Professional Documents
Culture Documents
Vitamin D Viewpoint
Uploaded by
Renan Lopez ViañaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vitamin D Viewpoint
Uploaded by
Renan Lopez ViañaCopyright:
Available Formats
Opinion
VIEWPOINT
JoAnn E. Manson, MD,
DrPH
Division of Preventive
Medicine, Brigham and
Womens Hospital,
Harvard Medical
School, Boston,
Massachusetts.
Shari S. Bassuk, ScD
Division of Preventive
Medicine, Brigham and
Womens Hospital,
Harvard Medical
School, Boston,
Massachusetts.
Author Reading at
jama.com
Corresponding
Author: JoAnn E.
Manson, MD, DrPH,
Division of Preventive
Medicine, Brigham and
Womens Hospital,
Harvard Medical
School, 900
Commonwealth Ave,
Boston, MA 02215
(jmanson@rics
.bwh.harvard.edu).
Vitamin D Research and Clinical Practice
At a Crossroads
Long recognized as important for bone health, vitamin D has attracted recent interest for its possible nonskeletal benefits. Many primary care clinicians now
include blood tests to measure vitamin D concentrations as part of routine laboratory work1 and recommend vitamin D supplements, often at high doses, to
their patients for the possible prevention of cancer,
cardiovascular disease (CVD), diabetes, autoimmune
disorders, cognitive decline, and other conditions.
Thus, screening rates and sales of vitamin D supplements have increased substantially in recent years.1,2
However, clinical enthusiasm for supplemental vitamin D has outpaced available evidence on its effectiveness and threatens to jeopardize the ability of researchers to conduct randomized trials in usual-risk
populations. Based on its recent systematic reviews of
the literature, the US Preventive Services Task Force
(USPSTF) concluded that data are insufficient to recommend vitamin D screening in routine clinical practice1 or
to assess the effectiveness and overall balance of benefits and risks of supplemental vitamin D taken for the
primary prevention of cancer and CVD.3 In an earlier review, the Institute of Medicine (IOM) reached the same
conclusionnamely, whether supplemental vitamin D
lowers risk of nonskeletal health outcomes, and what
dose might be required to do so, is uncertain.4
Given the lack of convincing evidence for nonbone
benefits of vitamin D, the IOM set the recommended dietary allowance (RDA) for vitamin D based on the
amount required for skeletal health: 600 IU per day for
persons aged 1 to 70 years and 800 IU per day for those
71 years and older. This is equivalent to 3 to 4 daily servings of fortified foods such as milk, yogurt, soy beverages, orange juice, or cereal, plus fatty fish twice per
week. These amounts are adequate for at least 97.5% of
US and Canadian residents, including those living in the
north during the winter, and correspond to a total
25-hydroxyvitamin D (25[OH]D) serum concentration of
approximately 20 ng/mL (to convert to nmol/L, multiply by 2.496). Many laboratories consider a level of 30
or 40 ng/mL to be optimal, but the IOM found little research to support this claim. The IOMs report challenges the notion that a majority of US adults are vitamin D deficient and does not endorse universal
25(OH)D testing. Even though there is dissent from some
individual experts,5 no major medical organization endorses population-wide screening for low vitamin D.
Moreover, in addition to the lack of consensus on the
definition of optimal 25(OH)D concentrations, emerging evidence suggests that bioavailable and free
25(OH)D may be more physiologically relevant indicators of vitamin D status than total 25(OH)D.1 Although
these findings cast further doubt on the utility of wide-
spread 25(OH)D testing, they do not negate the importance of targeted vitamin D assessment and therapeutic intervention for patients with risk factors for, or clinical
conditions associated with, vitamin D insufficiency, such
as malabsorption or osteoporosis.
That vitamin D might confer benefits beyond
bone health was first suggested by ecologic studies
showing lower cancer and cardiovascular mortality in
regions with greater exposure to solar UV-B radiation
(associated with greater cutaneous synthesis of vitamin D). Laboratory investigations subsequently confirmed the existence of plausible mechanisms of vitamin D action in pathways relevant to CVD, cancer, and
other chronic diseases, as well as the expression of
the vitamin D receptor and 1-hydroxylase in many
tissues.4,6 Observational studies also provide some
support for nonskeletal benefits, with associations
between low intakes or serum levels of vitamin D and
increased risk for CVD, cancer, diabetes, and other
nonskeletal diseases in some cohorts. However, the
observational data are inconsistent and are susceptible to confounding and other biases that preclude
their use for establishing causality.4,6 Major confounders include outdoor physical activity (which correlates
with sun exposure), adiposity (which decreases
25[OH]D bioavailability), and overall nutritional status. These factors may act singly or in combination to
yield spurious protective effects for vitamin D,
whereas null findings may result from vitamin D
intakes that are too low to yield significant benefits.
