Professional Documents
Culture Documents
Endodontic 199 144
Uploaded by
Amee PatelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endodontic 199 144
Uploaded by
Amee PatelCopyright:
Available Formats
The Rationale for Endodontic Therapy
Lisa Germain, DDS, MScD
Why it works
My husband is an attorney, the corporate kind, not the slip and fall kind. He doesnt go to
court, and has never sued anyone. He interprets fine print all day long. His world is very
different from mine as an endodontist. While he patiently listens to me jibber jabber about
the marvelous cutting efficiency of the latest rotary file, the number of pixels in the newest
imaging system, anecdotes about nutty patients and the fact that I did not have time today
topowder my nose, I can see that he is baffled. Baffled somewhat by my enthusiasm
after all these years, but more so by the dogma that drives my beliefs about endodontics,
which clearly leaves no room for interpretation.
Lately, I hear rumblings from dentists who
profess that root canal therapy does not
work. Over the years, I have educated and
treated literally, thousands of patients who
have sought my expertise to help them retain
their natural teeth. So this shift in thinking
that endodontically treated teeth are
doomed from the start has me asking, Has
Endodontics become disconnected from the
other practice areas of dentistry? Could it
possibly be true that all the teeth that I have
treated endodontically will eventually be
replaced with implants?
The answer to these questions of course
is no. I can say with total conviction that
while death and taxes are certain, so is
root canal therapy. Endodontics is alive
and well. It is predictable, and has a very
high rate of success.1 And, while much
of our technology has changed in the
field of endodontics, the Rationale for
Endodontic Therapy remains constant
and will always resonate for me in the
same way that it did the first time I
heard it from my mentor, Dr. Herbert
Schilder. So here goes:
Has Endodontics become disconnected
from the other practice areas of dentistry?
Inside every tooth there is a piece of soft
tissue, which is susceptible to necrosis,
gangrene, and death. This pulp tissue dies
for three reasons: 2,3
1. The tissue has a very small blood supply
making it very difficult to regenerate
on its own once it is injured.
2. It lies inside the unyielding walls of
dentin and therefore when it becomes
inflamed does not have room to swell.
virtually never just a single tube. Hence a
root canal system is a complex anatomical
space within the root of the tooth. Most
main canals terminate in the PDL at an exit
point close to the end of the root. However,
because of the lateral branches inherent in
root systems, it is not unusual for a root
canal system to have more than one exit
point. These portals of exit (POE) can occur
anywhere along the cementum of the periradicular anatomy, but are quite common in
the apical one third. 2,3,4
3. It is a terminal circulation, like the
appendix, which once diseased, needs
to be removed.
The most common cause of nerve pathology
that leads to pulp necrosis is caries, with
trauma being the second most common. Add
to that parafunction, plus the inflammation
that is created from dental procedures alone,
and it is amazing that any pulps actually
remain vital and asymptomatic. Fortunately,
many do but the higher the frequency as well
as the greater the duration and magnitude
of the injury or insult to the tooth, the
more likely the pulp will succumb to an
irreversible, pathological change ranging
from inflammation with pain to an abscess
with swelling. 2,3
Any given roots canals (not a typo) are
comprised of a system of channels and are
Endodontics
is alive and well.
Figure 1: Micro CT image of an extracted lower
premolar illustrating accessory canals and multiple
portals of exit. Scan by Marco Versiani DDS, MS, PhD
When the pulp begins to break down, the
bacterial by-products of cellular necrosis
egress from within the root canal system
through the POEs into the surrounding
PDL and bone. These toxins in turn will
destroy the healthy peri-radicular tissues and
create bone loss, which in endo-speak is
called a LEO (lesion of endodontic origin).
Because a LEO arises secondary to tissue
breakdown within the root canal system, the
tooth is the source of the disease. The disease
however is manifested in the bone.
Doing the most
expedient thing is not
necessarily the same as
doing the right thing.
