Professional Documents
Culture Documents
SMART Asthma Therapy
Uploaded by
Ken WonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SMART Asthma Therapy
Uploaded by
Ken WonCopyright:
Available Formats
PRESCRIBING IN PRACTICE n
Benefits of SMART therapy
for asthma management
William M Storrar MRCP and Anoop J Chauhan PhD, FRCP
SPL
A combination ICS and LABA
in a single inhaler can
improve adherence, and
data suggest it can also
reduce frequency of severe
exacerbations.
sthma affects over 5 million patients
in the UK and has an annual treatment cost exceeding 1 billion per year.1
Poorly controlled asthma leads to significant morbidity, and results in 4.1 million
GP consultations per year and 1.1 million
work days lost. The recent confidential
enquiry, National Review of Asthma
Deaths (NRAD), highlighted a number of
deficiencies in asthma care that might be
contributing to the still significant mortality associated with asthma.2
Despite good pharmacological treatments for asthma symptoms, many
patients have symptoms that remain
poorly controlled. There are several reasons that might contribute to this that
include poor treatment adherence, under
recognition of signs and symptoms of
poor asthma control, and inappropriate
prescribing practices.
The NRAD report highlighted both
under prescribing of preventer medications
and inappropriate long-acting beta2 agonist
(LABA) prescriptions as contributory factors
in a number of the asthma deaths
reviewed. A total of 80 per cent of cases
reviewed had received fewer than 12 preventer medication prescriptions in the year
preceding their death. A total of 14 per cent
of patients who died had been prescribed
a single agent LABA at the time of death
and at least 3 per cent were on LABA
monotherapy without inhaled corticosteroid
(ICS) preventer therapy. The key recommendations associated with these findings were
that adherence to medication should be
prescriber.co.uk
Figure 1. Combination ICS and LABA in a single inhaler as maintenance and reliever therapy
routinely checked and that where LABA
bronchodilators are prescribed for people
with asthma, they should be prescribed in
a single combination inhaler with an ICS.
One possible treatment strategy that
might address both of these concerns is
the use of combination ICS and LABA in
a single inhaler as both maintenance and
reliever therapy (SMART).
There is evidence that ICS use
increases in patients who are prescribed
SMART therapy implying that SMART may
be a useful strategy to overcome poor
adherence with ICS.3 Clinical trial data
have also shown that the benefits of
SMART go beyond improved adherence
and the convenience of a single inhaler
device: reduced frequency of severe exacerbations and reduced hospitalisation
rates have been seen in SMART-treated
populations on lower ICS doses than
fixed-dose inhaler comparator groups.
The place for SMART
Guideline-based asthma management,
such as described in the British
Thoracic Society/Scottish Intercollegiate
Guidelines Network (BTS/SIGN) asthma
guideline (2014), advocates the use of
SMART therapy in patients whose asthma
remains poorly controlled despite the regPrescriber 5 April 2015 z 29
Asthma
l PRESCRIBING IN PRACTICE n
Product
ICS
LABA
Inhaler device
SMART dosing
Max daily
dose
30 day cost
equivalent
(1 puff bd)
Symbicort 200/6
Budesonide
200g
Formoterol
6g
DPI Turbohaler
12 puffs bd + up to additional
8 puffs/24hrs
12 puffs
19.00
Symbicort 100/6
Budesonide
100g
Formoterol
6g
DPI Turbohaler
12 puffs bd + up to additional
8 puffs/24hrs
12 puffs
16.50
DuoResp 200/6
Budesonide
200g
Formoterol
6g
DPI Spiromax
12 puffs bd + up to additional
8 puffs/24hrs
12 puffs
14.98
Fostair 100/6
Beclometasone Formoterol
100g
6g
MDI
2 puffs bd + up to additional
6 puffs/24hrs
10 puffs
14.66
Table 1. Combination inhaler preparations licensed for use as SMART therapy
ular use of an ICS (step 3).4 At this step,
prescription of a combination inhaler containing both ICS and LABA is recommended in order to aid treatment
compliance and ensure that the LABA is
not being taken without the ICS. Most
patients at Step 3 will be on at least two
inhalers a combination ICS/LABA
inhaler and a short-acting beta2 agonist
(SABA) inhaler so using a single inhaler
for maintenance and reliever therapy has
the additional benefit of simplifying the
treatment regimen for patients.
