Professional Documents
Culture Documents
Estabilidad de Drogas
Uploaded by
Estefany MartinezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Estabilidad de Drogas
Uploaded by
Estefany MartinezCopyright:
Available Formats
FABAD J. Pharm. Sci.
, 33, 8794, 2008
RESEARCH ARTICLE
Comparison of Dissolution Profiles of Two
Commercially Available Co-Trimoxazole Tablets
Esin SAYAR*,**, Selma AHN*, emsettin CEVHEROLU**, A. Atilla HINCAL*
Comparison of Dissolution Profiles of Two Commercially
Available Co-Trimoxazole Tablets
Piyasada Mevcut ki Kotrimoksazol Tabletin
Dissolsyon Profillerinin Karlatrlmas
Summary
zet
The dissolution test is intended to measure the time required
for a given drug in an oral solid dosage form to go into solution
under specified set of conditions. It is used to assess the batchto-batch quality of a drug product, guide to development
of a new formulation, ensure continuing product quality,
support the bioavailability of a new product, bioequivalence
of an essentially similar product. The aim of this study was
to investigate the influence of dissolution medium on the
in vitro release of trimethoprim/sulfamethoxazole (TMP/
SMX: 160/800 mg) from, two commercially available Cotrimoxazole tablets. Three different buffers (pH 1.2, 4.6 and
6.8) were used as the dissolution medium (900 mL) and the
paddle rotation speed was kept at 50 rpm. The dissolution
profiles of both tablets were compared using difference (f1)
and similarity (f2) factors. Release of both TMP and SMX
from Co-trimoxazole tablets was found to be pH dependent.
Although the dissolution profiles of TMP obtained for test and
reference products at pH 1.2 medium (50 rpm) was similar,
based on f1 and f2 values, the dissolution profiles of TMP were
dissimilar for other conditions (pH 4.6 and 6.8 with 50 rpm).
On the other hand, for all three dissolution media given above,
all dissolution profiles of SMX obtained for test and reference
formulations were different (f1 > 25 and f2 < 37 for all
mediums). All these results indicate that dissolution studies
are not sufficient to demonstrate the similarity of these tablet
formulations, and that further in vivo studies are required.
znme testi bir ilacn belirlenmi koullar altnda bir
oral kat dozaj eklinden zeltiye gemesi iin gerekli olan
srenin llmesini amalamaktadr. Bir ila rnnn
seriden seriye kalitesini lmek, yeni bir formlasyonun
gelitilmesine rehberlik etmek, rn kalitesinin devamn
salamak, yeni bir rnn biyoyararlanmn ve esasta benzer
bir rnn biyoedeerliini desteklemek amacyla kullanlr.
Bu almann amac, piyasada mevcut olan iki kotrimoksazol
tabletten trimetoprim/slfametoksazol (TMP/SMX: 160/800
mg)n in vitro salm zerine znme ortamlarnn etkisini
incelemektir. znme ortam (900 mL) olarak farkl
tampon (pH 1.2, 4.6 and 6.8) kullanlm ve pedal dnme
hz 50 rpmye ayarlanmtr. Her iki tabletin znrlk
profilleri fark (f1) ve benzerlik (f2) faktrleri kullanlarak
karlatrlmtr.
TMP ve SMXin kotrimoksazol
tabletlerinden salmnn pHya baml olduu bulunmutur.
pH 1.2 ortamnda (50 rpm) test ve referans rnlerden
TMPnin znrlk profilleri benzer olmasna ramen,
dier koullarda (pH 4.6 and 6.8) TMPnin znrlk
profilleri benzer deildir. Dier taraftan, yukarda verilen
znrlk ortamnda test ve referans formlasyonlarndan
SMX iin elde edilen dissolsyon profilleri farkldr ( tm
ortamlar iin f1 > 25 ve f2 < 37). Tm bu sonular bu tablet
formlasyonlarnn benzerliini gstermek iin znrlk
profillerinin yeterli olmadn ve ilave in vivo almalarn
gerektiini gstermektedir.
Key Words: Dissolution, Trimethoprim, Sulfamethoxazole,
Co-trimozaxole
Anahtar
Kelimeler:
Dissolsyon,
Slfametoksazol, Kotrimoksazol
Trimetoprim,
Received: 26.11.2009
Revised: 05.02.2010
Accepted: 12.02.2010
* Hacettepe University, Faculty of Pharmacy, Ankara, Turkey
** Ministry of Defense, Army Drug Factory, Ankara, Turkey
Corresponding author E-mail: selmas@hacettepe.edu.tr
87
Sayar, ahin, Cevherolu, Hncal
INTRODUCTION
Drug absorption from a solid dosage form after
oral administration depends on the release of drug
substance from the drug product, the dissolution
or solubilization of the drug under physiological
conditions and the permeability across the
gastrointestinal tract. Because of the critical nature of
the first two of these steps, in vitro dissolution may
be relevant to the prediction of in vivo performance.
Based on this general consideration, in vitro dissolution
test for immediate release solid oral dosage forms
(i.e. tablets, capsules) is used to assess the batch-tobatch quality control of a drug product; guide the
development of new formulations; and ensure the
sustainability of the product quality and performance
after certain changes, such as those in the formulation,
the manufacturing process, the site of manufacture,
and the scale-up of the manufacturing process.
Dissolution test can also be used to support the
bioavailability of a new product, the bioequivalence
of an essentially similar product or variations (1,2).
The biopharmaceutics classification system (BCS)
is a scientific framework for classifying drug
substances based on their aqueous solubility and
intestinal permeability. When combined with the
dissolution of the drug product, the BCS takes into
account three major factors that govern the rate and
extent of drug absorption from immediate release
dosage forms: dissolution, solubility and intestinal
permeability. According to the BCS, the drug
substances are classified as class 1 (high solubility
and high permeability), 2 (low solubility and high
permeability), 3 (high solubility and low permeability)
and 4 (low solubility and low permeability). In
addition, immediate release (IR) oral dosage forms
are categorized as having rapid or slow dissolution.
