Professional Documents
Culture Documents
Leptospirosis
Uploaded by
Sanda Puspa RiniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Leptospirosis
Uploaded by
Sanda Puspa RiniCopyright:
Available Formats
Diagnostic Microbiology and Infectious Disease 78 (2014) 18
Contents lists available at ScienceDirect
Diagnostic Microbiology and Infectious Disease
journal homepage: www.elsevier.com/locate/diagmicrobio
Review
Rapid tests for diagnosis of leptospirosis: Current tools and emerging technologies
Mathieu Picardeau a, Eric Bertherat b, Michel Jancloes c, Andreas N. Skouloudis d,
Kara Durski b, Rudy A. Hartskeerl e,
a
Institut Pasteur, Unit de Biologie des Spirochtes, National Reference Center and WHO Collaborating Center for Leptospirosis, Paris, France
World Health Organization, Health Security and Environment/Pandemic and Epidemic Diseases, 20 Av Appia, 1211, Geneva 27, Switzerland
Health and Climate Foundation, 1425K St NW suite 350, Washington DC 20005, USA
d
Institute for Environment and Sustainability, Joint Research Centre, European Commission, Ispra VA, Italy
e
Royal Tropical Institute, KIT Biomedical Research, WHO/FAO/OIE and National Collaborating Centre for Reference and Research on Leptospirosis, Amsterdam, The Netherlands
b
c
a r t i c l e
i n f o
Article history:
Received 23 July 2013
Received in revised form 9 September 2013
Accepted 15 September 2013
Available online 1 October 2013
Keywords:
Leptospirosis
Diagnostics
Outbreak
Surveillance
Diagnostic test
Early warning
Early diagnosis
Innovation
a b s t r a c t
Leptospirosis is an emerging zoonosis with a worldwide distribution but is more commonly found in
impoverished populations in developing countries and tropical regions with frequent ooding. The rapid
detection of leptospirosis is a critical step to effectively manage the disease and to control outbreaks in both
human and animal populations. Therefore, there is a need for accurate and rapid diagnostic tests and
appropriate surveillance and alert systems to identify outbreaks. This review describes current in-house
methods and commercialized tests for the rapid diagnosis of acute leptospirosis. It focuses on diagnostic tests
that can be performed with minimal training and limited equipment in less-developed and newly
industrialized countries, particularly in resource-limited settings and with results in minutes to less than 4
hours. We also describe recent technological advances in the eld of diagnostic tests that could allow for the
development of innovative rapid tests in the near future.
2014 Elsevier Inc. All rights reserved.
1. Introduction
Leptospirosis is of particular public health concern due to its
global distribution, its epidemic potential, its presence in animals
and the natural environment, and its high potential for human
mortality, if left untreated. A World Health Organization (WHO)
lead experts' group estimated the global burden of leptospirosis to
be 873,000 severe annual cases and 49,000 deaths (http://www.
who.int/zoonoses/diseases/lerg/en/index.html). The recent outbreaks of leptospirosis in the South East Asia have increased the
awareness of the need for improved diagnostic tests for leptospirosis (Agampodi et al., 2011; Amilasan et al., 2012). Leptospirosis is
also one of the most important zoonotic diseases over the world.
Human infection results from contacts with carrier animals or
environment contaminated with leptospires. It is a major environmental endemic disease with increased threat of severe epidemics
often linked with natural disasters such as oods and hurricanes
(Lau et al., 2010; Levett, 2001).
Because there is much overlap in the clinical presentation of
undifferentiated febrile illnesses, which includes leptospirosis, malaria, rickettsioses, and arboviral diseases, it is not possible to reliably
predict the pathogen based on clinical signs and symptoms (WHO,
2003). The lack of adequate and easy-to-use lab diagnostics is key in
leptospirosis: it largely contributes to the under-recognition of its
burden and it is an obstacle to the understanding of the natural history
of the infection. This means that many questions related to the control
strategy remain unanswered, including on case management, particularly in epidemic situation.
Public health authorities and clinicians have pointed out the
urgent need for developing more effective technologies on case
detection and diagnosis.
Culture and the microscopic agglutination test (MAT), which are
gold standard methods for leptospirosis diagnosis, are not useful for
early diagnosis: culture of Leptospira, which are slow-growing
bacteria, is difcult, and anti-Leptospira antibodies can only be
detected by the second week after symptoms (Levett, 2001).
Moreover, these techniques require specic equipment and/or
laboratory and highly trained staff. Early and accurate diagnosis, so
that treatment with antibiotics can be started without delay, may
contribute to improved patient outcomes (Bharti et al., 2003). This
may also minimize the cost of hospitalization.
2. Diagnostic test needs
Corresponding author. Tel.: +31-20-5665438; fax: +31-20-6971841.
E-mail address: r.hartskeerl@kit.nl (R.A. Hartskeerl).
0732-8893/$ see front matter 2014 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.diagmicrobio.2013.09.012
The choice for the use of a diagnostic test will depend on a number
of factors, including its diagnostic accuracy, nancial feasibility,
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
technical or practical feasibility, and the need for an early and/or
rapid result.
2.1. Performance of diagnostic tests
The diagnostic accuracy of tests is frequently expressed in terms of
sensitivity, specicity, and predictive values. However, most of the
diagnostic tests for leptospirosis, both commercially available and inhouse tests, have been presented without a solid validation scheme
such as STARD principles (http://www.stard-statement.org), thus
hampering the selection of the test of choice (Goris et al., 2011).
Moreover, especially rapid diagnostic tests and enzyme-linked
immunosorbent assays (ELISAs) have been reported with varying
diagnostic performances in distinct countries or regions. There might
be several explanations for the reported variations in diagnostic assay
performance: i) The retrospective use of selected samples and the
choice of case denition may be a source of bias; ii) it is a
misunderstanding that rapid tests are easy and thus do not require
experience. The subjective judgement of test results by eye, mostly for
serological tests, may also introduce a degree of bias, particularly in
the case of untrained personnel. iii) It may reect population-related
differences such as past exposure to leptospirosis, exposure to
environmental leptospires, or infection with other infectious agents.
This is particularly true for tests based on whole-bacteriaderived
antigens that can lead to false positives due to persistent or crossreacting antibodies. This point is not easily solved by using
recombinant antigens. While these will enable more specic test
results with antigen-homologous infections, sequence variation
between Leptospira species and serovars will reduce test sensitivity
in case of many, if not most, other serovars.
The best approach for applying the most optimal test would be to
perform a valid local evaluation prior to introduction or, alternatively,
have tests validated by globally representative serum banks present
on accredited international reference centres that are familiar with
validation schemes of tests.
The need for a high diagnostic accuracy should always be
considered within the scope of local requirements. While conrmation in expert reference centres requires a high level of diagnostic
accuracy, rapid screening tests might sufce for peripheral health care
centres, certainly when the local epidemiology has been well
assessed. Moreover, such tests are very useful for monitoring of
outbreaks when a rapid unusual accumulation of cases might give an
early alert, provided that specimens are collected, transported, and
stored in an adequate manner.
baseline data on the local epidemiology is critical for the interpretation of test results or for the prediction, prevention, or early
intervention of outbreaks. For adequate surveillance of leptospirosis,
the availability of diagnostic tests is pivotal. The higher the diagnostic
accuracy of the test, the better it is for surveillance, although any type
of diagnostic test might be helpful for this purpose, provided that its
performance has been well assessed.
3. What sample(s) for early diagnosis?
Typically, acute symptoms develop 712 days after infection,
although rarely, the incubation period can be as short as 23 days or
as long as 30 days. Infection by pathogenic Leptospira can be divided into
2 phases (Fig. 1). The rst phase of leptospirosis is the septicemic or
acute phase, which lasts for 37 days with fever, headache, and myalgia.
During this stage, Leptospira are found in the bloodstream in decreasing
numbers up to 15 days (Agampodi et al., 2012; Bharti et al., 2003). To
detect Leptospira, blood samples have to be collected until 2 days after
the start of antibiotic therapy, since antibiotics quickly remove
Leptospira from the blood. The second stage of the disease or immune
phase generally appears during the second week after the onset of
symptoms, and antibodies usually persist for several months (Silva
et al., 1995). During this stage, leptospires are cleared from the
bloodstream as the titres of IgM class antibodies increase (Levett, 2001).
Absence of detection of leptospiral antigen or DNA in conrmed
cases of leptospirosis can be attributed to a low or a short
leptospiremia during the acute phase of the disease, to blood samples
taken late in the disease, or to the administration of antibiotics. For
antibody-based tests, the window of time prior to or during early
sero-conversion may lead to false-negative test results in the early
acute phase of disease.
PCR on serum and plasma from whole blood anticoagulated with
heparine, a natural inhibitor of PCR, was found to be less sensitive
than PCR performed on other fractions for detection of Leptospira DNA
(Bourhy et al., 2011; Kositanont et al., 2007; Levett et al., 2005;
Smythe et al., 2002; Stoddard et al., 2009). Previous studies have
generally found that plasma from EDTA anticoagulated whole blood
gave optimal results for DNA amplication (Ahmed et al., 2009). For
serology assays, the use of serum or plasma, either heparin or EDTA
anticoagulated, produces equivalent results (Goris et al., 2012).
Alternatively, leptospires can also be detected by culture and PCR
2.2. Rapid versus early diagnostic tests
A rapid diagnostic test (RDT) does not equal an early test. While a
rapid test provides a quick test result, an early test conrms a clinical
suspicion at the early acute phase of the disease. For leptospirosis,
early detection is particularly important to eliminate differential
diagnoses and to start the appropriate treatment as soon as possible.