The pan-European INSPIRE study
(n=3415), which looked at the attitudes
and actions of asthma patients on regular
maintenance therapy, found that most
patients felt confident that they could
self-manage their asthma (88 per cent).5
Most patients wanted treatment giving
immediate relief of symptoms (90 per
cent), but were concerned about taking
too much medication when they felt well
(54 per cent). The self-control offered by
SMART therapy would be particularly suitable for this cohort of patients.
As with any symptom-directed therapy, there will be patients for whom
SMART therapy is not suitable, such as
habitual users of reliever medication and
under perceivers of asthma symptoms. It
is important that all patients being considered for SMART therapy have an
understanding of the maximum daily
allowance of additional reliever use and
it is recognised that SMART therapy is not
a treatment for all.
We would recommend that patients
on SMART therapy use an appropriate
self-management plan (see Figure 2).
prescriber.co.uk
Licensed products
Budesonide/formoterol combination
products Symbicort and more recently
DuoResp are licensed for use as SMART
therapy in adult patients (>18 years). The
beclometasone/formoterol combination
inhaler, Fostair, has also recently been
licensed for use as SMART therapy in
adult patients (>18 years).
Both combinations of ICS and LABA
are suitable for use as maintenance and
reliever therapy as they contain the LABA
formoterol. Formoterol is a potent beta2
agonist that is well suited to maintenance
and reliever therapy by virtue of its rapid
onset of action (within one to three minutes of inhalation), required for quick
symptom relief, and a lack of tolerability
issues enabling repeated dosing.
formoterol and can be prescribed as
100/6 two puffs daily in two divided
doses for maintenance with up to six additional puffs daily as required for relief of
symptoms.
It should be noted that patients
requiring 1 puff/day for the relief of
symptoms should have their maintenance treatment reviewed and escalated
if appropriate, as this would suggest that
their asthma control is sub-optimal. It is
also worth noting that Fostair, DuoResp
and Symbicort inhalers all contain 120
actuations; a patient using the maximum
daily dose for maintenance and reliever
therapy will use a Symbicort or DuoResp
inhaler in 10 days and a Fostair inhaler
in 15 days.
Product choice
Dosing
The maximum daily dose of formoterol is
72g, which limits the number of inhalations that can be used in a single day.
Symbicort SMART regimens use the
6g formulations (200/6 or 100/6).
Symbicort inhalers containing 12g are
not licensed for use as SMART. Symbicort
SMART can be prescribed as 100/6 or
200/6 two to four puffs in two divided
doses for maintenance with up to eight
additional puffs daily as required for relief
of symptoms.
DuoResp 200/6 is also licensed at
the same dose; two to four puffs in two
divided doses for maintenance with up to
eight additional puffs daily as required for
relief of symptoms. The DuoResp inhaler
containing 12g is not licensed for use as
SMART. Fostair 100/6 contains 6g of
The decision to prescribe Symbicort,
DuoResp or Fostair should take account
of the following.
Inhaler device
Symbicort and DuoResp are delivered by
dry-powder inhaler (DPI) devices.
Symbicort uses a Turbohaler device,
while DuoResp uses the breath-activated
inhaler device, Spiromax. Fostair is delivered via a metered-dose inhaler (MDI).
The MDI is compatible with spacer
devices. Patient preference for different
inhaler devices and competence at using
the device will influence choice.6
Particle size
Fostair delivers beclometasone/formoterol as an extra fine hydrofluoroalkane particle formulation, targeting
Prescriber 5 April 2015 z 31
n PRESCRIBING IN PRACTICE l Asthma
both large and small airways with
improved deposition in the smaller airways compared with the other combination inhalers. Patients with small airways
dysfunction (reduced forced expiratory
flow2575%) might benefit from Fostair targeting the smaller airways.7
Clinical evidence
In 2005, evidence was published to
support the use of budesonide/formoterol as both maintenance and
reliever medication in asthma. 8 This
double-blind, randomised controlled
trial of 2760 patients using low maintenance dose budesonide/formoterol
showed that in those patients where
SABA was replaced with budesonide/
formoterol as reliever medication there
was an increased time to first severe
exacerbation (p<0.001) resulting in a
4547 per cent lower exacerbation risk
SABA
Step 1
Mild intermittent asthma
Inhaled SABA as required for
symptom relief
compared to budesonide/formoterol
with SABA reliever.