When the in vivo dissolution of an IR solid oral dosage
form is rapid in relation to the gastric emptying and
the drug has high permeability, the rate and extent
of drug absorption is unlikely to be dependent on
dissolution and/or gastrointestinal transit time.
Under such circumstances, demonstration of in
vivo bioavailability or bioequivalence may not be
necessary for highly soluble and highly permeable
class 1 substances in IR solid oral dosage form
88
that exhibit rapid in vitro dissolution using the
recommended test methods (3).
The combination of trimethoprim (TMP) and
sulfamethoxazole (SMX) in a 1:5 ratio, known as Cotrimoxazole, has been used for the treatment of a
wide variety of infections due to Gram-positive and
Gram-negative organisms; particularly those of the
urinary, respiratory, and gastro-intestinal tracts (4-6).
The synergistic bactericidal effect of the combination
is due to sequential blockade of bacterial enzyme
systems associated with tetrahydrofolate synthesis.
SMX inhibits bacterial synthesis of dihydrofolic
acid by competing with paraaminobenzoic acid.
TMP blocks the production of tetrahyrofolic acid
from dihydrofolic acid by binding to and reversibly
inhibiting the dihydrofolate reductase (7,8). Based
on BCS (9) and biopharmaceutics drug disposition
classification system (10), SMX is a class 2 compound,
whereas, TMP is a class 3 compound.
Co-trimoxazole was originally formulated as tablets
in two strengths (80/400 mg and 160/800 mg TMP/
SMX). Furthermore, several generic formulations are
commercially available in the Turkish Drug Market.
The objective of this study was to investigate the
influence of dissolution medium on the in vitro
release of TMP/SMX (160/800 mg) from two
commercially available Co-trimoxazole tablets.
MATERIALS AND METHODS
Materials
TMP was a BP reference standard and SMX was a
USP reference standard. Acetonitrile and methanol
were of HPLC grade and purchased from Merck.
All other chemicals were of analytical grade and
obtained from Merck.
Quality Control Tests for the Test and Reference
Tablets
Dissolution studies on the test (Batch no:0412522001)
and reference (Bactrim 160/800mg, TMP/SMX;
Batch no:B1105) tablets were conducted using
USP Apparatus II (paddle method) with twelve
replicates at 37 0.5C (Sotax, Switzerland). Three
different buffers (pH 1.2, 4.6 and 6.8) were used as
the dissolution medium (900 mL) and the paddle
FABAD J. Pharm. Sci., 33, 8794, 2008
rotation speed was kept at 50 rpm. 0.1N HCl was
used as the pH 1.2 buffer. The pH 4.6 buffer consisted
of 0.2M potassium biphthalate (50 mL), 0.2M sodium
hydroxide (11.1 mL) and distilled water (q.s. 200
mL). On the other hand, the pH 6.8 buffer consisted
of 0.2M potassium phthalate monobasic (50 mL),
0.2M sodium hydroxide (22.4 mL) and distilled
water (q.s. 200 mL) (11). Additionally, in accordance
with the USP method, dissolution studies with test
and reference tablets were performed in 900 mL of
pH 1.2 buffer at a paddle stirring rate of 75 rpm (11).
In all experiments, at predetermined time intervals
(5, 10, 15, 30, 45 and 60 min), 2 mL sample was
withdrawn and replaced with an equal volume of
fresh medium to maintain a constant total volume.
After the filtration and dilution of the dissolution
samples with the mobile phase, the concentrations of
TMP and SMX were determined simultaneously by a
validated HPLC method.
In addition, weight variation, diameters and thickness,
hardness, friability, disintegration time, and content
uniformity of active ingredients (TMP and SMX)
were determined for the quality control of test and
reference tablets. For the determination of weight
variation, 20 tablets were weighed individually on an
analytical balance (Sartorious, Germany), and then
mean and standard deviation were calculated for
test and reference tablets. Diameters and thickness of
the tablets were determined from 20 tablets with an
electronic compass (Bochem, Germany). Hardness
of 10 tablets were measured using a hardness tester
(Pharma Test, Germany). Dusted and accurately
weighed 20 tablets were placed in a friabilator (Pharma
Test, Germany) and rotated 4 min (100 revolution).
To remove adhering particles, the tablets were
dusted again and then weighed. The mean percent
friability was calculated from the difference in tablet
weights. The disintegration time of tablets (n=6) was
determined at 37oC in water using disintegration
tester (Komet, Turkey). Content uniformity of test
and reference tablets was performed as described
in the official monograph. Briefly, twenty tablets
were weighed and finely powdered. TMP and SMX
amounts were then determined from the accurately
weighed portion of the powder, equivalent to about
160 mg of SMX (11).
HPLC Analysis of Trimethoprim/
Sulfamethoxazole
The HPLC system operating in isocratic mode,
consisted of Waters (USA) equipments including
a 515 solvent delivery system, a Waters 717 plus
autosampler, and a Waters 996 Photodiode array
detector. Reverse phase C8 column packed with 5 m
dimethyl octadecylsilyl bonded amorphous silica
(4.6 mm 250 mm) was used as the stationary phase.
Chromatographic analysis was carried out at ambient
temperature. The compounds were separated using
a mobile phase consisted of acetonitrile:water:acetic
acid (50:49:1). The mobile phase was prepared daily,
filtered (0.45 m), sonicated before use, and delivered
at a flow rate of 1 mL/min. The detector responses
were set at 254 nm. The amount of the compounds
dissolved were determined using calibration curves
constructed over the range of 8 to 25 g/mL for TMP
and 40 to 120 g/mL for SMX. The proposed method
was validated as to selectivity, sensitivity, linearity
and precision (system repeatability and intra-day
repeatability).
Data Analysis
Dissolution profiles were compared using two
model-independent parameters: the difference (f1)
and similarity (f2) factors (1). The difference factor
(f1) calculates the percent (%) difference between the
two curves at each time point and is a measurement
of the relative error between the two curves (1):
where n is the number of time points, Rt is the
dissolution value of the reference batch at time t, and
Tt is the dissolution value of the test batch at time t.