While molecular tests, such as the polymerase chain reaction (PCR),
demonstrating the presence of the causative agent in a clinical sample,
mainly enable conrmation during the rst 5 days post onset of the
disease (DPO), serological tests depend on the accumulation of
detectable amounts of anti-Leptospira antibodies in late acute to
convalescent samples (Ahmed et al., 2009, 2012; Goris et al., 2012).
Hence, serological tests, by denition, conrm the disease afterwards
and thus do not directly contribute to the timely management of the
individual patient.
In summary, novel often expensive early or standard diagnostic
tests are best placed at expert reference centres where conrmation of
RDT results can be performed or at hospitals with the required
expertise. RDTs are highly useful at peripheral facilities and might be
key for early outbreak warning. For all situations, the availability of
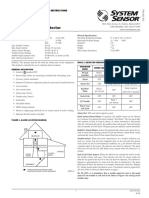
Fig. 1. The kinetics of leptospiral infection in blood. Infection produces leptospiraemia
in the rst few days after exposure, which is rapidly followed by migration of
leptospires to target organs. Anti-Leptospira IgM antibodies are detectable before the
appearance of agglutinating and IgG antibodies. The broken line ( ) indicates the
dynamics of the presence of leptospires or leptospiral antigen and DNA in the blood;
the solid line indicates the level of IgM anti-Leptospira antibodies; the dashed line ()
indicates the dynamics of the anti-Leptospira IgG antibody response. The depicted
dynamics are relative and are not intended to indicate quantitative levels, which vary
between patient species and individuals.
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
from urine 1014 days after the onset of symptoms albeit that this
does not contribute to an early diagnosis (Levett, 2001).
The nucleic acidbased diagnostic tests involve nucleic acid
purication. Commercially available kits usually allow a good
recovery of DNA from blood within less than 1 hour (Bourhy et al.,
2011). The use of magnetic beads allows concentration of nucleic acid
or antigens in samples (Schreier et al., 2012; Taylor et al., 1997). To
simplify DNA extraction procedures, use of whole blood spotted on
Whatman FTA lter paper, which is a chemically treated lter paper,
can allow for the rapid isolation of pure DNA. Similarly, serological
studies can be performed from dried whole blood spotted onto
Whatman lter paper (Desvars et al., 2011). These commercially
available reagents are an easy and inexpensive means for the
collection and storage of samples in resource-limited settings or for
the shipment of samples to reference centres.
4. Current diagnostic tools
As current diagnostic tools, we consider the direct examination
of blood, the rapid nucleic-acid diagnosis, and rapid antibodybased tests.
4.1. Direct examination of blood
The bacterial load in blood ranges from 10 2 to 10 6 Leptospira per
millilitre (Agampodi et al., 2012) in the acute phase. In theory,
leptospirosis can therefore be diagnosed by dark-eld microscopy of
blood taken during the rst week of illness. The limit of detection was
determined as approximately 10 4 leptospires per millilitre of blood or
urine (Table 2). Although it is relatively inexpensive, this test
requires a dark-eld microscope, which is rarely available or
affordable in resource-limited settings. Dark-eld microscopy of
blood is unreliable as Brownian movement of collagen brils, red
blood cell membranes, and other artefacts can resemble viable
leptospires (Vijayachari et al., 2001).
4.2. Rapid nucleic acidbased diagnostic test
4.2.1. Polymerase chain reaction
PCR-based methods are becoming more widely used for the
detection of pathogenic Leptospira strains, in part because of their
superior sensitivity and ability to establish an early diagnosis. Realtime PCR, either using SYBR Green or Taqman technology, has the
advantage that it gives a result much faster than conventional PCR and
is less prone to contamination. The commercialization of portable PCR
thermocyclers compatible with real-time PCR chemistries may also
allow the rapid detection of pathogens in the eld.
Several conventional (including nested PCR) and real-time PCRs
have been developed for the detection of leptospires, targeting whole
arrays of genes, whether or not conned to pathogenic species,
exemplied by secY and lipL32, respectively. However, relatively few
assays have been validated for use with a variety of human and
canine samples (Ahmed et al., 2012; Ahmed et al.; Slack et al., 2007;
Thaipadungpanit et al., 2011; Villumsen et al., 2012). This is
surprising because a good diagnostic accuracy as revealed by a solid
validation should be the prime criterion of choice for implementing a
diagnostic PCR. The limit of detection of PCR assays was generally
determined as 1001000 bacteria per millilitre of blood or urine
(Bourhy et al., 2011; Slack et al., 2006; Smythe et al., 2002; Stoddard
et al., 2009). Bacterial load may be obtained if quantitative standards
are included in the amplication run and a standard curve has been
produced. However, this may not be informative as the quantitative
leptospiremia was not always correlated with the vital prognosis of
patients (Agampodi et al., 2012; Segura et al., 2005; Truccolo et al.,
2001). A positive PCR usually indicates that one of the members of the
pathogenic Leptospira species is present in the sample but PCR cannot
be used to predict the leptospiral serovar. There are many methods of
post-amplication analysis, but only a few have been described for
the identication of leptospiral genotype or serovar, including melt
curve analysis (Merien et al., 2005) and DNA sequencing (Perez and
Goarant, 2010). Further studies should evaluate the usefulness of
other post-amplication analyses such as high-resolution melt
analysis (which measures the melting temperature of amplicons in
real time, using a uorescent DNA-binding dye) and microarray
analysis for the identication of Leptospira at the subspecies level
(Ahmed et al., 2010).
4.2.2. Isothermal methods
An increasing number of isothermal amplication techniques,
including nucleic acid sequencebased amplication, loop-mediated
isothermal amplication (LAMP), helicase-dependent amplication,
rolling circle amplication, and strand displacement amplication,
have been recently developed, some of which have been applied to
leptospirosis (Colenbrander et al., 1994; Koizumi et al., 2012; Lin et al.,
2009; Sonthayanon et al., 2011). Isothermal amplication is an
attractive alternative to PCR-based methods since thermocyclers are
not required. It simply requires a heating device to maintain a
constant temperature of 6065 C, making it particularly suited to
resource-limited settings. In LAMP, specic and efcient amplication
of DNA is performed within 1 hour by Bst DNA polymerase using 6
primers under isothermal conditions. The amplied DNA can be
detected by visual inspection of uorescence or turbidity, without the
need for gel electrophoresis (Mori and Notomi, 2009). The method
may also enable direct amplication from clinical specimens, thereby
eliminating the need for an additional nucleic acid purication step.
LAMP assays targeting the lipL41 or rrs genes were recently developed
for the rapid detection of pathogenic Leptospira spp. (Koizumi et al.,
2012; Lin et al., 2009; Sonthayanon et al., 2011). The specicity of
LAMP assays was moderate to low, and the limit of detection was
determined between 2 and 100 leptospires per reaction mixture
(Ahmed et al., 2009; Slack et al., 2007;Sonthayanon et al., 2011).
Besides, current costs of an LAMP assay are similar to those of a realtime PCR and it is as yet unclear whether LAMP will become
economically competitive. Despite its advantages, the usefulness of
LAMP for the diagnosis of leptospirosis needs to be further evaluated
in endemic area with resource-limited settings.
4.3. Rapid leptospirosis antibody-based tests
4.3.1. ELISA
Traditional serological methods such the ELISA are widely used for
the diagnosis of leptospirosis. ELISA can be performed with minimal
training and typically provides results in 24 hours. Numerous
commercial IgM ELISAs have been developed based on detection of
antibodies against whole cell Leptospira (Table 1), usually, the
saprophyte Leptospira biexa, which shares many surface antigens
with pathogenic strains. In-house IgM ELISA based on a whole cell
antigen extract obtained from a local isolate can also be used (Goris
et al., 2012).
Recombinant surface proteins or lipoproteins of Leptospira have
also been used as antigens. In general, the antigens used for ELISA may
not recognize the diversity of circulating strains, and the overall
sensitivity of these tests is poor (Levett, 2001; McBride et al., 2005). A
conclusive serological diagnosis of leptospirosis cannot be made by
ELISA alone but needs laboratory conrmation through MAT, PCR, or
culture. The results of ELISA are usually obtained in a few hours
(Table 2), and it may require several samples to decrease the cost of
the assay.
Despite the varying performance of ELISA, studies have
generally found that the assay detects anti-Leptospira antibodies
earlier in the course of the disease than MAT (Aviat et al., 2010;
Bajani et al., 2003;Cumberland et al., 1999; Doungchawee et al.,
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
Table 1
Commercial tests used for the diagnosis of acute leptospirosis.
