Professional Documents
Culture Documents
Family-Centered Critical Care
Uploaded by
pauljbnCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Family-Centered Critical Care
Uploaded by
pauljbnCopyright:
Available Formats
Family-Centered
Critical Care: A
Practical Approach
to Making It Happen
Elizabeth A. Henneman, RN, PhD, CCNS
Suzette Cardin, RN, DNSc, CNAA
he needs of
f a m i l y
members of
critically ill
patients are
well established: the
need for information, the need for reassurance and support, and the need to
be near the patient. 1-7 Despite a
wealth of evidence supporting
these basic needs, many critical
care units continue to struggle
with implementing or maintaining family-centered critical care.
Elizabeth Henneman has been a
critical care nurse, clinical nurse
specialist, and nursing educator for
more than 20 years. She has lectured
and published extensively on the
topic of families of the critically ill.
Suzette Cardin has been a critical
care nurse, administrator, and
educator for more than 25 years. She
is nationally renowned for her
expertise in the area of critical care
management.
To purchase reprints contact The InnoVision
Group, 101 Columbia, Aliso Viejo, CA 92656.
Phone, (800) 809-2273 or (949) 362-2050 (ext
532); fax, (949) 362-2049; e-mail,
reprints@aacn.org.
Family-centered care moves
beyond a theoretical recognition
of the centrality of patients family
members in healthcare. A familyfocused unit views a patients
family as the unit to be cared
for and organizes care delivery
around the patients family, as
opposed to the more traditional
patient-centered model.4
Providing family-centered
care is not a simple endeavor. Our
experience indicates that units
that are successful in adopting a
family-centered approach typically have characteristics such as
strong leaders, a caring staff, and
the support of a committed multidisciplinary team. Promoting a
family-centered environment
takes time and patience. Members of the team who may be
resistant to a change to familycentered care typically have very
real concerns that are based on
their underlying beliefs and
attitudes. For example, research
suggests that nurses may view
visitors as physiologically stressful
to patients and thus will try to
restrict visitation in order to protect patients.8 Limiting visitation
in the intensive care unit is also
12 CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002
perceived as important for patients family members, to allow
them time to care for themselves
and prevent exhaustion.8
Our current healthcare era,
marked by consumerism, shorter
stays in the intensive care unit
and the hospital, and nursing
shortages, makes family-centered
critical care less of an option than
it once was. Family members are
now active participants in planning the care of their loved ones.
Shorter hospital stays mean that
patients family members are taking on an ever-increasing role as
direct caregivers. Higher acuity of
patients and nursing shortages
mean that family members will
play a critical role in the delivery
of care both in and out of the hospital. It is not only inappropriate
but also impractical to ignore
family members waiting outside
the double doors to the critical
care unit. The time has come to
embrace the family members of
our patients and integrate them
into a holistic plan of care.
Although much has been written about the needs of patients
families and the need for change
in practice, little has been pub-
lished about how to make familycentered care work. Our purpose
in this article is to offer practical
suggestions for implementing or
improving family-centered care in
the critical care environment. We
think that the information presented in this article, which is
based on research and our own
experiences, will be useful to clinicians and administrators who are
committed to fostering familycentered care.
STEP 1: KNOW WHAT
FAMILY-CENTERED
CRITICAL CARE
REALLY MEANS
Much confusion remains over
what family-centered critical care
actually is. Many clinicians incorrectly equate family-centered
care with open visiting. This misconception stems, in part, from
the widespread implementation
of policies for flexible visiting
hours in units that are attempting to provide more family-oriented care. Family-centered care
is not a singular intervention but
rather a philosophical approach
to care that recognizes the needs
of patients family members as
well as the important role that
family members play during a
patients illness.
No single intervention and not
even a group of interventions will
ensure a family-focused environment. For example, it would be
incorrect to assume that simply
allowing a family member to be at
a patients bedside 24 hours a day
would mean the staff was meeting
the familys needs. In fact, having
a family member present in a situation in which staff members are
not equipped to meet the familys
needs could ultimately have
adverse consequences. Family
members may be more stressed if
they are ignored by a nurse or are
made to believe that they are
somehow in the way or interfering
with the patients care.