The similarity factor (f2 ) is a logarithmic reciprocal
square root transformation of the sum of squared
error and is a measurement of the similarity in the
percent (%) dissolution between the two curves (1).
89
Sayar, ahin, Cevherolu, Hncal
precise, accurate, specific and sensitive enough for
simultaneous determination of TMP and SMX in
dissolution samples.
RESULTS AND DISCUSSIONS
Validation of the Analytical Method
Method validation is the process used to confirm
that the analytical procedure employed for a
specific test is suitable for its intended use. Results
from method validation can be used to judge the
quality, reliability and consistency of analytical
results; it is an integral part of any good analytical
practice (12). In this study, the HPLC method used
for simultaneous determination of TMP and SMX
was validated with respect to selectivity, sensitivity,
linearity and precision. TMP and SMX were well
separated with retention times of 2.7 min for TMP
and 4.3 min for SMX, with no interfering peaks in the
chromatograms. The calibration curves were linear
for both TMP (8-25 mg/mL) and SMX (40-120 mg/mL)
with determination coefficients always greater than
0.999. The relative standard deviations calculated
for the precision of the system repeatability were
lower than 2% for both TMP and SMX. The relative
standard deviations and Bias values estimated for the
intra-day repeatability of the assay were within the
acceptable limits (< 2%) indicating that the precision
and accuracy of the proposed HPLC method were
satisfactory. The detection and quantification limits
were 0.38 and 1.24 g/mL for SMX, 0.55 and 1.53
g/mL for TMP, respectively. All the results clearly
indicate that the developed HPLC method was
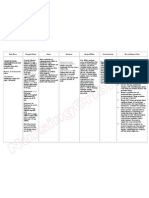
Quality Control Tests
The quantitative evaluation and assessment of
a tablets chemical, physical and bioavailability
properties are important in the design of tablets and
to monitor product quality. These properties are
important since chemical breakdown or interactions
between tablet components may alter the physical
tablet properties, and greatly affect the bioavailability
of the tablet system. There are various standards that
have been set regarding the quality of pharmaceutical
tablets. These include the diameter, size, shape,
thickness, weight, hardness, disintegration and
dissolution characters. The diameters and shape
depends on the die and punches selected for the
compression of tablets. The remaining specifications
assure that tablets do not vary from one production
lot to another (13). The quality control values
determined for the test and reference tablets are
summarized in Table 1. Although friability and
disintegration of the test formulation were slightly
higher than those of the reference product, all
quality control parameters were within the specified
limits (e.g. weight variation <5%, friability <1% and
disintegration time <15 min).
For poorly soluble drugs, the rate limiting step
in the absorption process is the dissolution rate.
Therefore, determination of dissolution rate can
be a useful guide for comparative bioavailability.
Table 1. Quality control values (mean SD) obtained for the test and reference tablets.
Parameter
Test
Reference
1166.0 19.9
1024.2 18.9
1539.3
1585.8
Friability (%)
0.36
0.004
Width (mm)*
8.84 0.01
8.92 0.02
Length (mm)*
19.1 0.01
19.1 0.02
Thickness (mm)*
8.05 0.02
7.29 0.03
Disintegration time (min)***
2.830.35
1.420.3
TMP: 101.3
SMX: 99.1
TMP: 99.3
SMX: 99.8
Weight (mg)*
Hardness (N)**
Content of active ingredient (%)
*n=20; **n=10; ***n=6
90
FABAD J. Pharm. Sci., 33, 8794, 2008
Since drug absorption and physiological availability
depend on the availability of the drug substance in
the dissolution state, having suitable dissolution
characteristics is important for a satisfactory tablet.
The dissolution test measures the amount of time
required for certain percentage of the drug substance
in a tablet to go into solution under a specified
set of conditions. It describes a step towards
physiological availability of the drug substance, but
it is not designed to measure the safety or efficacy
of the tablet being tested. It provides in vitro control
procedure to eliminate variation among production
batches. The dissolution medium must be aqueous
and the pH of the medium should be controlled and
should simulate the biological conditions (14,15).
The results of the dissolution studies were
summarized in Table 2 for TMP and Table 3 for SMX.
Corresponding dissolution profiles were given in
Figures 1 and 2, respectively. It can be seen from the
results that dissolution of both TMP and SMX from
Co-trimoxazole tablets was pH dependent. With an
increase in the pH of the dissolution media from
1.2 to 6.8, release of TMP from test and reference
products was decreased. In the case of SMX,
dissolved amount was decreased initially when the
pH of the dissolution medium rose from 1.2 to 4.6,
probably due to a decrease in the surface ionization
at this pH, and then increased with and increase of
the dissolution medium to 6.8. These observations
are in accordance with the solubilities of TMP and
SMX. Although solubility of TMP decreases as a
function of pH (from 154.1 to 55.1 mg/mL for pH 1.2
to 6.8, respectively), SMX shows similar pattern in
solubility too (506 mg/mL for pH 1.2; 159 mg/mL
for pH 4.6 and 670 mg/mL for pH 6.8) (16).
The dissolution profiles of test and reference products
Table 2. Percent dissolved for TMP as a function of time.
Percent Dissolved
Test
Reference
Time
(min)
pH 1.2 (USP)*
pH 1.2**
pH 4.6**
5
10
15
30
45
60
92.8 4.7
99.1 3.1
98.6 1.3
98.7 9.1
95.5 3.1
95.1 2.9
79.4 11.0
77.2 7.0
83.3 4.4
84.6 4.8
86.4 3.2
87.2 2.8
42.5 7.1
56.7 8.4
67.1 5.1
74.5 8.4
80.6 4.9
82.4 4.9
pH 6.8**
pH 1.2
(USP)*
pH 1.2**
pH 4.6**
pH 6.8**
16.9 3.1
28.6 3.0
37.9 2.5
57.0 4.7
68.3 4.4
73.1 7.0
68.5 23.7
91.1 2.2
90.7 2.6
92.3 1.4
88.2 6.8
91.3 4.5
73.6 8.3
78.2 6.9
83.1 4.6
89.8 3.3
91.1 2.5
89.5 5.4
26.1 5.0
37.3 9.0
48.3 7.4
63.2 10.0
70.7 9.7
78.3 7.5
10.6 2.2
17.9 2.6
25.4 2.5
41.8 9.3
65.1 7.2
70.5 5.8
* 75 rpm (mean SD; n=6); **50 rpm (mean SD; n=12)
Table 3. Percent dissolved for SMX as a function of time.
