Professional Documents
Culture Documents
Nursing Care Plan Example
Uploaded by
BrittanyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan Example
Uploaded by
BrittanyCopyright:
Available Formats
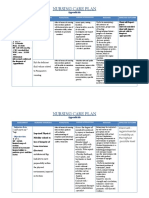
FORTIS COLLEGE
PATIENT-CENTERED CARE PLAN
Student's Name
Brittany Barnes
Patient's Name
Age
86
M. Ford
Room No.
ER 1
Sex
Admitting __ER _____
Surgical Dx. N/A
Medical Dx. CVA
ASSESSMENT
ANALYSIS
PLAN
IMPLEMENTATION
Data Collection
Subjective & Objective
Nursing
Diagnosis
NANDA
Patient-centered
Goals With
Measurable
Outcome
Nursing Orders/Action
Include Rationale & References
O- 86 year old
Impaired
O-Night Incontinence
swallowing r/t
O- Very drowsy
O- Difficulty rousing
O- Difficulty
swallowing
neuromuscular
dysfunction
1. Client will
demonstrate
effective
swallowing
without signs
of aspiration
before
08/31/2015.
2. Client will
remain free
from
aspiration
(e.g. lungs
clear,
temperature
within normal
range) by
08/31/2015.
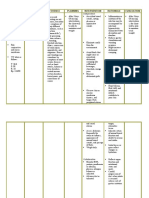
The Fortis College Student Nurse
will for all intervention will:
1.1 Manage impaired swallowing by
using a dysphagia team
comprised of a rehabilitation
nurse, speech pathologist,
dietician, physician, and
radiologist. Rationale: The
dysphagia team can help the
client learn to swallow safely
and maintain a good
nutritional status. (Wieseke,
Bantz,& Siktberg 2008).
1.2 Watch for signs of malnutrition
and dehydration and keep a
record of food intake. Rationale:
Malnutrition is common in
dysphagic clients. Clients with
dysphagia are at serious risk
for malnutrition and
dehydration which can lead to
aspiration pneumonia
EVALUATION
Evaluate Each Outcome
Criterion and Make
Recommendations
1. Goal was met. With
plans from the clients
dysphagia team, the
client was able to
demonstrate effective
swallowing without signs
of aspiration upon
discharge date of
08/31/2015.
2. Goal was partially met,
the client was able to
remain free from
aspiration, but the
clients temperature was
slightly elevated past the
normal range at 100.7
and patient was given a
dose of Tylenol.
Recommendation:
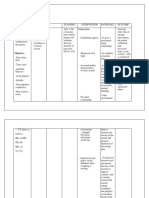
resulting froma depressed
immune function and
weakness, lethargy, and
decreased cough. (Wieseke,
Bantz,& Siktberg 2008).
1.3 Check the oral cavity from
proper emptying after the client
swallows and after the client
finishes the meal. Provide oral
care at the end of the meal. It
may be necessary to manually
remove food from the clients
mouth. If this is the case, use
gloves and keep the clients
teeth apart with a padded tongue
blade. Rationale: Food may
become pocketed on the
affected side and cause
stomatitis, tooth decay, and
possible later aspiration.
(Ackley 795).
2 Follow general aspiration
precautions which include sitting
90 degrees for all oral feedings,
take small bites/sips, slow rates,
and no straws. Rationale: An
upright posture after eating
has been associated with a
decreased incidence of
pneumonia aspiration.
(Coleman, 2004).
If signs of aspiration or
pneumonia are present,
auscultate lung sounds after
Client should continue therapy
with the use of rehabilitation
nurse, speech pathologist,
dietician, physician, and
radiologist to enhance
swallowing ability and enhance
compensatory strategies.
Discharge Teaching:
Teach the client and family
exercises prescribed by the
dysphagia team.
Teach the family how to monitor
the client to prevent and detect
aspiration during eating.
feeding. Note new onset of
crackles or wheezing, and note
elevated temperature.
Rationale: Auscultation of
bronchial lung sounds was
shown to be specific in
identifying clients at risk for
aspirating (Shaw et al, 2004).
Keep the client in an upright
position for 45 minutes to an hour
after a meal. Rationale: A study
demonstrated that the number
of elderly clients developing a
fever was significantly
reduced when clients were
kept sitting upright after eating
(Matsui et al, 2002).
