Professional Documents
Culture Documents
Whats New in Asthma and COPD
Uploaded by
sobanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Whats New in Asthma and COPD
Uploaded by
sobanCopyright:
Available Formats
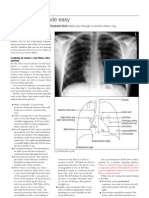
WHAT'S NEW IN ASTHMA AND COPD
Published with
Volume 31:8 2003
Whats new in ...
Asthma and COPD
Medicine
P M A Calverley and Paul Walker
Airways disease remains important in the workload of hospital
respiratory physicians, and the respiratory workload of family doctors.
Much research on asthma and chronic obstructive pulmonary disease
(COPD) involves basic pathophysiology, including genetics, but this
article deals with advances of importance to non-specialists, both now
and in the future.
Asthma
Guidelines and delivery of care many
patients with asthma experience frequent
symptoms with consequent limitation of
activity. Individuals with persistent symptoms often believe that their asthma is well
controlled and do not discuss these symptoms or the restrictions with health-care
professionals. Potential consequences of
poor control include fixed airway obstruction and high numbers of exacerbations and
hospital admissions. The Global Initiative
for Asthma guidelines, though not evidencebased, attempt to highlight what the aims
of asthma management should be; these
include minimal chronic symptoms, no
limitation of activity and minimal use of
rescue medication.1 The British Thoracic
Society/Scottish Intercollegiate Guidelines
Network asthma guidelines are evidencebased, and it is hoped that they will help to
address current shortcomings in management and delivery of care.2 An established
principle in these guidelines is that asthma
in adolescents ( 12 years) should be managed as in adults.
Provision of written self-management
plans after hospital admission can have
a beneficial effect on symptoms (day and
night) and reduce re-admission rates over
the next year. A fivefold reduction in readmission was seen in patients who were
given such plans on their first admission.3
Proactive structured review in primary
care is associated with up to a threefold
reduction in days on which normal activity is limited by the symptoms of asthma.4
The latest UK asthma guidelines based on
a systematic review of data recommend
that a nurse trained in asthma management
should regularly review patients managed
in primary care, and that self-management
education, including written action plans,
should be provided to all patients.
Pharmacological therapy significant
advances have been made in the treatment
of asthma, largely involving improvements
in existing therapies such as corticosteroids
and -agonists.
When to commence inhaled corticosteroids has been debated for many years.
The START study assessed this in 7241
patients with mild persistent asthma of
less than 2 years duration who had not
previously undergone regular inhaled
corticosteroid treatment.5 Compared with
placebo, budesonide, 400 g once daily for
3 years, reduced the incidence of severe
asthma exacerbations by 44%, and led to
a decrease in both the number of courses
of oral corticosteroids required and the
symptoms. The results indicate that lowdose inhaled corticosteroids should be
commenced even in patients with mild
asthma of recent onset.
In patients with poorly controlled
asthma who are taking low-dose inhaled
corticosteroids and rescue short-acting
-agonists, the next step should be the
P M A Calverley FRCP FRCP(Ed) is Professor of Medicine at the University of Liverpool, UK.
Paul Walker MRCP is Specialist Registrar in Respiratory Medicine at University Hospital Aintree,
Liverpool, UK.
MEDICINE
addition of a long-acting -agonist, regardless of the severity of the asthma. This was
established several years ago in patients
with moderate-to-severe asthma, and more
recently in those with mild asthma in the
OPTIMA study.6 In this study, 1272 patients
with mild asthma who were taking only a
low dose of inhaled corticosteroid were
randomized to either 100 g or 200 g of
budesonide twice per day and either 4.5 g
of formoterol twice per day or placebo.
Those on the higher dose of budesonide
alone gained only minor benefit, whereas
asthma control was significantly improved
in those taking formoterol with either dose
of budesonide. Addition of formoterol reduced the risk of a first asthma exacerbation by 43%, the number of poorly controlled asthma days by 30%, and the incidence of severe exacerbations by 52%.
Addition of a long-acting -agonist and
an increase in the inhaled corticosteroid
dose are both superior to other therapies
(e.g. leukotriene receptor antagonists,
theophylline), which can be considered
if control remains poor. Current evidence
supports the fact that combinations of
inhaled corticosteroids and long-acting
-agonists are at least as effective as their
individual components and may help
adherence to therapy.
New therapies inhaled corticosteroids
with a more favourable efficacy:toxicity
ratio and hence fewer systemic side-effects
have been developed. Ciclesonide has the
advantage of once-daily dosing. Mometasone is an inhaled corticosteroid that has
recently been launched in the UK for mildto-moderate asthma and can also be used
once per day for maintenance therapy.
