Professional Documents
Culture Documents
En - 0101 2800 JBN 36 03 0396
Uploaded by
Lanna HarumiyaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
En - 0101 2800 JBN 36 03 0396
Uploaded by
Lanna HarumiyaCopyright:
Available Formats
Update Article
Neuropsychiatric disorders and renal diseases: an update
Authors
Abstract
Silvia Mendona da Matta1
Neuropsychiatric symptoms are frequently
associated to renal dysfunction and may
compromise negatively the clinical course as
well as the quality of life, and the functional
status of the patients. The neuropsychiatric
disorders associated with renal disease may
present various forms according to the
natural history of the disease, and remain
underdiagnosed and undertreated. There
are few data in the literature regarding
the treatment of these patients, and a lot
of controversies still exist. The objective of
this paper is to describe the most frequent
neuropsychiatric disorders in patients with
renal diseases.
Janaina Matos Moreira1
Arthur Melo e Kummer1
Izabela Guimares Barbosa1
Antnio Lcio Teixeira1
Ana Cristina Simes e Silva1
Interdisciplinary Medical
Research Laboratory, School of
Medicine, Federal University of
Minas Gerais (UFMG).
1
Keywords: acute kidney injury; anxiety;
depression; kidney diseases.
(CKD) may suffer from limited
functional capacity, impaired productivity, and reduced quality of
life.4 Psychiatric disorders are highly
prevalent in patients with CKD.
Kimmel et al.5 showed that patients
with CKD had to be hospitalized for
psychiatric disorders (particularly
depression, dementia, and substance
abuse) 1.5 to three times more
than individuals with other chronic
diseases. Yet, they are still underdiagnosed and undertreated.6
This paper discusses some of the
neuropsychiatric disorders often associated with kidney disease.
Neuropsychiatric
Submitted on: 10/08/2013.
Approved on: 10/11/2013.
Correspondence to:
Ana Cristina Simes e Silva.
Interdisciplinary Medical Research
Laboratory, School of Medicine,
Federal University of Minas Gerais
(UFMG).
Av. Alfredo Balena, n 190, 2
andar, sala 281. Belo Horizonte,
MG, Brasil. CEP: 30130-100
E-mail: acssilva@hotmail.com
Tel: (31) 3409-8073.
DOI: 10.5935/0101-2800.20140056
396
disorders associated
Introduction
with kidney disease
The psychiatric disorders associated
with kidney disease take many forms,
depending on the natural history of
the disease. Classically, uremia has
been cited as the cause of delirium.1
Symptoms such as somnolence and
psychomotor agitation may be present
among the clinical signs of acute kidney
injury (AKI). 2 Drug regimens should also be considered as a potential source
of psychiatric disorders. Steroids and
cyclosporine, used in the treatment of
various glomerulopathies and administered subsequently to renal transplantation, have been associated with depression, mania and psychotic symptoms. 3
Delirium is an acute behavioral disorder caused by impaired brain
activity, leading to cognitive impairment usually secondary to a
systemic disorder. 7 It is a condition of abrupt onset, characterized
mainly by decreases in the affected
subjects level of consciousness,
attention disorders, temporal/spatial disorientation, disorganized
thinking, and fluctuation of symptoms throughout the day. Agitation,
delusion, visual hallucinations,
and mood swings may also occur.
Changes in the patients EEG are
usually observed within the first
48 hours of onset of renal failure
As in every chronic condition,
patients with chronic kidney disease
Delirium
Neuropsychiatry and kidney disease
and anomalous findings may persist for up to
three weeks after the cessation of dialysis.4
Many are the predisposing factors for
delirium in renal diseases. The causes of
delirium may be common to other patients, and
may include fever, hemodynamic instability,
polypharmacy, hypo/hypernatremia, acid-base
disorders, hypercalcemia, hyper/hypoglycemia,
anemia and vitamin deficiency (thiamine
and cyanocobalamin).3 However, in patients
with renal failure, some specific causes must
be considered, such as uremia, aluminum
toxicity, subdural hematoma (associated with
anticoagulants and platelet dysfunction), and
dialysis disequilibrium syndrome.8
Dialysis disequilibrium syndrome (DDS)
is caused by a sudden correction in azotemia
and a consequent change in pH and osmotic
pressure, which produce a pressure gradient
between the central nervous system and
plasma, leading to cerebral edema. DDS may
set in 3-4 hours after the start of dialysis and
may last for 8-48 hours after the end of dialysis.