Of note, a U-shaped relation has been found in several
cohorts, with elevated risk for adverse outcomes
including CVD and all-cause mortalityobserved at
not only low but also at high levels (50-60 ng/mL of
25[OH]D). 4 These findings suggest that, although
moderate doses of vitamin D may be beneficial, more
is not necessarily betterand may be worse.
Well-designed randomized clinical trials overcome
biases inherent to observational studies and are necessary to establish the long-term consequences of taking
high-dose supplemental vitamin D. However, most vitamin D trials completed to date have been of modest
size and have focused on bone-related outcomes; when
cancer, CVD, or other nonskeletal end points have been
examined, analyses have often been underpowered,
post hoc, and without rigorous end point adjudication.
It is perhaps not surprising that such trials have yielded
mostly null results. To fill the knowledge gap, several
large-scale, general-population vitamin D supplementation trials with cancer, CVD, or total mortality as primary prespecified end points have been launched in the
past 5 years and are under way (Table). In aggregate,
these trials are expected to enroll close to 100 000 par-
jama.com
(Reprinted) JAMA April 7, 2015 Volume 313, Number 13
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Thomas Jefferson University User on 05/13/2015
1311
Opinion Viewpoint
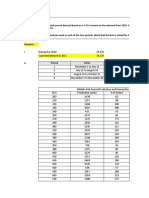
Table. Ongoing Large-Scale Randomized Trials (N10000 Participants) of Vitamin D Supplementation Worldwidea
Trial, Location
Vitamin D and Omega-3
Trial (VITAL), United
States
Sample
Sizeb
Age Range, y
25 874
50 for men;
55 for
women
Treatment
Duration, y
Vitamin D Intervention
2000 IU/d (oral)
D-Health, Australia
20 000
60-84
Finnish Vitamin D trial
(FIND), Finland
18 000
60 for men;
65 for
women
Vitamin D and Longevity
(VIDAL), United
Kingdomc
20 000
65-84
60 000 IU/mo (oral)
Trial Registry No.
NCT01169259
Total mortality, cancer
1600 IU/d or 3200 IU/d (oral) Cancer, CVD
100 000 IU/mo (oral)
Total mortality, cancer
ACTRN12613000743763
NCT01463813
ISRCTN46328341
Abbreviations: CVD, cardiovascular disease.
VITAL has completed recruitment; enrollment for other trials is in progress.
In pilot phase.
Several moderate-sized randomized trials (2000-<10 000 participants) also
are in progress in the United States and worldwide.
ticipants in the United States, Europe, and Australia. Their eventual
results, the first of which are expected to be available in late 2017,
should allow a definitive determination of whether high-dose vitamin D offers a more favorable balance of benefits and risks than
vitamin D taken at the current RDA. However, these trials will be informative only if the results are not diluted by widespread out-ofstudy prescription and use of high-dose vitamin D supplementation in the enrolled populations. Primary care physicians who
routinely screen for 25(OH)D and prescribe high-dose supplements in the absence of a clear clinical indication may reduce differences in intakes between study groups, jeopardizing the opportunity for the trials to yield informative results.
The medical communitys past experience with several other nutritional interventions should raise a note of caution regarding highdose supplementation. Many times in recent decades, promising preliminary findings were not confirmed when rigorously tested in
randomized trials. Large trials of other widely used supplements have
sometimes found benefits, but in other casessuch as with high
doses of beta carotene, vitamin E, and seleniumhave disproven
some health claims for these supplements and identified health risks
that may not have otherwise been detected.3,4,6
Skepticism regarding the value of high-dose vitamin D supplementation is increasing in the research literature. One group of
investigators has asserted the futility of conducting additional
randomized trials, arguing that recent meta-analyses of completed
randomized trials have proven that supplemental vitamin D is largely
ineffective for disease prevention and that future trials are unlikely
to substantially alter these conclusions.7 Although this assertion
could be challenged (because of the aforementioned limitations of
available randomized trial data), this viewpointconsidered in
juxtaposition with that of the IOM and other influential authorities
that more trials are desperately needed8highlights the lack of scientific consensus on vitamin D.