Phosphodiesterase-4 inhibitors have a
broad anti-inflammatory effect and roflumilast is currently being assessed in clinical
trials, though data published in abstract
form have been disappointing.
Omalizumab is a blocking antibody
to IgE that has been investigated in 546
2003 The Medicine Publishing Company Ltd
WHAT'S NEW IN ASTHMA AND COPD
moderate-to-severe allergic asthmatics. A
reduction of more than 50% in asthma
exacerbations was achieved, despite a
reduction in the dose of inhaled corticosteroids.7 The drug also has positive effects
on lung function, asthma symptoms and
quality of life, and its benefits continue for
up to 1 year.8 However, because of its action
on IgE it is likely to be useful only in atopic
asthma, and its cost and subcutaneous
administration mean that it will probably
be given only to carefully selected patients
with moderate-to-severe asthma.
Corticosteroid side-effects corticosteroids remain the primary diseasemodifying therapy in asthma, and sideeffects are an important issue. Currently
available inhaled corticosteroids undergo
significant systemic absorption, and this
is associated with reduced bone mineral
density. Recent work has shown a small
but significant increase in the incidence
of hip fracture in recent users of inhaled
corticosteroids; this association appears to
be dose related and is reduced only slightly
by adjustment for oral corticosteroid use.9
There is also an association between oral
corticosteroid dose and vertebral fracture
in patients with chronic lung disease.10 It
is important to reduce the dose of inhaled
corticosteroid to the minimum possible,
and patients taking high-dose inhaled or
regular oral corticosteroids should be considered for prophylactic therapy to prevent
reduction of bone mineral density.
Acute exacerbations management
of acute exacerbations has remained unchanged for many years, based on highflow oxygen, nebulized and intravenous
bronchodilators and oral or intravenous
corticosteroids. Magnesium has long been
recognized as a bronchodilator, however,
and has now been shown to be an effective
adjunct to conventional therapy in both
adults and children with acute severe
asthma exacerbations.11 Currently, a single
intravenous dose is usually prescribed.
Debate remains about the role of increased inhaled corticosteroid dose during
exacerbations. Clear evidence on which to
make recommendations is lacking.
Disease monitoring asthma therapy
is assessed by symptoms, exacerbations
and measures of lung function. These
are important, but are distant surrogates
for processes in the airways. Research
on different means of guiding treatment
has shown positive benefits on outcome
measures.
MEDICINE
Bronchial challenge testing is a measure
of airway smooth muscle reactivity that has
been used for many years as a diagnostic
test for asthma. Use of 3-monthly bronchial challenge tests to guide therapy in
75 patients with mild-to-moderate asthma
led to a near halving of mild exacerbations
over 2 years.12 At the end of 2 years, bronchial biopsy showed histological improvement that correlated with the eosinophil
count in the biopsies. Alternatively, the
eosinophil count in induced sputum can
be used to guide treatment. This has been
compared with standard management in
74 moderate-to-severe asthmatics.13 In the
sputum management group, there was
a threefold reduction in severe asthma
exacerbations and fewer hospitalizations
despite no significant difference in oral or
inhaled corticosteroid dose. A large reduction in sputum eosinophil count was also
seen in the sputum management group.
Neither of these strategies is currently
applicable to general respiratory practice,
but they may be increasingly used in trials
of new therapies and may be helpful in
selected individuals.
COPD
Guidelines many national and international bodies produce guidelines for
the management of COPD. The Global
Initiative for Chronic Obstructive Lung
Disease (www.goldcopd.com) guidelines
are a recent addition.14 These are the first
evidence-based guidelines and are updated
every July. The aim is that they will remain
up to date and promote international consensus on management.
Smoking cessation following diagnosis of COPD, the foundation of treatment
is encouraging smoking cessation in those
who have yet to stop. Long-term studies
have shown that decline in lung function is
accelerated in individuals who continue to
smoke. Furthermore, in the general population, self-reported smoking cessation is
associated with an approximately 40%
reduction in the rate of hospitalization for
exacerbation of COPD later in life. There
was no reduction in those who smoked less
but did not quit.15
Physiological tests abnormal spirometry is a cardinal diagnostic feature of
COPD, but remains a poor predictor of
exercise performance and response to
therapy. The reason for this has now been
shown by the observation that, in COPD,
end-expiratory lung volume increases
during exercise (dynamic hyperinflation),
rather than decreasing as in normal subjects. This explains the intensity of dyspnoea, at least in more severe disease, and
is associated with limitation of expiratory
airflow during tidal breathing, which can
be measured by applying negative pressure
during expiration (NEP). Although NEP is
little affected by bronchodilators at rest,16
the decrease in dynamic hyperinflation
after administration of a bronchodilator
is a better predictor of change in exercise
performance than is the change in forced
expiratory volume in 1 second (FEV1).17
Pulmonary rehabilitation out-patient
pulmonary rehabilitation is important in
the management of COPD. There is clear
evidence that it leads to improvements in
breathlessness, physical functioning, quality of life and hospitalizations. The benefits
last for at least 1 year, but then appear to
decline. Results of studies of maintenance
programmes have been disappointing.
