Professional Documents
Culture Documents
Inhalational Anesthetics
Uploaded by
John Christopher LucesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inhalational Anesthetics
Uploaded by
John Christopher LucesCopyright:
Available Formats
Common Features
used primarily for maintenance of anesthesia
after IV administration
Very steep dose-response curves and very
narrow therapeutic indice
Nitric oxide and volatile halogenate
hydrocarbons
Decrease cerebrovascular resistance
INHALATIONAL ANESTHETICS
Potency
Uptake and Distribution
defined quantitatively as the minimum alveolar The principal objective of inhalation anesthesia
concentration (MAC)
is a constant and optimal brain partial pressure
(Pbr) of inhaled anesthetic
MAC is the median effective dose (ED50) of the
anesthetic, expressed as the percentage of gas The partial pressure of an anesthetic gas at the
in a mixture
origin of the respiratory pathway is
required to achieve that effect
the driving force moving the anesthetic into the
alveolar space and, hence, into the blood
Potent anesthetic: LOW MAC
Less Potent: High MAC
Steady state
partial pressure n each compartment is
MAC values: compare pharmacologic effects of
equivalent to that in the inspired
different anesthetics
mixture
Increase brain perfusion
They cause bronchodilation but also decrease
both spontaneous ventilation and hypoxic
pulmonary vasoconstriction
Lipid solubility
o More lipid solube the lower
concentration needed to provde
anesthesia thus HIGHER POTENCY
Factors affecting STEADY STATE
1. Alveolar Wash-in
- replacement of normal lung gases with
inspired anesthetic mixture
- directly proportional to FRC
Inversely proportional to ventilator rate
2.
Anemia, Hypercalcemia, Hyponaterima: Decreases
MAC
Hypernatremia: Increases MAC
Brain, Heart, Liver, Kidney and Endocrine glands
Anesthetic uptake
- removal to peripheral tissue other than
brain
- uptake: product of gas solubility in blood,
cardiac output and gradient between
alveolar and blood anesthetic partial
pressure
Solubility n blood
Determined by physical property of
anesthetics
Low (Nitric Oxide)
quickly saturate blod thus faster
effect
few additional molecules to
anesthetic are required to raise
arerial anesthetic partial pssure
High (Halothane)
Dissolves more completely
Slower effect
Mechanism of Action
General Anesthesia
Increased sensitivy of GABA receptors
Increased CL influx and hyperpolarization of neurons
NO and Ketamine:
Inhibits NMDA receptors
Decrease Glutamine activators
Rapidly achieve steady state
Skeletal Muscle
Poorly perfused
Prolongs timerequired to achievesteady
state
Fats
Poorly perfused but alrge capacity to store
Prolongs required to achieve steady state
Cardiac Output
Affects removal of anesthetic to
peripheral tissues
High CO
Removes anesthetic from alveoli
faster due to increased ood flow
through lungs
Takes longer for gas to reach
equilibrium
SLOWER INDUCTION
Low CO
Speeds rateof rise of alveolar
concentration
FASTER INDUCTION
Alveolar to venous partial pressure gradient
Driving force of anesthetic delivey
Greater difference in anesthetic
concentration between alveolar and
venous blood-> Increase uptake->
Decreased Induction
NITROUS OXIDE
Only INORGANIC ANESTHETIC GAS
Colorless and odorless
Nonirritating potent analgesic but weak general anesthetic
Cant produce surgical anesthesia but is commonly combined with other more potent agent
Poorly soluble in blood-> allowing it to move rapidly in and out of the body
DIFFUSION HYPOXIA: complication due to retardation of O2 uptake during recovey
DONT depress respiration and DONT prduce muscle relaxation
