Professional Documents
Culture Documents
Rheumatology 2013 Cramer Rheumatology Ket264
Uploaded by
PrissilmaTaniaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rheumatology 2013 Cramer Rheumatology Ket264
Uploaded by
PrissilmaTaniaCopyright:
Available Formats
Rheumatology Advance Access published August 9, 2013
RHEUMATOLOGY
53, 258, 268
Concise report
doi:10.1093/rheumatology/ket264
Yoga for rheumatic diseases: a systematic review
Holger Cramer1, Romy Lauche1, Jost Langhorst1 and Gustav Dobos1
Abstract
Objective. To evaluate the quality of evidence and the strength of recommendation for yoga as an
ancillary intervention in rheumatic diseases.
Conclusion. Based on the results of this review, only weak recommendations can be made for the
ancillary use of yoga in the management of FM syndrome, OA and RA at this point.
Key words: yoga, complementary therapies, rheumatology, rheumatoid arthritis, osteoarthritis, fibromyalgia,
carpal tunnel syndrome, review.
Introduction
Yoga is widely used by patients with a variety of rheumatic
diseases. According to the 2002 National Health Interview
Survey, patients with rheumatic diseases were 1.56 times
more likely to have practiced yoga within the last
12 months compared with the general population [1].
Deriving from ancient Indian philosophy, yoga comprises
physical exercise, relaxation and lifestyle modification [2].
In North America and Europe, yoga is most often associated with physical postures, breathing techniques and
meditation [3]. Systematic reviews have shown that yoga
seems to be a safe and effective intervention for patients
with arthritis [4] or FM [5]. However, no systematic review
has thoroughly investigated the effects of yoga on rheumatic diseases as a whole. The aim of this systematic
1
Department of Internal and Integrative Medicine, Kliniken EssenMitte, Faculty of Medicine, University of Duisburg-Essen, Essen,
Germany.
Submitted 13 March 2013; revised version accepted 20 June 2013.
Correspondence to: Holger Cramer, Kliniken Essen-Mitte, Klinik fur
Naturheilkunde und Integrative Medizin, Knappschafts-Krankenhaus,
Am Deimelsberg 34a, 45276 Essen, Germany.
E-mail: h.cramer@kliniken-essen-mitte.de
review was to evaluate the quality of available evidence
and the strength of the recommendation for yoga as
a therapeutic means in the management of rheumatic
diseases.
Methods
Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) guidelines [6] and the
recommendations of the Cochrane Collaboration [7]
were followed.
Eligibility criteria
Types of studies
Randomized controlled trials (RCTs) and randomized
crossover studies were eligible. No language restrictions
were applied.
Types of participants
Patients with rheumatic diseases (e.g. RA, OA, FM, osteoporosis, gout, lupus erythematosus, Pagets disease, PsA,
Raynauds disease, reactive arthritis, bursitis, tendinitis,
CTS, tarsal tunnel syndrome, plantar fasciitis, SpA, SSc
and vasculitis) were eligible.
! The Author 2013. Published by Oxford University Press on behalf of the British Society for Rheumatology. All rights reserved. For Permissions, please email: journals.permissions@oup.com
CLINICAL
SCIENCE
Results. Eight RCTs with a total of 559 subjects were included; two RCTs had a low risk of bias. In two
RCTs on FM syndrome, there was very low evidence for effects on pain and low evidence for effects on
disability. In three RCTs on OA, there was very low evidence for effects on pain and disability. Based on
two RCTs, very low evidence was found for effects on pain in RA. No evidence for effects on pain was
found in one RCT on CTS. No RCT explicitly reported safety data.
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
Methods. Medline/PubMed, Scopus, the Cochrane Library and IndMED were searched through February
2013. Randomized controlled trials (RCTs) comparing yoga with control interventions in patients with
rheumatic diseases were included. Two authors independently assessed the risk of bias using the
Cochrane Back Review Group risk of bias tool. The quality of evidence and the strength of the recommendation for or against yoga were graded according to the GRADE recommendations.
