Professional Documents
Culture Documents
Bowel Obstruction
Uploaded by
Niña Victoria BacligOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bowel Obstruction
Uploaded by
Niña Victoria BacligCopyright:
Available Formats
Bowel Obstruction
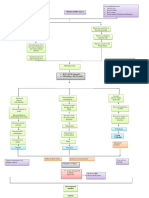
Intestinal obstruction is a blockage that keeps food or liquid from passing through
your small intestine or large intestine (colon). Causes of intestinal obstruction may
include fibrous bands of tissue (adhesions) in the abdomen that form after surgery,
an inflamed intestine (Crohn's disease), infected pouches in your intestine
(diverticulitis), hernias and colon cancer.
Without treatment, the blocked parts of the intestine can die, leading to serious
problems. However, with prompt medical care, intestinal obstruction often can be
successfully treated.
Small bowel obstruction
Small bowel obstruction is a potentially dangerous condition. There are a number of
conditions in which the contractions of the bowel muscles make the process of
moving the food very slow.
There are two types of small bowel obstruction:
functional there is no physical blockage, however, the bowels are not moving
food through the digestive tract
mechanical there is a blockage preventing the movement of food.
Funtional causes may include:
Muscle or nerve damage that may be the result of abdominal surgery, or disorders
such as Parkinson's disease
Infections
Certain medications that paralyze the contractions. Strong narcotics have this
effect.
There are also serious conditions which may require immediate intervention:
Hernias probably the most common condition in children and adults, in which a
small part of the intestine protrudes through another part of the body. Adhesions
may also be a cause. Scar tissue can form that blocks the intestinal canal.
Inflammatory Bowel Disease a condition in which the walls of the intestine
become inflamed
Tumors in the intestine that impede the flow
A volvulus, or a twisting of the intestine
Intussusception, a condition in which a segment of the intestine collapses into
itself
Symptoms of Small Bowel Obstruction
intermittent pain due to peristalsis
distension of the stomach depending on where the obstruction is located
vomiting
constipation
fever and tachycardia
Diagnosis
Lab tests
The following are adjunctive lab tests used in the evaluation of SBO:
Serum chemistries
Blood urea nitrogen (BUN) level
Creatinine
Complete blood count (CBC)
Lactate dehydrogenase tests
Urinalysis
Type and crossmatch
Laboratory tests to exclude biliary or hepatic disease are also needed; they include
the following:
Phosphate level
Creatine kinase level
Liver panels
Imaging tests
Obtain plain radiographs first for patients in whom SBO is suspected. At least 2
views, supine or flat and upright, are required. Plain radiographs are diagnostically
more accurate in cases of simple obstruction.
Enteroclysis is valuable in detecting the presence of obstruction and in
differentiating partial from complete blockages. This study is useful when plain
radiographic findings are normal in the presence of clinical signs of SBO or when
plain radiographic findings are nonspecific.
Computed tomography (CT) scanning is the study of choice if the patient has fever,
tachycardia, localized abdominal pain, and/or leukocytosis.
Ultrasonography is less costly and invasive than CT scanning and may reliably
exclude SBO in as many as 89% of patients; specificity is reportedly 100%.
Management
Nonoperative treatment
Malignant tumor - Obstruction by tumor is usually caused by metastasis; initial
treatment should be nonoperative (surgical resection is recommended when
feasible)
Inflammatory bowel disease - To reduce the inflammatory process, treatment
generally is nonoperative in combination with high-dose steroids; consider
parenteral treatment for prolonged periods of bowel rest, and undertake surgical
treatment, bowel resection, and/or stricturoplasty if nonoperative treatment fails.
Intra-abdominal abscess - CT scan guided drainage is usually sufficient to relieve
obstruction
Radiation enteritis - If obstruction follows radiation therapy acutely, nonoperative
treatment accompanied by steroids is usually sufficient; if the obstruction is a
chronic sequela of radiation therapy, surgical treatment is indicated
Incarcerated hernia - Initially use manual reduction and observation; advise
elective hernia repair as soon as possible after reduction
Acute postoperative obstruction - This is difficult to diagnose, because symptoms
often are attributed to incisional pain and postoperative ileus; treatment should be
nonoperative
Adhesions - Decreasing intraoperative trauma to the peritoneal surfaces can
prevent adhesion formation
Surgical care
A strangulated obstruction is a surgical emergency. In patients with a complete
small-bowel obstruction (SBO), the risk of strangulation is high and early surgical
intervention is warranted. Laparoscopy has been shown to be safe and effective in
selected cases of SBO.