Complications:
Megaloblastic anemia
Peripheral neuropathy
Pernicious anemia
Teratogenic effect
Pneumothorax
METHOXYFLURANE
MOST POTENT OF LL
LOWEST MAC
Sweet, fruity odor
HIGH SOLUBILITY
ENUFLURANE
HALOTHANE
ISOFLURANE
DESFLURANE
SEVOFLURANE
Vasopressin-resistant High-Output renal failure
Non-purgent and non-flammabe
Depresses myocardial contractility and sensitizes myocardium to epinephrine
TONIC-CLONIC SEIZURES
Rapid induction
Quick recovery
POTENT ANESTHETIC BUT WEAK ANALGESIC
POTENT BRONCHODILATOR
Used in obstetrics when uterine relaxation indicated
ADVERSE EFFECTS:
Increased Sensitivity to Catecholamines
Inhibited respiratory reflexes
Increased risk for Hepatic toxicity
Cardiac Effects
o Atropine-sensitive Bradycardia (Decrease CO)
o Cardiac Arrhytmias
o Concentration dependent hypotension (Tx: Phenylephrine)
o Malignant Hypertension (Tx: Dantrolex)
NOT TOXIC TO LIVER OR KIDNEY
DONT INDUCE CARDIAC ARRHYTHMIAS OR SENSITIZE HEART TO CATECHOLAMINES
Dose-dependent Hypotension
Stimulates Respiratory Reflexes
Corneal Steal Syndrome
o Dilatation of normal coronary arteries and divert blood away from stenotic lesions
o Regional MI during tachycardia or drops of perfusion present
GOOD BRONCHODILATOR
Purgent
Very rapid onset and recovey due to LOW blood solubility
Popular anesthetic for outpatient procedures
Stimulates respiratory reflexes-> not used for inhalational induction
Boils at rom temperature at high altitude
Auses rapid wash in and wash ot
Most commonly used because of its sweet odor
Halogenated with fluorine
Non-pungency and rapid increase in alveolar
Concentration
Excellent choice for pediatric and adult
patients
Low blood solubility
Rapid emergence
Compound A
- Fluoromethy-2,2-difluoro-1-vinyl ether)
- Nephrotoxic end product of soda lime +
Sevoflurane
o Avoid in patients with pre-existing renal dysfunction
Contraindications:
- Severe hypovolemia
- Susceptibility to malignant hyperthermia
- Intracranial hypertension
INTRAVENOUS ANESTHETICS
RAPID ONSET, SHORTER HALF-LIFE
LESSER ENVIRONMENTAL RISK vs INHALATIONAL ANESTHESIA
DESCRIPTION
INDUCTION
RECOVERY
After entering blood: % of drug binds to plasma
Primary role as induction agents
Due to redistribution from site in the CNS
proteins and the rest are free
Maintenance with total
Drug diffuses into other tissues with less bod
intravenous anesthesia
supply
Degree of protein binding
Rapid redistribution
Secondary uptake (Skeletal muscle): plasma
depends on physil characterstic of the
Shorter half lives
concentrion of the drug falls allowing the
drug
Environmental risk of
drug to diffuse out of the CNS
IONIZATION and LIPID SOLUBILITY
inhalational agents
Rapid distribution to vessel rich
High proportion of initial drug bolus is divered to the
tissues
cerebral circulation and then passes along a
concentraton gradientfrom blood into the brain
IV Non-opiods Anesthetics
Widely used to facilitate rapid
Rate of transfer:
induction of anesthesia
ARTERIAL CONCENTRATION of the FREE
High lipid solubility allows for rapid
DRUG
induction
LIPID solubility
Terminationredistribution of
Degree of Ionization
the drug into less perfused and
inactive tissues such as skeletal
muscles
and fats
Characteristics of an Ideal Intravenous
Anesthetic
Agent
EFFECT OF REDUCED CO ON ANESTHETICS
Reduced CO: body compensates by diverting
more CO to the cerebral circulation thus
GREATER PROPORTION of IV Anesthetics enters
the Cerebral circuion
SLOW TITRATION OREDUCED DOSAGE: key to
safe induction patients with Reduced CO
Thiopental and other barbiturates are
not ideal IV anesthetics because they
provide only HYPNOSIS.
