Professional Documents
Culture Documents
Oral Vs IV
Uploaded by
rizkyswandaruOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Vs IV
Uploaded by
rizkyswandaruCopyright:
Available Formats
Oral vs IV Corticosteroids for
In-hospital Treatment of COPD
Exacerbations
course of COPD is punctuated by
T heacuteclinical
exacerbations. These have been defined as
an event in the natural course of the disease
characterized by a change in the patients baseline
dyspnea, cough and/or sputum that is beyond normal
day-to-day variation, is acute in onset and may
warrant a change in regular medication . . .1 The
worsening symptoms are accompanied by variable
decrements in lung function and worsening health
status, with improvement in dyspnea and lung function generally within 1 to 2 weeks after initiation of
treatment.2 However, the decline in health status
may persist for months or even longer in cases of
frequently recurring exacerbations,3 and frequent
exacerbations may augment the accelerated rate of
lung function decline that characterizes disease
progression in COPD.4 While most patients with
an acute exacerbation of COPD (AECOPD) are
managed as outpatients, the treatment failure rate
(requirement for intensification of therapy, unscheduled office or emergency department visits
or hospitalization) is high, and epidemiologic studies5 indicate that 15 to 22% may require hospitalization.
Hospital admissions for AECOPD have increased
in recent years; in-hospital mortality rates of approximately 10% overall have been reported,6 while
much higher rates (approximately 25%) have been
observed in patients with acute ventilatory failure requiring admission to an ICU.7 Moreover, follow-up
studies6 have revealed a mortality rate of 33% within a
year of hospitalization for AECOPD. Besides its deleterious impact on the health and survival of individual
patients, hospitalization for AECOPD is an important
societal health issue, accounting for 70% of the $18
billion in direct health-care costs for COPD in the
United States.8
Because of the serious impact of acute exacerbations, a major goal of COPD management is their
prevention and treatment. Maintenance therapy
with inhaled bronchodilators with or without inhaled
corticosteroids has been shown to be beneficial
as preventive therapy for reducing the frequency
of exacerbations.9 Regarding the management of
AECOPD, current guidelines recommend an intensification of short-acting inhaled bronchodilator therapy, antibiotics (for patients with sputum
purulence or those requiring mechanical ventilation), a 7- to 10-day course of oral corticosteroids
(30 to 40 mg/d of prednisolone) for home management, and oral or IV corticosteroids for hospital
1728
Downloaded From: http://journal.publications.chestnet.org/ on 07/03/2016
treatment.1 The recommendation of systemic corticosteroid therapy is based on evidence from
well-designed randomized controlled clinical trials
that demonstrate such benefits as shortening of
recovery time, earlier improvement in lung function, decrease in the risk of early relapse, and
reduction in the length of hospital stay. For
hospital management, both IV and oral corticosteroids have been found to be effective,10,11 with no
evidence that prolonged extension of oral therapy
(8 weeks vs 2 weeks) is more efficacious.10 What is
still unclear, however, is whether any greater
efficacy ensues from the IV vs oral route of
administration, and from higher doses (eg, 125 mg
of methylprednisolone q6h IV for the first 3
hospital days)10 than lower ones (eg, 30 mg of
prednisone po qd),11 although higher doses have
been shown to increase the risk of side effects (eg,
hyperglycemia).10
In the current issue of CHEST (see page 1741),
de Jong and colleagues12 address the first of these
two questions. They hypothesized that oral prednisolone is not inferior to IV prednisolone when
administered in bioequivalent doses (60 mg) over
5 days to patients hospitalized for management of
a severe AECOPD, followed by a gradual tapering
regimen of oral prednisolone beginning with a
dose of 30 mg/d for a total 11-day course. The
authors found that the oral and IV routes resulted
in equivalent rates of treatment failure (the primary end point, defined as death, ICU admission,
rehospitalization for COPD, or the need to intensify pharmacotherapy). Secondary outcomes were
also equivalent, including improvement in FEV1
and quality of life from the day of hospital admission and length of hospital stay. A strength of the
study is its carefully controlled, double-blind, double-dummy experimental design with stratified
allocation to the treatment arms to achieve balance between the two groups on potentially influential baseline features, so that the results are