Holger Cramer et al.
Types of intervention
Studies that compared yoga interventions with no treatment or any active treatment were eligible. Studies were
excluded if yoga was not the main intervention but part of
a multimodal intervention. No restrictions were made regarding yoga tradition, length, frequency or duration of the
program. Co-interventions were allowed.
Types of outcome
For inclusion, RCTs had to assess at least one primary
outcome, i.e. pain intensity orfunction. Secondary outcomes included quality of life, psychological distress
and safety of the intervention.
Search methods
Data extraction and management
Data on patients, methods, interventions, control interventions, outcomes and results were extracted by two
authors independently using an a priori developed data
extraction form. Discrepancies were discussed with a
third review author until consensus was reached.
Risk of bias in individual studies
The risk of bias was assessed by two authors independently using the risk of bias tool proposed by the Cochrane
Back Review Group [8]. This tool assesses the risk of
selection bias, performance bias, attrition bias, reporting
bias and detection bias using 12 criteria (ratings: low, unclear or high risk of bias). Differences of opinion were discussed with a third review author until a consensus was
reached. Studies that met at least 6 of the 12 criteria and
had no serious flaw were rated as having a low risk of
bias. Studies that met fewer than six criteria or had a serious flaw were rated as having a high risk of bias [8].
Quality of evidence
Based on the methodological quality and the confidence
in the results, the quality of evidence for each outcome in
each specific disease was assessed according to the
GRADE recommendations as high quality, moderate quality, low quality or very low quality [9].
Strength of recommendation
Based on the direction and quality of the evidence and
the risk of undesirable effects of the intervention, the
Results
Literature search
The literature search revealed 269 non-duplicate records,
of which 250 were excluded because they were not RCTs,
did not include patients with rheumatic diseases and/or
did not include yoga as an intervention. Of 19 full texts
assessed for eligibility, 5 articles were excluded because
they were either not randomized [1013] or did not include
yoga interventions [14]. Another article was excluded that
compared yoga with yoga combined with massage [15].
Thirteen full-text articles reporting on eight RCTs were
finally included in the analysis [1628] (Fig. 1).
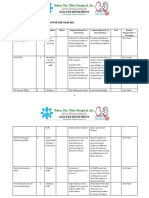
The characteristics and overall risk of bias of the
included studies are shown in Table 1. In-depth information on the characteristics and results of the included
studies can be found in supplementary Table S2, available
as supplementary data at Rheumatology Online.
Supplementary Table S3, available as supplementary
data at Rheumatology Online, shows a detailed risk of
bias assessment of the included studies. GRADE criteria
for each disease and outcome are shown in supplementary Table S4, available as supplementary data at
Rheumatology Online.
FM syndrome
An RCT with low risk of bias from the USA assessed the
effects of an 8-week Yoga of Awareness intervention
compared with usual care in 56 female FM patients
(mean age 53.7 years) [17, 18]. The yoga intervention
included yoga postures, meditation, breathing techniques
and lessons on yogic coping strategies. Outcome measures included pain, using number of tender points and
extent of tenderness, and disability, using the
Fibromyalgia Impact Questionnaire (FIQ). Significant
group differences were found for disability only; no
safety data were reported.
A second RCT originated from Brazil, had low risk of
bias and assessed the effects of a water-based breathing
yoga intervention, 60 min four times a week over a period
of 4 weeks, in 40 female FM patients (mean age 46.06
years) [26]. The intervention included breathing techniques, but no yoga postures or meditation. Both the
intervention and the control group participated in recreational activities once weekly. This RCT reported significant group differences favouring the yoga group in pain
on a visual analogue scale (VAS), disability on the FIQ and
anxiety on the Hamilton Anxiety Scale (HAS). No safety
data were reported.