The ideal IV anesthetic drug would
provide hypnosis, amnesia, analgesia
and muscle relaxation
without undesirable cardiac and
respiratory depression
Physical Properties
Soluble in water
Stable in solution
Stable to light exposure
Absence of pain on injection
No local irritation
Long shelf life
Pharmacokinetic Properties
Rapid onset of action
Ability to titrate
Predictable duration of effect
Short duration of effect
Short elimination doses half-life
Rapid recovery
Rapid biotransformation
Inactive metabolites
Nontoxic metabolites
Pharmacodynamic Properties
Reliable induction of anesthesia
Anxiolytic at sub-anesthetic doses
Analgesic at sub-anesthetic doses
Amnesic at sub-anesthetic
Minimal cardiovascular effects
High therapeutic index
Small interindividual variation
No allergy
You might also like
- Pharmacology of Anesthetic Drugs LectureDocument90 pagesPharmacology of Anesthetic Drugs LectureTefera LeteboNo ratings yet
- General AnestheticsDocument36 pagesGeneral AnestheticsnidyaNo ratings yet
- Inhalational Anaesthesia Mesi IDocument84 pagesInhalational Anaesthesia Mesi IBiserat GetnetNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- IV Induction Agents UMAIDDocument63 pagesIV Induction Agents UMAIDUmaid Mirza100% (1)
- Thyroid Disease Anesthetic ConsiderationsDocument30 pagesThyroid Disease Anesthetic Considerationssachin10dulkarNo ratings yet
- Muscle RelaxantsDocument8 pagesMuscle RelaxantsFemi AustinNo ratings yet
- Factors Affectin Block HeightDocument37 pagesFactors Affectin Block HeightshikhaNo ratings yet
- Top Drawer Drugs and Their UsesDocument63 pagesTop Drawer Drugs and Their UsesArabbetNo ratings yet
- SRNA Orientation Checklist TitleDocument40 pagesSRNA Orientation Checklist Titleihtisham1No ratings yet
- Anaesthetic Drug Crib Sheet-8Document1 pageAnaesthetic Drug Crib Sheet-8Tiarnán Byrne0% (2)
- Chapter 13 Drugs Used in Heart FailureDocument7 pagesChapter 13 Drugs Used in Heart FailureChristine Annmarie TapawanNo ratings yet
- Regional Anesthesia - FinalDocument46 pagesRegional Anesthesia - Finalvan016_bunnyNo ratings yet
- Obesity & Anaesthesia: Co-Ordinator - Dr. Chavi Sethi (MD) Speaker - Dr. Uday Pratap SinghDocument56 pagesObesity & Anaesthesia: Co-Ordinator - Dr. Chavi Sethi (MD) Speaker - Dr. Uday Pratap SinghRafi ramdhanNo ratings yet
- Anaesthesia For Thyroid Surgery....Document46 pagesAnaesthesia For Thyroid Surgery....Parvathy R NairNo ratings yet
- General anesthesia procedure, indications, and comparison to local anesthesiaDocument9 pagesGeneral anesthesia procedure, indications, and comparison to local anesthesiaRavi PatelNo ratings yet
- Rapid Seq InductionDocument6 pagesRapid Seq InductionandikszuhriNo ratings yet
- Treat Hypokalemia, Hypomagnesemia, Hypocalcemia, and HypophosphatemiaDocument20 pagesTreat Hypokalemia, Hypomagnesemia, Hypocalcemia, and Hypophosphatemiaamal.fathullahNo ratings yet
- Regional Anesthesia Notes for AppendectomyDocument5 pagesRegional Anesthesia Notes for AppendectomyBetina HernandezNo ratings yet
- Basic Practice of Anesthesiology FinalDocument70 pagesBasic Practice of Anesthesiology FinalAfiqah So JasmiNo ratings yet
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiNo ratings yet
- Electrolyte DisordersDocument10 pagesElectrolyte DisordersSlavicaNo ratings yet
- 145 One Lung VentilationDocument6 pages145 One Lung VentilationEyad AbdeljawadNo ratings yet