It is a transient condition characterized by
headaches, nausea, cramps, delirium, epileptic
seizures, and coma.4
Early detection of delirium is of paramount
importance, and treatment must be individualized for each patient.9 Prevention is the first
step when it comes to dealing with delirium.
This can be done by identifying and treating
predisposing factors and with early patient
immobilization. There is no evidence to support the use of drugs in the prevention of
delirium.
First-line treatment includes non-pharmacological approaches such as sleep facilitation,
constant reorientation, sensory deprivation control, and pain management. Antipsychotics are
commonly used to treat delirium both in hospital and intensive care unit settings. However,
the scientific evidence to support the use of
drug regimens to treat delirium is limited, and
no medication has been approved to that end.10
Although the pathophysiological models of
delirium describe a dysregulation in cholinergic
neurotransmission, the use of anticholinesterases is not recommended. In 2010, a trial on the
use of an anticholinesterase to treat delirium
had to be discontinued, as the drug failed to
benefit patients and possibly caused them harm,
as a tendency for higher mortality was observed
in the treatment group.11
Uremic encephalopathy
The term uremia was first used in 1840 by
Piorry and lHeritier, to relay the view that
the clinical signs of renal failure were related
to toxicity by urea. Currently, uremia is
described as a clinical syndrome associated
with renal failure and accumulation of
nitrogen compounds. However, no specific
substance has been implicated to date. 12
Factors such as hormonal disorders, oxidative
stress, accumulation of metabolites (such as
guanidine compounds, kynurenine pathway
metabolites), imbalance between excitatory
and
inhibitory
neurotransmitters,
and
disorders of intermediary metabolism have
been identified as possible contributing
factors. 13 Uremic encephalopathy is more
severe and progresses more rapidly in patients
with acute deterioration of renal function.14
In addition to the symptoms present in
delirium, in uremic encephalopathy symptoms may
progress along a continuum, from mildly altered
levels of consciousness to deep coma. Headache,
visual disturbances, tremor, multifocal myoclonus,
and epileptic seizures are frequently present. Clinical
signs also fluctuate over hours or days.13 Patients
may experience progressive cognitive impairment
over days to the day of dilise.15 However, levels of
azotemia (nitrogen compounds) have been poorly
correlated with neurological disorders.14
Most symptoms resolve with renal replacement
therapy - dialysis or transplantation.16
Cognitive alterations
Cognitive deficits in patients with chronic kidney
disease are common but poorly recognized. The
identification of deficits may have a positive
impact on patient outcome, especially when
they are secondary to depression or delirium,
potentially treatable conditions that must
be considered in the differential diagnosis of
cognitive impairment.17,18 Alzheimers and
vascular dementia in particular are commonly
seen in patients with CKD, the latter due to
J Bras Nefrol 2014;36(3):396-400
397
Neuropsychiatry and kidney disease
comorbidities with hypertension, diabetes and
atherosclerosis.19 Dementia has been associated
with greater levels of disability, more deaths and
hospitalizations, and interruption of dialysis.5,17
Patients on dialysis for more than a year may
suffer from a progressive neurological syndrome
called dialysis dementia, characterized by
dysarthria, dysphagia, and global dementia
with preservation of the level of consciousness.