Test/kit
Manufacturer
Technology
Serion ELISA Classic Leptospira IgM Test kit
Leptospira IgM ELISA
Leptospira IgM
Leptospira IgM Microwell serum ELISA
Leptospira IgG/IgM Microwell serum ELISA
ELISA (IgM/IgG)
Mouse Leptospira IgG ELISA Kitb
Leptospira IgG/IgM Combo rapid Test
IHA
Leptospira-MC Test
LeptoTek Lateral Flowa
Test-it
Leptocheck-WB
SD Leptospira LF
IgM lateral ow test
LeptoTek Dri Dot
Leptorapide
Primergen Lepto LipL32
AdiavetTM Lepto RealTimeb
FastPanel PCR Canine Leptospirosis Proleb
Institut Virion/Serion GmbH (Germany)
Panbio Ltd (Australia)
Diagnostic Automation/Cortez Diagnostics, Inc. (USA)
IVD Research Inc. (USA)
IVD Research Inc. (USA)
Standard Diagnostics (Korea)
My-Bio-Source (USA)
CTK Biotech, Inc. (USA)
Mayo medical Laboratories (USA)
Japan Lyophilization Laboratory (Japan)
BioMerieux (the Netherlands)
Life Assays (South Africa)
Zephyr (India)
Standard Diagnostics (Korea)
Omega Diagnostics (United Kingdom)
BioMerieux (the Netherlands)
Linnodee, Northern (Ireland)
PrimerDesign (France)
Adiagen, BioMerieux (France)
Antech Diagnostics (USA)
ELISA
ELISA
ELISA
ELISA
ELISA
ELISA
ELISA
IHA
Indirect hemagglutination test
Microcapsule agglutination test
LFA
LFA
LFA
LFA
LFA
Latex card-agglutination test
Latex card-agglutination test
Real-time PCR
Real time-PCR
Real time-PCR
a
b
Expected to be available soon by IMACCESS.
Veterinarian use.
2008; Levett, 2001; Signorini et al., 2013). Anti-Leptospira IgM
antibodies are not detectable before 45 days after onset of
symptoms (Fig. 1) but appear earlier than IgG and agglutinating
antibodies (Silva et al., 1995).
4.3.2. Other rapid antibody detection methods
Other rapid antibody detection methods include macroagglutination, immunouorescence assay, indirect hemagglutination assay
(IHA), latex agglutination, lateral ow assays (LFA), and IgM dipstick
(McBride et al., 2005).
Immunouorescence makes use of antibodies conjugated to a
uorescent dye as detection reagent. The method can detect
specic antibodies in body uids or antigen in tissue sections.
The sensitivity and specicity of the indirect uorescent antibody
(IFA) test correspond to those of the ELISA (Appassakij et al., 1995).
However, this test is not commercially available, and it requires a
uorescence microscope.
The macroscopic slide agglutination test (MSAT) uses dense
suspensions of killed Leptospira serovars (Wolff and Bohlander,
1966). The antigen should consist of all locally prevalent strains or,
alternatively, the saprophyte L. biexa serovar Patoc, which shares
many surface antigens with pathogenic strains. A drop of serum is
mixed on a glass plate with the antigen, briey incubated at ambient
temperature and inspected by naked eye for presence of agglutination. The MSAT is relatively insensitive for diagnosis but may be useful
for epidemiological screening (Marin-Leon et al., 1997).
IHA uses red blood cells sensitized with an extract of an
erythrocyte-sensitizing substance from L. biexa serovar Patoc
(Chang et al., 1957; McComb et al., 1957). IHA detects both IgM
and IgG antibodies. Heat-inactivated serum is mixed with sensitized
red blood cells, and agglutination is examined by the naked eye.
Estimates of the sensitivity of the IHA in populations in which
leptospirosis is endemic have varied from good (Levett and
Whittington, 1998) to poor (Efer et al., 2000), possibly because
of differences in case ascertainment and study design, including
inclusion of epidemiological distinct populations and the unavailability of prospective unbiased samples (Hull-Jackson et al., 2006;
McBride et al., 2007).
Table 2
Performance of rapid diagnostic tests during the acute phase of leptospirosis.
Test
Approximate
cost a
Execution time
Equipment
Sensitivityb
Specicity
Optimal detection
windowc
Direct examination
b 1
15 min
Dark eld microscope
low
Early acute
Commercialized
IgM ELISA
In house IgM ELISA
816
12 h
ELISA washer and reader
104/mLd
(analytical)
N90%
8895%
24 h
ELISA washer and reader
93%
98-100%
81%
96%
LFA
25
1520 min
Cold room/refrigerator
Conventional PCR
68
90100%
68
Thermal cycler and gel
electrophoresis system
Real Time thermal cycler
60100%
Real-time PCR
60100%
90100%
Early acute
Isothermal method
1015
5 h (including DNA
extraction with a kit)
2 h (including DNA
extraction with a kit)
2 h (including DNA
extraction with a kit)
Late acute to
convalescent
Late acute to
convalescent
Late acute to
convalescent
Early acute
Heating device and, in most
cases, gel electrophoresis system
Less than PCR
Less than
PCR
Early acute
The generalized data on costs and diagnostic accuracy listed in this table, in part, summarize the data presented by Hartskeerl et al. (2011).
a
Direct costs, not including use of DNA extraction kit, salaries, equipment, etc., but dependent on local import taxes.
b
First 10 days after the onset of symptoms, depending on the stage of disease.
c
Optimal sensitivity expressed in phase of disease: early acute is 5 DPO, late acute is 510 DPO, convalescent is N10 DPO.
d
From Levett, 2001.
e
Several novel LFAs can be stored for months at ambient temperature.
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
The microcapsule agglutination test is using a synthetic polymer in
place of red blood cells (Arimitsu et al., 1982) coated with a mixture of
whole cellderived antigens from pools of serovars, for example,
Australis, Autumnalis, and Hebdomadis. The test has been evaluated
at various reference centres (Arimitsu et al., 1994). It showed
sensitivity similar to the MAT and IgM-ELISA in early acute phase
samples but failed to detect infections caused by some serovars.
The complement xation (CF) test is used as a serological
technique but can also be applied for antigen detection. The test is
based on the fact that if the serum contains antibodies against the
antigen of interest, they will form antigen-antibody complexes,
leading to reaction with the complement system and cell lysis. In the
test, antigen of the suspected infectious agent is added to the heated
serum together with complement proteins. Causative agent-specic
antibodies bind to the antigen, and the resulting complex binds the
complement, thus inhibiting the haemolysis of the erythrocytes.
Absence of haemolysis constitutes a positive test. CF is a tedious inhouse test that has not found a widespread application and lacks
valid evaluations of its diagnostic accuracy (Andreescu, 1990).
LFA can be performed at the bedside of the patient, as whole blood
(nger prick) can be used for testing, and results can be obtained in
10 minutes. The mobile phase is usually made of colloidal goldlabelled anti-IgM antibody, specic for the human or animal patient.
An LFA based on whole cell antigen extract from the saprophyte L.
biexa was developed by the Royal Tropical Institute (Amsterdam,
The Netherlands) and enables the rapid detection of Leptospiraspecic IgM antibodies in human sera (Smits et al., 2001). This assay,
which is available as a commercial test, showed performances that
are similar to ELISA and has been tested in the eld (Sehgal et al.,
2003). A recent prospective evaluation of 3 RDTs, including 2 LFAs,
revealed a changing diagnostic performance of these tests through
time, and it was argued that companies might need to apply more
strict quality checks at the production procedures (Goris et al., 2013).
An LFA based on recombinant leptospiral immunoglobulin-like (Lig)
proteins, which are surface-exposed proteins specic to pathogenic
Leptospira strains, demonstrated high performance in identifying
leptospirosis during urban epidemics in Brazil (Nabity et al., 2012).
However, this assay does not appear to be generalizable because of its
limited ability to detect antibodies against serovars not belonging to
the serogroup Icterohaemorrhagiae, which is the predominant
serogroup in urban Brazil (Nabity et al., 2012). Another immunochromatographic rapid diagnostic test for the early detection of antiLeptospira human IgM is also currently under evaluation at the
Institutes Pasteur in Paris and Nouma. In this assay, whole killed
bacteria of the intermediate species Leptospira fainei, which may
share common antigenic features with saprophytes and pathogens,
were used as an antigen (Bourhy et al., 2013; Goarant et al., 2013).
Although some of the aforementioned tests are commercially
available, these tests are usually restricted to specic areas (for
example, IFA is mostly used in Thailand), and they are not widely
used in the diagnosis of acute leptospirosis.
5. Tests and operational applications
Early testing for effective case management and early case nding
for outbreak management are critical. This requires the use of early
tests during the 5 DPO. To date, PCR and, more particularly, real-time
PCR, are the most appropriate because of its early diagnostic accuracy.
Further operational research, however, has to be developed in
different epidemiological and operational conditions for making its
use more cost-effective and ensuring early registration at the national
reference centre. In particular, the usefulness of isothermal amplication techniques needs further evaluation in endemic areas with
resource-limited settings.
Diagnosis should be done at the peripheral level, using RDTs for
rapid, but preliminary, determination, while at a referral laboratory
level, denitive conrmation can be done, using more sophisticated
and expensive tests, such as isolation by culturing, MAT, or real-time
PCR. MAT would remain the best choice if a high early diagnostic
accuracy is not feasible and/or if presumptive information on infecting
serogroups is needed. It is stressed that notably for sero-diagnostics,
local validation is required given the varying performances of such
tests within different epidemiological conditions.
The development of conrmation algorithms has to take into
consideration undifferentiated acute fevers, including malaria, dengue, rickettsiosis, yellow fever, and typhoid (WHO, 2003). Some
operational research on the use of multiplex tests is underway.
6. Challenges towards improvement of rapid diagnostic tests
6.1. Sample collection
It is a challenge to determine which type of sample to collect in
order to achieve the greatest diagnostic accuracy. Sample collection
should preferably be non-invasive or be limited to small intervention
(nger prick).
Urine presents a good non-invasive diagnostic sample. The use of
urine has a disadvantage, that is, leptospires are only reliably shed
from the late acute phase and claims on early diagnostic potential of
antigen detection tests using urine still wait for valid evaluation of the
diagnostic performance (Saengjaruk et al., 2002). However, it is
conceivable that Leptospira derived breakdown components or early
immune response molecules are present in the urine at an early stage.