unlikely to be confounded by differences in disease severity, preadmission therapy, or prior exacerbation history. Other strengths are the inclusion
of patients who had failed outpatient treatment
with oral corticosteroids, thereby making the results relevant to real-world clinical scenarios, and
the completeness of the follow-up data for accurate capture of treatment failures following hospital discharge. A weakness of the study, however, is
the exclusion of patients with very severe exacerbations manifested by acute ventilatory failure or
with significant comorbidities, so that the results
cannot be extrapolated to these not uncommon
subsets of patients hospitalized with a COPD
exacerbation. A surprising finding is the relatively
Editorials
high treatment failure rate in both treatment
groups at 90 days (61.7% and 56.3%), which is
higher than the failure rate at a comparable time
period in the study of Nieweoehner et al (37%).10
A subanalysis suggests that differences between
the two studies in entry criteria (the latter study
excluded patients who had used systemic corticosteroids within the preceding 30 days) probably do
not explain this discrepancy. However, the lower
treatment failure rate in the study by Niewoehner
et al10 might be attributable to the much higher
3-day initial and 15-day cumulative doses of prednisolone administered in that study (total of 1,680
mg) compared to the doses used in the current
study over 11 days (405 mg). Future carefully
designed trials will need to address the impact of
different dosing regimens of systemic corticosteroids on outcomes in patients hospitalized with an
AECOPD. Nonetheless, since doses were equivalent between the two treatment arms in the study
of de Jong et al,12 their observations of similar
efficacy in a head-to-head equivalence trial of oral
vs IV corticosteroids provide convincing support
for the more convenient and less costly oral route
in the inpatient management of AECOPD whenever oral intake is feasible.
Donald P. Tashkin, MD, FCCP
Los Angeles, CA
Dr. Taskin is Professor of Medicine, David Geffen School of
Medicine at UCLA.
The author has no conflict of interest to disclose.
Reproduction of this article is prohibited without written permission
from the American College of Chest Physicians (www.chestjournal.
org/misc/reprints.shtml).
Correspondence to: Donald P. Tashkin, MD, FCCP, Professor of
Medicine, David Geffen School of Medicine at UCLA, 10833 Le
Conte Ave, Los Angeles, CA 90095-1690; e-mail: dtashkin@
mednet.ucla.edu
DOI: 10.1378/chest.07-1622
References
1 Global initiative for chronic obstructive pulmonary disease.
Global strategy for the diagnosis, management and prevention of COPD 2006. Available at: www.goldcopd.org/
Guideline item. Accessed January 22, 2007
2 Parker CM, Voduc N, Aaron SC, et al. Physiological changes
during symptom recovery from moderate exacerbations of
COPD. Eur Respir J 2005; 26:376 378
3 Spencer S, Jones PW, GLOBE Study Group. Time course of
recovery of health status following an infective exacerbation
of chronic bronchitis. Thorax 2003; 58:589 593
4 Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002;
57:847 852
5 Celli BR, Barnes PJ. Exacerbations of chronic obstructive
pulmonary disease. Eur Respir J 2007; 29:1224 1238
6 Gunen H, Hacievliyagil SS, Kosar F, et al. Factors affecting
survival of hospitalized patients with COPD. Eur Respir J
2005; 26:234 241
www.chestjournal.org
Downloaded From: http://journal.publications.chestnet.org/ on 07/03/2016
7 Ai-Ping C, Lee K-H, Lim T-K. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of
COPD: a retrospective study. Chest 2005; 128:518 524
8 Wouters EF. Economic analysis of the Confronting COPD
survey: an overview of results. Respir Med 2003; 97(Suppl
C):S3S14
9 Sin DD, McAlister FA, Man SFP, et al. Contemporary
management of chronic obstructive pulmonary disease: scientific review. JAMA 2003; 290:23012312
10 Niewoehner DE, Erbland MC, Deupree RH, et al. Effect
of systemic glucocorticoids on exacerbations of chronic
obstructive pulmonary disease. N Engl J Med 1999; 340:
19411947
11 Davies L, Angus RM, Calverley PMA. Oral corticosteroids in
patients admitted to hospital with exacerbations of chronic
obstructive pulmonary disease: a prospective randomized
controlled trial. Lancet 1999; 354:456 460
12 de Jong YP, Uil SM, Grotjohan HP, et al. Oral or intravenous
prednisolone in the treatment of COPD exacerbations: a
randomized controlled, double-blind study. Chest 2007; 132:
17411747
Hypercapnic Obstructive Sleep
Apnea
An Underappreciated Marker of
Severity
during wakefulness is a marker of
H ypercapnia
disease severity in patients with sleep apnea.