In many ways, family-centered
care can be thought of as an
extension of patient-focused care,
a concept that gained widespread
attention in the early 1990s. The
underlying premise of patientfocused care was that delivery of
care should be centered on the
needs of the patient as opposed to
a more traditional approach in
which care was based on what
worked well from an organizational perspective. Family-centered
care simply takes patient-focused
care to the next step and widens
the circle of concern to include
those persons who are important
in a patients life.
The confusion over family-centered care often gives way to frustrations for many staff members
who think that family-focused care
may not be in the best interest of
either patients or nurses. For example, family-centered care does
not mean that patients lose their
rights to privacy or control over
their environment. Patients who
are able should always be asked to
what extent (if any) they want
their family to participate in care.
Patients may, in fact, not want any
visitors or any information given
out to family members. Familycentered care simply recognizes
the familys involvement as a
choice and lets patients know that
family members are welcome
should the patients so choose.
The important point that we
must stress here is that the needs
of the patient are always the priority, even in a family-centered environment. Research indicates that
it is important to patients family
members to be assured that the
patient is receiving the best possi-
ble care. 9 Interventions such as
having family members present
during procedures and resuscitations help to reassure family
members that everything possible
is being done for the patient. 8
Meeting a patients needs should
always be the priority for both the
patients family and the nurse.
Staff members are also sometimes concerned that familycentered care demands that staff
relinquish all structures within
the unit that allow some semblance of order in this otherwise
chaotic environment. This concern is absolutely not the case.
During a critical illness, patients
families will benefit from guidance and structure to help them
to cope. What a family-centered
philosophy does require is that
outdated rules and regulations
that were imposed for the benefit of the organization rather
than patients or patients families should be reexamined.
Structures (such as assessment
tools) and policies that provide
for the support and safety of
patients and their family members are generally welcomed by
family members and help staff
members to carry out their responsibilities in a timely and efficient
manner.
One intervention that can be
useful in clarifying misconceptions about family-centered care
is to post an informational flyer in
the unit (Table 1). This type of
document gives staff members
straightforward, useful information that clarifies a sometimes
nebulous concept. It is helpful for
staff members to see that the essence of family-centered care is
consistent with patient-centered
care. In addition, staff members
are often reassured by knowing
that boundaries and limitations
CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002 13
Table 1 Family-centered critical care: what it is and is not
What it is
Family-centered care is a philosophical approach for providing care to patients
and their families. The basic premise of this philosophy is that patients are part
of a larger "whole" of which we must be aware if we are to provide the best
possible care.
Family-centered care is care that demands a collaborative approach to care in
which all members of the team support and value this philosophy.
Providing care that is family centered means that we recognize our responsibility
to help the family as well as the patient survive the crisis of an illness. It means
we have an obligation to meet the 3 basic needs of the family:
1. The need for information
2. The need for reassurance/support
3. The need to be near the patient
What it is not
Family-centered care is not new. Many clinicians (such as in pediatrics) have
been practicing family-centered care for a long time with much success.
Family-centered care does not mean that staff must relinquish all decision
making to patients family members. Patients families need and appreciate
structure and guidance during a time of crisis.
Family-centered care does not mean that patients families have the right to be
rude or abusive to staff.
Family-centered care is not difficult, but it requires a thoughtful and caring
appreciation of the needs of patients and their families.
are still in place and that the
expertise of staff members remains
a critical factor in ensuring the
success of family-centered care.
Although not all encompassing,
such a flyer gives the staff a chance
to see in writing what family-centered care is and is not and provides a point for future discussion.
STEP 2: KNOW
WHAT THE NEEDS
OF FAMILIES
REALLY ARE
As mentioned previously, the
most important needs of families
of critically ill patients are the
need for information, the need for
reassurance and support, and the
need to be near the patient. 1-7
Although seemingly straightforward, these needs can be inter-
preted in many ways. Depending
on how the needs of families are
interpreted, nurses may have concerns about their ability to meet
those needs in addition to all their
other responsibilities for patients.
Thus, it is important that nurses
receive clarification about what
meeting needs of patients families actually entails.