Individuals with dialysis dementia may die within
6-12 months if not treated properly. The most
widely accepted pathophysiology of dialysis
dementia revolves around toxicity of the aluminum
salts found in dialysis fluids. The introduction of
preventive measures (discontinuation of the use of
aluminum salts in dialysis fluids and phosphate
binders containing aluminum) led to a significant
reduction in the number of cases.4
Major
depressive disorder, recurrent depressive
disorder, and suicide
Depressive disorder is the most frequently
described psychiatric condition in patients with
end-stage renal disease (ESRD).6 Prevalence can
be as high as 100%, depending on the criteria utilized and the population analyzed.18 Two studies
carried out in Brazil with patients on hemodialysis reported prevalences of major depressive
disorder of 44.8% when the Beck Depression
Inventory (BDI) was used and of 7.8% when the
10-item screening questionnaire of the Center for
Epidemiologic Studies Depression Scale (CES-D)
was applied.19,20
In a recent meta-analysis, patients on dialysis
were reported to have higher rates of depression
and increased risk of hospitalization due to
psychiatric disorders than individuals undergoing conservative treatment and post-transplant patients.5,21
Among dialysis patients, subjects on peritoneal
dialysis had a lower prevalence of depression,
anxiety symptoms, and sleep disorders than
individuals on hemodialysis.22,23
Notably, the presence of depression symptoms
may adversely affect the outcome of patients
with ESRD.24 Possible consequences are reduced
compliance to treatment, nutritional status deterioration, impaired immune system function,
and higher death rates.18,25
398
J Bras Nefrol 2014;36(3):396-400
Despite the significant prevalence of depression
and the associated morbidity, most cases remain
underdiagnosed and undertreated.6,15 A significant
portion of the somatic complaints associated
with CKD - fatigue, anorexia, weight and sleep
disorders - may mimic depression symptoms. It has
been suggested that the presence of non-vegetative
symptoms (depressed mood, suicidal thoughts,
pessimism, hopelessness, guilt, and aboulia)
would be more adequate in the characterization
of depression.4 Diagnostic screening scales such as
the BDI and the CES-D appear to be useful for
patients with CKD, given the high prevalence of
depression and morbidities affecting this group of
individuals.26
Patients with CKD are at a significantly higher
risk of committing suicide than the general population, particularly in subgroups of subjects aged
over 75 years, individuals suffering from alcohol
and substance abuse, and patients recently hospitalized for psychiatric disorders.27
Few studies have looked into the treatment
of depressive disorders for patients with CKD.
Efficacy has been attributed to cognitive
behavioral therapy (CBT) in terms of compliance
to treatment and management of depression
symptoms in patients with CKD. CBT has been
recommended as an alternative or a complement
to drug therapy.15,26 Drug interactions and side
effects (especially in transplant patients and
subjects on immunosuppressants) must be
considered when patients are offered medication
for depression.3 A more favorable side effect
profile has turned Selective Serotonin Re-uptake
Inhibitors (SSRIs) into the drug class of choice.
Caution is needed when SSRIs are prescribed.
Patients are usually started on a dose equivalent
to 30% of what would be considered the usual
dosage and must be monitored closely for
response and signs of toxicity.4,18
Anxiety disorders
Anxiety is one of the most frequently diagnosed
symptoms in patients with chronic disease.15 However,
the literature on the presence of anxiety disorders in
CKD patients is still scarce.
Forty-five percent of 50 ESRD patients on
dialysis were diagnosed with some form of anxiety
disorder; 30% of them were not treated and had
Neuropsychiatry and kidney disease
persisting symptoms 16 months into follow-up.28
Patients on hemodialysis have anxiety symptoms
more frequently than individuals on peritoneal
dialysis.23
A study carried out in Brazil with individuals
diagnosed with familial glomerulonephritis and
autosomal dominant polycystic kidney disease
reported that this group of individuals had higher
anxiety scores than subjects with other chronic
conditions.29 Another Brazilian study with 244
patients on hemodialysis reported that 5.3% of
the subjects had social phobia.30
Very little has been said or written about
the treatment of anxiety symptoms in patients
with CKD. Thus, proposed therapies have been
extrapolated from treatments offered to patients
with anxiety disorders alone. CBT and SSRIs
have surfaced as the treatments of choice.31
Benzodiazepines should be avoided and used only
in acute situations and for the shortest possible
time, given their potential to cause dependence
and associating with clinical complications such
as delirium.31 When needed, drugs with inactive
metabolites, such as lorazepam and oxazepam,
should be preferred. The cited benzodiazepines
may have their half-lives quadrupled in ESRD
patients and cannot be removed by dialysis.
Thus, extreme caution is required when these
medications are prescribed to patients with
ESRD.32
Fatigue
Fatigue is one of the most common symptoms
seen in patients with chronic disease, and
may be observed in about 50% of adults
and 25% of children and adolescents with
CKD.33,34 Among the factors possibly related
to the development of fatigue are circulating
endotoxins, inflammatory cytokines, and
increased oxidative stress. 33 Fatigue has
been positively correlated with depression,
sleep disorders, and poor quality of life.33,34
Moreover, fatigue has also been established
as a predictor for cardiovascular events,
independently from other known risk
factors. 35 The approach to fatigue in CKD
patients includes aggressive treatment of
anemia, introduction of physical activity, and
screening and treatment for depression. 36
Conclusion
Despite the growing attention given to the
psychiatric disorders of individuals with renal
disease, patients still remain underdiagnosed
and undertreated. Very few studies have been
published on the treatment of neuropsychiatric
disorders in this population, and doubts still
hover over treatment effectiveness and safety.