A 1-year study of 85 COPD patients
involving the addition of monthly rehabilitation follow-up sessions to periodic
encouragement showed no benefit from
additional sessions, and less than onehalf of the subjects remained in the active
treatment arm by the end of the study.18
Another, larger study involved 172 patients
randomized to either weekly telephone
follow-up plus monthly rehabilitation sessions for 12 months, or standard care. In
the intervention group, improvements in
exercise capacity and health status were
better maintained over the first year, but
there was no difference in symptoms or
quality of life. After 2 years, there were
no differences between the groups and
patients had returned to levels close to
those before rehabilitation.19
Major barriers to continuing exercise
appear to be frequent exacerbations, and
problems with exercising during exacerbations or restarting exercise afterwards.
Whether rehabilitation can be enhanced by
nutritional supplementation or pharmacological intervention (e.g. growth hormone,
anabolic steroids) is unclear. Despite the
benefits, many UK hospitals UK do not provide a pulmonary rehabilitation service.
Lung volume reduction surgery there
has been much interest in lung volume
reduction surgery in COPD; however,
surgery is appropriate only in selected
patients. The National Emphysema Treatment Trial was established to determine
2003 The Medicine Publishing Company Ltd
WHAT'S NEW IN ASTHMA AND COPD
those likely to benefit. An early analysis
showed unacceptably high mortality in
patients with FEV1 less than 20% predicted and either a homogenous pattern
of emphysema on CT (no clearly severely
affected area to remove) or DLCO less
than 20% predicted.20 Full results were
published recently; patients lacking predominant upper lobe emphysema and with
good exercise capacity after pulmonary
rehabilitation exhibited excess mortality
with little long-term functional or quality
of life improvement. The patients most
likely to benefit are those with upper lobe
disease and poor exercise capacity after
rehabilitation.21
A promising new area of research is
bronchoscopic lung volume reduction surgery, which may be suitable for those who
are unsuitable for or refuse the operative
procedure.22 An early report of the insertion
of endobronchial valves in eight patients
has suggested that the procedure is safe
in the short term and can improve lung
function. However, much work is required
before the procedure can be deemed safe
or useful for a wider patient group.
Pharmacological therapy recent
evidence supports the use of combination
long-acting -agonist/inhaled corticosteroid inhalers. The TRISTAN study recruited
1465 patients with widely ranging severities
of COPD and random-ized them to a fluticasone/salmeterol combination (Seretide),
the individual components or placebo.23
The combin-ation therapy produced superior improvements in lung function and
a clinically significant improvement in
health status, with the greatest improvement in daily symptoms. Another study
of 812 subjects with moderate-to-severe
COPD compared a budesonide/formoterol
combination (Symbicort) with its components and placebo.24 The combination
treatment reduced the mean number of
severe exacerbations and improved lung
function compared with other treatment
arms, and produced the greatest decrease
in symptom scores.
The phosphodiesterase inhibitors
cilomilast and roflumilast are antiinflammatory agents with modest benefits
in clinical trials.25 They are currently not
licensed in the UK.
Exacerbations exacerbations are more
common in patients with worse baseline
lung function, and recovery takes longer
and is less likely to be complete. Quality
of life is worse and decline in lung func-
MEDICINE
tion more rapid in individuals who suffer
frequent exacerbations.26 Patients with
COPD not uncommonly harbour colonizing bacteria in their airways, and these
individuals suffer more frequent exacerbations, more airway inflammation and more
rapid disease progression.27 Colonization
with Haemophilus influenzae appears to be
particularly important.28 Timely treatment
of infective exacerbations is appropriate,
but there is currently no evidence to support a more aggressive policy of eradication
of bacteria. Small areas of bronchiectesis
are often seen on high-resolution CT in
patients with COPD, but the importance
of these is unclear.u
13
14
15
16
17
REFERENCES
Global Initiative for Asthma: Global Strategy for
Asthma Management and Prevention
Updated April 2002. Scientific Information and
Recommendations for Asthma Programs. NIH
Publication No. 023659.