For some family members, the
crisis of their loved ones illness has
created a situation that requires
more intensive family support or
counseling. In these situations,
additional help and support from
our colleagues in social services
and spiritual care is required.
However, nurses can be reassured
that for most family members,
important needs can be met by
basic nursing interventions such
14 CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002
as giving information about the
patients well-being, providing
reassurance, and offering families
a flexible visiting schedule.
The Need for Information
The type of information that
families want from nurses is
related to the patients general
well-being. Patients family members look to nurses for information about vital signs (stable vs
unstable), comfort level, and
sleeping patterns. They do not
expect the nurses to give information about prognosis, diagnosis, or treatment plan. 2 This
statement does mean that nurses
cannot or should not give this
type of information. Nor should
it suggest that nurses do not play
an important role in helping
patients family members understand or interpret this type of
information. It simply means
that nurses should not feel overwhelmed or be concerned about
the amount of information they
are expected to impart to patients families. Nurses have several roles related to meeting the
information needs of patients
families. One is to assess the
families needs and ensure that
the appropriate party addresses
their questions and concerns.
The other is to be familiar with
the information given to families
by others and to provide clarification when questions or concerns arise.
The Need for Reassurance
and Support
Family members need to know
that their loved one is being cared
for in the best way possible and
that everything that can be done is
being done. The need for reassurance and support does not mean
that families want false hope for
a recovery that will not occur.
Dramatic examples of providing
reassurance and support often
occur in situations in which a patient is dying and the patients
family is assured that the patients
comfort is the ultimate priority.
When a patient is dying, assisting
with end-of-life issues is of great
value and comfort to both the patient and the patients family. The
most effective means of providing
reassurance and support often has
little to do with spoken words, but
rather are demonstrated to the
family by the gentle ministering of
a caring practitioner.
The Need to Be With
the Patient
Family members want to be
near their loved ones who are sick.
Not only do they want to provide
support by being there but also
physical presence allows them to
witness how their family member
is being cared for. The success of
flexible visiting practices may
stem, in part, from simply allowing patients and their families to
be together, thereby facilitating
meeting the families needs for
information and support.
Although the needs of family
members may seem straightforward, it is a mistake to assume that
all personnel working in the unit
know what these needs are. Multiple interventions must be implemented by unit managers and
clinicians interested in promoting
a family-centered approach. Strategies such as hanging colorful
posters outlining the needs of patients families in high-visibility
areas in staff conference rooms or
including a list outlining those
needs in a hospital/staff newsletter
can be effective in increasing staff
awareness.
STEP 3: INTEGRATE
FAMILY-CENTERED
VALUES INTO YOUR
UNITS STANDARDS
AND POLICIES
Units with family-centered
philosophies incorporate familycentered care into all appropriate
standards and policies for the
units. It is important to translate
this philosophy into concrete messages for patients, their families,
and staff. For example, family
members should be told on their
first visit that the unit has a family
focus. New staff members should
also be made aware of the units
family focus. The nurse recruiter
or manager interviewing potential
employees should emphasize the
role of all staff members in meeting the needs of patients families
(Table 2).
Hospital and unit administrators play a key role in ensuring that
family-centered care is valued in
the organization. Administrators
can serve as powerful role models
by participating in decisions related
to family-centered care and in
valuing and rewarding staff members who demonstrate familyfocused behaviors (Table 2).
STEP 4: USE
HOSPITAL
RESOURCES TO
PROVIDE FAMILYCENTERED CARE
Bedside nurses cannot meet
the needs of patients families and
take care of the patients all by
themselves. The key to effective
family-centered care is to train all
staff members about the needs of
patients families. Programs related
to meeting the needs of patients
family members must include
every member of the healthcare
team.
Unit secretaries, security
guards, volunteers, housekeepers,
and aides are often the first contact that patients families have
with the hospital or unit. These
persons can be enormously helpful and effective in providing support to the family members. For
example, instead of being viewed
as gatekeepers, unit secretaries
should function as liaisons between patients families and nursing staff, assisting in relaying
information and helping support
family-centered decisions (such
as appropriateness of visitation).
