Professional Documents
Culture Documents
Sepsis Effects On Organs
Uploaded by
RLI23nyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sepsis Effects On Organs
Uploaded by
RLI23nyCopyright:
Available Formats
Topic Review: Sepsis Spectrum and effect on Organs
Systemic
Inflammatory
Response
Syndrome
(SIRS)
Sepsis
Severe Sepsis
Septic Shock
2 of the following
Temperature > 38C or <36C
Heart Rate > 90 beats per minute
Respiration Rate > 20 breaths per minute (Tachypnea) or PaCO2 < 32 mmHg
White Blood Cells > 12,000 cells/mm3, or <4,000 cells/mm3, or > 10% band cells
SIRS + suspected infections
Sepsis + organ dysfunction, hypoperfusion, or hypotension
Signs of hypoperfusion may include lactic acidosis, oligouria, change in mental status
Sepsis-induced hypotension despite adequate fluid resuscitation, along with signs of
hypoperfusion
Patients typically have abnormal vital signs (tachycardia and tachypnea) and a narrow pulse
pressure in addition to low blood pressure.
Shock Basic Definition: Generalized hypoperfusion of the body (i.e., not enough blood is being circulated to
supply the organs with the oxygen they require)
Presentation of Shock: Presents with tachycardia, hypotension, and malfunction of under perfused organs.
o Autonomic Response:
Autonomic response vagal response, heart rate (HR), cardiac output (CO), glycogenolysis
and gluconeogenesis
Baroreceptors detect blood pressure (BP) activates Sympathetic nervous system (Cathecolamines
may be secreted (Epi and NE)
- Cardiac Effects Force of contractions, Rate, and CO
- Peripheral Effects
Arteriolar constriction (via Adrenergic stim) Pre-/Post- Capillary sphincter contraction
SVR Maintained CO and BP
Intracapillary hydrostatic pressure transcapillary refill from interstitial fluid
intravascular fluid volume venous return Maintained CO and BP
Peripheral resistance
Shunting of blood to core organs
o
Neurologic/Brain: CNS dysfunction (altered mental status/loss of consciousness)
Continuum of mental status changes frequently encountered in shock begins with agitation,
progresses to confusion or delirium, and ends in coma.
Renal: Anuria/oligouria BUN/Cr ratio
Physiologic response of the kidney to hypoperfusion is to conserve salt and water.
- Renal blood flow (RBF) and afferent arteriolar resistance accounts for glomerular filtration
rate (GFR)
- Blood flow to kidney Kidneys secrete renin Initiating Renin-Angiotensin-Aldosterone
System (RAAS) Angiotensin stimulates aldosterone leads to reabsorption of sodium and
water urine formation.
- BP initiates ADH (vasopressin) release from posterior pituitary gland H2O reabsorption
by kidneys conserves blood volume urine output
- Aldosterone and Vasopressin enhance H2O reabsorption and cause vasoconstriction
Toxic injury causes necrosis of tubular epithelium and tubular obstruction by cellular debris with
back leak of filtrate
Depletion of renal ATP stores that occurs with prolonged renal hypoperfusion contributes to
subsequent impairment of renal function
Page 1 of 8
Blood: Lactic acid production Lactic Acidosis
Sympathetic Nervous System (Hormonal): Anterior pituitary releases adrenocorticotropic hormones
stimulates adrenal cortex to release glucocorticoids blood sugar increase to meet Basal
Metabolic Rate (BMR)
- BMR amount of energy used in the functioning of vital organs.
Anaerobic metabolism energy needed is not being supplied by enough oxygen created through
the breaking down of carbohydrates.
- Breakdown of glucose to pyruvate to ultimately lactate (minimal net energy production)
- Plasma lactate indicates anaerobic metabolism and inadequate tissue perfusion
- Metabolic acidosis develops as shock progresses, reflecting decreased clearance of lactate by the
Liver: Increased AST and ALT
Ischemic hepatitis due to hypoxia and/or low BP inadequate O2 to liver causes centrolobular
hepatocellular necrosis (most sensitive to hypoxic damage) results in increased aspartate
aminotransferase (AST) and alanine aminotransferase (ALT) concentrations (usually > 1000 IU/I)
Pulmonary/Respiratory: Shortness of breath
Tachypnea Hypoxia Respiratory alkalosis atelectasis acute lung injury acute
respiratory distress syndrome (ARDS)
- Shock-induced tachypnea tidal volume, dead space and minute ventilation
- Tachypnea + Hypoxia induce a respiratory alkalosis
- Recumbency and involuntary restriction of ventilation secondary to pain reduce functional
residual capacity may lead to atelectasis
- Shock and, in particular, resuscitation-induced oxidant radical generation, is recognized as a
major cause of acute lung injury and subsequent acute respiratory distress syndrome
Cardiovascular/Heart: Tachycardia, Chest pain
Systemic tissue perfusion is determined by the cardiac output (CO) and systemic vascular
resistance (SVR) Systemic tissue perfusion is a consequence of diminished CO, SVR, or both
SVR is the vascular tone and is a large determinant of diastolic BP.