This hypothesis needs to be investigated.
Blood is an excellent diagnostic sample since leptospires are
present in the rst 45 days after onset of disease, which enables early
diagnosis. In the near future, non-invasive blood tests with microportable devices will become available.
Saliva: the interest of this specimen is doubtful as presence of
leptospires, leptospiral antigens, or anti-Leptospira antibodies in saliva
is largely unclear or unknown. As potential non-invasive specimens,
saliva and sputum would deserve further investigations.
Breath has been investigated as a diagnostic sample for several
diseases, including TB. The idea is that the composition of breathed air
changes by infection and may contain components of the causative
agent or body degradation products (Kolk et al., 2012). Breath might
present an interesting diagnostic sample, certainly with the pulmonary syndrome.
Furthermore, one should consider the use of the test-upontreatment principle (treatment will increase the concentration of
degradation products that can be more easily detected for conrmative diagnosis than the whole bacterium) as an attractive approach
that, basically, could be combined with any of these clinical samples.
6.2. Multiplex tests for differential diagnosis
In tropical climates, leptospirosis must be differentiated from
other clinically similar acute febrile illnesses that could be prevalent in
the same regions. Leptospirosis PCR- or antibody-based tests could be
combined with other febrile illnesses to assess a specimen for a wide
variety of microorganisms. A multiplex real-time PCR assay, which
allows the sensitive detection of different DNA targets in a single
reaction, could also be developed for the simultaneous detection of
agents of febrile illnesses (e.g., leptospirosis, rickettsioses, dengue,
and other viral haemorrhagic infections). Alternatively, one might
choose for a multiplex system that separates bacterial from viral
diseases, which is of major importance for taking decisions on
treatment. Novel, innovative platforms such as the circular multianalyte point-of-care devices present valuable approaches for
multiplex serological detection (http://www.kit.nl/kit/Sylis-enHIV-test) and might be adaptable for molecular detection.
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
6.3. Antigen capture and/or amplication
Despite intensive investigations, a major challenge remains to
discover surface-exposed antigens or genetic targets that are
conserved across the major leptospiral strains. The genus Leptospira
comprises 21 species subdivided in 9 pathogenic species that are the
etiological agents of leptospirosis, 7 saprophytic species, and 5
intermediates species (Cerqueira and Picardeau, 2009). Pathogenic
Leptospira spp. are classied into more than 250 serovars on the basis
of structural heterogeneity in the carbohydrate component of the
lipopolysaccharide (LPS). The genomes of 5 Leptospira spp. (L. biexa,
L. interrogans, L. santarosai, L. borgpetersenii, and L. licerasiae) have
been sequenced (Bulach et al., 2006; Chou et al., 2012; Picardeau et al.,
2008; Ren et al., 2003; Ricaldi et al., 2012), and an on-going project
should allow the sequencing of about 200 leptospiral strains by the J.
Craig Venter Institute using next-generation DNA sequencing approaches (http://gsc.jcvi.org/projects.php). This new sequencing
information will make it possible to identify novel diagnostic targets
for specic antigen or nucleic acid detection.
Immunomagnetic capture is used in a number of tests to
concentrate nucleic acid or antigens in clinical specimens. Magnetic
beads could be conjugated with specic antibodies, which can
recognize and capture target antigen. Immunomagnetic capture
systems could, for example, be made serogroup or serovar specic.
Magnetic beads can also be used to concentrate pure nucleic acid
extracted from clinical samples. It should be stressed that DNA extraction
is the less efcient step in the amplication process. Concentration of
DNA with maximal removal of inhibitors thus should provide an
improvement of the sensitivity for amplication-based methods.
Otherwise, the value of less inhibitor sensitive methods like LAMP or
enzyme free amplication methods needs further investigation.
For isothermal methods that present a promising alternative to
PCR in resource-limited settings, more studies are required to
evaluate their performance characteristics and determine their
ideal application.
6.4. Detection systems
LFAs have successfully been used to detect antigens from bacterial
pathogens in clinical samples. These assays are usually based on
monoclonal antibodies selected to have broad reactivity against
antigen(s) of the pathogen. One limitation for the development of
such a test for the diagnosis of leptospirosis is the relatively low
number of bacteria (b10 6 Leptospira/mL) found in blood and the
duration of time in which the bacterium can be detected. Moreover,
our knowledge of the expression of leptospiral antigens during the
infection remains limited. LPS constitute the main antigen for
Leptospira, but this antigen is serovar specic. Antibodies directed
against leptospiral LPS are therefore restricted to the detection of
antigenic related serovars (or serovars with serologically related LPS).
Although based on in vitro data, it has been shown, for example, that
the conserved lipoprotein LipL32 is the most abundant protein of L.
interrogans at 38,000 copies per cell (Malmstrom et al., 2009).
Monoclonal antibodies targeting this highly expressed protein will
then need to be evaluated for the ability to react with the wide
diversity of leptospiral serovars.
For DNA detection, multiplex real-time PCR assays for the
diagnostic of leptospirosis, together with other agents of febrile
illnesses will be a major improvement (see above). Microarray tests
remain expensive for routine use, and data interpretation usually
requires an adequate training in the use of analysis software.
6.5. Incorporating new technologies
For antigen detection, one of the most promising areas in
molecular diagnostics is the use of nanomaterials. Nanobiosensors,
detecting changing electronic, optic, or other physical parameters
upon capturing the antigen, could detect low levels of antigen in a
biological sample. Moreover, we speculate that the use of quick
response codes on RDTs combined with data and location recording
by a smart phone or even more innovative lab-on-a-chip approaches
that enable online transmission of data to a central point in a country
or region might provide effective tools for surveillance and early
outbreak monitoring. In turn, this will contribute to the understanding of the dynamics of outbreaks and hence to the rational design of
cost effective prevention and early intervention measures.
Such types of biosensors could be suitable not only for the
diagnosis of the disease on humans; it could also become an
important instrument for environmental monitoring as part of
network of sensors for water pollution monitoring (Rickerby and
Skouloudis, 2011). Sensors and biosensors are useful analytical tools
for environmental monitoring because they provide cheap and rapid
analysis of data. Biosensors consist of a biological sensing element,
which may be an antibody, antigen, enzyme or whole cell, interfaced
to a transducer, such as an electrode or optical bre. It was found that
that the afnity and sensitivity of imprinted polymers were
comparable to those of polyclonal antibodies. Biosensors integrated
with wireless telecommunication systems could revolutionise environmental monitoring due to the following advantages. The nanobiotechnology-based diagnostic techniques can potentially detect a
wide range of aquatic contaminants and toxins that are of relevance
for leptospiral survival outside the host and, hence, in effect, expose
risks. It will improve the geographical resolution and furnish higher
sensitivity for local detection of sources. It provides a multi-parameter
analysis allowing simultaneous measurements and provides remote
surveillance and control capability for continuous real-time monitoring, early warning, and fast response.
7. Conclusion
Rapid diagnostic tests should ideally be accurate, simple to use,
relatively inexpensive, easy to interpret, stable under extreme
conditions, with little or no processing, and give the results within
12 hours (Banoo et al., 2010). None of the available tests described
above for the diagnosis of acute leptospirosis meet all these criteria.
Diagnostic tests are often sold and used in low- and middleincome countries without any evidence of effectiveness; this is
particularly true for IgM ELISAs and RDTs that show variable
performance for the diagnosis of acute leptospirosis (Goris et al.,
2013). These differences may be inuenced by the characteristics of
the population, the circulating strains, or the methodology (Banoo
et al., 2010). Therefore, test evaluations should be performed under
the range of conditions in which they are likely to be used in
practice. This will help to choose for the most appropriate test in
case of an outbreak. Participation in a program of inter-laboratory
comparison or prociency testing of rapid tests such as the one
established for MAT (Chappel et al., 2004) should help in producing
reliable and accurate results in endemic countries.
As described above, recent technological advances in the eld of
diagnostic tests could allow for the development of innovative rapid
tests in the near future, enabling online surveillance and early
outbreak warning. However, there may be few organizations
interested in investing in the development of RDTs for neglected
tropical diseases because of a perceived lack of return of investment
from low- and middle-income countries; these are not considered a
viable commercial market.
One major goal is to develop rapid multiplex tests (PCR- or
antibody-based methods) that will differentiate between, for example, leptospirosis and dengue or other similar major infectious
diseases. Use of multiplex tests will be very helpful in tropical
countries and could lead to improved patient outcomes. Supporting
the development of rapid tests has been dened as a priority by the
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
Global Leptospirosis Environmental Action Network (GLEAN). GLEAN
was developed by WHO and the Health and Climate Foundation to
strengthen current public health strategies and to mitigate the risk
and impact of leptospirosis outbreaks in populations at high risk
through a cross-sectorial, multidisciplinary approach (http://www.
glean-lepto.org). GLEAN aims include the denition of the challenges
and needs in terms of research and development for rapid testing as
well as the evaluation of the performance of the tests currently
available or under development with the setup of a globally
representative bank of sera. GLEAN also promotes innovative
mechanisms to support research and development of new diagnostic
tools suitable for various aspects of leptospirosis from environmental
monitoring to diagnosis and public health impact assessments.
Acknowledgments
The authors would like to thank all participants of the GLEAN
meetings for their fruitful discussions.
This work is part of the deliverables of the working group Detect
of GLEAN, which main purpose is to help countries in developing and
implementing policies and tools for early outbreak detection, with a
focus on surveillance and diagnostics.