Early diagnosis is essential to enhance patient
quality of life and improve the outcome of renal
disease. Therefore, having a multidisciplinary
team to care for patients with kidney disease is
becoming increasingly important.
References
1.
Menninger KA. Paranoid psychosis with uremia. J
Nerv Ment Disord 1924:60:26-34. DOI: http://dx.doi.
org/10.1097/00005053-192407000-00003
2. Yu L, Santos BFC, Burdmann EA, Suassuna JHR, Batista PBP.
Diretrizes da Associao Mdica Brasileira- Sociedade Brasileira
de Nefrologia - Insuficincia Renal Aguda 2007 [Acesso 04 de
maio de 2013]. Disponvel em: www.nefrologiaonline.com.br/
Diretrizes/DiretrizesIRAnovo.doc
3. Butler J. Renal disease. In: Lloyd G & Guthrie E, editors.
Handbook of Liaison Psychiatry. 1st ed. New York: Cambridge
University Press; 2007. p.506-26.
4. Wyszynski AA. The patient with kidney disease. In: Wyszynski
AA, Wyszynski B, eds. Manual of Psychiatric Care for the
Medically III. Washington: American Psychiatric Publishing;
2005. p.69-84.
5. Kimmel PL, Thamer M, Richard CM, Ray NF. Psychiatric
illness in patients with end-stage renal disease. Am J Med
1998;105:214-21. DOI: http://dx.doi.org/10.1016/S00029343(98)00245-9
6.
Finkelstein FO, Finkelstein SH. Depression in chronic
dialysis patients: assessment and treatment. Nephrol Dial
Transplant 2000;15:1911-3. DOI: http://dx.doi.org/10.1093/
ndt/15.12.1911
7. Wacker P, Nunes PV, Forlenza OV. Delirium: uma perspectiva
histrica. Rev Psiq Cln 2005;32:97-103. DOI: http://dx.doi.
org/10.1590/S0101-60832005000300001
8. Polycarpou P, Anastassiades E, Antoniades L. From the heart to
the soul. Nephrol Dial Transplant 2007;22:945-8. DOI: http://
dx.doi.org/10.1093/ndt/gfl726
9. De Sousa A. Psychiatric issues in renal failure and dialysis.
Indian J Nephrol 2008;18:47-50. DOI: http://dx.doi.
org/10.4103/0971-4065.42337
10. Devlin JW, Al-Qadhee NS, Skrobik Y. Pharmacologic prevention
and treatment of delirium in critically ill and non-critically
ill hospitalised patients: a review of data from prospective,
randomised studies. Best Pract Res Clin Anaesthesiol 2012;26:289309. DOI: http://dx.doi.org/10.1016/j.bpa.2012.07.005
11. van Eijk MM, Roes KC, Honing ML, Kuiper MA, Karakus A,
van der Jagt M, et al. Effect of rivastigmine as an adjunct to usual
care with haloperidol on duration of delirium and mortality in
critically ill patients: a multicentre, double-blind, placebo-controlled
randomised trial. Lancet 2010;376:1829-37. PMID: 21056464
DOI: http://dx.doi.org/10.1016/S0140-6736(10)61855-7
12. Wills MR. Uremic toxins, and their effect on intermediary
metabolism. Clin Chem 1985;31:5-13.
13. Scaini G, Ferreira GK, Streck EL. Mecanismos bsicos da
encefalopatia urmica. Rev Bras Ter Intensiva 2010;22:206-11.
DOI: http://dx.doi.org/10.1590/S0103-507X2010000200016
J Bras Nefrol 2014;36(3):396-400
399
Neuropsychiatry and kidney disease
14. Burn DJ, Bates D. Neurology and the kidney. J Neurol
Neurosurg Psychiatry 1998;65:810-21. PMID: 9854955 DOI:
http://dx.doi.org/10.1136/jnnp.65.6.810
15. Cohen LM, Levy NB, Tessier EG, Germain, MJ. Renal Disease.
In: Levenson JL, ed. The American Psychiatric Publishing
textbook of psychosomatic medicine. 1st ed. Washington:
American Psychiatric Publishing; 2005 p.483-90.