- Pediatric Anesthesia For StudentsDocument4 pagesPediatric Anesthesia For StudentsMarco TolentinoNo ratings yet
- Essential Concepts for Airway ManagementDocument42 pagesEssential Concepts for Airway Managementkader abdiNo ratings yet
- Pharmacology Unit 1 OverviewDocument15 pagesPharmacology Unit 1 OverviewBabita kumariNo ratings yet
- Cardiac Output Monitoring Mark VivianDocument32 pagesCardiac Output Monitoring Mark VivianpritaNo ratings yet
- Intravenous Induction AgentsDocument59 pagesIntravenous Induction Agentsroundnumber100% (1)
- Intravenous Anesthetic Agents: by Miss Maidah MehtabDocument49 pagesIntravenous Anesthetic Agents: by Miss Maidah MehtabLuqman QadirNo ratings yet
- Anaesthesia in Liver Disease PatientDocument49 pagesAnaesthesia in Liver Disease PatientVG FernandezNo ratings yet
- Epidural Anesthesia GuideDocument3 pagesEpidural Anesthesia GuidezooNo ratings yet
- Bronchial AsthmaDocument25 pagesBronchial AsthmaKamil HannaNo ratings yet
- Liver Disease in AnesthesiaDocument31 pagesLiver Disease in AnesthesiaAnnan Agyekum JoshuaNo ratings yet
- IV FluidsDocument47 pagesIV FluidsMuvenn Kannan100% (1)
- General Anaesthesia OverviewDocument21 pagesGeneral Anaesthesia OverviewKamel HadyNo ratings yet
- Fluid and Electrolyte BalanceDocument5 pagesFluid and Electrolyte BalanceBumi Zulheri HermanNo ratings yet
- Pediatric Fluid ReplacementDocument2 pagesPediatric Fluid ReplacementLori Arney100% (1)
- DrugsDocument155 pagesDrugsAkankshaNo ratings yet
- Case Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InternDocument22 pagesCase Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InterngeethaNo ratings yet
- Group 2 - ABG INTERPRETATIONDocument2 pagesGroup 2 - ABG INTERPRETATIONJilkiah Mae Alfoja CampomanesNo ratings yet
- Regional AnesthesiaDocument54 pagesRegional AnesthesiaIdza Fariha AfriNo ratings yet
- Controlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewDocument49 pagesControlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewAnn Susan MathewNo ratings yet
- Aluminium Phosphide PoisoningDocument15 pagesAluminium Phosphide PoisoningDr.Roby RajanNo ratings yet
- Liver AnesthesiaDocument141 pagesLiver Anesthesiadrimrangafoor75% (4)
- Anesthesia ManualDocument21 pagesAnesthesia ManualDocFrankNo ratings yet
- Routine Anesthesia Set UpDocument4 pagesRoutine Anesthesia Set UpSteve Johnstone100% (2)
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali sNo ratings yet
- Geriartry and AnethesiaDocument5 pagesGeriartry and AnethesiaDavidVictoriousLukasNo ratings yet
- Pharmacology of EthanolDocument5 pagesPharmacology of EthanolJoshua RemonNo ratings yet
- Post Op DeliriumDocument26 pagesPost Op DeliriumKannan GNo ratings yet
- Monitoring in AnesthesiaDocument69 pagesMonitoring in AnesthesiaGiridhar GrishNo ratings yet
- HypoxiaDocument21 pagesHypoxiaJojo RyelciusNo ratings yet
- STAGES of AnesthesiaDocument4 pagesSTAGES of AnesthesiaMabz Posadas BisnarNo ratings yet
- Onset Positions in Induction of Anesthesia Spinal Anesthesia Nitrous Oxide Respiratory Complications Respiratory ObstructionDocument7 pagesOnset Positions in Induction of Anesthesia Spinal Anesthesia Nitrous Oxide Respiratory Complications Respiratory ObstructionArvin Ian Penaflor50% (2)
- ICU Sedation and Analgesia GuideDocument10 pagesICU Sedation and Analgesia GuideAvi CNo ratings yet
- AnestheticsDocument32 pagesAnestheticsAnkit JainNo ratings yet
- Basics of AnesthesiaDocument34 pagesBasics of Anesthesiadremad1974No ratings yet