A Cochrane Review published in
2013 assessed the efficacy and safety
of SMART (budesonide/formoterol) in
comparison with maintenance treatment
provided by combination inhalers with
higher ICS dose and SABA for relief of
symptoms.9 Four studies with a total of
9130 patients were included. All of the
studies were funded by the pharmaceutical company AstraZeneca. The review
concluded that SMART therapy reduces
the number of patients having an asthma
exacerbation requiring oral steroids and
the number requiring hospitalisation or
emergency department visit compared
with those treated with fixed-dose combination inhalers.
The mean daily dose of ICS required in
the SMART therapy group was lower than
in the fixed-dose combination inhaler
ICS
Step 2
Regular preventer therapy
Add ICS (200800g BDP or
equivalent) as regular preventer
group, suggesting that increasing the ICS
in response to symptoms, but keeping the
dose lower when stable, is more effective
and leads to lower overall ICS requirements. The review was unable to comment
on several secondary outcomes such as
lung function measures, quality of life and
asthma symptom control.
In order to address the issue of
whether SMART therapy improves asthma
control, a large post hoc analysis was carried out on five clinical trials (>12,000
patients) of budesonide/formoterol
SMART treatment.10 This concluded that
the proportion of patients achieving target
levels of current clinical control were similar or higher with SMART compared with
the same or a higher fixed-dose combination inhaler plus SABA as reliever.
A recent study that evaluated the use
of beclometasone/formoterol as SMART
therapy supporting its licence for this treat-
LABA
Step 3
Initial add-on therapy
Add LABA to ICS and continue
SABA reliever
Three single medication inhaler approach (no longer recommended)
SABA
Step 1
Mild intermittent asthma
Inhaled SABA as required for
symptom relief
ICS
Step 2
Regular preventer therapy
Add ICS (200800g BDP or
equivalent) as regular preventer
Combination ICS+LABA
Step 3
Initial add-on therapy
Add combination inhaler
ICS+LABA and continue SABA
reliever
Two inhaler approach (combination inhaler preventer and SABA reliever)
SABA
Step 1
Mild intermittent asthma
Inhaled SABA as required for
symptom relief
ICS
Step 2
Regular preventer therapy
Add ICS (200800g BDP or
equivalent) as regular preventer
SMART
Step 3
Initial add-on therapy
Use combination inhaler ICS+
formoterol LABA as single inhaler
maintenance and reliever therapy
One inhaler SMART approach (Single inhaler maintenance and reliever therapy)
Figure 2. Three approaches to inhaler medication prescription at BTS Step 3 asthma treatment; BDP = beclometasone dipropionate
32 z Prescriber 5 April 2015
prescriber.co.uk
Asthma
ment regimen extended the results seen
with budesonide/formoterol SMART.11 A
total of 1714 patients were randomised to
receive either beclometasone/formoterol
plus SABA as required or beclometasone/
formoterol plus beclometasone/formoterol
as required (up to eight inhalations per
day). Beclometasone/formoterol SMART
significantly prolonged the time to first
exacerbation (by 75 days; p=0.0003) and
significantly reduced the risk of experiencing a severe exacerbation by 36 per cent
(95% CI 18 to 51 per cent; p=0.0005).
Beclometasone/formoterol SMART
also reduced the yearly rate of severe exacerbations by 34 per cent, hospitalisations
and emergency department visits by 33
per cent and oral corticosteroid courses by
35 per cent (all p<0.001) when compared
to beclometasone/formoterol and SABA.
patients, but for selected patients there
are clear advantages.
Owing to its simplicity, the treatment
regimen may help to improve adherence
while reducing the overall ICS dose
required to achieve asthma control. This
may have an impact on long-term treatment side-effects and their associated
morbidity.
