Professional Documents
Culture Documents
WHO Preeklampsia Prevention PDF
Uploaded by
Rendra Artha Ida BagusOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WHO Preeklampsia Prevention PDF
Uploaded by
Rendra Artha Ida BagusCopyright:
Available Formats
WHO Recommendations for Prevention and
Treatment of Pre-Eclampsia and Eclampsia:
Implications and Actions
Background
Nearly one-tenth of maternal deaths in Asia and Africa and one-quarter of maternal deaths in
Latin America are associated with hypertensive disorders of pregnancy. Among the hypertensive
disorders, pre-eclampsia and eclampsia have the greatest impact on maternal and newborn
morbidity and mortality. Yet the majority of deaths related to pre-eclampsia and eclampsia could
be avoided if women received timely and effective care, delivered according to evidence-based
standards.
Criteria for Diagnosis of Pre-eclampsia and Eclampsia
Pre-eclampsia:
Onset of a new episode of hypertension during pregnancy, characterized by:
Persistent hypertension (diastolic blood pressure 90 mm Hg) and
Substantial proteinuria (> 0.3 g/24 hours).
Eclampsia:
Generalized seizures, generally in addition to pre-eclampsia criteria
The primary goal of the WHO Recommendations for Prevention
and Treatment of Pre-eclampsia and Eclampsia is to improve the
quality of care and outcomes for pregnant women who develop the
two most dangerous hypertensive disorders. While the
recommendations are not intended to be comprehensive, they are
intended to promote proven, evidence-based clinical practices in
the management of women with pre-eclampsia and eclampsia.
Guideline Content and Development Process
WHOs guidelines were developed in accordance with the WHO
Handbook for Guideline Development, through a process
involving: (1) identification of critical questions and critical
outcomes; (2) retrieval of evidence; (3) assessment, grading, and
synthesis of the evidence; (4) formulation of recommendations;
and (5) planning for dissemination, implementation, impact evaluation, and updating. In
addition to staff from the WHO Departments of Reproductive Health and Research, Making
Pregnancy Safer, and Nutrition for Health and Development, many international stakeholders
and external experts, including 173 participants in an online consultation and 25 experts at a
technical consultation, were involved in the guideline development process. Evidence related to
each specific question, drawn primarily from Cochrane reviews, was rigorously examined and
graded according to its strength. Likewise, the strength of each recommendation was determined
based on the grade of the evidence as well as the magnitude of the effect, the balance of
advantages versus disadvantages, resource use, and feasibility.
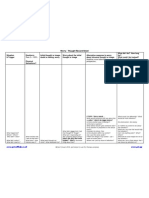
CLINICAL PRACTICE RECOMMENDATIONS FOR THE PREVENTION AND MANAGEMENT OF
PRE-ECLAMPSIA AND ECLAMPSIA1
During Antenatal Care
Practices
Recommended
Practices NOT
Recommended
Practice Implication
Calcium supplementation during
pregnancy in areas where calcium intake
is low
Vitamin D supplementation during
pregnancy
Calcium supplementation during
pregnancy in areas where calcium
deficiency is not present
Low-dose acetylsalicylic acid (aspirin,
75 mg) for the prevention of preeclampsia in women at high risk of
developing the condition
Individual or combined vitamin C
and vitamin E supplementation
Antihypertensive drugs for pregnant
women with severe hypertension
Use of diuretics, particularly
thiazides, for prevention of preeclampsia and its complications
Give antihypertensive drugs, but
not diuretics, to pregnant women
with severe hypertension.
Advice to rest at home
Do not advise rest or dietary salt
restriction for pregnant women to
prevent pre-eclampsia or its
complications.
Strict bed rest for pregnant women
with hypertension (with or without
proteinuria)
Provide calcium to all women
and acetylsalicylic acid to
selected groups for the
prevention of PE/E. While
vitamin supplementation can be
useful for other health
conditions, do not provide
Vitamins C, D, or E, to pregnant
women as part of a strategy for
prevention of PE/E.
