J.D. et al. (1996) The effect of thalidomide on the pathogenesis of human immunodeficiency virus type 1 and M. tuberculosis
infection. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 11, 247257
42 Turner, J. et al. (2000) Effective preexposure tuberculosis vaccines fail
to protect when they are given in an immunotherapeutic mode. Infect.
Immun. 68, 1706 1709
43 Moreira, A.L. et al. (2002) Mycobacterial antigens exacerbate disease
manifestations in Mycobacterium tuberculosis-infected mice. Infect.
Immun. 70, 2100 2107
44 Rook, G.A.W. and Hernandez-Pando, R. (1996) The pathogenesis of
tuberculosis. Annu. Rev. Microbiol. 50, 259 284
45 Taylor, J.L. et al. (2003) Pulmonary necrosis resulting from DNA
vaccination against tuberculosis. Infect. Immun. 71, 2192 2198
46 Lowrie, D.B. et al. (1999) Therapy of tuberculosis in mice by DNA
vaccination. Nature 400, 269 271
47 Zuany-Amorim, C. et al. (2002) Suppression of airway eosinophilia
by killed Mycobacterium vaccae-induced allergen-specific regulatory
T-cells. Nat. Med. 8, 625 629
48 Buddle, B.M. et al. (2003) Revaccination of neonatal calves with
Mycobacterium bovis BCG reduces the level of protection against
bovine tuberculosis induced by a single vaccination. Infect. Immun. 71,
6411 6419
49 Lima, K.M. et al. (2001) Comparison of different delivery systems
of vaccination for the induction of protection against tuberculosis in
mice. Vaccine 19, 3518 3525
50 Seah, G.T. and Rook, G.A.W. (2001) IL-4 influences apoptosis of
mycobacterium-reactive lymphocytes in the presence of TNFa.
J. Immunol. 167, 1230 1237
51 Wilson, M.E. et al. (1995) Geographic latitude and the efficacy of
bacillus Calmette Guerin vaccine. Clin. Infect. Dis. 20, 982 991
52 Demissie, A. et al. (2004) Healthy individuals that control latent
infection with M. tuberculosis express high levels of Th1 cytokines and
the IL-4 antagonist IL-4d2. J. Immunol. 172, 6938 6943
53 Fletcher, H.A. et al. Increased expression of mRNA encoding IL-4 and
its splice variant IL-4d2 in cells from contacts of Mycobacterium
tuberculosis in the absence of in vitro stimulation. Immunology
(in press)
54 Ordway, D. et al. Increased IL-4 production by CD8 and gd T cells in
health care workers is associated with the subsequent development of
active tuberculosis. J. Infect. Dis. (in press)
55 Bogdan, C. et al. (1994) Mechanism of suppression of nitric oxide
synthase expression by interleukin-4 in primary mouse macrophages.
J. Leukoc. Biol. 55, 227 233
56 Krutzik, S.R. et al. (2003) Activation and regulation of Toll-like
receptors 2 and 1 in human leprosy. Nat. Med. 9, 525 532
57 Gordon, S. (2003) Alternative activation of macrophages. Nat. Rev.
Immunol. 3, 23 35
58 Pathan, A.A. et al. (2001) Direct ex vivo analysis of antigen-specific
IFN-g-secreting CD4 T cells in Mycobacterium tuberculosis-infected
individuals: associations with clinical disease state and effect of
treatment. J. Immunol. 167, 5217 5225
59 Minty, A. et al. (1997) The related cytokines interleukin-13 and
interleukin-4 are distinguished by differential production and differential effects on T lymphocytes. Eur. Cytokine Netw. 8, 203 213
488
Review
TRENDS in Immunology
60 Umland, S.P. et al. (1998) Interleukin-5 mRNA stability in human
T cells is regulated differently than interleukin-2, interleukin-3,
interleukin-4, granulocyte/macrophage colony-stimulating factor, and
interferon-g. Am. J. Respir. Cell Mol. Biol. 18, 631 642
61 Atamas, S.P. et al. (1996) An alternative splice variant of human IL-4,
IL-4d2, inhibits IL- 4-stimulated T cell proliferation. J. Immunol. 156,
435 441
62 Vasiliev, A.M. et al. (2003) Structural and functional properties of
IL-4d2, an alternative splice variant of human IL-4. J. Proteome Res. 2,
273 281
63 Gautherot, I. et al. (2002) Cloning of interleukin-4d2 splice variant
(IL-4d2) in chimpanzee and cynomolgus macaque: phylogenetic
analysis of d2 splice variant appearance, and implications for the
study of IL-4-driven immune processes. Immunogenetics 54, 635 644
64 Seah, G.T. and Rook, G.A. (1999) A sensitive, non-radioactive quantitative method for measuring IL-4 and IL-4d2 mRNA in unstimulated
cells from multiple clinical samples, using nested RT-PCR. J. Immunol.