So to get to the actual root of the problem (pun intended), the pulp and its
diseased remnants must be removed since they are the source of the problem
in the bone. The leaking root canal system must be eliminated. Extraction
is certainly one way to accomplish this, and once the tooth is gone the clear
evidence of healing is bone regeneration. But, if you have a hang nail, would
you cut your finger off? Doing the most expedient thing is not necessarily the
same as doing the right thing. A rule of thumb (pun intended) would be to ask
yourself what you would do if it were your own tooth. Honoring the answer to
that question helps me sleep at night.
If the tooth is restorable, if the periodontal condition is stable or can be made
so, and if the root is intact, I would chose the root canal every time. It is more
conservative, and less traumatic to the patient both physically and mentally. Yes,
a root canal system must be shaped, cleaned and sterilized properly. And, the
tooth structure must be maintained by using conservative preparation methods.6
But when all goes well, and it should, the POEs can be sealed extraordinarily
well. Then sit back and watch those LEOs heal (Figure 2). Problem solved.
pre-op
post-op
2 year follow-up
Figure 2: Digital image illustrating the results of
root canal therapy on tooth #19, with peri-radicular
healing of the bone around several POEs.
Lisa Germain is pictured with her daughter.
Lisa Germain, DDS, MScD., graduated from Boston University School of Graduate Dentistry with
a Masters of Science Degree in Endodontics in 1981. She is a Diplomate of the American Board of
Endodontics, a Fellow of the International Congress of Oral Implantologists, and a senior faculty
member of The American Academy of Facial Esthetics. Dr. Germain maintains a full time private
practice in New Orleans, LA. specializing in Endodontics, Implantology and Facial Pain Management.
References:
1. Rotstein I., Salehrabi R. (December 2004), Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study, JOE:12 (30): 84650
2. Schilder H. Lecture notes. 1979 Boston University Goldman School of Dental Medicine. Boston, Mass.
3. Schilder H. Cleaning and shaping the root canalDentClin NorthAm. 1974; 18: 269-296.
4. Buchanan LS. Everythings changed except the anatomy,Dent Today 2012; 16:36; 100-104.
5. Yu D. Radiographic location of accessory canals. PrivateDentistry, February 2006:36-43.
6. Clark D, Khademi JA. Case studies in modern molar endodontic access and directed dentin conservationDentClin NorthAm. 2010:54:275-289
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Dentinal Defects Before and After Rotary Root Canal Instrumentation With Three Different Obturation Techniques and Two Obturating MaterialsDocument5 pagesDentinal Defects Before and After Rotary Root Canal Instrumentation With Three Different Obturation Techniques and Two Obturating MaterialsAmee PatelNo ratings yet
- The Ability of Different Nickel-Titanium Rotary Instruments To Induce Dentinal Damage During Canal PreparationDocument3 pagesThe Ability of Different Nickel-Titanium Rotary Instruments To Induce Dentinal Damage During Canal PreparationAmee PatelNo ratings yet
- Traumatic Injuries Notes 22nk8pfDocument16 pagesTraumatic Injuries Notes 22nk8pfAmee PatelNo ratings yet
- Ijrpb 2 (5) 3 Deepak Viswanath 1384-1388Document5 pagesIjrpb 2 (5) 3 Deepak Viswanath 1384-1388Vinisha Vipin SharmaNo ratings yet
- Stereomicroscopic Evaluation of Dentinal Defects Induced by New Rotary System: "Protaper Next"Document4 pagesStereomicroscopic Evaluation of Dentinal Defects Induced by New Rotary System: "Protaper Next"Amee PatelNo ratings yet