Restriction in dietary salt intake
In women with severe pre-eclampsia,
if there is a viable fetus and the
pregnancy is less than 36 (plus 6 days)
weeks of gestation, expectant
management can be considered,
provided that uncontrolled maternal
hypertension, increasing maternal organ
dysfunction, and fetal distress do not
occur and the conditions can be
monitored.
For a woman with pre-eclampsia
during a preterm pregnancy (< 37
weeks), clinicians can monitor the
woman if: (1) her blood pressure is
under control, (2) there is no fetal
distress, and (3) there are no signs
of maternal organ dysfunction.
Continuous monitoring is
necessary during this period of
expectant management.
During Labor and Birth
Recommended Practices
Induction of labor for women with severe pre-eclampsia
at a gestational age when the fetus is not viable or is unlikely
to achieve viability within one or two weeks
Practice Implication
Conduct an expedited delivery for women with severe
pre-eclampsia remote from term, whether or not the
fetus is viable.
Expedited delivery for women with severe pre-eclampsia
at term
Recommended Practices
Magnesium sulfate, in preference to other
anticonvulsants, for the prevention of eclampsia in women
with severe pre-eclampsia
Magnesium sulfate, in preference to other
anticonvulsants, for treatment of women with eclampsia
The full intravenous or intramuscular magnesium sulfate
regimen for the prevention and treatment of eclampsia
Practice Implication
Magnesium sulfate is the anticonvulsant of choice for
women with severe pre-eclampsia or eclampsia. If
possible, give a full regimen of magnesium sulfate to
women with eclampsia or severe pre-eclampsia. If the
administration of a full regimen is not possible, these
women should be given the loading dose of magnesium
sulfate and should immediately transferred to a higherlevel health care facility for further treatment.
For women with severe pre-eclampsia or eclampsia, in
settings where it is not possible to administer the full
magnesium sulfate regimen, use the magnesium sulfate
loading dose followed by immediate transfer to a higher-level
health care facility
1 A full report of the recommendations can be found in WHO Recommendations for Prevention and Treatment of Pre-eclampsia and
Eclampsia (http://whqlibdoc.who.int/publications/2011/9789241548335_eng.pdf), and a full listing of the evidence supporting
these recommendations can be found in WHO Recommendations for Prevention and Treatment of Pre-eclampsia and Eclampsia:
Evidence Base http://whqlibdoc.who.int/hq/2011/WHO_RHR_11.25_eng.pdf).
CLINICAL PRACTICE RECOMMENDATIONS FOR THE PREVENTION AND MANAGEMENT OF
PRE-ECLAMPSIA AND ECLAMPSIA1
During Postpartum Care
Recommended Practices
Continued antihypertensive drugs during the postpartum
period for women treated with antihypertensive drugs during
the antenatal period care
Antihypertensive drugs for women with severe
postpartum hypertension
Practice Implication
Treat women with antihypertensive drugs during the
postpartum if they: (1) have severe postpartum
hypertension, or (2) were treated with antihypertensive
drugs during pregnancy.
Program Actions
The ultimate goal of these guidelines is to improve the quality of care and health outcomes
related to pre-eclampsia and eclampsia. The recommendations, especially those that represent a
change from previous practice, will require actions at the national, district, and local levels. The
following actions are needed:
1. Revise national guidelines or protocols to include evidence-based practices.
Each countrys approach to promoting the use of the recommendations should be tailored to
the specific national and local context. The revision of existing national guidelines should be
a well-planned and participatory, consensus-driven process, and any modifications should be
made in an explicit and transparent manner and based on clear justification. The revision
process should include these steps:
Convene a national working group of recognized clinical experts from government agencies,
medical and nursing/midwifery educational institutions, professional organizations, key
nongovernmental organizations (NGOs), and other experts to review the WHO
recommendations and consider what adaptations are necessary for the local context.
Develop clear and practical clinical protocols that reflect the recommendations.
Develop clear and practical guidance for community health workers.
Ensure that policy, including job descriptions, reflect the new recommendations.
Ensure that all skilled birth attendants are authorized to give magnesium sulfate
and antihypertensives for severe pre-eclampsia and eclampsia.
Ensure that trained community health workers are authorized to counsel and provide
calcium in areas of calcium deficiency.