References
Agampodi SB, Matthias MA, Moreno AC, Vinetz JM. Utility of quantitative polymerase
chain reaction in leptospirosis diagnosis: association of level of leptospiremia and
clinical manifestations in Sri Lanka. Clin Infect Dis 2012;54(9):124955. [available
from: PM:22354922].
Agampodi SB, Peacock SJ, Thevanesam V, Nugegoda DB, Smythe L, Thaipadungpanit J,
Craig SB, Burns MA, Dohnt M, Boonsilp S, Senaratne T, Kumara A, Palihawadana P,
Perera S, Vinetz JM. Leptospirosis outbreak in Sri Lanka in 2008: lessons for
assessing the global burden of disease. Am J Trop Med Hyg 2011;85(3):4718.
[available from: PM:21896807?].
Ahmed A, Klaassen HLMB, Van der Veen M, Van der Linden H, Goris MGA, Hartskeerl
RA. Evaluation of real-time PCR and culturing for the detection of leptospires in
canine samples. Advances in Microbiology 2012;2(2):16270.
Ahmed A, Anthony RM, Hartskeerl RA. A simple and rapid molecular method for
Leptospira species identication. Infect Genet Evol 2010;10(7):95562. [available
from: PM:20547247].
Ahmed A, Engelberts MF, Boer KR, Ahmed N, Hartskeerl RA. Development and
validation of a real-time PCR for detection of pathogenic leptospira species in
clinical materials. PLoS One 2009;4(9):e7093. [available from: PM:19763264].
Amilasan AS, Ujiie M, Suzuki M, Salva E, Belo MC, Koizumi N, Yoshimatsu K, Schmidt
WP, Marte S, Dimaano EM, Villarama JB, Ariyoshi K. Outbreak of leptospirosis after
ood, the Philippines, 2009. Emerg Infect Dis 2012;18(1):914. [available from:
PM:22257492].
Andreescu N. A new prepatory method of thermically inactivated Leptospira Patoc
antigen for rapid slide agglutination used as serosurvey test for human leptospiroses.
Arch Roum Pathol Exp Microbiol 1990;49(3):2237. [available from: PM:2134149].
Appassakij H, Silpapojakul K, Wansit R, Woodtayakorn J. Evaluation of the immunouorescent antibody test for the diagnosis of human leptospirosis. Am J Trop Med
Hyg 1995;52(4):3403. [available from: PM:7741173].
Arimitsu Y, Kmety E, Ananyina Y, Baranton G, Ferguson IR, Smythe L, Terpstra WJ.
Evaluation of the one-point microcapsule agglutination test for diagnosis of
leptospirosis. Bull World Health Organ 1994;72(3):3959. [available from: PM:
8062397].
Arimitsu Y, Kobayashi S, Akama K, Matuhasi T. Development of a simple serological
method for diagnosing leptospirosis: a microcapsule agglutination test. J Clin
Microbiol 1982;15(5):83541. [available from: PM:7096558].
Aviat F, Rochereau-Roulet S, Branger C, Estavoyer JM, Chatrenet B, Orsonneau JL, Thorin
C, Andre-Fontaine G. Synthetic peptide issued from Hap1/LipL32 for new early
serodiagnosis of human leptospirosis. Comp Immunol Microbiol Infect Dis
2010;33(5):37587. [available from: PM:19307019].
Bajani MD, Ashford DA, Bragg SL, Woods CW, Aye T, Spiegel RA, Plikaytis BD, Perkins BA,
Phelan M, Levett PN, Weyant RS. Evaluation of four commercially available rapid
serologic tests for diagnosis of leptospirosis. J Clin Microbiol 2003;41(2):8039.
[available from: PM:12574287].
Banoo S, Bell D, Bossuyt P, Herring A, Mabey D, Poole F, Smith PG, Sriram N,
Wongsrichanalai C, Linke R, O'Brien R, Perkins M, Cunningham J, Matsoso P,
Nathanson CM, Olliaro P, Peeling RW, Ramsay A. Evaluation of diagnostic tests for
infectious diseases: general principles. Nat Rev Microbiol 2010;8(12 Suppl):
S1729. [available from: PM:21548184].
Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, Levett PN, Gilman RH,
Willig MR, Gotuzzo E, Vinetz JM. Leptospirosis: a zoonotic disease of global
importance. Lancet Infect Dis 2003;3(12):75771. [available from: PM:14652202].
Bourhy P, Bremont S, Zinini F, Giry C, Picardeau M. Comparison of real-time PCR assays
for detection of pathogenic Leptospira spp. in blood and identication of variations
in target sequences. J Clin Microbiol 2011;49(6):215460. [available from: PM:
21471336].
Bourhy P, Vray M, Picardeau M. Evaluation of an in-house ELISA using the intermediate
species Leptospira fainei for diagnosis of leptospirosis. J Med Microbiol 2013;62(Pt
6):8227. [available from: PM:23493028].
Bulach DM, Zuerner RL, Wilson P, Seemann T, McGrath A, Cullen PA, Davis J, Johnson M,
Kuczek E, Alt DP, Peterson-Burch B, Coppel RL, Rood JI, Davies JK, Adler B. Genome
reduction in Leptospira borgpetersenii reects limited transmission potential. Proc
Natl Acad Sci U S A 2006;103(39):145605. [available from: PM:16973745?].
Cerqueira GM, Picardeau M. A century of Leptospira strain typing. Infect Genet Evol
2009;9(5):7608. [available from: PM:19540362].
Chang RS, Smith DJ, McComb DE, Sharp CF, Tonge JI. The use of erythrocyte sensitizing
substance in the diagnosis of leptospiroses. II. The sensitized erythrocyte lysis test.
Am J Trop Med Hyg 1957;6(1):1017. [available from: PM:13403131].
Chappel RJ, Goris M, Palmer MF, Hartskeerl RA. Impact of prociency testing on results
of the microscopic agglutination test for diagnosis of leptospirosis. J Clin Microbiol
2004;42(12):54848. [available from: PM:15583270].
Chou LF, Chen YT, Lu CW, Ko YC, Tang CY, Pan MJ, Tian YC, Chiu CH, Hung CC, Yang CW.
Sequence of Leptospira santarosai serovar Shermani genome and prediction of
virulence-associated genes. Gene 2012;511(2):36470. [available from: PM:
23041083].
Colenbrander AC, Van Gemen B, Gravekamp C, Hartskeerl RA. Detectie van pathogene
leptospiren met behulp van NASBA [Dutch]. Ned Tijdschrift Geneeskd
1994;138(8):436.
Cumberland P, Everard CO, Levett PN. Assessment of the efcacy of an IgM-elisa and
microscopic agglutination test (MAT) in the diagnosis of acute leptospirosis. Am J
Trop Med Hyg 1999;61(5):7314. [available from: PM:10586903].
Desvars A, Gigan J, Hoarau G, Gerardin P, Favier F, Michault A. Short report:
seroprevalence of human leptospirosis in Reunion Island (Indian Ocean) assessed
by microscopic agglutination test on paper disc-absorbed whole blood. Am J Trop
Med Hyg 2011;85(6):10979. [available from: PM:22144451?].
Doungchawee G, Kositanont U, Niwetpathomwat A, Inwisai T, Sagarasaeranee P, Haake
DA. Early diagnosis of leptospirosis by immunoglobulin M immunoblot testing. Clin
Vaccine Immunol 2008;15(3):4928. [available from: PM:18184827].
Efer PV, Domen HY, Bragg SL, Aye T, Sasaki DM. Evaluation of the indirect
hemagglutination assay for diagnosis of acute leptospirosis in Hawaii. J Clin
Microbiol 2000;38(3):10814. [available from: PM:10699001].
Goarant C, Bourhy P, D'Ortenzio E, Dartevelle S, Mauron C, Soupe-Gilbert ME, BruyereOstells L, Gourinat AC, Picardeau M, Nato F, Chanteau S. Sensitivity and specicity of
a new vertical ow rapid diagnostic test for the serodiagnosis of human
leptospirosis. PLoS Negl Trop Dis 2013;7(6):e2289. [available from: PM:23826401].
Goris MGA, Leeang MMG, Loden M, Wagenaar JFP, Klatser PR, Hartskeerl RA, Boer KR.
Prospective evaluation of three rapid diagnostic tests for diagnosis of human
leptospirosis. PLoS Negl Trop Dis 2013;7(7).
Goris MGA, Boer KR, Bouman-Strijker M, Hartskeerl RH, Lucas C, Leeang MM.
Serological laboratory tests for diagnosis of human leptospirosis in patients
presenting with clinical symptoms (Protocol). Cochrane Database Syst Rev
2011(11).
Goris MGA, Leeang MMG, Boer KR, Goeijebier M, Van Gorp ECM, Wagenaar JFP,
Hartskeerl RH. Establishment of valid laboratory case denition for human
leptospirosis. J Bacteriol Parasitol 2012;3(2).
Hartskeerl RA, Collares-Pereira H, Ellis WA. Emergence, control and re-emerging
leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect
2011;17:494501.
Hull-Jackson C, Glass MB, Ari MD, Bragg SL, Branch SL, Whittington CU, Edwards CN,
Levett PN. Evaluation of a commercial latex agglutination assay for serological
diagnosis of leptospirosis. J Clin Microbiol 2006;44(5):18535. [available from: PM:
16672421].