Percent Dissolved
Test
Reference
Time
(min)
pH 1.2 (USP)*
pH 1.2**
pH 4.6**
pH 6.8**
pH 1.2 (USP)*
pH 1.2**
pH 4.6**
pH 6.8**
5
10
15
30
45
60
78.3 5.0
91.1 1.9
93.5 0.6
94.1 3.1
96.9 3.9
95.7 2.4
61.3 10.3
32.7 5.8
44.5 6.4
41.7 15.7
23.8 3.7
9.6 2.0
18.2 3.5
68.5 6.6
77.4 4.2
82.6 4.5
85.1 3.5
87.0 4.6
41.1 7.1
49.2 3.3
56.3 8.4
61.5 3.9
61.9 6.3
55.9 5.4
62.1 4.5
73.9 5.9
80.3 5.6
81.5 7.7
80.6 5.4
92.0 4.3
100.0 2.5
96.9 7.7
100.1 4.6
36.4 2.9
49.0 2.1
71.2 5.3
79.6 5.3
83.0 8.0
14.4 3.7
21.3 3.5
33.8 3.9
41.2 2.8
50.1 2.5
29.4 3.6
39.5 3.0
53.7 11.4
75.0 7.3
77.9 6.6
* 75 rpm (mean SD; n=6); **50 rpm (mean SD; n=12)
91
Sayar, ahin, Cevherolu, Hncal
A.
A.
0.1 N HCl
0.1 N HCl
pH 4.6
100
pH 6.8
100
80
60
S MX releas e (% )
T MP releas e (% )
pH 4.6
40
20
0
0
10
20
30
40
50
pH 6.8
80
60
40
20
0
0
60
10
20
30
40
50
60
T im e (h)
T im e (h)
B.
B.
0.1 NHCl
0.1 NHCl
pH 4.6
pH 6.8
80
60
40
20
0
0
10
20
30
40
50
60
pH 4.6
S MX releas e (% )
T MP releas e (% )
100
100
80
60
40
20
0
pH 6.8
10
20
T im e (h)
Figure 1. Mean ( SD) in vitro dissolution profiles of TMP
from test (A) and reference (B) products. Three different
buffers (pH 1.2, 4.6 and 6.8) were used as the dissolution
medium (900 mL) and the paddle rotation speed was kept
at 50 rpm.
were compared using difference (f1) and similarity
(f2) factors. When calculated values of f1 lie between
0 and 15 and those of f2 lie above 50, the dissolution
profiles are interpreted to be similar (1,3). When the
USP method (pH 1.2, 75 rpm) was used, both TMP
and SMX in test and reference products dissolved
more than 85% of the labeled amount of the drug in
15 min, the profile comparison with and f1 and f2 tests
was, thus, unnecessary (Tables 2 and 3). Although
the dissolution profiles of TMP obtained for test and
reference products at pH 1.2 medium (50 rpm) were
similar, based on f1 and f2 values, the dissolution
profiles of TMP were dissimilar for other conditions
(pH 4.6 and 6.8 with 50 rpm; Table 4). In the case of
SMX, for all three dissolution media given above, all
dissolution profiles obtained for test and reference
formulations were different (f1 > 25 and f2 < 37 for
all mediums; Table 4). All these results indicate that
92
30
40
50
60
T im e (h)
Figure 2. Mean ( SD) in vitro dissolution profiles of SMX
from test (A) and reference (B) products. Three different
buffers (pH 1.2, 4.6 and 6.8) were used as the dissolution
medium (900 mL) and the paddle rotation speed was kept
at 50 rpm.
dissolution studies are not sufficient to demonstrate
the similarities of these tablet formulations, and that
further in vivo studies are required.
CONCLUSIONS
The developed HPLC method was precise, accurate,
specific and sensitive enough for simultaneous
determination of TMP and SMX from dissolution
samples. In FDA guidance (3), an immediate release
Table 4. Difference (f1) and similarity (f2) values obtained
for TPM and SMX.
TMP
SMX
Medium
(50 rpm)
f1
f2
f1
f2
pH 1.2
pH 4.6
pH 6.8
3.1
21.4
20.0
72.8
42.7
49.5
25.5
68.0
28.4
34.9
32.3
36.9
FABAD J. Pharm. Sci., 33, 8794, 2008
drug product is considered rapidly dissolving
when no less than 85% of the labeled amount of the
drug substance dissolves within 30 min, using U.S.
Pharmacopeia Apparatus II at 50 rpm (or Apparatus
I at 100 rpm) in a volume of 900 mL or less in each of
0.1N HCl, pH 4.6 and pH 6.8 media. Therefore, all
dissolution studies except the USP method (75 rpm),
were performed in three different buffers (pH 1.2, 4.6,
6.8) at 50 rpm. Dissolution profiles of both TMP and
SMX were pH-dependent. When the USP method
(pH 1.2, 75 rpm) was used, both TMP and SMX in
test and reference products dissolved more than
85% of the labeled amount of the drug in 15 min, the
profile comparison with and f1 and f2 tests was, thus,
unnecessary. Although the dissolution profiles of
A.
Released Amount (%)
T
120
100
80
60
40
20
0
0
10
20
30
40
50
60
Time (h)
Released Amount (%)
B
T
120
100
80
60
40
20
0
0
10
20
30
40
50
60
Time (h)
Figure 3. Mean ( SD) in vitro dissolution profiles
of TMP (A) and SMX (B) from test (T) and reference
(R) products. Dissolution studies were performed in
0.1 N HCl (900 mL) with paddle rotation speed of
75 rpm.