Hospital volunteers have been
successfully employed as family
caregivers in an intensive care
unit to provide nonmedical information, comfort, and support.10
Professional support from our
colleagues in medicine, social
work, and pastoral care is essential
if family-centered critical care is to
be effective. Unfortunately, the expertise of these professionals is
often not sought out until a crisis
has occurred. A better strategy is
to have standards that provide a
consistent, proactive approach to
Table 2 Examples of familyfocused statements from employee
interview and performance
evaluation
Interview
1. Describe a situation in which a
patient/family was upset and how
you intervened.
Performance evaluation
1. Provides age-appropriate
assessment and interventions to
meet needs of patients/families
served.
2. Directs and supports alternative
teaching strategies based on
response, knowledge, and skills of
patient/family/significant other.
Reproduced with permission from UCLA Medical
Center, Los Angeles, Calif.
CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002 15
meeting the needs of patients
families.
STEP 5: CREATE
TOOLS TO HELP
A variety of tools such as information booklets and checklists
have been suggested as ways to
meet the information needs of patients families. 11,12 Information
booklets provide family members
with concrete information about
who is who and what to expect in
a unit. Checklists outlining the
specifics of what to say and do
during a family members visit are
especially helpful for new employees and ensure consistency
from one staff member to the
next11 (Table 3). Family-centered
assessment tools and policies are
other examples of structures that
support family-centered care
(Tables 4 and 5).
Teaching materials related to
procedures, including routine
bedside care, can be helpful to
patients families and can save
nursing time. For example, family
members can be taught to provide basic care such as passive
range of motion and mouth care.
Instructions for these basic care
procedures can be posted in the
patients room for a reference,
along with a list of family members
who have received instructions
and have demonstrated that they
can successfully provide the care.
STEP 6: DO NOT
CONFUSE FAMILY
ISSUES WITH
SECURITY OR
CONFIDENTIALITY
ISSUES
Concern over violence in the
workplace is a frequent deterrent
Table 3 Example of family assessment/information checklist to be used at
initial admission and during follow-up family visits
Initial visit
1. Introduce yourself as soon as possible. Determine the relationship of the
family member to the patient.
2. Give the patient/family information about the routine/plan. (Example: "I will be
asking some questions, taking your blood pressure, etc, and then the doctor
will be in to see you.")
3. Offer the patient/family a copy of your information booklet. Point out
important information. Write your name on the booklet.
4. Review the visiting policy. Let them know that you have a family-focused unit
and that they are welcome!
5. Give them the "family phone" number. Make sure it is written on the booklet.
Reassure them that its OK to call and inquire about their loved ones
condition.
6. Always ask if they have questions or concerns before you walk away.
Follow-up visits
1. Introduce yourself. If you dont already know, find out who the visitor is and
his or her relationship to the patient. Find out if this is the visitors first visit.
2. Give a brief update on the patients condition.
3. Ask for questions/concerns.
4. Ask if the visitor would like to speak with a physician or other team member.
5. Assess desire/ability to participate in patient care activities (cool cloth, ice
chips, etc). MAKE NO ASSUMPTIONS!
6. Encourage family members to bring in familiar objects (pictures/music/stuffed
animals).
16 CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002
to establishing a family-centered
environment. Obviously, the safety
of staff members and patients is a
primary concern. All security issues
must be addressed, and steps must
be taken to ensure safety. On the
other hand, the potential for violence should not preclude patients
and families from being together
and having their needs met during
a critical illness.
One approach to attending to
security and family issues is to
include representatives from the
hospital security department in
discussions and planning when
visiting policies are being examined. The expertise of these team
members will be valuable not only
initially but also later as problems
and concerns arise.
Front-line personnel such as
security teams play a critical role
in ensuring that the needs of patients and patients family members are met. As initial responders
or greeters, these personnel set
the standards and expectations
for patients families. The primary
message conveyed to family
members should be that they are
valued and welcome. At the same
time, however, it should be made
clear that there are certain standards (eg, calling before entering
the unit) that must be adhered to.
STEP 7: BE
CONSISTENT WITH
PATIENTS FAMILIES
A frequent concern voiced by
patients and their families is the
inconsistency in the information
they receive. Perhaps the most
classic example of this inconsistency is related to visiting hours.