Using the GRADE approach, the quality of evidence for
pain in FM syndrome was very low and the quality of evidence for disability was low. Overall, a weak recommendation can be made for the use of yoga in FM syndrome.
www.rheumatology.oxfordjournals.org
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
Medline/PubMed, Scopus, the Cochrane Library and
IndMED were searched from their inception through
11 February 2013. The complete search strategies for
each database are shown in supplementary Table S1,
available as supplementary data at Rheumatology
Online. Reference lists of identified original articles or reviews and the tables of contents of the International
Journal of Yoga Therapy and the Journal of Yoga &
Physical Therapy were searched manually. Two review
authors independently screened abstracts identified
during the literature review and potentially eligible articles
were read in full to determine whether they met the eligibility criteria.
strength of the recommendation for or against yoga as a
therapeutic option for each specific disease was judged
according to the GRADE recommendations as either
strong or weak [9].
Yoga for rheumatic diseases
FIG. 1 Flowchart of the results of the literature search.
An Indian trial with a high risk of bias included 250 patients
with OA of the knee (69.9% female; mean age 59.49
years). This RCT compared a 2-week hatha yoga intervention including yoga postures, meditation, relaxation,
breathing techniques and lectures for 40 min each day
with an aerobic exercise intervention of matched intensity
[1922]. Significant group differences were found for pain
at rest and while walking assessed on a VAS, disability on
the WOMAC, all subscales of health-related quality of life
on the Short Form 36 Health Survey (SF-36) and anxiety
on the State-Trait Anxiety Inventory (STAI). While safety
data were not included, three drop-outs due to adverse
events in the control group and none in the yoga group
were reported [1922].
An RCT from the USA included 25 patients with OA of
the interphalangeal joints. The RCT had a risk of bias. Age
ranged from 52 to 79 years and 56% were female [24].
Compared with usual care, a 10-week Iyengar yoga intervention including 60 min of yoga postures, relaxation and
education twice weekly resulted in significant group differences in hand pain during activities on a VAS but not
in pain at rest on a VAS or disability on the Stanford
Hand Assessment Questionnaire. Safety data were not
reported [24].
Originating from the USA, a third RCT compared chair
yoga (sitting meditation) twice weekly for 45 min over
8 weeks with Reiki (a spiritual healing intervention) once
weekly for 30 min over 8 weeks [27]. Twenty-one patients
with OA of different joints were included (mean age 80.0
www.rheumatology.oxfordjournals.org
years). Significant group differences were found for the
WOMAC disability scale but not for the WOMAC pain
scale or depression on the Center for Epidemiologic
Studies Depression Scale (CES-D). No safety data were
reported [27].
According to the GRADE approach, the overall quality
of evidence for effects of yoga on pain and disability in OA
was graded very low. A weak recommendation can be
made for the use of yoga in OA.
RA
An RCT with a high risk of bias from the USA compared a
6-week Iyengar yoga intervention including yoga postures
and relaxation 90 min twice weekly with usual care [23].
The RCT included 30 young women (mean age 29.9 years)
with RA. The RCT found no group differences in bodily
pain on the SF-36. Significant effects were reported for
disability using the Health Assessment Questionnaire
Disability Index (HAQ-DI) and the Pain Disability Index
(PDI), for vitality and general health on the SF-36 and for
distress on the Brief Symptom Inventory. Safety was not
reported.
A second RCT originating from India had a high risk of
bias [28]. This RCT included 80 patients with RA (mean
age 35.08 years, 70% female). The yoga intervention
included postures, cleansing practices, breathing techniques, meditation and lifestyle advice for 90 min six
times each week for 7 weeks. Compared with usual
care, yoga significantly reduced pain on the Simple
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
OA
RA
OA of the hand
CTS
FM syndrome
OA of the hip
or knee
RA
Evans et al. [23]
Garfinkel et al. [24]
Garfinkel et al. [25]
Ide et al. [26]
Park et al. [27]
FIQ-R: Revised FIQ.
Singh et al. [28]
OA of the knee
Ebnezar et al.