2 British Thoracic Society, Scottish Intercollegiate
Guidelines Network. British Guideline on the
Management of Asthma. Thorax 2003; 58:
(Suppl. 1): i194.
3 Thoonen B P et al. Self-management of Asthma in
General Practice, Asthma Control and Quality of
Life: A Randomised Controlled Trial. Thorax 2003;
58: 306.
4 Osman L M et al. A Randomised Trial of
Self-management Planning for Adult Patients
Admitted to Hospital with Acute Asthma. Thorax
2002; 57: 86974.
5 Pauwels R A et al. Early Intervention with
Budesonide in Mild Persistent Asthma:
A Randomised, Double-blind Trial. Lancet 2003;
361: 10716.
6 OByrne P M et al. Low Dose Inhaled Budesonide
and Formoterol in Mild Persistent Asthma:
The OPTIMA Randomized Trial. Am J Respir Crit
Care Med 2001; 164: 13927.
7 Soler M et al. The Anti-IgE Antibody Omalizumab
Reduces Exacerbations and Steroid Requirement
in Allergic Asthmatics. Eur Respir J 2001; 18(2):
25461.
8 Buhl R et al. Omalizumab Provides Long-term
Control in Patients with Moderate-to-severe
Asthma. Eur Respir J 2002; 20: 738.
9 Hubbard R B et al. Inhaled Corticosteroids and
Hip Fracture: A Population-based Case-control
Study. Am J Respir Crit Care Med 2002; 166:
15636.
10 Walsh L J et al. The Impact of Oral Corticosteroid
Use on Bone Mineral Density and Vertebral
Fracture. Am J Respir Crit Care Med 2002; 166:
6915.
11 Silverman R A et al. IV Magnesium Sulfate in the
Treatment of Acute Severe Asthma: A Multicenter
Randomized Controlled Trial. Chest 2002; 122:
48997.
12 Sont J K et al. Clinical Control and Histopathologic
Outcome of Asthma when using Airway
Hyperresponsiveness as an Additional Guide to
1
18
19
20
21
22
23
24
25
26
27
28
Long-term Treatment. The AMPUL Study Group.
Am J Respir Crit Care Med 1999; 159: 104351.
Green R H et al. Asthma Exacerbations and
Sputum Eosinophil Counts: A Randomised
Controlled Trial. Lancet 2002; 360: 171521.
Pauwels R A et al. Global Strategy for the
Diagnosis, Management, and Prevention of
Chronic Obstructive Pulmonary Disease. NHLBI/
WHO Global Initiative for Chronic Obstructive
Lung Disease (GOLD) Workshop Summary. Am J
Respir Crit Care Med 2001; 163: 125676.
Godtfredsen N S et al. Risk of Hospital Admission
for COPD following Smoking Cessation and
Reduction: A Danish Population Study. Thorax
2002; 57: 96772.
Hadcroft J, Calverley P M. Alternative Methods for
Assessing Bronchodilator Reversibility in Chronic
Obstructive Pulmonary Disease. Thorax 2001; 56:
71320.
ODonnell D E et al. Spirometric Correlates of
Improvement in Exercise Performance after
Anticholinergic Therapy in Chronic Obstructive
Pulmonary Disease. Am J Respir Crit Care Med
1999; 160: 5429.
Brooks D et al. The Effect of Postrehabilitation
Programmes among Individuals with Chronic
Obstructive Pulmonary Disease. Eur Respir J
2002; 20: 209.
Ries A L et al. Maintenance after Pulmonary
Rehabilitation in Chronic Lung Disease:
A Randomized Trial. Am J Respir Crit Care Med
2003; 167: 8808.
National Emphysema Treatment Trial Research
Group. Patients at High Risk of Death after
Lung-volume-reduction Surgery. N Engl J Med
2001; 345: 107583.
Fishman A et al. A Randomized Trial Comparing
Lung-volume-Reduction Surgery with Medical
Therapy for Severe Emphysema. N Engl J Med
2003; 348: 205973.
Toma T P et al. Bronchoscopic Volume Reduction
with Valve Implants in Patients with Severe
Emphysema. Lancet 2003; 361: 9313.
Calverley P et al. Combined Salmeterol and
Fluticasone in the Treatment of Chronic
Obstructive Pulmonary Disease: A Randomised
Controlled Trial. Lancet 2003; 361: 44956.
Szafranski W et al. Efficacy and Safety of
Budesonide/formoterol in the Management of
Chronic Obstructive Pulmonary Disease. Eur
Respir J 2003; 21: 7481.
Compton C H et al. Cilomilast, a Selective
Phosphodiesterase-4 Inhibitor for Treatment of
Patients with Chronic Obstructive Pulmonary
Disease: A Randomised, Dose-ranging Study.