Methods 228, 139 149
Vol.25 No.9 September 2004
65 Lawrence, C.E. et al. (1998) IL-4-regulated enteropathy in an
intestinal nematode infection. Eur. J. Immunol. 28, 2672 2684
66 Ferluga, J. et al. (1979) Increased hepatotoxicity of bacterial lipopolysaccharide in mice infected with Schistosoma mansoni. Parasite
Immunol. 1, 289 294
67 Wynn, T.A. et al. (1995) An IL-12-based vaccination method for
preventing fibrosis induced by schistosome infection. Nature 376,
594 596
68 Kam, J.C. et al. (1993) Combination IL-2 and IL-4 reduces glucocorticoid receptor-binding affinity and T cell response to glucocorticoids.
J. Immunol. 151, 3460 3466
69 Iademarco, M.F. et al. (1995) Regulation of vascular cell adhesion
molecule-1 expression by IL-4 and TNF-a in cultured endothelial cells.
J. Clin. Invest. 95, 264 271
70 Voskuil, M.I. et al. (2003) Inhibition of respiration by nitric oxide
induces a Mycobacterium tuberculosis dormancy program. J. Exp.
Med. 198, 705 713
Immunology online
General information
An Immune System Glossary: http://www.molbiol.ox.ac.uk/pathology/tig/gloss.html
AMADEO: Free Medical Literature Guide: http://www.amedeo.com/
Immunology Index: http://www.keratin.com/am/
Glossary of Immunology: http://www-micro.msb.le.ac.uk/MBChB/ImmGloss.html
Molecular Immunology: http://www.mi.interhealth.info/
Spiders and Immunology: http://www.xs4all.nl/~ednieuw/
Societies
British Society for Immunology: http://www.immunology.org/
American Academy of Allergy, Asthma and Immunology: http://www.aaaai.org/
Clinical Immunology Society: http://www.clinimmsoc.org/
Society for Mucosal Immunology: http://www.socmucimm.org/
Australasian Society for Immunology: http://www.wehi.edu.au/collegiate/ASI/
Canadian Society of Allergy and Clinical Immunology: http://csaci.medical.org/
International Society for Interferon and Cytokine Research: http://www.isicr.org/
Federation of Clinical Immunology Societies: http://www.focisnet.org/
Discussion groups:
BioWWW.net: http://biowww.net/
Nomenclature
CD: http://www.immunologylink.com/cdantigen1.htm
HLA: http://www.ebi.ac.uk/imgt/hla/
KIR: http://www.gene.ucl.ac.uk/nomenclature/genefamily/kir.html
http://www.ncbi.nlm.nih.gov/prow/guide/679664748_g.htm
LILR: http://www.gene.ucl.ac.uk/nomenclature/genefamily/lilr.html
Immunoglobulins
Immunoglobulin Structure/Function: http://www.path.cam.ac.uk/~mrc7/mikeimages.html
Porcine Immunology Resources: http://eis.bris.ac.uk/~lvkh/welpig.htm
If you know of any other useful online resources that you think should be featured in Trends in Immunology please let us know at
immunology@current-trends.com
www.sciencedirect.com
You might also like
- Bing Portofolio 1Document10 pagesBing Portofolio 1singgih2008No ratings yet
- Name of ProductDocument6 pagesName of Productsinggih2008No ratings yet
- Spesifikasi Keterangan Tambahan Riwayat HargaDocument10 pagesSpesifikasi Keterangan Tambahan Riwayat Hargasinggih2008No ratings yet
- Fluorochrome Absorption and Emission SpectraDocument7 pagesFluorochrome Absorption and Emission Spectrasinggih2008No ratings yet
- MM HiperkalsemiaDocument6 pagesMM Hiperkalsemiasinggih2008No ratings yet
- C Reaktive ProteinDocument4 pagesC Reaktive Proteinsinggih2008No ratings yet
- PB0912 Dengue Cassette Web NoticeDocument2 pagesPB0912 Dengue Cassette Web Noticesinggih2008No ratings yet