[1922]
Carson et al. [17, 18] FM syndrome
Rheumatic
disease
80
29
51
40
25
30
250
56
8
4
10
12
8
Exercise,
280 min/week
Usual care
Control
intervention
Yoga, 540 min/week
Chair yoga, 90 min/week
Iyengar yoga, 90 min/week
Yoga breathing exercise,
240 min/week
Iyengar yoga, 60 min/week
6 weeks
14 weeks
10 weeks
8 weeks
5 months
2 weeks
14 weeks
Outcome
assessment
Usual care
7 weeks
Wrist splint
8 weeks
Recreational
4 weeks
activities,
60 min/week
Reiki, 30 min/week 8 weeks
Usual care
Iyengar yoga, 180 min/week Usual care
Yoga of awareness,
120 min/week
Hatha yoga, 280 min/week
Sample
Treatment
size, n duration, weeks Experimental intervention
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
Reference
TABLE 1 Characteristics of the included studies
Disability (WOMAC), depression
(CES-D)
Pain (SDPIS)
Pain (myalgic tender points), disability
(FIQ-R)
Pain (pain at rest, pain while walking
on VAS), disability (WOMAC), quality
of life (SF-36), anxiety (STAI), safety
(drop-outs)
Disability (PDI, HAQ-DI), quality of life
(SF-36), distress (BSI)
Pain (pain at rest, pain during activity
on VAS), disability (Stanford Hand
Assessment Questionnaire)
Pain (VAS)
Pain (VAS), disability (FIQ), quality
of life (SF-36), anxiety (HAS)
Outcome measures
High
High
High
Low
High
High
High
Low
Risk of
bias
Holger Cramer et al.
www.rheumatology.oxfordjournals.org
Yoga for rheumatic diseases
Descriptive Pain Intensity Scale (SDPIS). Safety data were
not reported.
Using GRADE, the quality of evidence for the effects of
yoga on pain was graded as very low. Only a weak recommendation can be made for the use of yoga in RA.
Only two RCTs had a low risk of bias. Therefore, while
the effects for FM found in this review seem to be robust
against methodological bias, the effects found for RA and
OA have to be interpreted with care.
Limitations
CTS
A US RCT with a high risk of bias included 51 CTS patients (mean age 48.08 years, 54.9% female). The RCT
compared an 8-week Iyengar yoga intervention, 90 min
twice weekly, including yoga postures and relaxation,
with a standard wrist splint [25]. As this RCT did not find
significant group differences in pain on a VAS and did not
report safety data, no recommendation can be made for
or against yoga in CTS.
Discussion
Agreements with prior systematic reviews
The findings of this review are partly in line with a prior
systematic review that found evidence of the effectiveness of yoga in improving pain and mental health in
patients with OA and RA but concluded that the heterogeneity of studies precluded preliminary conclusions [4].
Based on the same RCTs as the present review [17, 18,
26], a systematic review on meditative movement therapies for FM found evidence of the effectiveness of yoga on
pain, depression and quality of life [5]. Mainly based on
low back pain studies, two recent meta-analyses on yoga
for musculoskeletal conditions [29] or pain [30] concluded
that there was good quality evidence of effectiveness on
pain and disability. Based on the same single RCT as the
present review [25], systematic reviews on conservative
treatment of CTS concluded that there was very limited
[35] to limited [36] evidence of the effectiveness of yoga in
this condition. A recent Cochrane review statistically reanalysed this RCT and found favourable effects of yoga
on pain [37].
External and internal validity
Patients of a wide age range with rheumatic diseases
diagnosed mainly by the ACR criteria were recruited
from secondary and tertiary care centres in North and
South America and Asia. Especially in RCTs on FM and
RA, mainly female patients were included. The results of
this review therefore seem to be applicable to most patients with rheumatic diseases in clinical practice while the
small number of studies on each disease limits this interpretation. The results for FM and RA might not be fully
applicable to male patients.
www.rheumatology.oxfordjournals.org
Conclusion
Based on the results of this review, weak recommendations can be made for the ancillary use of yoga in the
management of FM syndrome, OA and RA.