Several studies have now shown
that SMART treatment can increase the
time to first exacerbation, and reduce
the frequency of severe exacerbations
and asthma hospitalisations. Asthma
exacerbations place a significant burden on healthcare resources and
means of controlling symptoms to
improve patients quality of life while
reducing healthcare expenditure should
be embraced.
l PRESCRIBING IN PRACTICE n
3. Sovani MP, et al. Br J Gen Pract 2008;
58;3743.
4. BTS/SIGN. British guideline on the management of asthma. A national clinical guideline.
October 2014 .
5. Partridge MR, et al. BMC Pulm Med
2006;6:13.
6. Chrystyn H, Price D. Prim Care Resp J
2009;18:2439.
7. De Backer W, et al. J Aerosol Med and Pulm
Drug Deliv 2010;23:13748.
8. OByrne PM, et al. Am J Respir Crit Care Med
2005;171;12936.
9. Kew KM, et al. Cochrane Database Syst Rev
2013;12:CD009019
10. Bateman ED, et al. Respir Res
2011;12:38.
11. Papi A, et al. Lancet Respir Med
2013;1:2331.
Declaration of interests
None to declare.
Conclusion
The use of a single combination ICS and
rapid-onset LABA for maintenance and
reliever therapy in patients with moderate-to-severe asthma has a number of
attractions. It may not be suitable for all
prescriber.co.uk
References
1. asthma UK. Asthma facts and FAQs.
http://bit.ly/U5IJXI.
2. RCP. Why asthma still kills. National Review
of Asthma Deaths (NRAD). May 2014
http://bit.ly/1wVCnMy.
Dr Storrar is Senior Clinical Research
Fellow and Professor Chauhan is consultant respiratory physician at the
Queen Alexandra Hospital, Portsmouth,
UK, part of the Wessex Asthma Network
Prescriber 5 April 2015 z 33
You might also like
- Chapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingDocument3 pagesChapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingKn VelasquezNo ratings yet
- History and Examination in Obstetrics and Gynaecology Obstetrics History - Detailed History and Examination For The Assessment of Mother and Fetus, Identify Risk Factors in Them and Plan ManagementDocument29 pagesHistory and Examination in Obstetrics and Gynaecology Obstetrics History - Detailed History and Examination For The Assessment of Mother and Fetus, Identify Risk Factors in Them and Plan ManagementÅbübâkêř Äbd-ëřhēēm BãřřîNo ratings yet
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults (UPTODATE)Document17 pagesDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults (UPTODATE)Annie K.No ratings yet
- History Taking Components for Patient AssessmentDocument20 pagesHistory Taking Components for Patient AssessmentCabdisacid yasinNo ratings yet
- STEMIDocument36 pagesSTEMIYellyasta Siusiu ImranNo ratings yet
- Adult Soap Note GuideDocument5 pagesAdult Soap Note Guidelizdp21No ratings yet
- Common Procedures in Paediatric IcuDocument17 pagesCommon Procedures in Paediatric IcuNeethu Mariya MathewNo ratings yet
- Diagnosis of ShockDocument9 pagesDiagnosis of ShockRejina RavindranNo ratings yet
- Leopando Hospice-Palliative3Document2 pagesLeopando Hospice-Palliative3Judy Ignacio EclarinoNo ratings yet
- Hypertension in PregnancyDocument20 pagesHypertension in PregnancyFAMED RESIDENTS CESMED100% (1)
- Eportfolio SampleDocument46 pagesEportfolio SampleJolaine ValloNo ratings yet
- TuberculosisDocument42 pagesTuberculosisGilbertoMpakaniyeNo ratings yet
- Principals of Paediatric History Taking and Physical ExaminationDocument17 pagesPrincipals of Paediatric History Taking and Physical ExaminationKingston HoNo ratings yet