TMP obtained for test and reference products at pH
1.2 medium (50 rpm) were similar, based on f1 and f2
values, the dissolution profiles of TMP were dissimilar
for other conditions (pH 4.6 and 6.8 with 50 rpm). In
the case of SMX, for all three dissolution media given
above, all dissolution profiles obtained for test and
reference formulations were different. All these results
indicate that dissolution studies are not sufficient to
demonstrate the similarities of these tablet formulations,
and that further in vivo studies are required.
REFERENCES
1. Guidance for Industry: Dissolution testing of
immediate release solid dosage forms. Food and
Drug Administration, CDER, 1997. Retrieved
from www.fda.gov/cder/guidance/index.htm
2. EMEA: CPMP Note for guidance on the investigation of bioavailability and bioequivalence,
CPMP, July 2001.
3. Food and Drug Administration, Guidance
for Industry: Waiver of in vivo bioavailability
and bioequivalence studies for immediate
release solid oral dosage forms based on a
biopharmaceutics classification system, Food
and Drug Administration, Rockville, MD, 2000.
Retrieved from www.fda.gov/cder/guidance/
index.htm.
4. Martindale, The Complete Drug Reference.
Thirty-third Edition. 2002. London S.C.
Sweetman (Ed.), Pharmaceutical Press.
5. Avgerinos A., Athanasiou G., Malamataris S.,
Rapid simultaneous determination of trimethoprim sulphametoxazole and acetylsulphametoxazole in human plasma and urine by highperformance liquid chromatography. J. Pharm.
Biomed. Analysis, 9(6): 507-510, 1991.
6. Garg S.K., Ghosm S.S., Mathur V.S. Comparative
pharmacokinetic study of four different sulfanamides in combination with trimethoprim in human volunteers. Int. J. Clin. Ther. Toxicol., 24(1): 2325, 1986.
7. Patel R.B., Welling P.G. Clinical pharmacokinetics of co-trimoxazole (trimethoprim-sulphamethoxazole). Clin. Pharmacokinet., 5: 405-423, 1980.
8. Petri W.A. Jr. Sulfonamides, trimethoprimsulfamethoxazole, quinolones, and agents for
urinary tract infections. Chapter 43. In: Goodman
and Gilmans The Pharmacological Basis of
Therapeutics. 8th edition. New York, 2006. A.G.
Gilman, T.W. Rall, A.S. Nies, P. Taylor (Eds.) The
McGraw-Hill.
93
Sayar, ahin, Cevherolu, Hncal
9. Amidon G.L. Lennernas H., Shah V.P. Crison J.R.
A theoretical basis for a biopharmaceutics drug
classification: the correlation on an in vitro drug
product dissolution and in vivo bioavailability.
Pharm. Res., 12, 413-420, 1995.
10. Wu C-Y., Benet L.Z. Predicting drug disposition
via application of BCS: Transport/ absorption/
elimination interplay and development of a biopharmaceutics drug disposition classification
system. Pharm. Res., 22 (1):11-23, 2005.
11. The United States Pharmacopeia XXII,
Dissolution <711>, 1990, p 1294.
12. FDA, Guidance for industry. Q2B Validation
of analytical procedures: methodology, US
department of healthy, food and drug
administration, center for drug evaluation and
research, 2001.
13. Liberman H.A.,
Lachman L., Schwatz J.B.
Pharmaceutical Dosage Forms: Tablets. Second
Edition, Revised and Expanded. Marcel and
Dekker Inc., New York and Basel, 1990.
94
14. Florence A. T., Halbert G. W. Formulation. In:
Comparative medicinal chemistry: The rational
design, mechanistic study and therapeutic
application of chemical compound. Hansch, C.,
Sammes, P. G. and Taylor, J. B. (Eds). 1 st Edition.
Pergamon Press Plc; 1990. Vol. 6. p. 567-592.
Oxford , UK .
15. Siewert M., Dressman, J., Brown C. K., Shah V.
P. FIP/AAPS Guidelines to dissolution/ in vitro
release testing of novel/special dosage forms.
AAPS PharmSciTech, 4 (1) Article 7 (www.
pharmscitech.org), 2003.
16. Sayar E. Jenerik Bir Trimetoprim ve
Slfametoksazol Tablet zerinde BSS ve
Biyoedeerlik
almalar.
Hacettepe
niversitesi,
Salk
Bilimleri
Enstits,
Biyofarmastik ve Farmakokinetik Program,
Doktora Tezi, Ankara, 2005.