- Sedation in The ICU PulmCritDocument32 pagesSedation in The ICU PulmCritchadchimaNo ratings yet
- Pre-Operative Orders Post-Op Orders (Ga)Document3 pagesPre-Operative Orders Post-Op Orders (Ga)Alissandra OcampoNo ratings yet
- Hi-Yield Notes in Legal MedDocument16 pagesHi-Yield Notes in Legal MedJohn Christopher Luces100% (1)
- Hi-Yield Notes in PCMDocument19 pagesHi-Yield Notes in PCMJohn Christopher Luces100% (1)
- Hi-Yield Notes in SurgeryDocument18 pagesHi-Yield Notes in SurgeryJohn Christopher Luces50% (2)
- Bacteria PDFDocument13 pagesBacteria PDFJohn Christopher LucesNo ratings yet
- MediastinumDocument3 pagesMediastinumJohn Christopher LucesNo ratings yet
- Blueprint For Questions Pharmacology and Therapeutics Subject Matter Question No. Recall Applica Tion Compre HensionDocument12 pagesBlueprint For Questions Pharmacology and Therapeutics Subject Matter Question No. Recall Applica Tion Compre HensionJohn Christopher LucesNo ratings yet
- Hi-Yield Notes in Ob-GyneDocument22 pagesHi-Yield Notes in Ob-GyneJohn Christopher LucesNo ratings yet
- AnatomyDocument47 pagesAnatomyJohn Christopher LucesNo ratings yet
- Malassezia furfur clinical syndrome and treatmentDocument3 pagesMalassezia furfur clinical syndrome and treatmentJohn Christopher Luces100% (1)
- SURGERY: Schwartz's Textbook QuestionsDocument102 pagesSURGERY: Schwartz's Textbook Questionsvaegmundig100% (1)
- Jose Gianni C. Espada Clinical ClerkDocument133 pagesJose Gianni C. Espada Clinical ClerkJohn Christopher LucesNo ratings yet
- Carbo Me TabDocument46 pagesCarbo Me TabJohn Christopher LucesNo ratings yet
- Microbiology: Eukaryotes & ProkaryotesDocument7 pagesMicrobiology: Eukaryotes & ProkaryotesJohn Christopher Luces100% (1)
- SVCSDocument6 pagesSVCSJohn Christopher LucesNo ratings yet
- MediastinumDocument3 pagesMediastinumJohn Christopher LucesNo ratings yet
- Pediatrics Congenital Anomalies and Developmental MilestonesDocument14 pagesPediatrics Congenital Anomalies and Developmental MilestonesJohn Christopher LucesNo ratings yet
- Recurrent Laryngeal NerbeDocument2 pagesRecurrent Laryngeal NerbeJohn Christopher LucesNo ratings yet
- Interpret Arterial Blood Gas ResultsDocument32 pagesInterpret Arterial Blood Gas ResultsJohn Christopher LucesNo ratings yet
- Parasit OlogyDocument3 pagesParasit OlogyJohn Christopher LucesNo ratings yet
- Legal MedicineDocument7 pagesLegal MedicineJohn Christopher LucesNo ratings yet
- OB & GyneDocument24 pagesOB & GyneJohn Christopher LucesNo ratings yet
- Medfools Fungus Chart for the USMLE IDocument4 pagesMedfools Fungus Chart for the USMLE IPrashant MishraNo ratings yet
- OphthalmologyDocument2 pagesOphthalmologyJohn Christopher LucesNo ratings yet
- PathologyDocument8 pagesPathologyJohn Christopher LucesNo ratings yet
- Orthopedics PDFDocument3 pagesOrthopedics PDFJohn Christopher LucesNo ratings yet
- Psychiatry Developmental Stages and ConceptsDocument10 pagesPsychiatry Developmental Stages and ConceptsJohn Christopher LucesNo ratings yet
- Osce PediaDocument17 pagesOsce PediaJohn Christopher LucesNo ratings yet
- ANTIHISTAMINICSDocument9 pagesANTIHISTAMINICSJohn Christopher Luces100% (1)
- PhysiologyDocument19 pagesPhysiologyJohn Christopher LucesNo ratings yet
- AntidepressantsDocument2 pagesAntidepressantsJohn Christopher LucesNo ratings yet
- Caesarean Section Performing Caesarean SectionDocument13 pagesCaesarean Section Performing Caesarean SectionBlablabla BlablablaNo ratings yet