- Presented By: Henna Dhir Roll No.: RP7005A01 Regd No.: 11002446Document31 pagesPresented By: Henna Dhir Roll No.: RP7005A01 Regd No.: 11002446hennadhir2No ratings yet
- History and Physical ExaminationDocument17 pagesHistory and Physical ExaminationNur Fatima SanaaniNo ratings yet
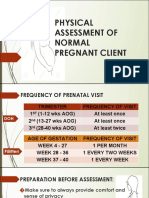
- Physical Assessment of a Pregnant ClientDocument25 pagesPhysical Assessment of a Pregnant ClientDe Leon, Austine Sydney D.No ratings yet
- Enteral Parenteral NutritionDocument80 pagesEnteral Parenteral NutritionJehangir AllamNo ratings yet
- ALD WITH ASCITES by VaibhavDocument22 pagesALD WITH ASCITES by VaibhavSandeep ChakravarthyNo ratings yet
- Pediatric Clinical ExaminationDocument37 pagesPediatric Clinical ExaminationHalema Al OkshNo ratings yet
- Junior Intern NotesDocument3 pagesJunior Intern NotesTin SumangaNo ratings yet
- 107 Rle Virtual Duty - Opd: Internal MedicineDocument6 pages107 Rle Virtual Duty - Opd: Internal MedicineGiel Margareth LindoNo ratings yet
- Tuberculosis: Therapeutics IIDocument54 pagesTuberculosis: Therapeutics IIdstu20No ratings yet
- Physician Order Sheet Format GuideDocument9 pagesPhysician Order Sheet Format GuideRoland Philip GoNo ratings yet
- Hypovolemic Shock: by DR Teh W.CDocument29 pagesHypovolemic Shock: by DR Teh W.CTeh Wai Choon100% (1)
- Patient with Eustachian Tube Dysfunction and Otitis MediaDocument5 pagesPatient with Eustachian Tube Dysfunction and Otitis MediaRenz Marion AlemaniaNo ratings yet
- Inhaler Testing BrochureDocument132 pagesInhaler Testing BrochureMathaiosVNo ratings yet
- Pediatric Tickler by RemDocument7 pagesPediatric Tickler by RemRem AlfelorNo ratings yet
- Pre-Operative Orders Post-Op Orders (Ga)Document3 pagesPre-Operative Orders Post-Op Orders (Ga)Alissandra OcampoNo ratings yet
- IM Cardiology Samplex All-In - LDocument35 pagesIM Cardiology Samplex All-In - LDeepbluexNo ratings yet
- National Guideline for Clinical Management of Dengue SyndromeDocument96 pagesNational Guideline for Clinical Management of Dengue SyndromeTapash GopeNo ratings yet
- First Line Drugs by Infection and ConditionDocument3 pagesFirst Line Drugs by Infection and ConditionKeisha Dela CernaNo ratings yet
- 19499-Enteral Parenteral NutritionDocument53 pages19499-Enteral Parenteral NutritionZunni HermawatiNo ratings yet
- Trials SummaryDocument12 pagesTrials SummaryReda SoNo ratings yet
- PEDIA ER FormularyDocument1 pagePEDIA ER FormularyAnonymous ic2CDkFNo ratings yet
- CPG PneumoniaDocument31 pagesCPG PneumoniaJo Anne100% (3)
- Carbuncle, Incision, Drainage, DebridementDocument11 pagesCarbuncle, Incision, Drainage, DebridementAlvin Germo PasuquinNo ratings yet
- TICKLER-PRINT-2 Pedia PDFDocument7 pagesTICKLER-PRINT-2 Pedia PDFCarlos H. AcuñaNo ratings yet
- Foundation Programme Curriculum 2016Document100 pagesFoundation Programme Curriculum 2016breadfanNo ratings yet
- Core Values of Family MedicineDocument68 pagesCore Values of Family MedicineJodene Rose RojasNo ratings yet
- Philippines TB CP Guidelines 2006Document151 pagesPhilippines TB CP Guidelines 2006wiltechworksNo ratings yet
- History Taking - The Critical First Step in DiagnosisDocument51 pagesHistory Taking - The Critical First Step in DiagnosisJAMES TONNY OKINYINo ratings yet