Koizumi N, Nakajima C, Harunari T, Tanikawa T, Tokiwa T, Uchimura E, Furuya T,
Mingala CN, Villanueva MA, Ohnishi M, Suzuki Y. A new loop-mediated isothermal
amplication method for rapid, simple, and sensitive detection of Leptospira spp. in
urine. J Clin Microbiol 2012;50(6):20724. [available from: PM:22422858].
Kolk AH, van Berkel JJ, Claassens MM, Walters E, Kuijper S, Dallinga JW, van Schooten FJ.
Breath analysis as a potential diagnostic tool for tuberculosis. Int. J. Tuberc. Lung Dis
2012;16(6):77782. [available from: PM:22507235].
Kositanont U, Rugsasuk S, Leelaporn A, Phulsuksombati D, Tantitanawat S, Naigowit P.
Detection and differentiation between pathogenic and saprophytic Leptospira spp.
by multiplex polymerase chain reaction. Diagn Microbiol Infect Dis 2007;57(2):
11722. [available from: PM:17020799].
Lau CL, Smythe LD, Craig SB, Weinstein P. Climate change, ooding, urbanisation and
leptospirosis: fuelling the re? Trans R Soc Trop Med Hyg 2010;104(10):6318.
[available from: PM:20813388].
Levett PN. Leptospirosis. Clin Microbiol Rev 2001;14(2):296326. [available from: PM:
11292640].
Levett PN, Morey RE, Galloway RL, Turner DE, Steigerwalt AG, Mayer LW. Detection of
pathogenic leptospires by real-time quantitative PCR. J Med Microbiol 2005;54(Pt
1):459. [available from: PM:15591254].
Levett PN, Whittington CU. Evaluation of the indirect hemagglutination assay for
diagnosis of acute leptospirosis. J Clin Microbiol 1998;36(1):114. [available from:
PM:9431911].
Lin X, Chen Y, Lu Y, Yan J, Yan J. Application of a loop-mediated isothermal amplication
method for the detection of pathogenic Leptospira. Diagn Microbiol Infect Dis
2009;63(3):23742. [available from: PM:19070450].
Malmstrom J, Beck M, Schmidt A, Lange V, Deutsch EW, Aebersold R. Proteome-wide
cellular protein concentrations of the human pathogen Leptospira interrogans.
Nature 2009;460(7256):7625. [available from: PM:19606093].
M. Picardeau et al. / Diagnostic Microbiology and Infectious Disease 78 (2014) 18
Marin-Leon I, Perez-Lozano MJ, De Villar-Conde E, Dastis-Bendala C, Vargas-Romero J.
Prospective evaluation of the macroagglutination slide test for Leptospira.
Serodiagn Immunother Infect Dis 1997;8:1913.
McBride AJ, Athanazio DA, Reis MG, Ko AI. Leptospirosis. Curr Opin Infect Dis
2005;18(5):37686. [available from: PM:16148523].
McBride AJ, Pereira FA, da Silva ED, de Matos RB, da Silva ED, Ferreira AG, Reis MG, Ko AI.
Evaluation of the EIE-IgM-Leptospirose assay for the serodiagnosis of leptospirosis.
Acta Trop 2007;102(3):20611. [available from: PM:17618860].
McComb DE, Smith DJ, Cofn DL, MacCready RA, Chang RS. The use of erythrocyte
sensitizing substance in the diagnosis of leptospiroses. I. The sensitized erythrocyte
agglutination test. Am J Trop Med Hyg 1957;6(1):90100. [available from: PM:
13403130].
Merien F, Portnoi D, Bourhy P, Charavay F, Berlioz-Arthaud A, Baranton G. A rapid and
quantitative method for the detection of Leptospira species in human leptospirosis.
FEMS Microbiol Lett 2005;249(1):13947. [PMID: 16006065].
Mori Y, Notomi T. Loop-mediated isothermal amplication (LAMP): a rapid, accurate,
and cost-effective diagnostic method for infectious diseases. J Infect Chemother
2009;15(2):629. [available from: PM:19396514].
Nabity SA, Ribeiro GS, Aquino CL, Takahashi D, Damiao AO, Goncalves AH, MirandaFilho DB, Greenwald R, Esfandiari J, Lyashchenko KP, Reis MG, Medeiros MA, Ko AI.
Accuracy of a dual path platform (DPP) assay for the rapid point-of-care diagnosis
of human leptospirosis. PLoS Negl Trop Dis 2012;6(11):e1878. [available from: PM:
23133686].
Perez J, Goarant C. Rapid Leptospira identication by direct sequencing of the diagnostic
PCR products in New Caledonia. BMC Microbiol 2010;10:325. [available from: PM:
21176235].
Picardeau M, Bulach DM, Bouchier C, Zuerner RL, Zidane N, Wilson PJ, Creno S, Kuczek
ES, Bommezzadri S, Davis JC, McGrath A, Johnson MJ, Boursaux-Eude C, Seemann T,
Rouy Z, Coppel RL, Rood JI, Lajus A, Davies JK, Medigue C, Adler B. Genome sequence
of the saprophyte Leptospira biexa provides insights into the evolution of
Leptospira and the pathogenesis of leptospirosis. PLoS One 2008;3(2):1607.
[available from: PM:18270594].
Ren SX, Fu G, Jiang XG, Zeng R, Miao YG, Xu H, Zhang YX, Xiong H, Lu G, Lu LF, Jiang HQ,
Jia J, Tu YF, Jiang JX, Gu WY, Zhang YQ, Cai Z, Sheng HH, Yin HF, Zhang Y, Zhu GF,
Wan M, Huang HL, Qian Z, Wang SY, Ma W, Yao ZJ, Shen Y, Qiang BQ, Xia QC, Guo
XK, Danchin A, Saint GI, Somerville RL, Wen YM, Shi MH, Chen Z, Xu JG, Zhao GP.
Unique physiological and pathogenic features of Leptospira interrogans revealed by
whole-genome sequencing. Nature 2003;422(6934):88893. [available from: PM:
12712204].
Ricaldi JN, Fouts DE, Selengut JD, Harkins DM, Patra KP, Moreno A, Lehmann JS, Purushe
J, Sanka R, Torres M, Webster NJ, Vinetz JM, Matthias MA. Whole genome analysis of
Leptospira licerasiae provides insight into leptospiral evolution and pathogenicity.
PLoS Negl Trop Dis 2012;6(10):1853. [available from: PM:23145189].
Rickerby DG, Skouloudis AN. Biosensor Networks for Monitoring Water Pollution. 2011
IEEE Global Humanitarian Technology Conference; 2011. p. 27682.
Saengjaruk P, Chaicumpa W, Watt G, Bunyaraksyotin G, Wuthiekanun V, Tapchaisri P,
Sittinont C, Panaphut T, Tomanakan K, Sakolvaree Y, Chongsa-Nguan M,
Mahakunkijcharoen Y, Kalambaheti T, Naigowit P, Wambangco MA, Kurazono H,
Hayashi H. Diagnosis of human leptospirosis by monoclonal antibody-based
antigen detection in urine. J Clin Microbiol 2002;40(2):4809. [available from: PM:
11825960].
Schreier S, Doungchawee G, Triampo D, Wangroongsarb P, Hartskeerl RA, Triampo W.
Development of a magnetic bead uorescence microscopy immunoassay to detect
and quantify Leptospira in environmental water samples. Acta Trop 2012;122(1):
11925. [available from: PM:22245149].
Segura ER, Ganoza CA, Campos K, Ricaldi JN, Torres S, Silva H, Cespedes MJ, Matthias
MA, Swancutt MA, Lopez LR, Gotuzzo E, Guerra H, Gilman RH, Vinetz JM. Clinical
spectrum of pulmonary involvement in leptospirosis in a region of endemicity,
with quantication of leptospiral burden. Clin Infect Dis 2005;40(3):34351.
[available from: PM:15668855].
Sehgal SC, Vijayachari P, Sugunan AP, Umapathi T. Field application of Lepto lateral ow
for rapid diagnosis of leptospirosis. J Med Microbiol 2003;52(Pt 10):897901.
[available from: PM:12972585].
Signorini ML, Lottersberger J, Tarabla HD, Vanasco NB. Enzyme-linked immunosorbent
assay to diagnose human leptospirosis: a meta-analysis of the published literature.
Epidemiol Infect 2013;141(1):2232. [available from: PM:22953720].
Silva MV, Camargo ED, Batista L, Vaz AJ, Brandao AP, Nakamura PM, Negrao JM.
Behaviour of specic IgM, IgG and IgA class antibodies in human leptospirosis
during the acute phase of the disease and during convalescence. J. Trop. Med. Hyg.
1995;98(4):26872. [available from: PM:7636924].
Slack A, Symonds M, Dohnt M, Harris C, Brookes D, Smythe L. Evaluation of a modied
Taqman assay detecting pathogenic Leptospira spp. against culture and Leptospiraspecic IgM enzyme-linked immunosorbent assay in a clinical environment. Diagn
Microbiol Infect Dis 2007;57(4):3616. [available from: PM:17188447].
Slack AT, Symonds ML, Dohnt MF, Smythe LD. Identication of pathogenic Leptospira
species by conventional or real-time PCR and sequencing of the DNA gyrase subunit
B encoding gene. BMC Microbiol 2006;6:95. [available from: PM:17067399].
Smits HL, Eapen CK, Sugathan S, Kuriakose M, Gasem MH, Yersin C, Sasaki D, Pujianto B,
Vestering M, Abdoel TH, Gussenhoven GC. Lateral-ow assay for rapid serodiagnosis of human leptospirosis. Clin Diagn Lab Immunol 2001;8(1):1669. [available
from: PM:11139212].