You might also like
- JPSR 03110106Document9 pagesJPSR 03110106sunilpdNo ratings yet
- Effect of Disintegrant Mode on Drug ReleaseDocument9 pagesEffect of Disintegrant Mode on Drug ReleaseIka YulianaNo ratings yet
- Biorelevant Dissolution: Methodology and Application in Drug DevelopmentDocument7 pagesBiorelevant Dissolution: Methodology and Application in Drug DevelopmentLudmila KawakamiNo ratings yet
- Coating Polymers For Colon Specific Drug Delivery: A ComparativeDocument7 pagesCoating Polymers For Colon Specific Drug Delivery: A ComparativeUmamahesh YadavNo ratings yet
- Dissolution Stability Study of Cefadroxil Extemporaneous SuspensionsDocument8 pagesDissolution Stability Study of Cefadroxil Extemporaneous Suspensionseinas omerNo ratings yet
- In Vivo and in Vitro Evaluation of Four Different Aqueous Polymeric Dispersions For Producing An Enteric Coated TabletDocument6 pagesIn Vivo and in Vitro Evaluation of Four Different Aqueous Polymeric Dispersions For Producing An Enteric Coated TabletSara QuirozNo ratings yet
- Evaluation of Dissolution Behavior of Paracetamol SuspensionsDocument6 pagesEvaluation of Dissolution Behavior of Paracetamol SuspensionsAyman KaramNo ratings yet
- Development and Evaluation of Buccoadhesive Propranolol Hudrochloride Tablet Formulations Effect of FillersDocument7 pagesDevelopment and Evaluation of Buccoadhesive Propranolol Hudrochloride Tablet Formulations Effect of FillersCesar Rodolfo Angulo DelgadoNo ratings yet
- Development and Validation of A Dissolution Test With Spectrophotometric Analysis For Gemifloxacin in Tablet Dosage FormDocument6 pagesDevelopment and Validation of A Dissolution Test With Spectrophotometric Analysis For Gemifloxacin in Tablet Dosage FormwiracanaNo ratings yet
- 608 2616 1 PBDocument5 pages608 2616 1 PBKeerthy VenthenNo ratings yet
- Once-Daily Sustained-Release Matrix Tablets of Metoprolol Tartrate: Formulation and In-Vitro EvaluationDocument5 pagesOnce-Daily Sustained-Release Matrix Tablets of Metoprolol Tartrate: Formulation and In-Vitro EvaluationAryanto DedyNo ratings yet
- Simultaneous Determination Ofloxacin + Ornidazole - SpectrophotometricDocument6 pagesSimultaneous Determination Ofloxacin + Ornidazole - SpectrophotometricNájla KassabNo ratings yet
- Caf5 PDFDocument5 pagesCaf5 PDFeinas omerNo ratings yet
- Abstract Fast Dissolving TabletsDocument7 pagesAbstract Fast Dissolving TabletsRamakant SharmaNo ratings yet
- Esomeprazole SR Tablet FormulationDocument9 pagesEsomeprazole SR Tablet Formulationsyed ali mesum rizviNo ratings yet
- Chapter.3 Review of LiteratureDocument5 pagesChapter.3 Review of LiteratureUmesh PrajapatiNo ratings yet
- Novel Starch Controls Drug Release Under Various ConditionsDocument16 pagesNovel Starch Controls Drug Release Under Various ConditionsBagus MaradiNo ratings yet
- Development and Validation of A Dissolution Method With Spectrophotometric Analysis For Diacerhein CapsulesDocument14 pagesDevelopment and Validation of A Dissolution Method With Spectrophotometric Analysis For Diacerhein CapsulestarakeshwararaoNo ratings yet
- 945C9B625252Document11 pages945C9B625252dini hanifaNo ratings yet
- Effect of excipients like sorbitol on drug bioequivalenceDocument8 pagesEffect of excipients like sorbitol on drug bioequivalenceDanaeNo ratings yet
- Stability of Metronidazole, Tetracycline HCL and Famotidine Alone and in CombinationDocument13 pagesStability of Metronidazole, Tetracycline HCL and Famotidine Alone and in CombinationDean D. PrahitaNo ratings yet
- In Vitro Release Kinetics Study of Diltiazem Hydrochloride From Wax and Kollidon SR Based Matrix TabletsDocument8 pagesIn Vitro Release Kinetics Study of Diltiazem Hydrochloride From Wax and Kollidon SR Based Matrix TabletsSajid Khan SadozaiNo ratings yet
- Formulation and Evaluation of Pregabalin Sustained Release TabletsDocument8 pagesFormulation and Evaluation of Pregabalin Sustained Release TabletsRisman BarkahNo ratings yet
- Development and Validation of A Simple HPLC Method For Simultaneous in Vitro Determination of Amoxicillin and Metronidazole at Single WavelengthDocument5 pagesDevelopment and Validation of A Simple HPLC Method For Simultaneous in Vitro Determination of Amoxicillin and Metronidazole at Single WavelengthAnkit VishnoiNo ratings yet
- Floating and Sustained-Release Characteristics of Effervescent Tablets Prepared With A Mixed Matrix of Eudragit L-100-55 and Eudragit E PODocument6 pagesFloating and Sustained-Release Characteristics of Effervescent Tablets Prepared With A Mixed Matrix of Eudragit L-100-55 and Eudragit E POJozef Al-GousousNo ratings yet
- Formulation and in Vitro Evaluation of Lansoprazole MicropelletsDocument11 pagesFormulation and in Vitro Evaluation of Lansoprazole MicropelletsVaibhavi JangdeNo ratings yet
- Valsartan Orodispersible Tablets Formulation in VIDocument9 pagesValsartan Orodispersible Tablets Formulation in VIRosa MarquezNo ratings yet
- Formulation, Development and Evaluation of Gastroretentive Mucoadhesive Matrix Tablets Using Natural Polymers For Treatment of DepressionDocument15 pagesFormulation, Development and Evaluation of Gastroretentive Mucoadhesive Matrix Tablets Using Natural Polymers For Treatment of DepressionabhitavNo ratings yet
- 71654-Article Text-155265-1-10-20111107Document7 pages71654-Article Text-155265-1-10-20111107Chandresh PatelNo ratings yet