- Hypovolemic Shock & DIC (Bernabe)Document4 pagesHypovolemic Shock & DIC (Bernabe)NoreenNo ratings yet
- Action Plan PICU FINALDocument2 pagesAction Plan PICU FINALMark MacasadduNo ratings yet
- Ortho History Taking & Physical ExaminationDocument28 pagesOrtho History Taking & Physical ExaminationCabdi WaliNo ratings yet
- 1st Lecture of Respiratory Histology by DR RoomiDocument24 pages1st Lecture of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Malaysia's National Essential Drug List 3rd Ed.Document10 pagesMalaysia's National Essential Drug List 3rd Ed.afiq83No ratings yet
- Acute Circulatory FailureDocument29 pagesAcute Circulatory FailureSanthoshi Sadhanaa SankarNo ratings yet
- Guide To The Comprehensive Pediatric H and P Write Up PDFDocument16 pagesGuide To The Comprehensive Pediatric H and P Write Up PDFnanaNo ratings yet
- TB Treatment Guidelines and Anti-Tuberculosis DrugsDocument43 pagesTB Treatment Guidelines and Anti-Tuberculosis DrugsQii ishNo ratings yet
- Emergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine SulfateDocument15 pagesEmergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine Sulfate092109No ratings yet
- Sample Three: Physician and Hospital ContractDocument12 pagesSample Three: Physician and Hospital ContractMario Lopez100% (1)
- Pedia DosesDocument7 pagesPedia DosesSai Krishna MaddiralaNo ratings yet
- PEDIATRIC HISTORY AND PHYSICAL TEMPLATEDocument3 pagesPEDIATRIC HISTORY AND PHYSICAL TEMPLATELauren GrandpreNo ratings yet
- Trinx Product Catalog 2019 ENDocument64 pagesTrinx Product Catalog 2019 ENFernando BlancoNo ratings yet
- Hap VapDocument18 pagesHap VapAgita GintingNo ratings yet
- Ioc Gold StandardDocument6 pagesIoc Gold StandardjohnNo ratings yet
- H&P GuideDocument7 pagesH&P GuideTBWPNo ratings yet
- Benefits of SMART Therapy For Asthma ManagementDocument4 pagesBenefits of SMART Therapy For Asthma ManagementREDANo ratings yet
- Asthma Control SABA UseDocument9 pagesAsthma Control SABA UsemapuxdNo ratings yet
- Effective asthma management with written action plansDocument4 pagesEffective asthma management with written action plansdarkheart1804No ratings yet
- AdultDocument295 pagesAdultKen WonNo ratings yet
- Asa PSC System PDFDocument2 pagesAsa PSC System PDFKen WonNo ratings yet
- Citizen InstructDocument18 pagesCitizen InstructKen WonNo ratings yet
- Adult Ascites EnhancedDocument96 pagesAdult Ascites EnhancedPutri Rafika ZahrahNo ratings yet
- Clerkship Handbook: Family MedicineDocument51 pagesClerkship Handbook: Family MedicineKen WonNo ratings yet
- Inter-Rater Reliability PSCDocument6 pagesInter-Rater Reliability PSCKen WonNo ratings yet
- 1 S PSCDocument8 pages1 S PSCKen WonNo ratings yet
- Transition To Practice Tips 2018Document17 pagesTransition To Practice Tips 2018Ken WonNo ratings yet
- ACLS Provider Manual Supplementary Material: © 2016 American Heart AssociationDocument74 pagesACLS Provider Manual Supplementary Material: © 2016 American Heart AssociationKen WonNo ratings yet
- Canon EOS FlashWorkDocument17 pagesCanon EOS FlashWorkKeith ClintonNo ratings yet
- I 30 I 40Document27 pagesI 30 I 40Ken WonNo ratings yet
- PHQ 9Document2 pagesPHQ 9zainasgher100% (1)
- Vineyard JohnDocument321 pagesVineyard JohnKen Won0% (1)
- Form Critical Analysis Is5Document12 pagesForm Critical Analysis Is5Ken WonNo ratings yet
- Laporan Kasus BronkopneumoniaDocument30 pagesLaporan Kasus BronkopneumoniaShifa Ali JannatinNo ratings yet