- Effect of Four Different Placement Techniques On Marginal Microleakage in Class II Composite Restorations An Iini Vitro StudyDocument6 pagesEffect of Four Different Placement Techniques On Marginal Microleakage in Class II Composite Restorations An Iini Vitro StudyAmee PatelNo ratings yet
- New Approaches in Vital Pulp Therapy in Permanent Teeth: Iranian Endodontic Journal 2014 9 (1) :15-22Document8 pagesNew Approaches in Vital Pulp Therapy in Permanent Teeth: Iranian Endodontic Journal 2014 9 (1) :15-22Amee PatelNo ratings yet
- The Ability of Different Nickel-Titanium Rotary Instruments To Induce Dentinal Damage During Canal PreparationDocument3 pagesThe Ability of Different Nickel-Titanium Rotary Instruments To Induce Dentinal Damage During Canal PreparationAmee PatelNo ratings yet
- DENTINAL DAMAGEDocument4 pagesDENTINAL DAMAGEAmee PatelNo ratings yet
- Kurtzman Coronal Leakage TriageDocument4 pagesKurtzman Coronal Leakage TriageAmee PatelNo ratings yet
- Kurtzman Coronal Leakage TriageDocument4 pagesKurtzman Coronal Leakage TriageAmee PatelNo ratings yet
- JPediatrDent211-2926579 080745Document4 pagesJPediatrDent211-2926579 080745Amee PatelNo ratings yet
- Case Selection 2cw1hoeDocument10 pagesCase Selection 2cw1hoeAmee PatelNo ratings yet
- New Approaches in Vital Pulp Therapy in Permanent Teeth: Iranian Endodontic Journal 2014 9 (1) :15-22Document8 pagesNew Approaches in Vital Pulp Therapy in Permanent Teeth: Iranian Endodontic Journal 2014 9 (1) :15-22Amee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Daily Restorative GameDocument10 pagesHTTP WWW - Styleitaliano.org Daily Restorative GameAmee PatelNo ratings yet
- Pulpdentincomplex1 140427062105 Phpapp01Document36 pagesPulpdentincomplex1 140427062105 Phpapp01Amee PatelNo ratings yet
- Efficient Aesthetics with Semi-Direct VeneersDocument11 pagesEfficient Aesthetics with Semi-Direct VeneersAmee PatelNo ratings yet
- Comparative Table Between CaOH and MTA 1cqw453Document1 pageComparative Table Between CaOH and MTA 1cqw453Amee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Sonic Adhesive CementationDocument6 pagesHTTP WWW - Styleitaliano.org Sonic Adhesive CementationAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Stamp Technique CommunityDocument11 pagesHTTP WWW - Styleitaliano.org Stamp Technique CommunityAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Clinic Meets Research 1Document12 pagesHTTP WWW - Styleitaliano.org Clinic Meets Research 1Amee PatelNo ratings yet
- Symmetry Tricks PDFDocument11 pagesSymmetry Tricks PDFAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Back To Basics A Step by Step ProtocolDocument10 pagesHTTP WWW - Styleitaliano.org Back To Basics A Step by Step ProtocolAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Trauma Fiber PostDocument6 pagesHTTP WWW - Styleitaliano.org Trauma Fiber PostAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Autotransplantation of Third MolarDocument6 pagesHTTP WWW - Styleitaliano.org Autotransplantation of Third MolarAmee Patel100% (1)
- 1728 4250 1 PBDocument12 pages1728 4250 1 PBAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Mobile Dental Photography Part IDocument7 pagesHTTP WWW - Styleitaliano.org Mobile Dental Photography Part IAmee PatelNo ratings yet
- HTTP WWW - Styleitaliano.org Aesthetics in PosteriorsDocument10 pagesHTTP WWW - Styleitaliano.org Aesthetics in PosteriorsAmee PatelNo ratings yet
- 457645Document5 pages457645Amee PatelNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Newborn Reflexes PDFDocument1 pageNewborn Reflexes PDFShara Sampang0% (1)