Treatment of Small Bowel Obstruction
Antiemetics are medications that keep you from throwing up
Analgesics are mild pain relievers
Antibiotics will attack any infection you may have
Bowel decompression is a procedure in which a tube is guided into the impacted
area in an attempt to reduce the pressure and address adhesions.
Surgery
Complications of Small Bowel Obstruction
Abdominal abscesses are pockets of infected pus in the abdominal cavity
Sepsis, a condition in which the blood becomes infected
Short Bowel Syndrome is a condition that results in malabsorption of nutrients
Large bowel (intestinal) obstruction
Large bowel (intestinal) obstruction occurs when there is a blockage in the large
bowel that prevents food from passing through. The blockage cuts off blood supply
to the bowel and a part of it dies. When this happens, the pressure causes a leak
that spreads bacteria into the body or blood.
What are the causes/risk factors of large bowel obstruction?
Cancers of the:
Colon (primary cause)
Stomach
Ovary
Lung
Breast
Abdominal surgery
Abdominal radiation
The most common symptoms are:
Not being able to pass gas
Not being able to have a bowel movement
Nausea
Vomiting
Bloating
Abdominal swelling
Abdominal pain
Risks Factors
People who:
Are any age, but more often those over 70
Have had surgery on abdomen
Have had radiation therapy on abdomen
Have/have had a form of cancer
Diagnosis
How is large bowel obstruction diagnosed?
Physical exam: The doctor will check to see if you have abdominal pain, vomiting, or
any movement of gas or stool in the bowel.
Complete Blood Count (CBC): Your blood will be checked for:
The number of red blood cells, white blood cells, and platelets
The amount of hemoglobin (the protein that carries oxygen) in the red blood cells
The portion of the blood sample made up of red blood cells
Electrolyte panel: A blood test that measures the levels of electrolytes, such as
sodium, potassium, and chloride.
Urinalysis: A test to check the color of urine and its contents--such as sugar, protein,
red blood cells, and white blood cells--is performed.
Abdominal x-ray: An x-ray of the organs inside the abdomen. An x-ray is a type of
energy beam that can go through the body and onto film, making a picture of areas
inside the body.
Barium enema: A liquid that contains barium (a silver-white metallic compound) is
put into the rectum. The barium coats the large bowel and x-rays are taken. This
test may show what part of the bowel is blocked.
CT (computed tomography--also called CAT) scan: This scan makes detailed pictures
of areas inside of the body.
Colonoscopy: A doctor inserts a colonoscope into the rectum. This scope is a long,
flexible tube-like instrument. It allows the transmission of an image of the colon
lining onto a screen for the doctor to view.
How is large bowel obstruction treated?
Fluid replacement therapy: A treatment to get the fluids in the body back to normal
amounts. Intravenous (IV) fluids may be given and medicines may be prescribed.
Electrolyte correction: A treatment to get the right amounts of chemicals in the
blood, such as sodium, potassium, and chloride. Fluids with electrolytes may be
given by infusion.
Surgery: Surgery may be done if serious symptoms are not relieved by other
treatments.
If you have a long-term bowel obstruction, it will be treated by:
Surgery: The obstruction is removed to relieve pain and improve quality of life.
Stent: A metal tube inserted into the bowel to open the area that is blocked.
Medicines: Injections of medicines may be given to you to relieve symptoms.
These medications can be used to treat pain, nausea, fullness of bowel, or more
than one symptom.
Constipation
Constipation is infrequent bowel movements or difficult passage of stools that
persists for several weeks or longer.Constipation is generally described as having
fewer than three bowel movements a week.Though occasional constipation is very
common, some people experience chronic constipation that can interfere with their
ability to go about their daily tasks. Chronic constipation may also cause excessive
straining to have a bowel movement and other signs and symptoms.Treatment for
chronic constipation depends on the underlying cause. Though, in some cases, a
cause for chronic constipation is never found
Symptoms
Passing fewer than three stools a week
Having lumpy or hard stools
Straining to have bowel movements
Feeling as though there's a blockage in your rectum that prevents bowel
movements
Feeling as though you can't completely empty the stool from your rectum
Needing help to empty your rectum, such as using your hands to press on your
abdomen and using a finger to remove stool from your rectum
Constipation may be considered chronic if you've experienced two or more of these
symptoms for the last three months
Cause Blockages in the colon or rectum
Blockages in the colon or rectum may slow or stop stool movement. Causes include:
Anal fissure
Bowel obstruction
Colon cancer
Narrowing of the colon (bowel stricture)
Other abdominal cancer that presses on the colon
Rectal cancer
Rectocele
Problems with the nerves around the colon and rectum
Hormones help balance fluids in your body. Diseases and conditions that upset the
balance of hormones may lead to constipation, including:
Diabetes
Overactive parathyroid gland (hyperparathyroidism)
Pregnancy
Underactive thyroid (hypothyroidism)s
Risk factors
Being an older adult
Being a woman
Being dehydrated
Eating a diet that's low in fiber
Getting little or no physical activity
Taking certain medications, including sedatives, narcotics or certain medications to
lower blood pressure
Complications
Swollen veins in your anus (hemorrhoids). Straining to have a bowel movement
may cause swelling in the veins in and around your anus.