You might also like
- ESOPHAGITISDocument5 pagesESOPHAGITISShenna RegaspiNo ratings yet
- Nursing Care Plan: Risk For Disuse SyndromeDocument2 pagesNursing Care Plan: Risk For Disuse SyndromeRozsy FakhrurNo ratings yet
- Child - ImmunizationsDocument1 pageChild - ImmunizationsJOHN100% (1)
- NCP For ConcussionDocument3 pagesNCP For Concussiontamtam_antonio100% (1)
- NCPDocument4 pagesNCPMarielle SorianoNo ratings yet
- Acute PainDocument5 pagesAcute PainJan Heartini SalvadorNo ratings yet
- NCPDocument2 pagesNCPShubhangi SarwanNo ratings yet
- Impaired Physical MobilityDocument1 pageImpaired Physical MobilitySheena Yen de Pano-PagdalianNo ratings yet
- Body Weakness NCPDocument1 pageBody Weakness NCPtwicetrashNo ratings yet
- Nursing Care Plan for Rheumatoid ArthritisDocument3 pagesNursing Care Plan for Rheumatoid ArthritisJashAnia MarIe EvArdo FloresNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationDocument3 pagesI. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationCherubim Lei DC FloresNo ratings yet
- NCP Impaired SkinDocument2 pagesNCP Impaired Skinarjay2306_obcq100% (1)
- Nursing Care Plan: Acute PainDocument4 pagesNursing Care Plan: Acute PainEvet VaxbmNo ratings yet
- Cue Problem Scientific Explanation Planning Interventions Rationale EvaluationDocument5 pagesCue Problem Scientific Explanation Planning Interventions Rationale EvaluationJanyn Abella ReyesNo ratings yet
- Nursing Care PlansDocument4 pagesNursing Care Plansapi-19762967No ratings yet
- NCP Lack of KnowledgeDocument3 pagesNCP Lack of KnowledgeFaye BartianaNo ratings yet
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDocument2 pagesNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- NCP 2 LRDR For PrintDocument2 pagesNCP 2 LRDR For PrintGeorge PandaNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care Planapi-309251523No ratings yet
- NCP Acitivity IntoleranceDocument3 pagesNCP Acitivity IntolerancegizelleNo ratings yet
- Risk AspirationDocument2 pagesRisk AspirationAnn OgoloNo ratings yet
- FractureDocument1 pageFractureReechie TeasoonNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- NCP For StokeDocument5 pagesNCP For StokeMemedNo ratings yet
- Nursing Care Plan for Peptic UlcerDocument3 pagesNursing Care Plan for Peptic UlcerJefferson Baluyot PalmaNo ratings yet
- NCP Alcoholic NeuropathyDocument5 pagesNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- NCP NutritionDocument2 pagesNCP NutritionBuhkz HermosoNo ratings yet
- Multiodular non toxic goiter nursing care planDocument1 pageMultiodular non toxic goiter nursing care plankzbreakerrNo ratings yet
- Enteral Feeding Nursing Care PlanDocument2 pagesEnteral Feeding Nursing Care PlanChebz Zy0% (1)
- Nursing Care Plan (NCP) For A Patient With Angina PectorisDocument3 pagesNursing Care Plan (NCP) For A Patient With Angina PectorisKian Herrera100% (1)
- Disturbed Sleep PatternDocument2 pagesDisturbed Sleep PatternROxanne S. RendonNo ratings yet
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway Clearancejae_007No ratings yet
- BPN NCPDocument6 pagesBPN NCPJoart EspinozaNo ratings yet
- NCP 3Document3 pagesNCP 3Grae TaclobNo ratings yet
- Nursing Care Plan for Infection and Bleeding PrecautionsDocument6 pagesNursing Care Plan for Infection and Bleeding Precautionshayascent hilarioNo ratings yet
- NCP InfectionDocument3 pagesNCP InfectionPrince AhmirNo ratings yet
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Document3 pagesNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaNo ratings yet
- NCP Proper - Obstructive JaundiceDocument8 pagesNCP Proper - Obstructive JaundiceWyen Cabatbat100% (1)
- Nursing Care Plan For Ineffective Airway ClearanceDocument6 pagesNursing Care Plan For Ineffective Airway ClearanceCaroline ChaNo ratings yet
- Teaching Plan: Involution (Bubble He)Document4 pagesTeaching Plan: Involution (Bubble He)Pamela BagabaldoNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKath RubioNo ratings yet
- Learning Derived (Lysha)Document1 pageLearning Derived (Lysha)Choy DavidNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalNo ratings yet
- Assessing and Managing Risk of AspirationDocument6 pagesAssessing and Managing Risk of AspirationaianrNo ratings yet
- Actual NCPDocument2 pagesActual NCPbaki0146No ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- NCPDocument4 pagesNCPMichelleNo ratings yet
- Care Plan ExampleDocument2 pagesCare Plan Exampleincess27100% (1)
- SP CSDocument4 pagesSP CSKhan HansNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionMitsika AnadiaNo ratings yet
- Incomplete Spinal Cord Injury Nursing CareDocument6 pagesIncomplete Spinal Cord Injury Nursing CareTherese MargaretNo ratings yet