These patients are often very obese, have long apnea
events with marked oxygen desaturation, evidence of
pulmonary hypertension, and right-heart failure.
Without appropriate treatment, such patients require frequent hospital admission1 and have alarming mortality rates.2 Fortunately, following the successful application of continuous positive airway
pressure (CPAP) or bilevel ventilation, daytime hypercapnia often improves3 and recurrent hospital
admission rates decrease.1
Unfortunately, clinicians may underestimate the
severity of illness of these patients and often miss
an opportunity to intervene. Presenting symptoms
are nonspecific and include fatigue, sleepiness,
subtle changes in mental status, and headaches.
Since there is often no increase in respiratory rate or
use of accessory muscles to breathe, their tenuous
status is not fully appreciated. Even the underlying
obstructive sleep apnea (OSA) as well as the
hypoventilation in these patients is often missed.
When oxyhemoglobin desaturation and right-heart
failure are detected, supplemental oxygen is often
provided without the knowledge of arterial blood
gas abnormalities. Therefore, these hypercapnic
patients often go unrecognized and undertreated
with high risk for recurrent hospitalization and
even early death.2
CHEST / 132 / 6 / DECEMBER, 2007
1729
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Oracle Fusion Financials Book Set Home Page SummaryDocument274 pagesOracle Fusion Financials Book Set Home Page SummaryAbhishek Agrawal100% (1)
- Trove Research Carbon Credit Demand Supply and Prices 1 June 2021Document51 pagesTrove Research Carbon Credit Demand Supply and Prices 1 June 2021Ceren ArkancanNo ratings yet
- Reaction rate determination and simulation of hydrogenation processDocument3 pagesReaction rate determination and simulation of hydrogenation processToMemNo ratings yet
- Moll000804 PDFDocument1 pageMoll000804 PDFrizkyswandaruNo ratings yet
- 5 Critical Care KuliahDocument37 pages5 Critical Care KuliahrizkyswandaruNo ratings yet
- Complication FractureDocument21 pagesComplication FractureApriyan YudhaNo ratings yet
- Allergies and Asthma TempDocument3 pagesAllergies and Asthma TempKonie LappinNo ratings yet
- Sepsis Induced CholestasisDocument12 pagesSepsis Induced CholestasisYusuf Hakim AjiNo ratings yet
- 211 Keles PDFDocument58 pages211 Keles PDFrizkyswandaruNo ratings yet
- Incidence of neonatal jaundice in PakistanDocument7 pagesIncidence of neonatal jaundice in PakistanrizkyswandaruNo ratings yet
- 1 Biology of Obesitas KuliahDocument50 pages1 Biology of Obesitas KuliahrizkyswandaruNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaLucky Arie SandiNo ratings yet
- Anxiety AlgorithmDocument4 pagesAnxiety AlgorithmrizkyswandaruNo ratings yet
- Intranasal CorticosteroidsDocument3 pagesIntranasal CorticosteroidsrizkyswandaruNo ratings yet
- ASD ADHD Brief ComparisonDocument2 pagesASD ADHD Brief ComparisonrizkyswandaruNo ratings yet
- Salter Chapter 15Document36 pagesSalter Chapter 15rizkyswandaruNo ratings yet
- Tonsil Dialiri Kelenjar Getah Bening Yang Berasal Dari Superior Deep Cervical NodesDocument5 pagesTonsil Dialiri Kelenjar Getah Bening Yang Berasal Dari Superior Deep Cervical NodesrizkyswandaruNo ratings yet
- Daftar Pustaka Low Back PainDocument1 pageDaftar Pustaka Low Back PainrizkyswandaruNo ratings yet
- FAQsprostatecancer 1Document3 pagesFAQsprostatecancer 1Human Res Human ResNo ratings yet
- ObatDocument3 pagesObatrizkyswandaruNo ratings yet
- Specific Birth Fractures & Elbow InjuriesDocument28 pagesSpecific Birth Fractures & Elbow InjuriesrizkyswandaruNo ratings yet