Torn skin in your anus (anal fissure). A large or hard stool can cause tiny tears in
the anus.
Stool that can't be expelled (fecal impaction). Chronic constipation may cause an
accumulation of hardened stool that gets stuck in your intestines.
Intestine that protrudes from the anus (rectal prolapse). Straining to have a bowel
movement can cause a small amount of the rectum to stretch and protrude from
the anus.
Tests and diagnosis
Examination of the rectum and lower, or sigmoid, colon (sigmoidoscopy). In this
procedure, your doctor inserts a lighted, flexible tube into your anus to examine
your rectum and the lower portion of your colon.
Examination of the rectum and entire colon (colonoscopy). This diagnostic
procedure allows your doctor to examine the entire colon with a flexible, cameraequipped tube.
Evaluation of anal sphincter muscle function (anorectal manometry). In this
procedure, your doctor inserts a narrow, flexible tube into your anus and rectum and
then inflates a small balloon at the tip of the tube. The device is then pulled back
through the sphincter muscle. This procedure allows your doctor to measure the
coordination of the muscles you use to move your bowels.
Evaluation of how well food moves through the colon (colonic transit study). In this
procedure, you'll swallow a capsule containing markers that show up on X-rays
taken over several days. Your doctor will look for signs of intestinal muscle
dysfunction and how well food moves through your colon.
An X-ray of the rectum during defecation (defecography). During this procedure,
your doctor inserts a soft paste made of barium into your rectum. You then pass the
barium paste as you would stool. The barium shows up on X-rays and may reveal a
prolapse or problems with muscle function and muscle coordination.
Treatments and drugs
Increase your fiber intake. Adding fiber to your diet increases the weight of your
stool and speeds its passage through your intestines. Slowly begin to eat more fresh
fruits and vegetables each day. Choose whole-grain breads and cereals.
Your doctor may recommend a specific number of grams of fiber to consume each
day. In general, aim for 14 grams of fiber for every 1,000 calories in your daily diet.
A sudden increase in the amount of fiber you eat can cause bloating and gas, so
start slowly and work your way up to your goal over a few weeks.
Exercise most days of the week. Physical activity increases muscle activity in your
intestines. Try to fit in exercise most days of the week.
Don't ignore the urge to have a bowel movement. Take your time in the bathroom,
allowing yourself enough time to have a bowel movement without distractions and
without feeling rushed.
Laxatives
Fiber supplements. Fiber supplements add bulk to your stool. Common ingredients
include methylcellulose, psyllium, calcium polycarbophil and guar gum. Brand
names include FiberCon, Metamucil, Konsyl and Citrucel.
Stimulants
Osmotics. Osmotic laxatives help fluids move through the colon. Examples include
milk of magnesia, magnesium citrate, lactulose, polyethylene glycol (MiraLax) and
sodium phosphate enema (Fleet Enema).
Lubricants. Lubricants enable stool to move through your colon more easily. One
example of a lubricant is mineral oil.
Stool softeners. Stool softeners moisten the stool by drawing water from the
intestines. Examples include Colace and Surfak.
Surgery
Surgery may be an option if you have tried other treatment and your chronic
constipation is caused by rectocele, anal fissure or stricture.