It is quite typical for individual
nurses to be comfortable letting
patients family members visit
quite liberally, regardless of the
actual visiting policy. When
Table 4 Sample of a family-focused initial assessment tool
Who usually supports you through difficult or stressful situations?
Family
Friends
Support group
Church group
Other
Would you like your family present during our morning rounds when we review
your condition and plan of care?
Yes
No
What is the best time for your family to communicate with the MICU Team?
Anytime
Mornings
Afternoons
Evenings
Dont know
Note to family members:
We understand that an illness can be very stressful to the family as well as the
patient. Is there anything special that we need to know about your family
member that will help us to better help you?
__________________________________________________________________________
__________________________________________________________________________
Reproduced with permission from the medical intensive care unit (MICU), UCLA Medical Center, Los Angeles,
Calif.
another nurse comes along on the
next shift or sometimes days later
and enforces the written policy,
confusion and often anger ensues
from the family members even
though the second nurse may actually be following the policy as it
is written.
Inconsistency wreaks havoc
with families who are struggling
to maintain some control over an
otherwise uncontrollable situation. When they see inconsistency
in a visiting policy, they may start
to question the existence of other
inconsistencies, such as how treatments are carried out and how individual nurses manage patients
problems (eg, pain).
Inconsistencies are also detrimental to staff members and set
up a good nursebad nurse
phenomenon that is difficult to
resolve. Antiquated visiting practices that restrict patients families are a good example of a policy
that sets up nurses to fail as they
struggle to meet the needs of
Table 5 Family-focused visiting hour policy
Purpose: To provide guidelines for visitors and patients at UCLA Medical
Center.
Policy: Visiting hours may be modified on any patient care unit to meet the
needs of the patient and the patients visitors. Patient care areas with 24-hour
visiting (eg, critical care) will provide visitors with specific information regarding
the units regulations.
Visiting regulations, specialized units: The intensive care units welcome
visitors 24 hours a day with the exception of change-of-shift report, 7-8 AM and
7-8 PM. The nursing staff determines the number of visitors who may be present
at the bedside at any one time.
Reproduced with permission from UCLA Medical Center, Los Angeles, Calif.
18 CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002
patients families by bending the
rules. The way to deal with this
problem is to establish policies
that allow nurses to coordinate visits depending on the needs of a
patient and his or her family as
opposed to establishing rules.
One of the most important
things nurses can do to help patients and patients family members cope during the crisis of an
illness is to be consistent. Consistency means that standards of
care are applied in the same way
to every patient and his or her
family, every time.
Ensuring that a consistent
standard of care is maintained
falls under the purview of the governing bodies of the critical care
units. The unit-based critical care
committee, together with nursing
and physician directors, plays an
important role in ensuring that
standards of care for patients and
patients families are met.
STEP 8: MAKE
FAMILY-CENTERED
CARE A
MULTIDISCIPLINARY
GROUP ENDEAVOR
Perhaps the biggest mistake a
unit can make is to view familycentered care as solely within the
domain of nursing. All members
of the team who have contact with
patients families play an important role in ensuring that the families needs are met. Among others,
these team members include physicians, nurses, respiratory therapists, physical therapists, pastoral
care, social workers, and dieticians. From the start, leaders
interested in promoting a family
focus must recognize the unique
contribution and expertise of
each member of the team relative
to the patients families in the unit.
When family care is a team func-
tion, not only do patients and their
families benefit, but also nurses
will be less overwhelmed with the
responsibility to provide care.
Most successful family-centered programs have a few key
persons who are committed to
making family-centered care happen in their organization. Together with key players in the
organization, this group serves as
the steering committee, exploring ways to prepare the staff and
create necessary changes.
STEP 9: RECOGNIZE
THE NEED FOR
ONGOING
ATTENTION AND
SUPPORT
Implementing a family-centered approach to care is only the
beginning of an ongoing institutional commitment. As is the case
with any process of change, the
more preparation that goes into
implementation, the more smoothly the process will ultimately go.