Rheumatology key messages
A limited number of randomized trials have investigated yoga as a treatment for rheumatic diseases.
. Yoga might be considered as an ancillary treatment
for FM syndrome, OA and RA.
.
Funding: This work was supported by the Rut- and KlausBahlsen-Foundation.
Disclosure statement: The authors have declared no
conflicts of interest.
Supplementary data
Supplementary data are available at Rheumatology
Online.
References
1 Birdee GS, Legedza AT, Saper RB et al. Characteristics of
yoga users: results of a national survey. J Gen Intern Med
2008;23:16538.
2 Iyengar BKS. Light on yoga. New York: Schocken Books,
1966.
3 Feuerstein G. The yoga tradition. Prescott, AZ: Hohm
Press, 1998.
4 Haaz S, Bartlett SJ. Yoga for arthritis: a scoping review.
Rheum Dis Clin North Am 2011;37:3346.
5 Langhorst J, Klose P, Dobos GJ et al. Efficacy and
safety of meditative movement therapies in fibromyalgia
syndrome: a systematic review and meta-analysis of
randomized controlled trials. Rheumatol Int 2013;33:
193207.
6 Moher D, Liberati A, Tetzlaff J et al. Preferred reporting
items for systematic reviews and meta-analyses: the
PRISMA statement. Ann Intern Med 2009;151:2649.
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
This systematic review of eight RCTs on yoga for rheumatic diseases found very low to low quality evidence
for FM, very low quality evidence for OA and RA and no
evidence for CTS. While no RCT reported safety data,
prior systematic reviews on other conditions found no evidence for severe adverse events [2934]. Therefore a
weak recommendation for the use of yoga as an ancillary
intervention in FM, OA and RA can be made.
The primary limitation of this review is the small number
and low methodological quality of the included RCTs.
Only for FM syndrome were high quality RCTs available
and the evidence drawn from these studies is still limited
by the heterogeneity of interventions and outcome measures. The evidence for effects on OA is further limited by
the heterogeneity of the affected joints studied in the
included trials. As no RCT reported safety data, the recommendations for yoga have to be regarded as preliminary until the safety of the interventions is clarified.
Holger Cramer et al.
8 Furlan AD, Pennick V, Bombardier C et al. 2009 updated
method guidelines for systematic reviews in the Cochrane
Back Review Group. Spine 2009;34:192941.
22 Ebnezar J, Yogitha B. Effectiveness of yoga therapy with
the therapeutic exercises on walking pain, tenderness,
early morning stiffness and disability in osteoarthritis of the
knee jointa comparative study. J Yoga Phys Ther 2012;
2:144.
9 Guyatt GH, Oxman AD, Vist GE et al. GRADE: an emerging
consensus on rating quality of evidence and strength of
recommendations. BMJ 2008;336:9246.
23 Evans S, Moieni M, Lung K et al. Impact of Iyengar yoga
on quality of life in young women with rheumatoid arthritis.
Clin J Pain 2013.
10 Badsha H, Chhabra V, Leibman C et al. The benefits of
yoga for rheumatoid arthritis: results of a preliminary,
structured 8-week program. Rheumatol Int 2009;29:
141721.
24 Garfinkel MS, Schumacher HR Jr, Husain A et al.
Evaluation of a yoga based regimen for treatment of
osteoarthritis of the hands. J Rheumatol 1994;21:23413.
7 Higgins JPT, Green S. Cochrane handbook for systematic
reviews of interventions. West Sussex, UK: Wiley, 2010.
11 Bedekar N, Prabhu A, Shyam A et al. Comparative study
of conventional therapy and additional yogasanas for knee
rehabilitation after total knee arthroplasty. Int J Yoga 2012;
5:11822.