When there is uncertainty about whether supplementation is
warranted, the usual medical principle is to err on the side of caution and to avoid excess. Thus, while awaiting the results of the large
trials now in progress, physicians would be well advised to follow
current USPSTF and IOM recommendations and avoid overscreening and overprescribing supplemental vitamin D. Doing so is not only
in the best interest of current patients but will also help advance
knowledge to benefit future patients and inform future public health
recommendations.
Preventive Services Task Force recommendation
statement. Ann Intern Med. 2015;162(2):133-140.
ARTICLE INFORMATION
Published Online: February 19, 2015.
doi:10.1001/jama.2015.1353.
Conflict of Interest Disclosures: Both authors
have completed and submitted the ICMJE Form for
Disclosure of Potential Conflicts of Interest and
none were reported.
Funding/Support: Drs Manson and Bassuk receive
funding from the National Institutes of Health to
conduct the Vitamin D and Omega-3 Trial (VITAL)
(CA138962).
Role of the Funder/Sponsor: The funding source
had no role in the preparation, review, or approval
of the manuscript.
REFERENCES
1. LeFevre ML; US Preventive Services Task Force.
Screening for vitamin D deficiency in adults: US
1312
Primary End Points
Cancer, CVD
2. Greider K. Has vitamin D been oversold? AARP
Bulletin. July 5, 2012. http://www.aarp.org/health
/drugs-supplements/info-07-2012/how-much
-vitamin-d-is-enough.1.html. Accessed February 11,
2015.
3. Moyer VA; US Preventive Services Task Force.
Vitamin, mineral, and multivitamin supplements for
the primary prevention of cardiovascular disease
and cancer: US Preventive Services Task Force
recommendation statement. Ann Intern Med. 2014;
160(8):558-564.
4. Institute of Medicine. Dietary Reference Intakes
for Calcium and Vitamin D. Washington, DC: National
Academies Press; 2011.
5. Heaney RP, Armas LA. Screening for vitamin D
deficiency: is the goal disease prevention or full
nutrient repletion? Ann Intern Med. 2015;162(2):
144-145.
6. Manson JE, Bassuk SS, Lee I-M, et al. The
VITamin D and OmegA-3 TriaL (VITAL): rationale
and design of a large randomized controlled trial of
vitamin D and marine omega-3 fatty acid
supplements for the primary prevention of cancer
and cardiovascular disease. Contemp Clin Trials.
2012;33(1):159-171.
7. Bolland MJ, Grey A, Gamble GD, Reid IR. The
effect of vitamin D supplementation on skeletal,
vascular, or cancer outcomes: a trial sequential
meta-analysis. Lancet Diabetes Endocrinol. 2014;2
(4):307-320.
8. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al;
Endocrine Society. Evaluation, treatment, and
prevention of vitamin D deficiency: an Endocrine
Society clinical practice guideline. J Clin Endocrinol
Metab. 2011;96(7):1911-1930.
JAMA April 7, 2015 Volume 313, Number 13 (Reprinted)
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Thomas Jefferson University User on 05/13/2015
jama.com
You might also like
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Vitamin D Intake and Risk of Cardiovascular Disease in US Men and WomenDocument9 pagesVitamin D Intake and Risk of Cardiovascular Disease in US Men and WomenAgafioNo ratings yet
- Multidisciplinary Approach to the Management of ObesityFrom EverandMultidisciplinary Approach to the Management of ObesityNo ratings yet
- Editorial: Enough Is Enough: Stop Wasting Money On Vitamin and Mineral SupplementsDocument4 pagesEditorial: Enough Is Enough: Stop Wasting Money On Vitamin and Mineral SupplementsSixto Gutiérrez SaavedraNo ratings yet
- Dissertation Vitamin D 2015Document4 pagesDissertation Vitamin D 2015BuyResumePaperFortCollins100% (1)
- Vitamin D StudyDocument6 pagesVitamin D StudyDeenNo ratings yet