- Data Skor PanssDocument10 pagesData Skor PanssrizkyswandaruNo ratings yet
- Laporan Diskusi Pemicu 5-8 Kelompok Diskusi 1 Modul Foundation of Clinical PracticeDocument1 pageLaporan Diskusi Pemicu 5-8 Kelompok Diskusi 1 Modul Foundation of Clinical PracticerizkyswandaruNo ratings yet
- FAMILIES FIRST Keys To Successful Family FunctioningDocument4 pagesFAMILIES FIRST Keys To Successful Family FunctioningIuliana RamascanuNo ratings yet
- Macronutrients 240715Document48 pagesMacronutrients 240715rizkyswandaru100% (1)
- Ekspresi EmosiDocument9 pagesEkspresi EmosirizkyswandaruNo ratings yet
- WFBSP SZ Guidelines Part1 2012 Acute SchizophreniaDocument61 pagesWFBSP SZ Guidelines Part1 2012 Acute Schizophreniascabrera_scribdNo ratings yet
- OROLO & W. D. GannDocument56 pagesOROLO & W. D. GannGaurav Garg100% (1)
- RestrukturisasiDocument17 pagesRestrukturisasimuhammad hayel wallaNo ratings yet
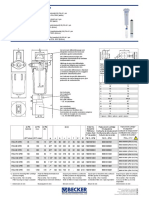
- Medical filter performance specificationsDocument1 pageMedical filter performance specificationsPT.Intidaya Dinamika SejatiNo ratings yet
- Bitcoin MambaDocument17 pagesBitcoin MambaJean MilenixNo ratings yet
- Choose the Best WordDocument7 pagesChoose the Best WordJohnny JohnnieeNo ratings yet
- 153C Final Exam Study Guide-2Document6 pages153C Final Exam Study Guide-2Soji AdimulaNo ratings yet
- DAT MAPEH 6 Final PDFDocument4 pagesDAT MAPEH 6 Final PDFMARLYN GAY EPANNo ratings yet
- EQ - Module - Cantilever MethodDocument17 pagesEQ - Module - Cantilever MethodAndrea MalateNo ratings yet
- Principles of Cost Accounting 1Document6 pagesPrinciples of Cost Accounting 1Alimamy KamaraNo ratings yet
- Trimble Oem Gnss Bro Usl 0422Document3 pagesTrimble Oem Gnss Bro Usl 0422rafaelNo ratings yet
- Sheqxel Bbs Participation Dashboard TemplateDocument39 pagesSheqxel Bbs Participation Dashboard TemplateMuhammad Adytio DarmawanNo ratings yet
- Tugas B InggrisDocument6 pagesTugas B Inggrisiqbal baleNo ratings yet
- E PortfolioDocument76 pagesE PortfolioMAGALLON ANDREWNo ratings yet
- About Version ControlDocument6 pagesAbout Version ControlMaria Kristina Cassandra HeukshorstNo ratings yet
- AC7114-2 Rev N Delta 1Document34 pagesAC7114-2 Rev N Delta 1Vijay YadavNo ratings yet
- Basic Calculus: Performance TaskDocument6 pagesBasic Calculus: Performance TasksammyNo ratings yet
- Crash Cart - General Checklist For Medical Supplies On Crash CartsDocument3 pagesCrash Cart - General Checklist For Medical Supplies On Crash CartsYassen ManiriNo ratings yet
- France: French HistoryDocument16 pagesFrance: French HistoryMyroslava MaksymtsivNo ratings yet
- Learning Online: Veletsianos, GeorgeDocument11 pagesLearning Online: Veletsianos, GeorgePsico XavierNo ratings yet
- Homo Sapiens ActivityDocument8 pagesHomo Sapiens ActivityJhon Leamarch BaliguatNo ratings yet
- R4 User GuideDocument48 pagesR4 User GuideAaron SmithNo ratings yet
- My16-Td My16-AtDocument6 pagesMy16-Td My16-AtRodrigo ChavesNo ratings yet
- D257272 1200 FDD 002 R1 PDFDocument420 pagesD257272 1200 FDD 002 R1 PDFTap Toan100% (1)
- Principles of Management NotesDocument61 pagesPrinciples of Management Notestulasinad123No ratings yet
- Power Bi ProjectsDocument15 pagesPower Bi ProjectssandeshNo ratings yet
- Policies and Regulations On EV Charging in India PPT KrishnaDocument9 pagesPolicies and Regulations On EV Charging in India PPT KrishnaSonal ChoudharyNo ratings yet
- 3.2 Probability DistributionDocument38 pages3.2 Probability Distributionyouservezeropurpose113No ratings yet