13 Krejci M. Yoga training application in overweight control of
seniors with arthritis/osteoarthritis. Fizjoterapia 2011;19:
38.
14 Joshi A, Mehta CS, Dave AR et al. Clinical effect of
Nirgundi Patra pinda sweda and Ashwagandhadi
Guggulu Yoga in the management of Sandhigata Vata
(Osteoarthritis). Ayu 2011;32:20712.
15 da Silva GD, Lorenzi-Filho G, Lage LV. Effects of yoga and
the addition of Tui Na in patients with fibromyalgia. J Altern
Complement Med 2007;13:110713.
16 Bhandari R, Singh V. A research paper on effect of yogic
package on rheumatic arthritis. Ind J Biomechanics 2009;
Special Issue (National Conference on Biomechanics
2009):1759.
17 Carson JW, Carson KM, Jones KD et al. A pilot
randomized controlled trial of the Yoga of Awareness
program in the management of fibromyalgia. Pain 2010;
151:5309.
18 Carson JW, Carson KM, Jones KD et al. Follow-up of yoga
of awareness for fibromyalgia: results at 3 months and
replication in the wait-list group. Clin J Pain 2012;28:
80413.
19 Ebnezar J, Nagarathna R, Bali Y et al. Effect of an
integrated approach of yoga therapy on quality of life in
osteoarthritis of the knee joint: a randomized control
study. Int J Yoga 2011;4:5563.
20 Ebnezar J, Nagarathna R, Yogitha B et al. Effects of an
integrated approach of hatha yoga therapy on functional
disability, pain, and flexibility in osteoarthritis of the knee
joint: a randomized controlled study. J Altern Complement
Med 2012;18:46372.
21 Ebnezar J, Nagarathna R, Yogitha B et al. Effect of
integrated yoga therapy on pain, morning stiffness and
anxiety in osteoarthritis of the knee joint: a randomized
control study. Int J Yoga 2012;5:2836.
26 Ide MR, Laurindo IMM, Rodrigue AL et al. Effect of aquatic
respiratory exercise-based program in patients with
fibromyalgia. Int J Rheumat Dis 2008;11:13140.
27 Park J, McCaffrey R, Dunn D et al. Managing osteoarthritis: comparisons of chair yoga, Reiki, and education
(pilot study). Holist Nurs Pract 2011;25:31626.
28 Singh VK, Bhandari RB, Rana BB. Effect of yogic package
on rheumatoid arthritis. Indian J Physiol Pharmacol 2011;
55:32935.
29 Ward L, Stebbings S, Cherkin D et al. Yoga for functional
ability, pain and psychosocial outcomes in musculoskeletal conditions: a systematic review and meta-analysis.
Musculoskeletal Care 2013.
30 Bussing A, Ostermann T, Ludtke R et al. Effects of yoga
interventions on pain and pain-associated disability:
a meta-analysis. J Pain 2012;13:19.
31 Cramer H, Lange S, Klose P et al. Yoga for breast cancer
patients and survivors: a systematic review and
meta-analysis. BMC Cancer 2012;12:412.
32 Cramer H, Lauche R, Haller H et al. A systematic review
and meta-analysis of yoga for low back pain. Clin J Pain
2013;29:45060.
33 Cramer H, Lauche R, Klose P et al. Yoga for schizophrenia: a systematic review and meta-analysis. BMC
Psychiatry 2013;13:32.
34 Cramer H, Lauche R, Langhorst J et al. Effectiveness of
yoga for menopausal symptoms: a systematic review and
meta-analysis of randomized controlled trials. Evid Based
Complement Alternat Med 2012;2012:863905.
35 Goodyear-Smith F, Arroll B. What can family physicians
offer patients with carpal tunnel syndrome other than
surgery? A systematic review of nonsurgical management.
Ann Fam Med 2004;2:26773.
36 Piazzini DB, Aprile I, Ferrara PE et al. A systematic review
of conservative treatment of carpal tunnel syndrome. Clin
Rehabil 2007;21:299314.