- What Vitamins Should I Be Taking, DoctorDocument6 pagesWhat Vitamins Should I Be Taking, DoctorDiego Bedón AscurraNo ratings yet
- Pubmed 18088161Document5 pagesPubmed 18088161DomenicaNo ratings yet
- Pi Is 0749379702005718Document9 pagesPi Is 0749379702005718audrey angelicaNo ratings yet
- Results in Relation To Other StudiesDocument3 pagesResults in Relation To Other StudiesBadseba TiweryNo ratings yet
- Vitamin D and Cancer: Uncertainty Persists Research ContinuesDocument2 pagesVitamin D and Cancer: Uncertainty Persists Research Continuesdear5643No ratings yet
- Article - (Design Vocab) The Miracle of Vitamin DDocument3 pagesArticle - (Design Vocab) The Miracle of Vitamin DAoun AlexNo ratings yet
- JNCI J Natl Cancer Inst 2008 Speers 1562 4Document3 pagesJNCI J Natl Cancer Inst 2008 Speers 1562 4Ramy Abo SamraNo ratings yet
- Vitaminsfinal HamrickCountsDocument43 pagesVitaminsfinal HamrickCountsĐặng Huy HoàngNo ratings yet
- VITAMINA D y Riesgo CardiovascularDocument12 pagesVITAMINA D y Riesgo CardiovascularAngusNo ratings yet
- Vitamin D For Postmenopausal WomenDocument2 pagesVitamin D For Postmenopausal Womensoos.edinaNo ratings yet
- Vitamin D Supplementation and Prevention of Type 2 Diabetes: Original ArticleDocument11 pagesVitamin D Supplementation and Prevention of Type 2 Diabetes: Original ArticleChristine BelindaNo ratings yet
- Cme DR PugudDocument4 pagesCme DR PugudBalqis AmatullahNo ratings yet
- Stoke NutritionDocument14 pagesStoke Nutritionapi-150223943No ratings yet
- Food and Vitamins and Supplements! Oh My!Document45 pagesFood and Vitamins and Supplements! Oh My!Ronald Rey GarciaNo ratings yet
- Vitamin D Insufficiency Linked To Asthma Severity: Medscape Medical NewsDocument6 pagesVitamin D Insufficiency Linked To Asthma Severity: Medscape Medical NewsMichal MajewskiNo ratings yet
- Suplementacion Con Vit DDocument31 pagesSuplementacion Con Vit Dyanet guzman aybarNo ratings yet
- Vitamin D in Health and Disease A Literature Review. Basit SDocument4 pagesVitamin D in Health and Disease A Literature Review. Basit SaflspyogfNo ratings yet
- Referencia 8. Pilz 2018Document19 pagesReferencia 8. Pilz 2018Erie RegaladoNo ratings yet
- Vitamin DDocument12 pagesVitamin DLia NadaNo ratings yet
- Vitamin D in Health and Disease A Literature Review PDFDocument8 pagesVitamin D in Health and Disease A Literature Review PDFafdtxmwjsNo ratings yet
- CA Próstata - Artigo - Overview of Dietary Supplements in Prostate CancerDocument6 pagesCA Próstata - Artigo - Overview of Dietary Supplements in Prostate CancerBeatriz GuimarãesNo ratings yet
- Accepted Manuscript: MaturitasDocument26 pagesAccepted Manuscript: MaturitasAlpha17 MedicsteenNo ratings yet
- Vegan Diet, Subnormal Vitamin B-12 Status and Cardiovascular Health - Woo 2012Document15 pagesVegan Diet, Subnormal Vitamin B-12 Status and Cardiovascular Health - Woo 2012acolpoNo ratings yet
- Vitamin D and Cardiovascular Disease: Time For Large Randomized TrialsDocument3 pagesVitamin D and Cardiovascular Disease: Time For Large Randomized TrialsOkky Winang SaktyawanNo ratings yet
- Research Paper Vitamin DDocument7 pagesResearch Paper Vitamin Dh00yfcc9100% (1)
- Dairy Intake Is Not Associated With Improvements.8Document8 pagesDairy Intake Is Not Associated With Improvements.8indiz emotionNo ratings yet
- Vitamin D Research PaperDocument7 pagesVitamin D Research Paperjsxmwytlg100% (1)
- Non-Cephalic Presentation in Late Pregnancy: EditorialsDocument2 pagesNon-Cephalic Presentation in Late Pregnancy: EditorialsNinosk Mendoza SolisNo ratings yet
- The Live Better Group Vitamins CancerDocument33 pagesThe Live Better Group Vitamins CancerGaura DasNo ratings yet
- Neurology 2011 SolomonDocument3 pagesNeurology 2011 SolomonHabib G. Moutran BarrosoNo ratings yet