- Cellulose AcetaeDocument11 pagesCellulose AcetaeDhole ArchuNo ratings yet
- MucoadhesifDocument26 pagesMucoadhesifFeny RafnasariNo ratings yet
- The Effect of Polymer Blends On Release Profiles of Diclofenac Sodium From MatricesDocument5 pagesThe Effect of Polymer Blends On Release Profiles of Diclofenac Sodium From MatricesVenkata RakeshreddyNo ratings yet
- 1984 8250 BjpsDocument20 pages1984 8250 BjpsAtiq Ur-RahmanNo ratings yet
- Comparative dissolution studies of Albendazole oral suspensionsDocument4 pagesComparative dissolution studies of Albendazole oral suspensionsDaniiel Miranda ZevallosNo ratings yet
- CumulativeReleaseofadrug PDFDocument4 pagesCumulativeReleaseofadrug PDFkumar purushotamNo ratings yet
- Research Article: May Almukainzi, Arthur Okumu, Hai Wei, and Raimar LöbenbergDocument5 pagesResearch Article: May Almukainzi, Arthur Okumu, Hai Wei, and Raimar LöbenbergIbrahim Al SharabiNo ratings yet
- Abu Afzal Mohammad Shakar Et Al (2012)Document6 pagesAbu Afzal Mohammad Shakar Et Al (2012)neil_vidhyaNo ratings yet
- Bladh 2007Document10 pagesBladh 2007NitaParkNo ratings yet
- Comparison of Lamivudine Tablet Dissolution ProfilesDocument6 pagesComparison of Lamivudine Tablet Dissolution ProfilesEmanuel CudemosNo ratings yet
- Comparative Bioequivalence Studies of Three Brands of Paracetamol With Panadol in Healthy Human VolunteersDocument4 pagesComparative Bioequivalence Studies of Three Brands of Paracetamol With Panadol in Healthy Human VolunteersNur Aini IktikhafsariNo ratings yet
- HPMCP & Cap As Enteric Coated &chitosan As Sustained ReleaseDocument9 pagesHPMCP & Cap As Enteric Coated &chitosan As Sustained ReleasejackbahlulNo ratings yet
- 4845-Article Text-28360-1-10-20150930Document4 pages4845-Article Text-28360-1-10-20150930Andika VarelNo ratings yet
- International Journal of Pharma and Bio Sciences V1 (2) 2010Document14 pagesInternational Journal of Pharma and Bio Sciences V1 (2) 2010Shulisamin PranataNo ratings yet
- Literature Review of Matrix Technique IbuprofenDocument9 pagesLiterature Review of Matrix Technique IbuprofenkharemixNo ratings yet
- Literature ReviewDocument10 pagesLiterature Review006giriNo ratings yet
- Validation of Analytical Method for Meloxicam DeterminationDocument16 pagesValidation of Analytical Method for Meloxicam DeterminationBerlian Rizky PutraNo ratings yet
- Brezofil PDFDocument4 pagesBrezofil PDFzahid kamal100% (1)
- Stabilitas ObatDocument11 pagesStabilitas ObatM Nadi FerdiansyahNo ratings yet
- Comparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsDocument5 pagesComparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsgeoaislaNo ratings yet
- 6 - Suvg - F.G. - 39-46Document8 pages6 - Suvg - F.G. - 39-46Valentina AnutaNo ratings yet
- JURNAL PEDIATRI 19-Vol.-3-Issue-1-Jan.-2012-RA-963-Paper-19Document3 pagesJURNAL PEDIATRI 19-Vol.-3-Issue-1-Jan.-2012-RA-963-Paper-19AnditapitalokaNo ratings yet
- 09 - Chapter 3Document44 pages09 - Chapter 3dini hanifa0% (1)
- Evaluation of Micro CapsulesDocument6 pagesEvaluation of Micro CapsulesPeeyush_Sharma_5529No ratings yet
- Simulated Body Fluids CompositionDocument14 pagesSimulated Body Fluids CompositionAnuj Sharma100% (1)
- Tylosin 2006 Vet Art 03Document5 pagesTylosin 2006 Vet Art 03rdvemedimNo ratings yet
- Al Ghazawihavbktyhdi36840Document6 pagesAl Ghazawihavbktyhdi36840Siti AnisadyahNo ratings yet
- My Research PaperDocument10 pagesMy Research PaperMamta AroraNo ratings yet
- Essential Pharmacokinetics: A Primer for Pharmaceutical ScientistsFrom EverandEssential Pharmacokinetics: A Primer for Pharmaceutical ScientistsRating: 5 out of 5 stars5/5 (1)
- A Comprehensive Book on Experimental PharmaceuticsFrom EverandA Comprehensive Book on Experimental PharmaceuticsRating: 5 out of 5 stars5/5 (1)
- Oral Formulation Roadmap from Early Drug Discovery to DevelopmentFrom EverandOral Formulation Roadmap from Early Drug Discovery to DevelopmentElizabeth KwongNo ratings yet
- Removal of Antibiotics From Water by Polymer of Intrinsic Microporosity: Isotherms, Kinetics, Thermodynamics, and Adsorption MechanismDocument14 pagesRemoval of Antibiotics From Water by Polymer of Intrinsic Microporosity: Isotherms, Kinetics, Thermodynamics, and Adsorption MechanismEstefany MartinezNo ratings yet
- Adsorcion Liquido Ionico RevisarDocument8 pagesAdsorcion Liquido Ionico RevisarEstefany MartinezNo ratings yet
- Acceptedproof-Final Levadura Revisar Cefatoxima PDFDocument6 pagesAcceptedproof-Final Levadura Revisar Cefatoxima PDFEstefany MartinezNo ratings yet
- Carbon de Hiervas Adsosrcion PDFDocument12 pagesCarbon de Hiervas Adsosrcion PDFEstefany MartinezNo ratings yet
- Removal of Antibiotics From Water by Polymer of Intrinsic Microporosity: Isotherms, Kinetics, Thermodynamics, and Adsorption MechanismDocument14 pagesRemoval of Antibiotics From Water by Polymer of Intrinsic Microporosity: Isotherms, Kinetics, Thermodynamics, and Adsorption MechanismEstefany MartinezNo ratings yet
- Adsorcion Por Cascara de Nuez RevisarDocument9 pagesAdsorcion Por Cascara de Nuez RevisarEstefany MartinezNo ratings yet
- Adsorcion Liquido Ionico RevisarDocument8 pagesAdsorcion Liquido Ionico RevisarEstefany MartinezNo ratings yet