37 Page MJ, OConnor D, Pitt V et al. Exercise and
mobilisation interventions for carpal tunnel syndrome.
Cochrane Database Syst Rev 2012;6:CD009899.
www.rheumatology.oxfordjournals.org
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 15, 2016
12 Haslock I, Monro R, Nagarathna R et al. Measuring the
effects of yoga in rheumatoid arthritis. Br J Rheumatol
1994;33:7878.
25 Garfinkel MS, Singhal A, Katz WA et al. Yoga-based
intervention for carpal tunnel syndrome: a randomized
trial. JAMA 1998;280:16013.
You might also like
- Penetrating Traumatic Brain Injury A Review of Current Evaluation Andmanagement Concepts 2155 9562 1000336Document7 pagesPenetrating Traumatic Brain Injury A Review of Current Evaluation Andmanagement Concepts 2155 9562 1000336PrissilmaTaniaNo ratings yet
- Eyes in Marfan SyndromeDocument8 pagesEyes in Marfan SyndromePrissilmaTaniaNo ratings yet
- Article Wrist Hand CTS MGT October2004 JOSPT MichlovitzDocument12 pagesArticle Wrist Hand CTS MGT October2004 JOSPT MichlovitzPrissilmaTaniaNo ratings yet
- Marfans Occular ReviewDocument3 pagesMarfans Occular ReviewPrissilmaTaniaNo ratings yet
- Article Wrist Hand CTS MGT October2004 JOSPT MichlovitzDocument12 pagesArticle Wrist Hand CTS MGT October2004 JOSPT MichlovitzPrissilmaTaniaNo ratings yet
- BR J Ophthalmol 2001 Falkner 1324 7Document5 pagesBR J Ophthalmol 2001 Falkner 1324 7PrissilmaTaniaNo ratings yet
- 0915RT Mini Cousins Wolfe YonekawaDocument5 pages0915RT Mini Cousins Wolfe YonekawaPrissilmaTaniaNo ratings yet
- BR J Ophthalmol 2015 Danis Bjophthalmol 2015 306823Document7 pagesBR J Ophthalmol 2015 Danis Bjophthalmol 2015 306823PrissilmaTaniaNo ratings yet
- Lecture 5 HMS Siklus MenstruasiDocument18 pagesLecture 5 HMS Siklus MenstruasiPrissilmaTaniaNo ratings yet
- Appendix RismanDocument45 pagesAppendix RismanPrissilmaTaniaNo ratings yet
- UK National Guideline For The Management of Pelvic Inflammatory Disease 2011 PDFDocument18 pagesUK National Guideline For The Management of Pelvic Inflammatory Disease 2011 PDFPrissilmaTaniaNo ratings yet
- 08 - GlaucomaDocument80 pages08 - GlaucomaabcdshNo ratings yet
- 084 Prissilma Tania JonardiDocument1 page084 Prissilma Tania JonardiPrissilmaTaniaNo ratings yet
- Modul 7Document31 pagesModul 7PrissilmaTaniaNo ratings yet
- Dr. H. I. Dr. H. I. Boediman Boediman,, Sp.A Sp.A (K) (K) : B Fdiii FR IlDocument49 pagesDr. H. I. Dr. H. I. Boediman Boediman,, Sp.A Sp.A (K) (K) : B Fdiii FR IlPrissilmaTaniaNo ratings yet
- Hostel Murah Di SingaporeDocument22 pagesHostel Murah Di SingaporePrissilmaTaniaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Aneurizma Bazilarke I TrombolizaDocument4 pagesAneurizma Bazilarke I TrombolizaAnja LjiljaNo ratings yet
- NRP 2015 7th Ed Update 04 2017 Claudia ReedDocument53 pagesNRP 2015 7th Ed Update 04 2017 Claudia Reeddistya.npNo ratings yet
- Kode Akses UAS Gasal 2021-2022 RegulerDocument5 pagesKode Akses UAS Gasal 2021-2022 RegulerGaluh Restuti Dyah PradwiptaNo ratings yet