For people who have tried other treatments without success and who have
abnormally slow movement of stool through the colon, surgical removal of part of
the colon may be an option. Surgery to remove the colon is rarely necessary.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Research Body Chapter 1 4Document56 pagesResearch Body Chapter 1 4Niña Victoria BacligNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- MENTAL STATUS EXAM Edited YassiDocument6 pagesMENTAL STATUS EXAM Edited YassiNiña Victoria BacligNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- AnaphyDocument5 pagesAnaphyIvan Louise Fajardo ManiquizNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- ARFA Experience at Tuguegarao North Central SchoolDocument2 pagesARFA Experience at Tuguegarao North Central SchoolNiña Victoria BacligNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Action Plan Activity Expected Outcome Time Frame Persons Responsible Materials NeededDocument2 pagesAction Plan Activity Expected Outcome Time Frame Persons Responsible Materials NeededNiña Victoria BacligNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Accomplishment Report CHN 03-22-15 YassiDocument2 pagesAccomplishment Report CHN 03-22-15 YassiNiña Victoria Baclig100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Accomplishment Report CHN 03-22-15 YassiDocument2 pagesAccomplishment Report CHN 03-22-15 YassiNiña Victoria BacligNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- NefIgArd TrialDocument12 pagesNefIgArd Trialfarah mujtabaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Red EyesDocument3 pagesRed EyesirijoaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Bozeman Deaconess Proposal For Big Sky HospitalDocument48 pagesBozeman Deaconess Proposal For Big Sky HospitalBozeman Daily ChronicleNo ratings yet
- EmpiricalBasis GottmanDocument10 pagesEmpiricalBasis GottmanMundoSinViolenciaNo ratings yet
- NSTP ProjDocument11 pagesNSTP ProjLeeroi Christian Q Rubio100% (2)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- DR Ambreen Sultana: Professional SummaryDocument2 pagesDR Ambreen Sultana: Professional SummaryActs N FactsNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Mycoplasma Genitalium A4Document1 pageMycoplasma Genitalium A4Nauli NasirNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Game Addiction PDFDocument9 pagesGame Addiction PDFRonaldas GadzimugometovasNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Eating Disorder 1Document44 pagesEating Disorder 1Trisha Mae MarquezNo ratings yet
- Acute Diseases and Life-Threatening Conditions: Assistant Professor Kenan KaravdićDocument33 pagesAcute Diseases and Life-Threatening Conditions: Assistant Professor Kenan KaravdićGoran MaliNo ratings yet
- Ahc Chapter 22 Infection ControlDocument20 pagesAhc Chapter 22 Infection Controlapi-209542414No ratings yet
- Applying TA To The Understanding of Narcissism PDFDocument7 pagesApplying TA To The Understanding of Narcissism PDFMircea RaduNo ratings yet
- Fact Sheet Squamous Cell Carcinoma Oct 2013Document10 pagesFact Sheet Squamous Cell Carcinoma Oct 2013Triven Nair HutabaratNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- WREBDocument94 pagesWREBJessica Bahga100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Huckstep Nail For Periimplant FractureDocument3 pagesHuckstep Nail For Periimplant FracturePurushothama Rao NalamatiNo ratings yet
- Antidepressants For The Treatment of Depression in People With Cáncer 2018Document78 pagesAntidepressants For The Treatment of Depression in People With Cáncer 2018José Luis Rivera Z.No ratings yet
- Range of Pest Control Services by Pest Control (India) Pvt. LTDDocument5 pagesRange of Pest Control Services by Pest Control (India) Pvt. LTDAvinash ToraneNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Applications of Humic and Fulvic Acids in AquacultureDocument2 pagesApplications of Humic and Fulvic Acids in AquacultureAlexandra Nathaly Beltran Contreras100% (1)
- Concept Map MarwahDocument5 pagesConcept Map MarwahAsniah Hadjiadatu AbdullahNo ratings yet
- Uterine FibroidDocument3 pagesUterine FibroiddebasishroutNo ratings yet
- Pap SmearDocument17 pagesPap SmearMaisarah IsmailNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Protection of Human Rights of Women PrisonersDocument5 pagesProtection of Human Rights of Women PrisonersBrajakanta NameirakpamNo ratings yet
- Eaclipt Cpe 2019Document9 pagesEaclipt Cpe 2019inas zahraNo ratings yet
- Casework Approaches in the PhilippinesDocument3 pagesCasework Approaches in the PhilippinesJerson RicorteNo ratings yet
- MEDUMAT Standard 2 83700-ENDocument16 pagesMEDUMAT Standard 2 83700-ENJagath PrasangaNo ratings yet
- Sketchy Pharm RuntimesDocument5 pagesSketchy Pharm RuntimesAmin ValenciaNo ratings yet
- Magnetic StimulationDocument5 pagesMagnetic StimulationMikaelNJonssonNo ratings yet
- Paedo Don TicsDocument103 pagesPaedo Don TicsIana RusuNo ratings yet
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMDocument349 pagesKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniNo ratings yet
- Abnormal Psychology, Thirteenth Edition, DSM-5 UpdateDocument43 pagesAbnormal Psychology, Thirteenth Edition, DSM-5 UpdateJasmin ValloNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)