- Research ArticleDocument5 pagesResearch ArticleiwanNo ratings yet
- Jama Jia 2022 Ed 220043 1655316061.73925Document2 pagesJama Jia 2022 Ed 220043 1655316061.73925Michaell GabrielNo ratings yet
- Vitamin D: An Evidence-Based ReviewDocument9 pagesVitamin D: An Evidence-Based ReviewWill TohallinoNo ratings yet
- ACS Guidelines PDFDocument38 pagesACS Guidelines PDFGabriel MateusNo ratings yet
- Essentials of Healthy Eating: A Guide: Journal of Midwifery and Women?s Health November 2010Document18 pagesEssentials of Healthy Eating: A Guide: Journal of Midwifery and Women?s Health November 2010Shathish JaiNo ratings yet
- Hutchinson 2010Document10 pagesHutchinson 2010pilarerasoNo ratings yet
- Vitamin D For Older People: How Much, For Whom And-Above All-Why?Document2 pagesVitamin D For Older People: How Much, For Whom And-Above All-Why?MohammedNo ratings yet
- Hypertension JournalDocument5 pagesHypertension JournalYola SurbaktiNo ratings yet
- 25-Hydroxyvitamin D Is Associated With Adiposity andDocument23 pages25-Hydroxyvitamin D Is Associated With Adiposity andRenata NunanNo ratings yet
- Dr. Rhonda Patrick - Rebuttal To 'Vitamins Are Bad'Document6 pagesDr. Rhonda Patrick - Rebuttal To 'Vitamins Are Bad'tylerdurdenmademe100% (1)
- D Inhealth and DiseaseDocument3 pagesD Inhealth and DiseaseSheila GouveiaNo ratings yet
- Vitamin D Supplementation Haines2012Document29 pagesVitamin D Supplementation Haines2012AmilaNo ratings yet
- Am J Clin Nutr 2007 85 289sDocument4 pagesAm J Clin Nutr 2007 85 289sthanosssNo ratings yet
- Hipovitaminoza DDocument29 pagesHipovitaminoza DekatarinaNo ratings yet
- Assignment 1 (ESAP)Document5 pagesAssignment 1 (ESAP)tharhanNo ratings yet
- J. Nutr.-2016-Salas-Salvadó-jn.115.218487Document9 pagesJ. Nutr.-2016-Salas-Salvadó-jn.115.218487chiclebluejmNo ratings yet
- CA Cancer J ClinDocument29 pagesCA Cancer J ClinanshunigamNo ratings yet
- Vitamina DDocument6 pagesVitamina DYuri YasuNo ratings yet
- 645 FullDocument8 pages645 FullCarrie Joy DecalanNo ratings yet
- SAMPLE: TERM PAPER (Prepared by ELC550 Students) Advantages and Disadvantages of Consuming Dietary SupplementsDocument4 pagesSAMPLE: TERM PAPER (Prepared by ELC550 Students) Advantages and Disadvantages of Consuming Dietary SupplementsSyafiqah ArinaNo ratings yet
- Lesson Plan 4 Powerpoint 4 2Document21 pagesLesson Plan 4 Powerpoint 4 2api-523266509100% (1)
- Biesalski Vitamin D RecommendationsDocument7 pagesBiesalski Vitamin D RecommendationsAleem MuhammadNo ratings yet
- 5 - Diabetes MellitusDocument9 pages5 - Diabetes MellitusNatnicha foongfaNo ratings yet
- Lipid Screen PedsDocument13 pagesLipid Screen PedsEnerolisa ParedesNo ratings yet
- Impact of Genetics On The Clinical Management of ChannelopathiesDocument12 pagesImpact of Genetics On The Clinical Management of ChannelopathiesRenan Lopez ViañaNo ratings yet
- UW ObjectivesDocument220 pagesUW ObjectivesRaymond Bernatowicz100% (2)
- Neurocysticercosis TtoDocument11 pagesNeurocysticercosis TtoRenan Lopez ViañaNo ratings yet
- Virus ZikaDocument76 pagesVirus ZikalgkarinaNo ratings yet
- AllisonDocument3 pagesAllisonKenneth RojoNo ratings yet
- Gprs/Umts: IAB Workshop February 29 - March 2, 2000 Jonne Soininen NokiaDocument34 pagesGprs/Umts: IAB Workshop February 29 - March 2, 2000 Jonne Soininen NokiaSajid HussainNo ratings yet
- Palladium Skill Book 1a.Document10 pagesPalladium Skill Book 1a.Randy DavisNo ratings yet
- Practice For Those Who Are DyingDocument10 pagesPractice For Those Who Are DyingBecze István / Stephen Becze100% (1)
- Good Governance and Social Responsibility-Module-1-Lesson-3Document11 pagesGood Governance and Social Responsibility-Module-1-Lesson-3Elyn PasuquinNo ratings yet
- VVP Engg. CollegeDocument32 pagesVVP Engg. Collegechotaimanav17No ratings yet