- Bentuk-Bentuk Terapi KomplementerDocument21 pagesBentuk-Bentuk Terapi KomplementeraikocanNo ratings yet
- Magnification and IlluminationDocument22 pagesMagnification and Illuminationwhussien7376100% (1)
- MCQs in DentistryDocument135 pagesMCQs in Dentistryyalahopa75% (4)
- Neonatal PneumoniaDocument2 pagesNeonatal PneumoniaJustin EduardoNo ratings yet
- Chelation of Gadolinium Oxford 2009Document3 pagesChelation of Gadolinium Oxford 2009gasfgdNo ratings yet
- Daftar Pustaka Delayed SpeechDocument2 pagesDaftar Pustaka Delayed SpeechAndi Tri SutrisnoNo ratings yet
- Staff Development Plan 2023Document5 pagesStaff Development Plan 2023SSNHI Dialysis Training CenterNo ratings yet
- Body Part Assessed Technique Used Actual Finding Interpretatio N SkinDocument3 pagesBody Part Assessed Technique Used Actual Finding Interpretatio N SkinSkyerexNo ratings yet
- Non-Retentive Adhesively Retained All-Ceramic Posterior RestorationDocument13 pagesNon-Retentive Adhesively Retained All-Ceramic Posterior RestorationMarian ButunoiNo ratings yet
- 2008 Annual Report-From ILAEDocument113 pages2008 Annual Report-From ILAEarmythunder100% (2)
- Deep Neck Space InfectionDocument48 pagesDeep Neck Space InfectionhaneiyahNo ratings yet
- May 17, 2013 Strathmore TimesDocument36 pagesMay 17, 2013 Strathmore TimesStrathmore TimesNo ratings yet
- Examples For Mara EssayDocument26 pagesExamples For Mara EssayMuizzuddin Nazri100% (1)
- 2019 Afk ProtocolDocument10 pages2019 Afk Protocoldrsunny159840% (1)
- Open Sim Tutorial 1Document10 pagesOpen Sim Tutorial 1Rayanne FlorianoNo ratings yet
- Sepsis Induced CholestasisDocument12 pagesSepsis Induced CholestasisYusuf Hakim AjiNo ratings yet
- Medical Treatment For Dandruff: in This Leafl Et: 2. Before You Use Selsun ShampooDocument2 pagesMedical Treatment For Dandruff: in This Leafl Et: 2. Before You Use Selsun ShampooCharles Franklin Joseph100% (1)
- Warfarin Dosing PDFDocument3 pagesWarfarin Dosing PDFOMGStudyNo ratings yet
- Case Report PresentationDocument41 pagesCase Report PresentationlukitaniningNo ratings yet
- Biomechanics of The HipDocument12 pagesBiomechanics of The HipSimon Ocares AranguizNo ratings yet
- Lingual Frenectomy With Electrocautery: Diagnostic Assessments For Case in PointDocument5 pagesLingual Frenectomy With Electrocautery: Diagnostic Assessments For Case in PointTasneem AbdNo ratings yet
- Nurse AnesthesiaDocument3 pagesNurse Anesthesiaapi-348841675No ratings yet
- FMGE Information BulletinDocument17 pagesFMGE Information Bulletinmahesh100% (4)
- Raja Rajeshwari Medical CollegeDocument11 pagesRaja Rajeshwari Medical CollegepentagoneducationNo ratings yet
- Cerebral PalsyDocument21 pagesCerebral Palsysuryakoduri93% (14)
- Constancia VisualDocument221 pagesConstancia VisualKaren CastroNo ratings yet
- AccreditationReadiness Booklet (Version 1.0) - May 2022Document44 pagesAccreditationReadiness Booklet (Version 1.0) - May 2022Leon GuerreroNo ratings yet