Lancet 2001; 358: 26570.
Donaldson G C et al. Relationship between
Exacerbation Frequency and Lung Function
Decline in Chronic Obstructive Pulmonary
Disease. Thorax 2002; 57: 84752
Wilkinson T M et al. Airway Bacterial Load and
FEV1 Decline in Patients with Chronic Obstructive
Pulmonary Disease. Am J Respir Crit Care Med
2003; 167: 10905.
Patel I S et al. Relationship between Bacterial
Colonisation and the Frequency, Character, and
Severity of COPD Exacerbations. Thorax 2002; 57:
75964.
2003 The Medicine Publishing Company Ltd
You might also like
- UWorld Notes Step 2 CKDocument11 pagesUWorld Notes Step 2 CKSamah Khan50% (2)
- Rome III Diagnostic Criteria FGIDsDocument14 pagesRome III Diagnostic Criteria FGIDsPutu Reza Sandhya PratamaNo ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyChrischia Yvonne GualbertoNo ratings yet
- The McKenzie MethodDocument72 pagesThe McKenzie MethodDr-Gehad Samy Halwagy100% (3)
- Princess Arianne Macaranas Seven Hello Rache PracticeDocument2 pagesPrincess Arianne Macaranas Seven Hello Rache PracticeDianne MacaranasNo ratings yet
- Mbdqor345235235 PDFDocument482 pagesMbdqor345235235 PDFM HaidarNo ratings yet
- PQCNC AIM RPC LS2 Volunteer Doula ProgramDocument23 pagesPQCNC AIM RPC LS2 Volunteer Doula ProgramkcochranNo ratings yet
- Gas GangreneDocument21 pagesGas GangreneSyaIra SamatNo ratings yet
- Liver Biopsy and AbdominalDocument25 pagesLiver Biopsy and AbdominalAfiq Mubasyyir AmranNo ratings yet
- Mksap PulmonaryDocument77 pagesMksap PulmonaryAna Roman100% (4)
- COPD Updated Guidelines and Newer TherapiesDocument90 pagesCOPD Updated Guidelines and Newer TherapiesVlad Constantin100% (1)
- Chapter 01 Introduction To Nursing PDFDocument7 pagesChapter 01 Introduction To Nursing PDFludwigs43100% (1)
- Ocluzie Intestinala Prin Stenoza Extrinseca de Colon TransversDocument8 pagesOcluzie Intestinala Prin Stenoza Extrinseca de Colon TransversClaudia DanielaNo ratings yet
- Medications For Chronic Obstructive Pulmonary Disease: 1) BronchodilatorsDocument5 pagesMedications For Chronic Obstructive Pulmonary Disease: 1) BronchodilatorsMOHAMMAD NAZMUL ISLAMNo ratings yet
- What's New in Respiratory DisordersDocument4 pagesWhat's New in Respiratory DisorderssobanNo ratings yet
- Inhaler MedicationsDocument11 pagesInhaler MedicationsNayzstNo ratings yet
- Abr10742 FMDocument4 pagesAbr10742 FMeraNo ratings yet
- Managing Acute COPD ExacerbationsDocument3 pagesManaging Acute COPD ExacerbationsCalca NeusNo ratings yet
- Hunter TherapeuticstableDocument17 pagesHunter Therapeuticstableapi-273656298No ratings yet
- Reviews: The Role of Long-Acting Bronchodilators in The Management of Stable COPDDocument11 pagesReviews: The Role of Long-Acting Bronchodilators in The Management of Stable COPDSatriani JeeNo ratings yet
- 1302 FullDocument9 pages1302 FullSupicha VichaiditNo ratings yet
- COPD Case Study GuideDocument5 pagesCOPD Case Study GuideMohammad KhalaylahNo ratings yet
- ??????? ??????????? ????????? ???????Document3 pages??????? ??????????? ????????? ???????Hạnh VũNo ratings yet
- Prescriber - 2019 - Chaplin - COPD Update and New Guidance On Antibiotics For ExacerbationsDocument4 pagesPrescriber - 2019 - Chaplin - COPD Update and New Guidance On Antibiotics For ExacerbationsWireifnitedNo ratings yet
- 136 Full CopdDocument7 pages136 Full CopdAnty FftNo ratings yet
- COPD Treatment Options for Refractory SymptomsDocument6 pagesCOPD Treatment Options for Refractory SymptomsAnonymous ZUaUz1wwNo ratings yet
- Non Farmako Mulhall ReviewDocument19 pagesNon Farmako Mulhall Reviewgita cahayaNo ratings yet
- COPD Case Study Assessment and Care PlanDocument7 pagesCOPD Case Study Assessment and Care PlanMohammad KhalaylahNo ratings yet