- Infection Control: Dr.T.V.Rao MD Professor of MicrobiologyDocument41 pagesInfection Control: Dr.T.V.Rao MD Professor of Microbiologytummalapalli venkateswara rao100% (1)
- Obstetric ExaminationDocument26 pagesObstetric Examinationshofa nur rahmannisaNo ratings yet
- Athletic Pubalgia (Sports Hernia) .Basu PDFDocument18 pagesAthletic Pubalgia (Sports Hernia) .Basu PDFPrabhu ashvaNo ratings yet
- General Surgery (Must Know)Document93 pagesGeneral Surgery (Must Know)Binit BharatiNo ratings yet
- Process of Elimination: Safety PrincipleDocument52 pagesProcess of Elimination: Safety Principlejennywatsurproblem100% (1)
- Work Performance of Month April 22Document3 pagesWork Performance of Month April 22Hari KiranNo ratings yet
- Region Name of LaboratoryDocument7 pagesRegion Name of LaboratorySabling DritzcNo ratings yet
- Learning Disability Eye Test LeafletDocument4 pagesLearning Disability Eye Test LeafletInclusionNorthNo ratings yet
- Covid 19 Open LetterDocument5 pagesCovid 19 Open LetterKOLD News 13No ratings yet
- Chunta 2020Document3 pagesChunta 2020intan jamaliahNo ratings yet
- Anadin Extra TabletsDocument6 pagesAnadin Extra TabletsZeynep AkıNo ratings yet
- Modified Pontic Design For Ridge DefectsDocument11 pagesModified Pontic Design For Ridge DefectsFaheemuddin MuhammadNo ratings yet
- Lippincott Williams & Wilkins Nursing Book Collection 2013: Publisher What's IncludedDocument8 pagesLippincott Williams & Wilkins Nursing Book Collection 2013: Publisher What's IncludedDasrizal0% (1)
- Multiple-Choice Questions: I Toward Self-Assessment CME. Category 1 CME Credits Not DesigDocument9 pagesMultiple-Choice Questions: I Toward Self-Assessment CME. Category 1 CME Credits Not DesigManish MauryaNo ratings yet
- Top 100 Study Items For The Otolaryngology (ENT) Board ExaminationDocument8 pagesTop 100 Study Items For The Otolaryngology (ENT) Board ExaminationsduxNo ratings yet
- Therapeutic Nursing Intervention PaperDocument10 pagesTherapeutic Nursing Intervention Paperapi-295425485No ratings yet
- Scripta Medica 46 2 English PDFDocument62 pagesScripta Medica 46 2 English PDFSinisa RisticNo ratings yet
- CH13 Ninenth Standard NCERT BOOKDocument26 pagesCH13 Ninenth Standard NCERT BOOKPrash ShanthNo ratings yet
- Hricak 2021Document37 pagesHricak 2021Xiomara CelyNo ratings yet
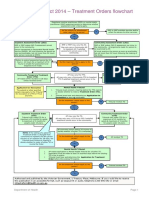
- Flowchart - Mental Health Act Treatment OrderDocument1 pageFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- Designer No Auxilio Ao Cobate Da Covid 19Document1 pageDesigner No Auxilio Ao Cobate Da Covid 19suzy luaNo ratings yet
- Emerging and Re Emerging DiseasesDocument63 pagesEmerging and Re Emerging DiseasesAljun MansalapusNo ratings yet
- A Rare Case Report: Abdominal Muscle Myoclonic JerksDocument4 pagesA Rare Case Report: Abdominal Muscle Myoclonic JerksasclepiuspdfsNo ratings yet
- Ryan Tarr RN ResumeDocument1 pageRyan Tarr RN Resumeapi-456377205No ratings yet
- Section16 - Questions and AnswersDocument62 pagesSection16 - Questions and Answersdivine venturoNo ratings yet
- Angie ResumeDocument2 pagesAngie Resumeapi-270344093No ratings yet
- Endoscopy Neo InfantsDocument490 pagesEndoscopy Neo InfantsAlexandra NechiforNo ratings yet
- 4 - Drug Product Design ParametersDocument7 pages4 - Drug Product Design ParametersVinz AlvarezNo ratings yet
- Lomitapide PDFDocument125 pagesLomitapide PDFAndrés Menéndez RojasNo ratings yet