SVR is governed by the vessel length, blood viscosity, and vessel diameter
CO is the major determinant of tissue perfusion
SV is determined by three parameters (1) ventricular filling (preload), (2) the resistance to
ventricular ejection (afterload), and (3) myocardial contractility
Preload = volume of blood in ventricles at end of diastole (EDV) (ed in Hypervolemia,
Regurgitation of cardiac valves, Heart Failure) Preload (Volume) SV (EDV)
EDV = filled ventricular volume prior to systolic contraction determined by preload
volume SV (via FrankStarling curves) where diastolic filling volumes CO
Filling pressures stimulate release of brain natriuretic peptide (BNP) to secrete
sodium and volume to relieve pressure on the heart.
Levels of BNP correlate with outcome following severe stress.
Page 2 of 8
Afterload = Resistance LV must overcome to circulate blood ( Afterload = Cardiac
Workload) (ed in HTN and vasoconstriction) Afterload (Contractility) SV
(ESV)
ESV = residual blood left in ventricle after emptying during systole determined by
cardiac contractility and it as heart ejects a greater percentage of its diastolic
volume.
Page 3 of 8
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PV LoopDocument1 pagePV LoopRLI23nyNo ratings yet
- Bio-Rad D-10 Dual ProgramDocument15 pagesBio-Rad D-10 Dual ProgramMeesam AliNo ratings yet
- Muscle ContractionsDocument1 pageMuscle ContractionsRLI23nyNo ratings yet
- Oxygen DissociationDocument1 pageOxygen DissociationRLI23nyNo ratings yet
- Gastric Cells and SecretionDocument1 pageGastric Cells and SecretionRLI23nyNo ratings yet
- HISTORY - There Is No Substitute For A Thorough Patient History For Determining Whether Other Conditions AreDocument9 pagesHISTORY - There Is No Substitute For A Thorough Patient History For Determining Whether Other Conditions AreRLI23nyNo ratings yet
- Type Description Principal Mechanism Clinical Examples Cardiogenic ShockDocument1 pageType Description Principal Mechanism Clinical Examples Cardiogenic ShockRLI23ny100% (1)
- Hypoxemia Interpretation of SpirometryDocument55 pagesHypoxemia Interpretation of SpirometryRLI23nyNo ratings yet
- CSF Characteris Tics: 40 (0 - 10) 40 40 May Be Elevated (50 - 100)Document5 pagesCSF Characteris Tics: 40 (0 - 10) 40 40 May Be Elevated (50 - 100)RLI23nyNo ratings yet
- Solute Transport in NephronDocument1 pageSolute Transport in NephronRLI23nyNo ratings yet
- Ascus: After Colposcopy Pap Smear Every 3 Months For 1 YearDocument1 pageAscus: After Colposcopy Pap Smear Every 3 Months For 1 YearRLI23nyNo ratings yet
- Exercise Is The Right Thing You Do: PolycythemiaDocument1 pageExercise Is The Right Thing You Do: PolycythemiaRLI23nyNo ratings yet
- X-Ray Review Chest Name Age Date View PA View: Most Common. Scapula Are NOT VisibleDocument2 pagesX-Ray Review Chest Name Age Date View PA View: Most Common. Scapula Are NOT VisibleRLI23nyNo ratings yet
- Disease Deficiency/ Defect Abnormal Levels Symptoms NotesDocument1 pageDisease Deficiency/ Defect Abnormal Levels Symptoms NotesRLI23nyNo ratings yet
- Practice Problem For Formats LogDocument4 pagesPractice Problem For Formats LogRLI23nyNo ratings yet
- Pulse Pulse Location Surface Anatomy (Not Palpated For Vital Signs)Document1 pagePulse Pulse Location Surface Anatomy (Not Palpated For Vital Signs)RLI23nyNo ratings yet
- Reporting of Vital SignsDocument1 pageReporting of Vital SignsRLI23nyNo ratings yet
- Abx Mech of ActionDocument1 pageAbx Mech of ActionRLI23nyNo ratings yet
- PT3 Guided WritingDocument8 pagesPT3 Guided WritingDayang Haffizah Abg AbdillahNo ratings yet
- Eureka Forbes ReportDocument75 pagesEureka Forbes ReportUjjval Jain0% (1)