- Chapter - 031.bridge To NCLEX Review Question AnswersDocument7 pagesChapter - 031.bridge To NCLEX Review Question AnswersJackie JuddNo ratings yet
- Jaa 4 001 PDFDocument12 pagesJaa 4 001 PDFRulianti BarantiNo ratings yet
- Corticoides Inhalados EpocDocument8 pagesCorticoides Inhalados EpocJohn MaynhamNo ratings yet
- BPOC in Medicina PrimaraDocument3 pagesBPOC in Medicina PrimaraAlina GheNo ratings yet
- Assessment and Management of Asthma and Chronic Obstructive Pulmonory Disease (Copd) - Converging ApproachesDocument6 pagesAssessment and Management of Asthma and Chronic Obstructive Pulmonory Disease (Copd) - Converging ApproachesmominamalikNo ratings yet
- Introduction To RefferenceDocument46 pagesIntroduction To RefferencebensonNo ratings yet
- Avances en Terapia de Rehabilitacion CardiopulmonarDocument13 pagesAvances en Terapia de Rehabilitacion CardiopulmonarMaría Camila Zuluaga AriasNo ratings yet
- EditDocument10 pagesEditParamitha HarmanNo ratings yet
- Jurnal Respirasi PDFDocument14 pagesJurnal Respirasi PDFakhirul_733759154No ratings yet
- AECOPD GuidelineDocument8 pagesAECOPD GuidelineRonlie RonneyNo ratings yet
- COPD Pulmonary Rehabilitation BenefitsDocument2 pagesCOPD Pulmonary Rehabilitation BenefitsMaura-Gabriela FeleaNo ratings yet
- Newer Therapies in COPD: Prem Parkash GuptaDocument6 pagesNewer Therapies in COPD: Prem Parkash GuptaKarthik TNo ratings yet
- Inhalasi Adrenergik AgonisDocument3 pagesInhalasi Adrenergik AgonisF MNo ratings yet
- Symptomatic Treatment of Cough Among Adult Patients With Lung Cancer CHEST Guideline and Expert Panel ReportDocument14 pagesSymptomatic Treatment of Cough Among Adult Patients With Lung Cancer CHEST Guideline and Expert Panel ReportThaísa NogueiraNo ratings yet
- COPD TX MNGDocument3 pagesCOPD TX MNGHydie Mae AlcabedosNo ratings yet
- Current COPD Treatments Compared: Bronchodilators, Corticosteroids, AntibioticsDocument5 pagesCurrent COPD Treatments Compared: Bronchodilators, Corticosteroids, Antibioticssmashraf2100% (1)
- New Treatments For Severe Treatment-Resistant Asthma - Lancet Resp Med 2013Document14 pagesNew Treatments For Severe Treatment-Resistant Asthma - Lancet Resp Med 2013Azan Al RasyidNo ratings yet
- Rational Prescribing For Ongoing Management of Asthma in AdultsDocument4 pagesRational Prescribing For Ongoing Management of Asthma in AdultsbangpatuiNo ratings yet
- Cystic Fibrosis Advances in The Management of Cystic FibrosisDocument19 pagesCystic Fibrosis Advances in The Management of Cystic FibrosisMehtab AlamNo ratings yet
- COPD Case Study: Improving Outcomes Through Evidence-Based Nursing CareDocument15 pagesCOPD Case Study: Improving Outcomes Through Evidence-Based Nursing CareSudeep BhandariNo ratings yet
- Azithromycin For The Prevention of COPD ExacerbationsDocument6 pagesAzithromycin For The Prevention of COPD ExacerbationsI Made AryanaNo ratings yet
- Approach Considerations: Respiratory Acidosis Treatment & ManagementDocument8 pagesApproach Considerations: Respiratory Acidosis Treatment & Managementprince1500No ratings yet
- CAM Therapies For Symptoms Management of Asthma and COPDDocument14 pagesCAM Therapies For Symptoms Management of Asthma and COPDCharlyn MoellersNo ratings yet
- The Clinical Case For Smoking Cessation For RESPIRATORY PATIENTSDocument4 pagesThe Clinical Case For Smoking Cessation For RESPIRATORY PATIENTSDianaAryantiNo ratings yet
- The Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Document4 pagesThe Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Agencia FaroNo ratings yet
- Asthma and COPD in The Emergency Department: Sa'ad Lahri RegistrarDocument31 pagesAsthma and COPD in The Emergency Department: Sa'ad Lahri RegistrarshashwathhNo ratings yet