- Waldenstrom 09Document1 pageWaldenstrom 09singgih2008No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Biotechnology Research and Integration With IndustDocument7 pagesBiotechnology Research and Integration With Industtanvipatel.121988No ratings yet
- TRUTH About Covid-19 and Covid-19 VaccinesDocument81 pagesTRUTH About Covid-19 and Covid-19 Vaccineshusain rizvi100% (24)
- Covid 19 TheoryDocument2 pagesCovid 19 TheoryChris WallsNo ratings yet
- Modul KPS SAINS SPMDocument54 pagesModul KPS SAINS SPMHuda WahabNo ratings yet
- Bacterial Meningitis in Children - ClinicalKeyDocument24 pagesBacterial Meningitis in Children - ClinicalKeyRubi Gonzalez SoberanoNo ratings yet
- US Code 1182 Chapter 12 - Immigration and NationalityDocument234 pagesUS Code 1182 Chapter 12 - Immigration and NationalityBarbara EspinosaNo ratings yet
- Ebook Medical Secrets PDF Full Chapter PDFDocument67 pagesEbook Medical Secrets PDF Full Chapter PDFregina.white324100% (25)
- Portfolio AlbertusDocument53 pagesPortfolio AlbertusDewi AzkiaNo ratings yet
- Thimerosal-Definite Cause of Autism by David Ayoub MDDocument6 pagesThimerosal-Definite Cause of Autism by David Ayoub MDFlorentina ClapaNo ratings yet
- Important Questions For CBSE Class 9 Science Chapter 13Document13 pagesImportant Questions For CBSE Class 9 Science Chapter 13Ankita GuptaNo ratings yet
- Paramedicine Vaccine Administration Memorandum of Agreement Cape CoralDocument29 pagesParamedicine Vaccine Administration Memorandum of Agreement Cape CoralNews-PressNo ratings yet
- POTSDocument2 pagesPOTSTSMTSMNo ratings yet
- Sentimental Medicine PDFDocument8 pagesSentimental Medicine PDF杨飞燕No ratings yet
- Community Health Nursing: MidtermsDocument8 pagesCommunity Health Nursing: MidtermsBeverly DatuNo ratings yet
- Lawatan Makmal Virtual Bioteknologi (A182950)Document2 pagesLawatan Makmal Virtual Bioteknologi (A182950)AINA AZRA BINTI NASHARUDDINNo ratings yet
- TimingsDocument1 pageTimingsRajeev kurupathNo ratings yet
- CertificateDocument1 pageCertificateShubham TiwariNo ratings yet
- Immunization in Children: Mary Beth F. Tanco, MD, FPPS Active Consultant Institute of Pediatrics and Child HealthDocument92 pagesImmunization in Children: Mary Beth F. Tanco, MD, FPPS Active Consultant Institute of Pediatrics and Child HealthPolychase Magaoay100% (1)
- Pneumovax PiDocument9 pagesPneumovax PipisucamiNo ratings yet
- De Cuong On Tap Tieng Anh 10 HK2 Nam 22 23Document11 pagesDe Cuong On Tap Tieng Anh 10 HK2 Nam 22 23hle06328No ratings yet
- Bill Little, CPRMC CEO, Letter To The CommunityDocument1 pageBill Little, CPRMC CEO, Letter To The CommunityWMBF NewsNo ratings yet
- 7th Edition 7.1Document50 pages7th Edition 7.1eshwar_org100% (1)
- Serological Monitoring by ELISADocument3 pagesSerological Monitoring by ELISAreza tavayef100% (1)
- Sugar PolioDocument3 pagesSugar PolioHenrikas StaniuleviciusNo ratings yet
- Ananthanarayan & Paniker's Textbook of Microbiology, 2005Document672 pagesAnanthanarayan & Paniker's Textbook of Microbiology, 2005Naga Raju Kandula67% (3)
- LTSC Handbook 2015Document143 pagesLTSC Handbook 2015gwzglNo ratings yet
- Residence Hall Application 2012Document2 pagesResidence Hall Application 2012Theo ChandlerNo ratings yet
- City of Cincinnati COVID-19 Vaccination Policy 9-21Document5 pagesCity of Cincinnati COVID-19 Vaccination Policy 9-21WCPO 9 NewsNo ratings yet
- ECCD Vaccine Evaluation AdvancedDocument47 pagesECCD Vaccine Evaluation Advancedko nayNo ratings yet
- Strigarianz 2nd YearDocument42 pagesStrigarianz 2nd YearKhaleedNo ratings yet