Smythe LD, Smith IL, Smith GA, Dohnt MF, Symonds ML, Barnett LJ, McKay DB. A
quantitative PCR (TaqMan) assay for pathogenic Leptospira spp. BMC Infect Dis
2002;2:13. [available from: PM:12100734].
Sonthayanon P, Chierakul W, Wuthiekanun V, Thaipadungpanit J, Kalambaheti T,
Boonsilp S, Amornchai P, Smythe LD, Limmathurotsakul D, Day NP, Peacock SJ.
Accuracy of loop-mediated isothermal amplication for diagnosis of human
leptospirosis in Thailand. Am J Trop Med Hyg 2011;84(4):61420. [available
from: PM:21460019].
Stoddard RA, Gee JE, Wilkins PP, McCaustland K, Hoffmaster AR. Detection of pathogenic
Leptospira spp. through TaqMan polymerase chain reaction targeting the LipL32 gene.
Diagn Microbiol Infect Dis 2009;64(3):24755. [available from: PM:19395218].
Taylor MJ, Ellis WA, Montgomery JM, Yan KT, McDowell SW, Mackie DP. Magnetic
immuno capture PCR assay (MIPA): detection of Leptospira borgpetersenii serovar
hardjo. Vet Microbiol 1997;56(12):13545. [available from: PM:9228689].
Thaipadungpanit J, Chierakul W, Wuthiekanun V, Limmathurotsakul D, Amornchai P,
Boonslip S, Smythe LD, Limpaiboon R, Hoffmaster AR, Day NP, Peacock SJ.
Diagnostic accuracy of real-time PCR assays targeting 16S rRNA and lipL32 genes
for human leptospirosis in Thailand: a casecontrol study. PLoS One 2011;6(1):
e16236. [available from: PM:21283633].
Truccolo J, Serais O, Merien F, Perolat P. Following the course of human leptospirosis:
evidence of a critical threshold for the vital prognosis using a quantitative PCR
assay. FEMS Microbiol Lett 2001;204(2):31721. [available from: PM:11731142].
Vijayachari P, Sugunan AP, Umapathi T, Sehgal SC. Evaluation of darkground
microscopy as a rapid diagnostic procedure in leptospirosis. Indian J Med Res
2001;114:548. [available from: PM:11785451].
Villumsen S, Pedersen R, Borre MB, Ahrens P, Jensen JS, Krogfelt KA. Novel TaqMan(R) PCR
for detection of Leptospira species in urine and blood: pit-falls of in silico validation.
J Microbiol Methods 2012;91(1):18490. [available from: PM:22750039].
Wolff JW, Bohlander HJ. Evaluation of Galton's macroscopic slide test for the
serodiagnosis of leptospirosis in human serum samples. Ann Soc Belges Med
Trop Parasitol Mycol 1966;46(1):12333. [available from: PM:5945743].
World Health Organization 2003. Human leptospirosis: guidance for diagnosis,
surveillance and control.
You might also like
- Project Title: Multiplexed Point-of-Care Test For Acute Febrile Illness (mPOCT) Project SummaryDocument2 pagesProject Title: Multiplexed Point-of-Care Test For Acute Febrile Illness (mPOCT) Project SummaryRukhsanaNo ratings yet
- 3 - Indentify Serotype DengueDocument11 pages3 - Indentify Serotype DengueBùi Thanh TùngNo ratings yet
- Detection of Typhoid CarriersDocument6 pagesDetection of Typhoid CarriersClarestaNo ratings yet
- Culturing of Microbiology Specimens in LaboratoriesDocument100 pagesCulturing of Microbiology Specimens in Laboratoriestummalapalli venkateswara raoNo ratings yet
- Laboratory Diagnosis of Infectious Diseases GuidelineDocument100 pagesLaboratory Diagnosis of Infectious Diseases GuidelineGalo PinosNo ratings yet
- Applications of Molecular Diagnostic Techniques For Infectious DiseasesDocument9 pagesApplications of Molecular Diagnostic Techniques For Infectious DiseasesKaily TrầnNo ratings yet
- Antibody Tests in Detecting SARS-CoV-2 MetanalisisDocument18 pagesAntibody Tests in Detecting SARS-CoV-2 MetanalisisRenato DesideriNo ratings yet
- Diagnostic Techniques For Inflammatory Eye Disease: Past, Present and Future: A ReviewDocument10 pagesDiagnostic Techniques For Inflammatory Eye Disease: Past, Present and Future: A ReviewAyu Ersya WindiraNo ratings yet
- Guidelines For The Diagnosis of Human Leptospirosis: June 2018Document21 pagesGuidelines For The Diagnosis of Human Leptospirosis: June 2018Heeyeon BaeNo ratings yet
- LeptospirosisDocument4 pagesLeptospirosisasril111No ratings yet
- COVID-19 Testing: A Reflection On Test Accuracy in The Real WorldDocument34 pagesCOVID-19 Testing: A Reflection On Test Accuracy in The Real Worldjoeboots78No ratings yet
- PARASITIC INFECTIONS (Why We Need Better Diagnostic Approaches)Document2 pagesPARASITIC INFECTIONS (Why We Need Better Diagnostic Approaches)tummalapalli venkateswara raoNo ratings yet
- Plasma Biomarkers To Detect Prevalent, or Predict Progressive, HIV-1-associated TuberculosisDocument21 pagesPlasma Biomarkers To Detect Prevalent, or Predict Progressive, HIV-1-associated TuberculosisPaulo MattosNo ratings yet
- Analytical Performance of COVID-19 Detection Methods (RT-PCR) : Scientific and Societal ConcernsDocument16 pagesAnalytical Performance of COVID-19 Detection Methods (RT-PCR) : Scientific and Societal ConcernsFre mobileNo ratings yet
- Ofad 120Document4 pagesOfad 120helderjamsNo ratings yet
- Journal of Infection and Public HealthDocument7 pagesJournal of Infection and Public HealthFajar Cah BumiayuNo ratings yet
- Lepto ChennaiDocument17 pagesLepto ChennaiRisma J AsifNo ratings yet
- HHS Public Access: The Role of Rapid Diagnostics in Managing Ebola EpidemicsDocument20 pagesHHS Public Access: The Role of Rapid Diagnostics in Managing Ebola Epidemicssri wahyuniNo ratings yet
- tmp6DB9 TMPDocument8 pagestmp6DB9 TMPFrontiersNo ratings yet
- International Journal For Parasitology: Birgit Nikolay, Simon J. Brooker, Rachel L. PullanDocument10 pagesInternational Journal For Parasitology: Birgit Nikolay, Simon J. Brooker, Rachel L. PullanValdy Najib BarmaNo ratings yet
- Basic Problems of Serological Laboratory DiagnosisDocument37 pagesBasic Problems of Serological Laboratory DiagnosisSuzan MatarNo ratings yet
- JBB2012 151967Document13 pagesJBB2012 151967Prodia Central Java RegionNo ratings yet
- TRZ 068Document8 pagesTRZ 068salsabilapraninditaNo ratings yet
- UNICEF Annual ReportDocument15 pagesUNICEF Annual ReportraissametasariNo ratings yet
- Natural history of disease and levels of preventionDocument9 pagesNatural history of disease and levels of preventionFarah FarahNo ratings yet
- Jurnal 2Document16 pagesJurnal 2grace liwantoNo ratings yet
- Molecular and Biomarker-Based Diagnostics in Early Sepsis - Current Challenges and Future Perspectives PDFDocument40 pagesMolecular and Biomarker-Based Diagnostics in Early Sepsis - Current Challenges and Future Perspectives PDFBram AjaNo ratings yet
- Biomarkers in Sepsis 2018 Critical Care ClinicsDocument14 pagesBiomarkers in Sepsis 2018 Critical Care ClinicsgiseladlrNo ratings yet
- Civ 609Document17 pagesCiv 609Descargar scribdNo ratings yet
- 1 s2.0 S1201971215000478 MainDocument5 pages1 s2.0 S1201971215000478 MainRay RamadhanNo ratings yet
- Jof 06 00216 v2Document18 pagesJof 06 00216 v2Grace Yuni Soesanti MhNo ratings yet
- Neonatal fungal infections diagnosis strategiesDocument4 pagesNeonatal fungal infections diagnosis strategiesirdinamarchsyaNo ratings yet
- Lepto SpirosDocument8 pagesLepto SpirosNisa UcilNo ratings yet
- Research ProposalDocument10 pagesResearch ProposalRuthNo ratings yet
- TRD 2021 0033Document11 pagesTRD 2021 0033Natasya elsha NadillahNo ratings yet
- Covid-19: Testing TimesDocument2 pagesCovid-19: Testing TimeshgfksqdnhcuiNo ratings yet
- Perspectives On Advances in Tuberculosis Diagnostics, Drugs, and VaccinesDocument17 pagesPerspectives On Advances in Tuberculosis Diagnostics, Drugs, and Vaccinesyenny handayani sihiteNo ratings yet
- Ijerph-18-11451 Meta Analysis StudyDocument14 pagesIjerph-18-11451 Meta Analysis StudySumit BediNo ratings yet
- Jurnal 2Document10 pagesJurnal 2GFORCE .ID.No ratings yet
- Challenges in Laboratory Diagnosis of The NovelDocument27 pagesChallenges in Laboratory Diagnosis of The NovelRidho Al Fiqri100% (1)
- JPAM Vol 14 Issue1 P 609-614Document6 pagesJPAM Vol 14 Issue1 P 609-614Tira Alfiani LaariyaNo ratings yet