- Indian Retail Industry: Structure, Drivers of Growth, Key ChallengesDocument15 pagesIndian Retail Industry: Structure, Drivers of Growth, Key ChallengesDhiraj YuvrajNo ratings yet
- Assisted Reproductive Technology945Document35 pagesAssisted Reproductive Technology945Praluki HerliawanNo ratings yet
- Pratham Bhardwaj: Education SkillsDocument1 pagePratham Bhardwaj: Education SkillsashuNo ratings yet
- Prismatic Battery Pack Se-Mi Auto Production Line ProposalDocument25 pagesPrismatic Battery Pack Se-Mi Auto Production Line ProposalCheemaNo ratings yet
- The Municipality of Santa BarbaraDocument10 pagesThe Municipality of Santa BarbaraEmel Grace Majaducon TevesNo ratings yet
- Spelling Power Workbook PDFDocument98 pagesSpelling Power Workbook PDFTinajazz100% (1)
- BCMSN30SG Vol.2 PDFDocument394 pagesBCMSN30SG Vol.2 PDFShemariyahNo ratings yet
- Botswana Ref Ranges PaperDocument7 pagesBotswana Ref Ranges PaperMunyaradzi MangwendezaNo ratings yet
- VC++ Splitter Windows & DLLDocument41 pagesVC++ Splitter Windows & DLLsbalajisathyaNo ratings yet
- Liddell Hart PDFDocument5 pagesLiddell Hart PDFMohamed Elkhder100% (1)
- The City of GodDocument16 pagesThe City of GodJei Em MonteflorNo ratings yet
- LPP-Graphical and Simplex MethodDocument23 pagesLPP-Graphical and Simplex MethodTushar DhandeNo ratings yet
- Raiders of The Lost Ark - Indiana JonesDocument3 pagesRaiders of The Lost Ark - Indiana JonesRobert Jazzbob Wagner100% (1)
- 4 Thematic AnalysisDocument32 pages4 Thematic Analysisapi-591181595No ratings yet
- Excavations OSHA 2226Document44 pagesExcavations OSHA 2226Al DubNo ratings yet
- Assessment On The Efficiency of Technology Use in Teaching and Learning Process at Emilio Aguinaldo College Cavite. ResponsesDocument14 pagesAssessment On The Efficiency of Technology Use in Teaching and Learning Process at Emilio Aguinaldo College Cavite. ResponsesZAMORA REYMARNo ratings yet
- Business Research Chapter 1Document27 pagesBusiness Research Chapter 1Toto H. Ali100% (2)
- LEARNING MODULE Entrep Lesson 1-2Document19 pagesLEARNING MODULE Entrep Lesson 1-2Cindy BononoNo ratings yet
- Bank ATM Use CasesDocument12 pagesBank ATM Use Casessbr11No ratings yet
- Millwright Local Union 2158 PAC - 8048 - VSRDocument10 pagesMillwright Local Union 2158 PAC - 8048 - VSRZach EdwardsNo ratings yet
- Athletic KnitDocument31 pagesAthletic KnitNish A0% (1)
- Cargill VinodDocument98 pagesCargill Vinodsaurajindal09No ratings yet
- Holistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaDocument4 pagesHolistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaPriyesh Dubey100% (2)
- Full Download Test Bank For Amgov Long Story Short 1st Edition Christine Barbour PDF Full ChapterDocument13 pagesFull Download Test Bank For Amgov Long Story Short 1st Edition Christine Barbour PDF Full Chaptertithly.decamplh56c7100% (20)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (351)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (3)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- Molecules of Emotion: Why You Feel the Way You FeelFrom EverandMolecules of Emotion: Why You Feel the Way You FeelRating: 4 out of 5 stars4/5 (128)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- The Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesFrom EverandThe Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesNo ratings yet
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (81)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseFrom EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseRating: 4.5 out of 5 stars4.5/5 (84)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingFrom EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingRating: 5 out of 5 stars5/5 (61)