- Monitor - Contec CMS8000 Service Manual v1.0Document46 pagesMonitor - Contec CMS8000 Service Manual v1.0Sbi Tucumán100% (6)
- Transitions of CareDocument3 pagesTransitions of Caredelap05No ratings yet
- List of Empanelled HospitalsDocument17 pagesList of Empanelled Hospitalsfathima555100% (1)
- CPG - Week 5Document8 pagesCPG - Week 5api-661920844No ratings yet
- Kemu Lahore MbbsDocument9 pagesKemu Lahore MbbsRayan ArhamNo ratings yet
- Healthcare Effectiveness Data and Information Set PPT Group 5 Module 4Document9 pagesHealthcare Effectiveness Data and Information Set PPT Group 5 Module 4api-301896269No ratings yet
- Maternal Resuscitation DrillDocument23 pagesMaternal Resuscitation Drillapi-219741636100% (2)
- Luc Montagnier, Nobel Prize Winner, Takes Homeopathy SeriouslyDocument8 pagesLuc Montagnier, Nobel Prize Winner, Takes Homeopathy SeriouslypathiayoNo ratings yet
- OCR BasicOphthalmology4MedicalStudents&PrimaryCareResidents8ed2004BradfordDocument244 pagesOCR BasicOphthalmology4MedicalStudents&PrimaryCareResidents8ed2004Bradfordハルァン ファ烏山No ratings yet
- Gastric Carcinoid After Long-Term Use of A Proton Pump InhibitorDocument6 pagesGastric Carcinoid After Long-Term Use of A Proton Pump InhibitorBpmStfbNo ratings yet
- Dokumen - Tips Jurnal-Traksi PDFDocument5 pagesDokumen - Tips Jurnal-Traksi PDFPrilii Ririie 'AnandaNo ratings yet
- Materi Sesi 1 - Pembicara 1 - Dr. Asri C. Adisasmita, MPH, PH.D (Seminar Kesehatan Nasional Universitas Indonesia Tahun 2017 FKM)Document33 pagesMateri Sesi 1 - Pembicara 1 - Dr. Asri C. Adisasmita, MPH, PH.D (Seminar Kesehatan Nasional Universitas Indonesia Tahun 2017 FKM)Niluh Putu DikaNo ratings yet
- Human Body PDFDocument9 pagesHuman Body PDFAnonymous W4MMefmCNo ratings yet
- 1.initial Assessment in Trauma PatientDocument52 pages1.initial Assessment in Trauma PatientmphebanggrainiNo ratings yet
- Manufacturing & Fitting The Jaipur Below-the-Knee ProsthesisDocument69 pagesManufacturing & Fitting The Jaipur Below-the-Knee ProsthesisoxideheraNo ratings yet
- PONV Guidelines Update 110110Document3 pagesPONV Guidelines Update 110110Fauzan Luthfi A MNo ratings yet
- Examination of NewbornsDocument33 pagesExamination of NewbornsWartuhi GrigoryanNo ratings yet
- PH Orthooutcomesreport 0904 Final SampleDocument15 pagesPH Orthooutcomesreport 0904 Final Sampleapi-550152465No ratings yet
- Motivation Letter Guideline Roy Bagus KurniawanDocument1 pageMotivation Letter Guideline Roy Bagus KurniawanRoy KurniawanNo ratings yet
- Postterm Pregnancy - UpToDateDocument16 pagesPostterm Pregnancy - UpToDateCarlos Jeiner Díaz SilvaNo ratings yet
- Brosur EnglishDocument2 pagesBrosur EnglishSumiari LuhNo ratings yet
- Practical Nursing Clinical 14/15 SyllabusDocument110 pagesPractical Nursing Clinical 14/15 Syllabusjedisay1No ratings yet
- Finnish Health Care GlossaryDocument8 pagesFinnish Health Care GlossaryVeronicaGelfgrenNo ratings yet
- Multi-Parameter Patient Monitor DS 7000Document2 pagesMulti-Parameter Patient Monitor DS 7000hani_qaisNo ratings yet
- Trauma WajahDocument37 pagesTrauma WajahdianNo ratings yet
- Clinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsDocument26 pagesClinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsNadia Ancharuz100% (1)
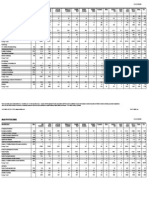
- AMA SpecialtyByTOPS 12-9-10Document10 pagesAMA SpecialtyByTOPS 12-9-10bmartindoyle6396No ratings yet
- Star Health InsuranceDocument21 pagesStar Health InsuranceShubham Chaudhari100% (1)
- Auditory pathway: From cochlea to auditory cortexDocument16 pagesAuditory pathway: From cochlea to auditory cortexDrsreeram ValluriNo ratings yet