16. Brouns R, De Deyn PP. Neurological complications in renal
failure: a review. Clin Neurol Neurosurg 2004;107:1-16. PMID:
15567546 DOI: http://dx.doi.org/10.1016/j.clineuro.2004.07.012
17.
Kurella Tamura M, Yaffe K. Dementia and cognitive
impairment in ESRD: diagnostic and therapeutic strategies.
Kidney Int 2011;79:14-22. PMID: 20861818 DOI: http://
dx.doi.org/10.1038/ki.2010.336
18. Cohen SD, Norris L, Acquaviva K, Peterson RA, Kimmel PL.
Screening, diagnosis, and treatment of depression in patients with
end-stage renal disease. Clin J Am Soc Nephrol 2007;2:133242. DOI: http://dx.doi.org/10.2215/CJN.03951106
19. Finger G, Pasqualotto FF, Marcon G, Medeiros GS, Abruzzi-Junior
J, May WS. Sintomas depressivos e suas caractersticas em pacientes
submetidos hemodilise. Rev AMRIGS 2011;55:333-8.
20. Santos PR. Depression and quality of life of hemodialysis patients
living in a poor region of Brazil. Rev Bras Psiquiatr 2011;33:332-7.
21. Palmer S, Vecchio M, Craig JC, Tonelli M, Johnson DW,
Nicolucci A, et al. Prevalence of depression in chronic kidney
disease: systematic review and meta-analysis of observational
studies. Kidney Int 2013;84:179-91. DOI: http://dx.doi.
org/10.1038/ki.2013.77
22. Panagopoulou A, Hardalias A, Berati S, Fourtounas C. Psychosocial issues and quality of life in patients on renal replacement
therapy. Saudi J Kidney Dis Transpl 2009;20:212-8.
23. Masoumi M, Naini AE, Aghaghazvini R, Amra B, Gholamrezaei
A. Sleep quality in patients on maintenance hemodialysis and
peritoneal dialysis. Int J Prev Med 2013;4:165-72.
24.
Marciano RC. Transtornos mentais e qualidade de vida
em crianas e adolescentes com doena renal crnica e em
seus cuidadores [Dissertao de mestrado]. Belo Horizonte:
Universidade Federal de Minas Gerais; 2009.
25. Kimmel PL, Peterson RA, Weihs KL, Simmens SJ, Alleyne S,
Cruz I, et al. Multiple measurements of depression predict
mortality in a longitudinal study of chronic hemodialysis
outpatients. Kidney Int 2000;57:2093-8. DOI: http://dx.doi.
org/10.1046/j.1523-1755.2000.00059.x
26. Hedayati SS, Minhajuddin AT, Toto RD, Morris DW, Rush
AJ. Prevalence of major depressive episode in CKD. Am J
Kidney Dis 2009;54:424-32. PMID: 19493599 DOI: http://
dx.doi.org/10.1053/j.ajkd.2009.03.017
400
J Bras Nefrol 2014;36(3):396-400
27. Kurella M, Kimmel PL, Young BS, Chertow GM. Suicide in
the United States end-stage renal disease program. J Am Soc
Nephrol 2005;16:774-81. DOI: http://dx.doi.org/10.1681/
ASN.2004070550
28. Cukor D, Coplan J, Brown C, Peterson RA, Kimmel PL.
Course of depression and anxiety diagnosis in patients treated
with hemodialysis: a 16-month follow-up. Clin J Am Soc
Nephrol 2008;3:1752-8. DOI: http://dx.doi.org/10.2215/
CJN.01120308
29. Barros BP, Nishiura JL, Heilberg IP, Kirsztajn GM. Ansiedade,
depresso e qualidade de vida em pacientes com glomerulonefrite
familiar ou doena renal policstica autossmica dominante. J
Bras Nefrol 2011;33:120-8. DOI: http://dx.doi.org/10.1590/
S0101-28002011000200002
30. Junior JAM, Souza CAM, Oliveira IR, Miranda RO. Prevalence
of psychiatric disorders in patients in hemodialysis in the state
of Bahia. J Bras Psiquiatr 2006;55:178-83.