- ArticleDocument12 pagesArticleRia DeviNo ratings yet
- 1° Artículo de EpocDocument8 pages1° Artículo de EpocNoelia ZavalaNo ratings yet
- Bronchodilator Beta2 AgonistDocument3 pagesBronchodilator Beta2 AgonistNararto PrijogoNo ratings yet
- Emphysema Guidelines - Guidelines Summary, Management of Acute Exacerbations of COPD, Pulmonary RehabilitationDocument6 pagesEmphysema Guidelines - Guidelines Summary, Management of Acute Exacerbations of COPD, Pulmonary Rehabilitationanusha bNo ratings yet
- Effect of Acbt & Postural Tapping On Fev1 &Fev1/Fvc in Moderate To Severe Copd PatientDocument6 pagesEffect of Acbt & Postural Tapping On Fev1 &Fev1/Fvc in Moderate To Severe Copd PatientManasvi MathurNo ratings yet
- COPD X Australian Guidelines For The Diagnosis and Management of Chronic Obstructive Pulmonary Disease - 2022 Update (MJA 2022)Document9 pagesCOPD X Australian Guidelines For The Diagnosis and Management of Chronic Obstructive Pulmonary Disease - 2022 Update (MJA 2022)Chih-I LeeNo ratings yet
- AsmathDocument6 pagesAsmathRido SaputraNo ratings yet
- Mukolitici U HOBPDocument3 pagesMukolitici U HOBPDejan ŽujovićNo ratings yet
- CTS COPD RX 2019 Guideline - FinalDocument24 pagesCTS COPD RX 2019 Guideline - FinalSharan SahotaNo ratings yet
- Stable COPD - Initial Pharmacologic Management - UpToDateDocument32 pagesStable COPD - Initial Pharmacologic Management - UpToDateLiz CampoverdeNo ratings yet
- Jurnal RhinosinusitisDocument26 pagesJurnal RhinosinusitisFarah F SifakNo ratings yet
- Cost-Utility Analysis of A Pharmacy-Led Self-Management Programme For Patients With COPDDocument10 pagesCost-Utility Analysis of A Pharmacy-Led Self-Management Programme For Patients With COPDoktarina puspitasariNo ratings yet
- Answer For McqsDocument3 pagesAnswer For Mcqseducare academy0% (1)
- Gold Copd 2017Document4 pagesGold Copd 2017ChrisNo ratings yet
- Asthma and COPD by AkkoDocument17 pagesAsthma and COPD by AkkoAvoy GhoshNo ratings yet
- Palliative CareDocument4 pagesPalliative CaresobanNo ratings yet
- Gastroenterology and AnaemiaDocument5 pagesGastroenterology and Anaemiasoban100% (1)
- The Immunocompromised Patient Primary ImmunodeficienciesDocument2 pagesThe Immunocompromised Patient Primary ImmunodeficienciessobanNo ratings yet
- Antiphospholipid SyndromeDocument4 pagesAntiphospholipid SyndromesobanNo ratings yet
- Antineoplastic SDocument20 pagesAntineoplastic SsobanNo ratings yet
- Urinary Tract ObstructionDocument3 pagesUrinary Tract ObstructionsobanNo ratings yet
- Acr Omega LyDocument3 pagesAcr Omega LysobanNo ratings yet
- The Wheezing InfantDocument4 pagesThe Wheezing InfantsobanNo ratings yet
- Adolescent NutritionDocument1 pageAdolescent NutritionsobanNo ratings yet
- Malnutrition and InfectionDocument3 pagesMalnutrition and InfectionsobanNo ratings yet
- Analgesic & AntimigraineDocument12 pagesAnalgesic & AntimigraineChin ChanNo ratings yet
- Autonomic & NeuromuscularDocument20 pagesAutonomic & Neuromuscularzeina32No ratings yet
- Vulval PainDocument3 pagesVulval PainsobanNo ratings yet
- Medicolegal Issues and STIsDocument3 pagesMedicolegal Issues and STIssobanNo ratings yet
- Drugs That Damage The LiverDocument5 pagesDrugs That Damage The LiversobanNo ratings yet
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- Case Scenarios Nutrition Growth and DevelopmentDocument4 pagesCase Scenarios Nutrition Growth and DevelopmentsobanNo ratings yet
- Contraception: What's New in ..Document4 pagesContraception: What's New in ..sobanNo ratings yet
- Non Epileptic Causes of Loss of ConsciousnessDocument3 pagesNon Epileptic Causes of Loss of ConsciousnesssobanNo ratings yet
- AppendixC NutrientChartDocument5 pagesAppendixC NutrientChartArianne Nicole LabitoriaNo ratings yet