However, regardless of the preparation, new challenges and issues
will inevitably arise in an organization dedicated to family-centered care.
It is unreasonable to expect
that staff members will suddenly
know how to handle every situation simply because a change in
philosophy has occurred. Time
must be devoted at unit staff meetings, conferences, or unit retreats
to discuss challenging cases and
concerns and to solve problems.
Adopting a family-centered
approach also does not mean that
difficult or challenging families will disappear. Despite the
best intentions, philosophies, or
standards, there will always be
patients families with needs different from the norm. However
disheartening or frustrating these
situations may be, everyone
involved should try to view these
families as the exception rather
than the rule. One goal of familycentered care should be to have
fewer of these challenging family
situations as a result of standards
of care that are proactive in meeting families needs. Early, aggressive, consistent attention to
patients family members can dissipate many of the typical family
concerns that could erupt into
more serious issues if the concerns
are not addressed.
5.
6.
7.
8.
9.
10.
STEP 10: BE PATIENT
Establishing a family-centered
unit does not happen overnight.
Adopting a family-centered philosophy and then creating standards and policies to support that
philosophy take time.
11.
12.
and future directions. Crit Care Clin
North Am. 1992;4:645-649.
Jamerson PA, Scheibmeir M, Bott MJ,
Crighton F, Hinton RH, Cobb AK. The
experience of families with a relative in
the intensive care unit. Heart Lung.
1996;25:467-474.
Price DM, Forrester A, Murphy PA,
Monaghan JF. Critical care family needs
in an urban teaching medical center.
Heart Lung. 1991;20:183-188.
Meyers TA, Eichhorn DJ, Guzzetta CE, et
al. Family presence during invasive procedures and resuscitation: the experience of family members, nurses and
physicians. Am J Nurs. February
2000;100:32-42.
Kirchhoff KT, Pugh E, Calame RM,
Reynolds N. Nurses beliefs and attitudes toward visiting in adult critical
care settings. Am J Crit Care. 1993;2:238245.
Haln MA. Support and reassurance
needs. Crit Care Clin North Am.
1992;4:633-643.
Appleyard ME, Gavaghan SR, Gonzalez
C, Ananian L, Tyrell R, Carroll DL.
Nurse-coached interventions for the
families of patients in critical care units.
Crit Care Nurse. June 2000;20:40-48.
Ward CR, Constancia PE, Kern L.
Nursing interventions for families of cardiac surgery patients. J Cardiovasc Nurs.
1990;5:34-42.
Henneman EA, McKenzie JB, Dewa CS.
An evaluation of interventions for meeting the information needs of families of
critically ill patients. Am J Crit Care.
1992;1:85-93.
CONCLUSION
The time has come to embrace
the practice of family-centered
care. Patients and their families
have basic needs that must be
met if healthcare institutions are
to be successful in addressing
consumers needs and providing
holistic care.
Strategies for ensuring successful family-centered care are not
difficult, but they require embracing a philosophy that recognizes the needs of patients
families and the value of a proactive approach to ensuring that
those needs are consistently met.
References
1. Molter NC. Needs of relatives of critically ill patients: a descriptive study. Heart
Lung. 1979;8:332-339.
2. Daley L. The perceived immediate needs
of families with relatives in the intensive
care setting. Heart Lung. 1984;13;231-237.
3. Leske JS. Needs of relatives of critically
ill patients: a follow up. Heart Lung.
1986;15:189-193.