31. Bandelow B, Sher L, Bunevicius R, Hollander E, Kasper S,
Zohar J, et al.; WFSBP Task Force on Mental Disorders in
Primary Care; WFSBP Task Force on Anxiety Disorders,
OCD and PTSD. Guidelines for the pharmacological
treatment of anxiety disorders, obsessive-compulsive
disorder and posttraumatic stress disorder in primary care.
Int J Psychiatry Clin Pract 2012;16:77-84. DOI: http://
dx.doi.org/10.3109/13651501.2012.667114
32. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson
JL, ed. The American Psychiatric Publishing textbook of
psychosomatic medicine. 1st ed. Washington, DC: American
Psychiatric Publishing; 2005. p.903-6.
33. Joshwa B, Khakha DC, Mahajan S. Fatigue and depression
and sleep problems among hemodialysis patients in a tertiary
care center. Saudi J Kidney Dis Transpl 2012;23:729-35. DOI:
http://dx.doi.org/10.4103/1319-2442.98149
34. Roumelioti ME, Wentz A, Schneider MF, Gerson AC, Hooper
S, Benfield M, et al. Sleep and fatigue symptoms in children
and adolescents with CKD: a cross-sectional analysis from the
chronic kidney disease in children (CKiD) study. Am J Kidney
Dis 2010;55:269-80. PMID: 20034719 DOI: http://dx.doi.
org/10.1053/j.ajkd.2009.09.021
35. Koyama H, Fukuda S, Shoji T, Inaba M, Tsujimoto Y,
Tabata T, et al. Fatigue is a predictor for cardiovascular
outcomes in patients undergoing hemodialysis. Clin J Am
Soc Nephrol 2010;5:659-66. DOI: http://dx.doi.org/10.2215/
CJN.08151109
36.
O'Connor NR, Corcoran AM. End-stage renal disease:
symptom management and advance care planning. Am Fam
Physician 2012;85:705-10. PMID: 22534347
You might also like
- Biophysical Characterization of Dry Facial Skin: J. L. Leveque, G. Grove, J. de Rigal, P. CorcuffDocument8 pagesBiophysical Characterization of Dry Facial Skin: J. L. Leveque, G. Grove, J. de Rigal, P. CorcuffLanna HarumiyaNo ratings yet
- 10 0000@Www Jstage JST Go jp@Article@Jat@23@11@2335436@ArticleDocument9 pages10 0000@Www Jstage JST Go jp@Article@Jat@23@11@2335436@ArticleLanna HarumiyaNo ratings yet
- Gloomy LifeDocument6 pagesGloomy LifeLanna HarumiyaNo ratings yet
- Click To Edit Master Subtitle StyleDocument4 pagesClick To Edit Master Subtitle StyleLanna HarumiyaNo ratings yet
- Click To Edit Master Subtitle StyleDocument4 pagesClick To Edit Master Subtitle StyleLanna HarumiyaNo ratings yet
- Presentation TitleDocument4 pagesPresentation TitleLanna HarumiyaNo ratings yet
- Click To Edit Master Title StyleDocument4 pagesClick To Edit Master Title StyleLanna HarumiyaNo ratings yet
- Frans Sarumpaet, Dr. Pembimbing: Bayu Rusfandi, DR., SPPDDocument13 pagesFrans Sarumpaet, Dr. Pembimbing: Bayu Rusfandi, DR., SPPDLanna HarumiyaNo ratings yet
- Title: SubheadingDocument7 pagesTitle: SubheadingLanna HarumiyaNo ratings yet
- Tentative Acara Workshop SimpoDocument7 pagesTentative Acara Workshop SimpoLanna HarumiyaNo ratings yet
- Kol Ditz 2016Document3 pagesKol Ditz 2016Lanna HarumiyaNo ratings yet
- Related InfectionDocument3 pagesRelated InfectionLanna HarumiyaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- (Q2) Electrochemistry 29th JulyDocument21 pages(Q2) Electrochemistry 29th JulySupritam KunduNo ratings yet
- Monitoring:: Steps of Adding New SiteDocument8 pagesMonitoring:: Steps of Adding New SiteMohammad ZakoutNo ratings yet