- Acceptedproof-Final Levadura Revisar Cefatoxima PDFDocument6 pagesAcceptedproof-Final Levadura Revisar Cefatoxima PDFEstefany MartinezNo ratings yet
- 1973 - PDF Revisar Combinado Levadura Con Nanoparticulas de HierroDocument9 pages1973 - PDF Revisar Combinado Levadura Con Nanoparticulas de HierroEstefany MartinezNo ratings yet
- Cinetica PDFDocument9 pagesCinetica PDFEstefany MartinezNo ratings yet
- Adikesavan2015 Levadura Nanoparticulsd de Mgo PDFDocument9 pagesAdikesavan2015 Levadura Nanoparticulsd de Mgo PDFEstefany MartinezNo ratings yet
- Adikesavan2015 Levadura Nanoparticulsd de Mgo PDFDocument9 pagesAdikesavan2015 Levadura Nanoparticulsd de Mgo PDFEstefany MartinezNo ratings yet
- Aritculo Indu 1 PDFDocument14 pagesAritculo Indu 1 PDFEstefany MartinezNo ratings yet
- Afshin2020 Algaa Revisat PDFDocument13 pagesAfshin2020 Algaa Revisat PDFEstefany MartinezNo ratings yet
- Oxidaxion Us H2ho2 PDFDocument12 pagesOxidaxion Us H2ho2 PDFEstefany MartinezNo ratings yet
- 5 QM in One DimensionDocument11 pages5 QM in One Dimensionxaviour111No ratings yet
- Carbon de Hiervas Adsosrcion PDFDocument12 pagesCarbon de Hiervas Adsosrcion PDFEstefany MartinezNo ratings yet
- Recent Technological Advances For The Determination of Food AuthenticityDocument10 pagesRecent Technological Advances For The Determination of Food AuthenticityEstefany MartinezNo ratings yet
- Drug InterationsDocument34 pagesDrug InterationsEstefany MartinezNo ratings yet
- Drug InterationsDocument34 pagesDrug InterationsEstefany MartinezNo ratings yet
- Kaufmann 2011Document17 pagesKaufmann 2011Estefany MartinezNo ratings yet
- Kaufmann 2011Document17 pagesKaufmann 2011Estefany MartinezNo ratings yet
- Drug StabilityDocument12 pagesDrug StabilityJamilNo ratings yet
- AireDocument12 pagesAireEstefany MartinezNo ratings yet
- 26 PDF PDFDocument12 pages26 PDF PDFEstefany MartinezNo ratings yet
- Bioadsorcion de Plomo (HECHO)Document7 pagesBioadsorcion de Plomo (HECHO)Estefany MartinezNo ratings yet
- PEDIATRIC Drug Formulary 2019-20Document56 pagesPEDIATRIC Drug Formulary 2019-20Eva Marie GonzalesNo ratings yet
- Consensus Statement Folic Acid Supplementation During PregnancyDocument2 pagesConsensus Statement Folic Acid Supplementation During PregnancyGeorge CaligaNo ratings yet
- IMCI AnswerDocument8 pagesIMCI AnswerQuia Benjch Uayan100% (3)
- Possible Drugs of Acute GlomerulonephritisDocument10 pagesPossible Drugs of Acute GlomerulonephritisJai - HoNo ratings yet
- Tugas BacaDocument20 pagesTugas BacaWayan FerlyNo ratings yet
- Antifolate Drugs 17970Document19 pagesAntifolate Drugs 17970TES SENNo ratings yet
- CotrimozaxoleDocument3 pagesCotrimozaxoleDane CunananNo ratings yet
- Care and Support Needs of People Living With Hiv and AidsDocument13 pagesCare and Support Needs of People Living With Hiv and AidsSalihu MustaphaNo ratings yet
- Trimethoprim-Sulfamethoxazole-Bactim-DSDocument4 pagesTrimethoprim-Sulfamethoxazole-Bactim-DSAnika Pleños100% (1)
- SulfonamidesDocument9 pagesSulfonamidestabletvoda100% (1)
- Antiinfectious Drugs and Cancer TreatmentsDocument9 pagesAntiinfectious Drugs and Cancer TreatmentsTapas Kumar0% (1)
- CompetitiveStrategy Dolmo PeDocument39 pagesCompetitiveStrategy Dolmo PenoqlwnNo ratings yet
- Joc 911151Document8 pagesJoc 911151Daniel BorgesNo ratings yet
- Sulfonamides: Miss Preeti Verma Assistant Professor Faculty of Pharmaceutical Sciences, Rama University, Kanpur, U.PDocument17 pagesSulfonamides: Miss Preeti Verma Assistant Professor Faculty of Pharmaceutical Sciences, Rama University, Kanpur, U.PYash SinghNo ratings yet
- SupriyaDocument15 pagesSupriyaprajwal karkiNo ratings yet
- Antimicrobial ChemotherapyDocument160 pagesAntimicrobial Chemotherapyokumu atanas0% (1)
- Case Study - HivDocument10 pagesCase Study - HivJoycee BurtanogNo ratings yet
- Sub: Pharmaceutical Chemistry-II: Topic: SulphonamidesDocument28 pagesSub: Pharmaceutical Chemistry-II: Topic: SulphonamidesRam PrajapatNo ratings yet
- Bactrim Oral Suspension and Tablets: What Is in This LeafletDocument5 pagesBactrim Oral Suspension and Tablets: What Is in This LeafletYsrael Laguio JrNo ratings yet
- Pharmacology Notes 201Document49 pagesPharmacology Notes 201Glaren HamiliNo ratings yet
- Pharmacology AT GLIMPSE PDFDocument252 pagesPharmacology AT GLIMPSE PDFBiswarup Das100% (1)
- Pneumocystis Pneumonia Causes, Symptoms, Diagnosis & PreventionDocument16 pagesPneumocystis Pneumonia Causes, Symptoms, Diagnosis & PreventionMaría Luisa MantillaNo ratings yet
- Drug StudyDocument7 pagesDrug StudyDiana Laura LeiNo ratings yet
- E-Poster PresentationDocument1 pageE-Poster PresentationOvamelia JulioNo ratings yet
- Folic Acid Synthesis InhibitorsDocument30 pagesFolic Acid Synthesis InhibitorsPROF DR SHAHMURADNo ratings yet
- AntibioticsDocument10 pagesAntibioticsStevhenson PortacioNo ratings yet
- Antifolate Drugs: Sulfonamides: Pharmacology IvDocument22 pagesAntifolate Drugs: Sulfonamides: Pharmacology IvShashidharan MenonNo ratings yet
- Trimethoprim Sulfamethoxazole (TMP SMZ) Co TrimoxazoleDocument1 pageTrimethoprim Sulfamethoxazole (TMP SMZ) Co TrimoxazoleRenmico Aquino0% (1)
- Cellulitis and Skin Abscess in Adults: TreatmentDocument30 pagesCellulitis and Skin Abscess in Adults: TreatmentsebasNo ratings yet
- Pharmacology Guide to Antimicrobials & ResistanceDocument86 pagesPharmacology Guide to Antimicrobials & ResistanceRuthvi Jain100% (1)