- NCP PancreatitisDocument2 pagesNCP PancreatitisJeanelle GenerosoNo ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- NCP - Acute Pain Related To EdemaDocument2 pagesNCP - Acute Pain Related To EdemaChenime Añana0% (1)
- Self Care DeficitDocument4 pagesSelf Care DeficitEllaine RamirezNo ratings yet
- Chapter 029Document6 pagesChapter 029Jackie JuddNo ratings yet
- Nursing Care Plan GoiterDocument3 pagesNursing Care Plan Goiterdee_day_8100% (4)
- Imbalance Nutrition Less Than Body WieghtDocument2 pagesImbalance Nutrition Less Than Body WieghtAustin Lorenz AlvarezNo ratings yet
- NCP-RISK For ASPIRATIONDocument3 pagesNCP-RISK For ASPIRATIONChristine S. Samaniego100% (1)
- Chapter 20 - LeadershipDocument62 pagesChapter 20 - LeadershipBrittanyNo ratings yet
- Pediatric HESI Review 2016Document9 pagesPediatric HESI Review 2016Brittany78% (9)
- Hesi 2 ReviewDocument2 pagesHesi 2 ReviewBrittanyNo ratings yet
- Community Exam 2 - Study GuideDocument2 pagesCommunity Exam 2 - Study GuideBrittanyNo ratings yet
- Pediatric HESI Review 2016Document9 pagesPediatric HESI Review 2016Brittany78% (9)
- Culturally Competent Nursing Care14Document5 pagesCulturally Competent Nursing Care14Brittany100% (1)
- Maternal-Newborn Exam 4 Study GuideDocument2 pagesMaternal-Newborn Exam 4 Study GuideBrittanyNo ratings yet
- Indian School SystemDocument7 pagesIndian School Systemthe dimitrijeNo ratings yet
- Education System of IndiaDocument14 pagesEducation System of IndiaCaraxu James Ballesteros AmbrosioNo ratings yet
- Legal Research and Law ReformDocument27 pagesLegal Research and Law ReformAdv Rakhi Vyas100% (2)
- The present simple tense for regular and habitual eventsDocument5 pagesThe present simple tense for regular and habitual eventsSEBAS G.FNo ratings yet
- Kom3364 1298941863Document29 pagesKom3364 1298941863wmana1970No ratings yet
- Automate Lab Management & Secure Student DataDocument3 pagesAutomate Lab Management & Secure Student DataathiraiNo ratings yet
- Introduction To AstronomyDocument4 pagesIntroduction To AstronomyJorge SantoferNo ratings yet
- Curriculum Vitae - Emily Daina ŠarasDocument17 pagesCurriculum Vitae - Emily Daina ŠarasemilydainasarasNo ratings yet
- Home - Eastern Pulaski Community School CorporatiDocument1 pageHome - Eastern Pulaski Community School CorporatijeremydiltsNo ratings yet
- Code of Ethics For Professional TeachersDocument26 pagesCode of Ethics For Professional TeachersMei Dabalos CuntapayNo ratings yet
- National Cadet Corps: Developing Youth Leadership Through ServiceDocument41 pagesNational Cadet Corps: Developing Youth Leadership Through ServiceRohit SharmaNo ratings yet
- Graphs, Equations and FactorizationDocument5 pagesGraphs, Equations and FactorizationMohammad Tayebur AhmedNo ratings yet
- Prabhdeep Singh Baweja: ContactDocument4 pagesPrabhdeep Singh Baweja: ContactmoorthyNo ratings yet
- A51810195 Fahmitha Shawkath PDocument1 pageA51810195 Fahmitha Shawkath PsandeepNo ratings yet
- Sme (Windows & Vmware) / Project Lead: Experience SkillsDocument5 pagesSme (Windows & Vmware) / Project Lead: Experience SkillsMandar JadhavNo ratings yet
- Primary Sources of Data and Secondary SoDocument5 pagesPrimary Sources of Data and Secondary Soashikur rahmanNo ratings yet
- Berg HEJDocument19 pagesBerg HEJRonie mar Del rosarioNo ratings yet
- K K K K K K K: K K K KDocument2 pagesK K K K K K K: K K K KZenith Joy JuanNo ratings yet
- MC Research Module 3Document8 pagesMC Research Module 3payno gelacioNo ratings yet
- CV Engineer Nizar Chiboub 2023Document5 pagesCV Engineer Nizar Chiboub 2023Nizar ChiboubNo ratings yet
- University of Illinois Archives Research MaterialsDocument82 pagesUniversity of Illinois Archives Research MaterialsThe RearrangerNo ratings yet
- Htcf2 Holy Trinity College of General Santos CityDocument2 pagesHtcf2 Holy Trinity College of General Santos CityChris Gelicame Dakingking100% (1)
- Teaching and Studying Literature in The Digital Era - From Text To Hypertext (#346643) - 354651 PDFDocument8 pagesTeaching and Studying Literature in The Digital Era - From Text To Hypertext (#346643) - 354651 PDFGil Bryan BalotNo ratings yet
- CGX2003-07 enDocument7 pagesCGX2003-07 enJunianto PwNo ratings yet
- Uniform Circular MotionDocument10 pagesUniform Circular MotionAndre YunusNo ratings yet
- Homework - Unit 2bDocument2 pagesHomework - Unit 2bRicardo SousaNo ratings yet
- 0511 s11 Ms 12 Mark SchemeDocument7 pages0511 s11 Ms 12 Mark SchemeNrupen ThoratNo ratings yet
- Resume Seminar Nasional "Ilmota International Conference Digital Transformation Society 5.0"Document7 pagesResume Seminar Nasional "Ilmota International Conference Digital Transformation Society 5.0"aris trias tyantoroNo ratings yet
- Critical Approach To ReadingDocument29 pagesCritical Approach To ReadingRovince CarlosNo ratings yet