- List of Irc Publications Referred To in The Specifications: AppendicesDocument17 pagesList of Irc Publications Referred To in The Specifications: AppendicesPrasad BoniNo ratings yet
- Orona Fault CodesDocument19 pagesOrona Fault CodesDanushka Bandara100% (1)
- Https - Threejs - Org - Examples - Webgl - Fire - HTMLDocument9 pagesHttps - Threejs - Org - Examples - Webgl - Fire - HTMLMara NdirNo ratings yet
- Linear Predictor: Nature of Linear PredictionDocument9 pagesLinear Predictor: Nature of Linear PredictionkvNo ratings yet
- Driver DST-4812 For 7.2 KG CMDocument5 pagesDriver DST-4812 For 7.2 KG CMWWW.150775.BUGME.PWNo ratings yet
- DHL Product Solutions Portfolio 2017Document1 pageDHL Product Solutions Portfolio 2017Hanzla TariqNo ratings yet
- tmpE0D4 TMPDocument7 pagestmpE0D4 TMPFrontiersNo ratings yet
- Saberon StratMan2Document3 pagesSaberon StratMan2paredesladyheart18No ratings yet
- 2nd Quarter - Summative Test in TleDocument2 pages2nd Quarter - Summative Test in TleRachelle Ann Dizon100% (1)
- Photography Techniques (Intermediate)Document43 pagesPhotography Techniques (Intermediate)Truc Nguyen100% (2)
- Drainage BasinsDocument4 pagesDrainage BasinsDannySP10100% (1)
- Math Diagnostic ExamDocument4 pagesMath Diagnostic ExamMananquil JeromeNo ratings yet
- Elements or Appurtenances of The Stilling BasinsDocument21 pagesElements or Appurtenances of The Stilling BasinsAhmad PshtiwanNo ratings yet
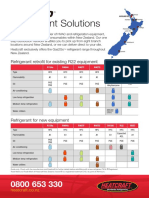
- Refrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentDocument2 pagesRefrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentpriyoNo ratings yet
- Versana Premier Transducer GuideDocument4 pagesVersana Premier Transducer GuideDigo OtávioNo ratings yet
- Graviola1 Triamazon, AntiCancer, InglesDocument2 pagesGraviola1 Triamazon, AntiCancer, InglesManuel SierraNo ratings yet
- Vital Judo Throwing TechniquesDocument193 pagesVital Judo Throwing TechniquesJuan Jose Opazo Carvajal100% (1)
- Electricity and MagnetismDocument29 pagesElectricity and MagnetismNashrul HaqNo ratings yet
- Pnbcontr0223en (Web)Document308 pagesPnbcontr0223en (Web)James GeorgeNo ratings yet
- Titanvene ll0209sr Product Data SheetpdfDocument1 pageTitanvene ll0209sr Product Data SheetpdfHanry WRNo ratings yet
- Power SupplyDocument79 pagesPower SupplySharad KumbharanaNo ratings yet
- Boil-Off Gas CalculationsDocument14 pagesBoil-Off Gas CalculationsAlberto100% (1)
- EOCR 종합 EN 2015 PDFDocument228 pagesEOCR 종합 EN 2015 PDFShubhankar KunduNo ratings yet
- The Modern Day Cult: by Antonio Panebianco, Jason Devine, Will RichardsDocument11 pagesThe Modern Day Cult: by Antonio Panebianco, Jason Devine, Will RichardsAntonio PanebiancoNo ratings yet
- Podar International School (Icse) Practice Sheet STD: IX Chapter 28: Distance FormulaDocument2 pagesPodar International School (Icse) Practice Sheet STD: IX Chapter 28: Distance FormulaVanshika MehrotraNo ratings yet
- Bams 1st Rachna Sharir Joints and Their Classification 16-05-2020Document15 pagesBams 1st Rachna Sharir Joints and Their Classification 16-05-2020Sanjana SajjanarNo ratings yet
- Design and Management of Mettur Dam by Predicting Seepage Losses Using Remote SensingDocument10 pagesDesign and Management of Mettur Dam by Predicting Seepage Losses Using Remote SensingInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- Appetizer Summative TestDocument36 pagesAppetizer Summative TestArgelynPadolinaPedernalNo ratings yet