- Neonatal Air Leak Syndrome and The Role Of.3Document9 pagesNeonatal Air Leak Syndrome and The Role Of.3Claudia KosztelnikNo ratings yet
- Generi Life Physician Statement FormDocument1 pageGeneri Life Physician Statement FormVennus RacraquinNo ratings yet
- Diseases of The Bone Marrow and Blood Conditions That Can Occur When The Blood-Forming Cells in The Bone Marrow Become AbnormalDocument4 pagesDiseases of The Bone Marrow and Blood Conditions That Can Occur When The Blood-Forming Cells in The Bone Marrow Become AbnormalLuqman QadirNo ratings yet
- Coronary Artery Disease (CAD) Angina Pectoris: Chapter 28: Management of Patients With CVDDocument3 pagesCoronary Artery Disease (CAD) Angina Pectoris: Chapter 28: Management of Patients With CVDLizzy WayNo ratings yet
- Immediate Life Support - NewDocument67 pagesImmediate Life Support - NewTalhaNo ratings yet
- Birth StoryDocument2 pagesBirth Storyapi-549201461No ratings yet
- Pathophysiology: Predisposing Factors: Precipitating FactorsDocument2 pagesPathophysiology: Predisposing Factors: Precipitating FactorsJemsMei Comparativo MensuradoNo ratings yet
- PolicyDocument8 pagesPolicyjoshiaruna539No ratings yet
- Vital Signs and Monitoring - Worksheet - IntermediateDocument5 pagesVital Signs and Monitoring - Worksheet - IntermediateVadim BulbakNo ratings yet
- ECSI Instructor Update 2021Document52 pagesECSI Instructor Update 2021Zach MatthewsNo ratings yet
- List of Hospitals in Delhi NCRDocument484 pagesList of Hospitals in Delhi NCRVaibhav BahetiNo ratings yet
- Faculty of Medicine and Health Sciences Score Sheet For CASE Write-UpDocument30 pagesFaculty of Medicine and Health Sciences Score Sheet For CASE Write-UpJared Khoo Er HauNo ratings yet
- Suxamethonium Apnoea Update 2003Document2 pagesSuxamethonium Apnoea Update 2003jira neaNo ratings yet
- Treatment Plan TemplatesDocument2 pagesTreatment Plan TemplatesShalini Dass100% (3)
- Types of Insulin For Diabetes TreatmentDocument2 pagesTypes of Insulin For Diabetes TreatmentKrystale Mae ValdezNo ratings yet
- DKA Protocol With Calculation SheetDocument7 pagesDKA Protocol With Calculation SheetAmanda Marie Best OsbourneNo ratings yet
- AJEERNA (Indigestion)Document37 pagesAJEERNA (Indigestion)m gouriNo ratings yet
- Personal Hygiene Habits for Better HealthDocument1 pagePersonal Hygiene Habits for Better HealthPISMP BA2100% (1)
- Ecmo TroubleshootingDocument1 pageEcmo TroubleshootingMitch ConnerNo ratings yet
- Circulatory SystemDocument21 pagesCirculatory SystemYusuf AzeezNo ratings yet
- AIAPGET 2018 analysisDocument4 pagesAIAPGET 2018 analysisarpit sachanNo ratings yet
- Mamas ReconstruccionDocument10 pagesMamas ReconstruccionDIOGENESNo ratings yet
- Andrew Eastman Resume 3Document2 pagesAndrew Eastman Resume 3api-281509868No ratings yet
- PercocetDocument2 pagesPercocetNinoska Garcia-OrtizNo ratings yet
- CH 14 Digestive-SystemDocument179 pagesCH 14 Digestive-SystemAntonio Calleja IINo ratings yet
- Umbilical Vein CatheterizationDocument3 pagesUmbilical Vein CatheterizationrohitNo ratings yet
- Mudra TherapyDocument72 pagesMudra TherapySundarskpNo ratings yet
- 6 Cognitive Behavioral Therapy Techniques For Bipolar DisorderDocument7 pages6 Cognitive Behavioral Therapy Techniques For Bipolar Disorderprabha50% (2)
- Cheatsheet PDFDocument2 pagesCheatsheet PDFJudaeo SandovalNo ratings yet