- The Management of Acute Renal FailureDocument4 pagesThe Management of Acute Renal Failuresoban100% (1)
- Disorders of PubertyDocument2 pagesDisorders of PubertysobanNo ratings yet
- Haemo Chroma To SisDocument4 pagesHaemo Chroma To SissobanNo ratings yet
- What Is DiabetesDocument2 pagesWhat Is DiabetessobanNo ratings yet
- Neuro DegenerativeDocument11 pagesNeuro DegenerativesobanNo ratings yet
- Renal Disease and PregnancyDocument4 pagesRenal Disease and PregnancysobanNo ratings yet
- Neuro DegenerativeDocument11 pagesNeuro DegenerativesobanNo ratings yet
- NCM 112 Guide to Caring for Patients with CancerDocument15 pagesNCM 112 Guide to Caring for Patients with CancerShiena Mae PelagioNo ratings yet
- Apollo Munich Health-Wallet-Brochure - NEW - 8x8 PDFDocument9 pagesApollo Munich Health-Wallet-Brochure - NEW - 8x8 PDFRajat GuptaNo ratings yet
- Dka Vs Hhs Edit 1Document25 pagesDka Vs Hhs Edit 1Razeen RiyasatNo ratings yet
- Developmental Disorders and Gifted ChildrenDocument2 pagesDevelopmental Disorders and Gifted ChildrenRiza Pepito - Leachon100% (1)
- ACOG The RH Factor How It Can Affect Your Pregnancy PDFDocument3 pagesACOG The RH Factor How It Can Affect Your Pregnancy PDFdoc moNo ratings yet
- Stab WoundsDocument57 pagesStab WoundsMushtaq AhmadNo ratings yet
- Priyadarshini, 2010Document9 pagesPriyadarshini, 2010AmandaNo ratings yet
- CPR Ratio For Adults, Children, and InfantsDocument14 pagesCPR Ratio For Adults, Children, and InfantsAnonymous FCOOcnNo ratings yet
- Lecture 1 - Chapter 1 - Introduction To First AidDocument18 pagesLecture 1 - Chapter 1 - Introduction To First AidCatherine Tagorda TiñaNo ratings yet
- End of Service Incubator 5400Document1 pageEnd of Service Incubator 5400Faizal FlNo ratings yet
- Original Articles_ Comparison of Urinary Albumin-Creatinine Ratio and Albumin Excretion Rate in the Diabetes Control and Complications Trial_Epidemiology of Diabetes Interventions and Complications StudyDocument16 pagesOriginal Articles_ Comparison of Urinary Albumin-Creatinine Ratio and Albumin Excretion Rate in the Diabetes Control and Complications Trial_Epidemiology of Diabetes Interventions and Complications StudyM Dwi SuprayogiNo ratings yet
- Depression, lung function, and BODE index in COPDDocument16 pagesDepression, lung function, and BODE index in COPDHera HeraNo ratings yet
- KMU Prospectus 2012 Excellence in Academics & ResearchDocument101 pagesKMU Prospectus 2012 Excellence in Academics & ResearchAkas RehmanNo ratings yet
- Effectiveness_of_Hydrotherapy_ (1)Document18 pagesEffectiveness_of_Hydrotherapy_ (1)dandiokasubantaraNo ratings yet
- Sickle Cell Case StudyDocument3 pagesSickle Cell Case StudyIsaac KipkemoiNo ratings yet
- Case Report "Febrile Seizures": Betsheba E. S. 123307018Document37 pagesCase Report "Febrile Seizures": Betsheba E. S. 123307018AmandaRizkaNo ratings yet
- 2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPDocument22 pages2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPorangenarwhalNo ratings yet
- PUGSOM Graduate-Entry Medical Curriculum 4-Year Schematic - Cohort 2022Document1 pagePUGSOM Graduate-Entry Medical Curriculum 4-Year Schematic - Cohort 2022Alvin YeeNo ratings yet
- Pediatric Pain Assessment in TDocument6 pagesPediatric Pain Assessment in TnurtiNo ratings yet
- Developmental Dysplasia of The HipDocument42 pagesDevelopmental Dysplasia of The HipVITHAAH PARAMESWARANNo ratings yet
- Documents - MX Fiziopatologia Termoreglarii Fiziopatologia Termoreglarii Hipotermia Hipertermia Reactia Febrila 10-12-2006Document42 pagesDocuments - MX Fiziopatologia Termoreglarii Fiziopatologia Termoreglarii Hipotermia Hipertermia Reactia Febrila 10-12-2006AndreiNo ratings yet