- 1984 Population Report EthiopiaDocument255 pages1984 Population Report EthiopiaOsvaldas ZagurskasNo ratings yet
- Sip Dissertation - Final - Final For CollegeDocument17 pagesSip Dissertation - Final - Final For Collegevikashirulkar922No ratings yet
- Beauty Therapy Thesis SampleDocument8 pagesBeauty Therapy Thesis Samplerachelvalenzuelaglendale100% (2)
- MicrosoftDynamicsNAVAdd OnsDocument620 pagesMicrosoftDynamicsNAVAdd OnsSadiq QudduseNo ratings yet
- High Performance Liquid Chromatography: University of Santo Tomas Faculty of Pharmacy Department of BiochemistryDocument32 pagesHigh Performance Liquid Chromatography: University of Santo Tomas Faculty of Pharmacy Department of BiochemistryMa. Ellah Patricia M. GutierrezNo ratings yet
- Opti Turn Tu 2004 V ManualDocument80 pagesOpti Turn Tu 2004 V ManualCharu NavneetNo ratings yet
- Static CMOS and Dynamic CircuitsDocument19 pagesStatic CMOS and Dynamic CircuitsAbhijna MaiyaNo ratings yet
- Dumel James Melchor DuayDocument3 pagesDumel James Melchor DuayBle DuayNo ratings yet
- Photography Techniques (Intermediate)Document43 pagesPhotography Techniques (Intermediate)Truc Nguyen100% (2)
- AD&D - Forgotten Realms - Menzoberranzan - EXTRAS - House Do'Urden RestrospectiveDocument16 pagesAD&D - Forgotten Realms - Menzoberranzan - EXTRAS - House Do'Urden RestrospectiveThiago RaulinoNo ratings yet
- Scattered Pearls: Selected Sayings and Anecdotes of The Illustrious AuliyaaDocument103 pagesScattered Pearls: Selected Sayings and Anecdotes of The Illustrious AuliyaaYeye17100% (1)
- Monitoring:: Steps of Adding New SiteDocument8 pagesMonitoring:: Steps of Adding New SiteMohammad ZakoutNo ratings yet
- Fourth Quarter ExamDocument4 pagesFourth Quarter Examjanice gumabao50% (4)
- Module 5: Safety and Health at Work: Participant's HandbookDocument24 pagesModule 5: Safety and Health at Work: Participant's HandbookChristian Surio RamosNo ratings yet
- Rolling Bearings VRMDocument2 pagesRolling Bearings VRMRollerJonnyNo ratings yet
- P eDocument22 pagesP eKiks AshNo ratings yet
- Massimo Cacciari, 1994. The Necessary AngelDocument133 pagesMassimo Cacciari, 1994. The Necessary AngelAbner J ColmenaresNo ratings yet
- Sarason ComplexFunctionTheory PDFDocument177 pagesSarason ComplexFunctionTheory PDFYanfan ChenNo ratings yet
- Medgroup Packet Tracer Skills Integration Challenge: - Design and Prototype The New Medgroup TopologyDocument4 pagesMedgroup Packet Tracer Skills Integration Challenge: - Design and Prototype The New Medgroup TopologyvilanchNo ratings yet
- Order,+ERC+Case+No.+2014 174+RCDocument9 pagesOrder,+ERC+Case+No.+2014 174+RCCoii Yee Jr.No ratings yet
- Exact Solution Tank DrainageDocument8 pagesExact Solution Tank DrainageFelipe CastNo ratings yet
- SSMTT-27 E1 PDFDocument8 pagesSSMTT-27 E1 PDFblackNo ratings yet
- L15 - Parallel Magnetic CircuitsDocument6 pagesL15 - Parallel Magnetic CircuitsParikshit MishraNo ratings yet
- HP Prodesk 400 G6 Microtower PC: Reliable and Ready Expansion For Your Growing BusinessDocument4 pagesHP Prodesk 400 G6 Microtower PC: Reliable and Ready Expansion For Your Growing BusinessPằngPằngChiuChiuNo ratings yet
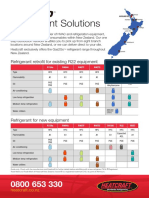
- Refrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentDocument2 pagesRefrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentpriyoNo ratings yet
- Unit-I: Digital Image Fundamentals & Image TransformsDocument70 pagesUnit-I: Digital Image Fundamentals & Image TransformsNuzhath FathimaNo ratings yet
- MS 005 For DUCT FABRICATION - INSULATION & INSTALLATION REV-1Document21 pagesMS 005 For DUCT FABRICATION - INSULATION & INSTALLATION REV-1vusal huseynli100% (2)