- Advances and Trends in Sepsis Diagnostics PDFDocument12 pagesAdvances and Trends in Sepsis Diagnostics PDFGRAÇAS PERFUMARIANo ratings yet
- Advanced Immunology Assignment Topics and Students April 2023Document35 pagesAdvanced Immunology Assignment Topics and Students April 2023Musa GebiNo ratings yet
- Editorials: Rapid and Simple Point of Care Diagnostics For StisDocument2 pagesEditorials: Rapid and Simple Point of Care Diagnostics For StisYazdi PusadanNo ratings yet
- Emergency Response For Evaluating Sars-Cov-2 Immune Status, Seroprevalence and Convalescent Plasma in ArgentinaDocument28 pagesEmergency Response For Evaluating Sars-Cov-2 Immune Status, Seroprevalence and Convalescent Plasma in ArgentinaCesar AlonsoNo ratings yet
- Clinical Value of Serology For The Diagnosis of Strongyloidiasis in Travelers and Migrants - A 4-Year Retrospective Study Using The Bordier IVD Strongyloides Ratti ELISA AssayDocument10 pagesClinical Value of Serology For The Diagnosis of Strongyloidiasis in Travelers and Migrants - A 4-Year Retrospective Study Using The Bordier IVD Strongyloides Ratti ELISA Assaygwyneth.green.512No ratings yet
- Leptospirosissurveillance PDFDocument4 pagesLeptospirosissurveillance PDFHye GoNo ratings yet
- Who Evd His Emp 15.2 EngDocument9 pagesWho Evd His Emp 15.2 EngSergio Cabrera CalzadillaNo ratings yet
- Basic Laboratory Procedure in Clinical BacteriologyDocument175 pagesBasic Laboratory Procedure in Clinical BacteriologyWoro Hapsari WahyuningrumNo ratings yet
- M7L7B4 Direct Diagnostic Tests For Lyme DiseaseDocument6 pagesM7L7B4 Direct Diagnostic Tests For Lyme DiseaseLeocadio Alcalá MORILLASNo ratings yet
- Febridx®: A Rapid Diagnostic Test For Differentiating Bacterial and Viral Aetiologies in Acute Respiratory InfectionsDocument7 pagesFebridx®: A Rapid Diagnostic Test For Differentiating Bacterial and Viral Aetiologies in Acute Respiratory InfectionsPhạm Trịnh Công BìnhNo ratings yet
- Current State-Of-The-Art Diagnostics For Norovirus Detection - Model Approaches For Point-Of-Care AnalysisDocument12 pagesCurrent State-Of-The-Art Diagnostics For Norovirus Detection - Model Approaches For Point-Of-Care AnalysisRayhan OpuNo ratings yet
- Point-Of-Care Diagnostics For SepsisDocument13 pagesPoint-Of-Care Diagnostics For SepsisSheyla ANo ratings yet
- COVID-19 Vaccine Mechanisms and ImmunityDocument1 pageCOVID-19 Vaccine Mechanisms and ImmunityAvinash KumbharNo ratings yet
- Jose Research v2Document10 pagesJose Research v2Jose Emmanuel FranciaNo ratings yet
- International Journal of Infectious DiseasesDocument7 pagesInternational Journal of Infectious DiseasesyurikaNo ratings yet
- Evaluation of Real-Time PCR and Culturing For The Detection of Leptospires in Canine SamplesDocument9 pagesEvaluation of Real-Time PCR and Culturing For The Detection of Leptospires in Canine SamplesraviggNo ratings yet
- SARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19From EverandSARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19Rating: 3 out of 5 stars3/5 (1)
- Okamoto Et Al-2018-Journal of Hepato-Biliary-Pancreatic SciencesDocument18 pagesOkamoto Et Al-2018-Journal of Hepato-Biliary-Pancreatic SciencesSanda Puspa RiniNo ratings yet
- Cancer Epidemiol Biomarkers Prev 2009 Dennis 2665 71Document8 pagesCancer Epidemiol Biomarkers Prev 2009 Dennis 2665 71Sanda Puspa RiniNo ratings yet
- Oral Manifestations in Chronic Renal Failure Patients Attending Two Hospitals in North Karnataka, India.Document7 pagesOral Manifestations in Chronic Renal Failure Patients Attending Two Hospitals in North Karnataka, India.Sanda Puspa RiniNo ratings yet
- Severe Acute Pancreatitis - A Serious Complication of LeptospirosisDocument3 pagesSevere Acute Pancreatitis - A Serious Complication of LeptospirosisSanda Puspa RiniNo ratings yet
- EPOSpocketguide2012 (Rinosinusitis Dan Polip Nasal)Document20 pagesEPOSpocketguide2012 (Rinosinusitis Dan Polip Nasal)Sanda Puspa RiniNo ratings yet
- Accupuncture On Stroke FK UNSDocument62 pagesAccupuncture On Stroke FK UNSdavidperdana100% (1)
- Global Water WL 400Document2 pagesGlobal Water WL 400へんティ ひだやNo ratings yet
- Data Download Hgm4010n Hgm4020n Hgm4010nc Hgm4020nc Hgm4010can Hgm4020can enDocument50 pagesData Download Hgm4010n Hgm4020n Hgm4010nc Hgm4020nc Hgm4010can Hgm4020can enalstomNo ratings yet
- Ruiz Misely Ramos Arthur Diseño Implementacion Sistemas Monitoreo AnexosDocument664 pagesRuiz Misely Ramos Arthur Diseño Implementacion Sistemas Monitoreo Anexosvicjosh003778No ratings yet
- SelectedDocument69 pagesSelectedDhruvNo ratings yet
- Wichita Tension Control Systems Catalogue en 2009Document44 pagesWichita Tension Control Systems Catalogue en 2009Ali RazuNo ratings yet
- ALR030 - Alarms, Environmental Emergency, Carbon MonoxideDocument4 pagesALR030 - Alarms, Environmental Emergency, Carbon MonoxideAhmad M NsouliNo ratings yet
- Hand Gesture VocalizerDocument4 pagesHand Gesture VocalizerEditor IJTSRDNo ratings yet
- BMW 10 OBD 11Document27 pagesBMW 10 OBD 11SalisburNo ratings yet
- Ujian Akhir Semester Sensor dan TransduserDocument5 pagesUjian Akhir Semester Sensor dan TransduserKhairiBudayawanNo ratings yet
- TexRay Application Hand Book Ver1.02Document22 pagesTexRay Application Hand Book Ver1.02kuwabbNo ratings yet
- Emissions Monitoring: Technical InstructionDocument16 pagesEmissions Monitoring: Technical InstructionJuly E. Maldonado M.No ratings yet
- Manual TC 900 RiDocument3 pagesManual TC 900 RiedgardoNo ratings yet
- Introduction To Visibility and Present Weather Technology: Nic WilsonDocument19 pagesIntroduction To Visibility and Present Weather Technology: Nic WilsonMuhamad HidayatNo ratings yet
- A5e00053276 04us Ds3paDocument152 pagesA5e00053276 04us Ds3paJulio Cesar Hernandez TrujilloNo ratings yet
- 4-LD5190!1!2 Weather StationDocument28 pages4-LD5190!1!2 Weather StationdanNo ratings yet
- Basic Electronics and Communication Engineering (21ELN14/21ELN24) - Embedded Systems (Module 3)Document130 pagesBasic Electronics and Communication Engineering (21ELN14/21ELN24) - Embedded Systems (Module 3)Shrishail Bhat100% (2)
- IOT102 ProjectDocument6 pagesIOT102 Projectduybkse173484No ratings yet
- Measuring Point List - Turbine PDFDocument43 pagesMeasuring Point List - Turbine PDFKhushboo PandeyNo ratings yet
- SMC Model 4100 Series - ManualDocument2 pagesSMC Model 4100 Series - ManualJeffNo ratings yet
- Honeywell XLS50EDocument40 pagesHoneywell XLS50EAnte KrstanovićNo ratings yet
- Fixturlaser Alignment ToolsDocument12 pagesFixturlaser Alignment ToolsFathoni Putra WIjayaNo ratings yet
- Unit 1 INTRODUCTION TO MECHATRONICS SYSTEM DESIGNDocument8 pagesUnit 1 INTRODUCTION TO MECHATRONICS SYSTEM DESIGN9740177035100% (1)
- GD Connect 12 BrochureDocument8 pagesGD Connect 12 BrochureprajwalNo ratings yet
- Walchem Pump EWN-Y Series ManualDocument128 pagesWalchem Pump EWN-Y Series ManualPromagEnviro.comNo ratings yet
- Accessories - TRAMIGO - ONE - PAGERSDocument1 pageAccessories - TRAMIGO - ONE - PAGERSleandro barbosaNo ratings yet
- 809 DW1002 Getting An E01 Error Code On The ControlDocument2 pages809 DW1002 Getting An E01 Error Code On The ControlplasmapeteNo ratings yet
- MC406 electronic converter overview and specificationsDocument17 pagesMC406 electronic converter overview and specificationszaidNo ratings yet
- CP 060 en PenningvacDocument8 pagesCP 060 en PenningvacMayur ChauhanNo ratings yet
- CFD Simulation of Vented Explosion and Turbulent Flame PropagationDocument6 pagesCFD Simulation of Vented Explosion and Turbulent Flame Propagationjohn smithNo ratings yet
- Lecture 1 General Introduction To MechatronicsDocument108 pagesLecture 1 General Introduction To MechatronicsKrit JiamjirochNo ratings yet