4. Hickey ML, Leske JS. Needs of families of
critically ill patients: state of the science
CRITICAL CARE NURSE Vol 22, No. 6, DECEMBER 2002 19
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Writing Case Notes SamplesDocument14 pagesWriting Case Notes SamplesJessa Molina71% (7)
- Rhetorical Analysis Rough DraftDocument7 pagesRhetorical Analysis Rough Draftapi-385246270No ratings yet
- Group 6 PMP Pma Code of Ethics 2Document12 pagesGroup 6 PMP Pma Code of Ethics 2Aya RutledgeNo ratings yet
- High Risk Consent Form: Doctor-In-Charge / Principal Surgeon / Principal InterventionistDocument5 pagesHigh Risk Consent Form: Doctor-In-Charge / Principal Surgeon / Principal InterventionistDrPraveen SharmaNo ratings yet
- Watson's Philosophy and Science of CaringDocument11 pagesWatson's Philosophy and Science of CaringKrishna100% (1)
- Hospital Management SystemDocument30 pagesHospital Management Systemsarah farooqiNo ratings yet
- Residency Manual 2020 28-Dec-2020Document127 pagesResidency Manual 2020 28-Dec-2020Asif KhanNo ratings yet
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankDocument36 pagesAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test Bankgraspingpirai2utcxx100% (9)
- Manager Healthcare Practice Laboratory in Boston MA Resume Eleonora KushilovskyDocument2 pagesManager Healthcare Practice Laboratory in Boston MA Resume Eleonora KushilovskyEleonora KushilovskyNo ratings yet
- Angela Taylor, MSW, LCSW: Social Work ExperienceDocument2 pagesAngela Taylor, MSW, LCSW: Social Work ExperienceKritika NigamNo ratings yet
- DoHS Annual Report FY 2076 77 For WebsiteDocument473 pagesDoHS Annual Report FY 2076 77 For WebsiteAkash AjayNo ratings yet
- Resume Sample For Nurse PractitionerDocument4 pagesResume Sample For Nurse Practitionerf5dvx95v100% (2)
- Full Download Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Test BankDocument35 pagesFull Download Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Test Bankzoism.waygoose.3fuhqv100% (32)
- BurkhartbryceDocument24 pagesBurkhartbryceapi-535300613No ratings yet
- Plab 2 Notes Day 2Document14 pagesPlab 2 Notes Day 2Adnan Al JafaryNo ratings yet
- Hot Sitz BathDocument4 pagesHot Sitz BathJessica TayagNo ratings yet
- Psychological Considerations For Complete Denture Patients.Document7 pagesPsychological Considerations For Complete Denture Patients.Prateek MishraNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For ConstipationDocument4 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For Constipationkenneth_bambaNo ratings yet
- Stephanie's CVDocument3 pagesStephanie's CVmadcat1425No ratings yet
- Jurnal IDocument8 pagesJurnal II Gusti Ayu Agung YuliantiNo ratings yet
- Hubungan Mutu Pelayanan Kesehatan Dengan Tingkat Kepuasan Pasien Rawat Inap Di Rsud Dr. Rasidin PadangDocument7 pagesHubungan Mutu Pelayanan Kesehatan Dengan Tingkat Kepuasan Pasien Rawat Inap Di Rsud Dr. Rasidin PadangEvelyne lubaNo ratings yet
- Oms FeridasDocument136 pagesOms FeridasPauloFerreira0% (1)
- Managing Healthcare QualityDocument7 pagesManaging Healthcare QualityTooba SiddiquiNo ratings yet
- Discourse CommunityDocument6 pagesDiscourse Communityapi-357123936No ratings yet
- Evaluating Effective Lawyer-Client CommunicationDocument29 pagesEvaluating Effective Lawyer-Client CommunicationabctandonNo ratings yet
- Labcorp VoucherDocument2 pagesLabcorp Voucherjesse.777No ratings yet
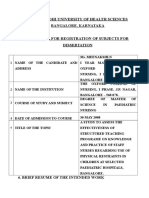
- Rajivgandhi University of Health Sciences Bangalore, KarnatakaDocument19 pagesRajivgandhi University of Health Sciences Bangalore, KarnatakaHUSSAINA BANONo ratings yet
- Role & Importance of Medical Records: Mahboob Ali Khan MHA, CPHQ Consultant HealthcareDocument60 pagesRole & Importance of Medical Records: Mahboob Ali Khan MHA, CPHQ Consultant HealthcareDr. Asma QureshiNo ratings yet
- Medicare Benefit Policy Manual - Chapter 1 PDFDocument52 pagesMedicare Benefit Policy Manual - Chapter 1 PDFDorothy YthorodNo ratings yet
- NSG 123 Reflective Summary Post Surgical Patients 2Document4 pagesNSG 123 Reflective Summary Post Surgical Patients 2api-725909264No ratings yet