Orient key governmental and NGO stakeholders and opinion leaders to the
recommendations and their implications for practice in facilities and communities.
Ensure that stakeholders at the national, district, and community levels are included
in the orientation.
Ensure that copies of the current guidelines are distributed to all facilities and
educational institutions.
2. Promote essential components that help ensure an enabling environment.
Selected processes and procedures should be put in place to ensure an enabling environment
for implementation of the recommendations.
Drugs such as magnesium sulfate, calcium gluconate, and antihypertensives (such as
labetalol, hydralazine, nifedipine, or methyldopa), as well as appropriate formulations of
calcium and acetylsalicylic acid, should be on the essential drug list.
Budgets and supply systems must accommodate continuous, ready access to essential
drugs and supplies. Each site where antenatal or labor and delivery care is provided must
have the following:
Functioning sphygmomanometers and stethoscopes
Appropriate antihypertensive drugs, such as labetalol, hydralazine, nifedipine, or
methyldopa
Magnesium sulfate and calcium gluconate
10 mL and 20 mL syringes
Normal saline or Ringers lactate IV solution
Job aid for the administration of magnesium sulfate
3
Health care workers should be committed to evidence-based clinical practices.
An eclampsia box, which includes all needed drugs and equipment (syringe, swabs,
intravenous line, etc.), as a practical solution to facilitate rapid action
Antenatal care skills should include the provision of preventive supplements.
All health care providers who care for pregnant women or women in labor must be
competent to detect and manage pre-eclampsia and eclampsia, to prevent women
with pre-eclampsia from developing eclampsia. Providers will also need the skills to
induce labor, perform operative delivery, or refer women who need a higher level of
care.
Health care providers should avoid the use of treatments and drugs that have been
shown to be ineffective or potentially harmful, and they should advocate against
these practices in their facilities and among their colleagues.
Evidence-based services should be established in the most peripheral settings that care for
pregnant and laboring women, to ensure equitable access to services and help initiate
emergency supportive care as early as possible when complications are detected.
3. Use participatory processes to change provider behavior with regard to evidencebased practices.
Health care providers and other key stakeholders in government and NGOs should be
involved in the process of guideline development and adaptation.
Providers should be involved in establishing evidence-based standards of care and in the
assessment of progress toward achieving the standards.
The competencies necessary to achieve these standards should be taught in pre-service
education and should be included in in-service training in facilities and communities as
needed. Curricula may need to be developed or revised, teaching materials may need to
be developed, and faculty and trainers may need to be trained.
E-health and informatics reminders and decision support, audit-and-feedback, and
supportive supervision should foster continuous improvement in the provision of quality
care and should recognize quality when it is achieved.
Professional networks and organizations can be enlisted to support implementation of
evidence-based guidelines.
Job aids should be available to remind providers of protocols and procedures.
4. Monitor and evaluate guideline implementation.
Monitoring and evaluation systems must include appropriate indicators that are
examined in a non-punitive manner and that can be used to guide the development,
management, and scale-up of services. Ideally, implementation of the recommendations
should be monitored at the health service level. Data can be supplemented with
secondary analysis of administrative or clinical databases. Clearly defined indicators are
needed and could be associated with locally determined targets. In this context, two
critical indicators are suggested:
The proportion of women with severe pre-eclampsia or eclampsia who receive
magnesium sulfate therapy (calculated as the number of women with severe preeclampsia/eclampsia receiving magnesium sulfate over the total number of women
who present with severe pre-eclampsia/eclampsia)
The proportion of pre-eclamptic women with severe hypertension who receive an antihypertensive agent over the total number of pre-eclamptic women with severe
hypertension
These indicators provide an overall measure of the use of magnesium sulfate as the first option
therapy for eclampsia, and appropriate use of antihypertensive agents.
The use of other locally determined process indicators is also recommended, particularly for the
assessment of the preventive use of magnesium sulfate and local protocol compliance during the
loading and maintenance phases.
You might also like
- 1 PDFDocument8 pages1 PDFRendra Artha Ida BagusNo ratings yet
- Alcazar PDFDocument4 pagesAlcazar PDFRendra Artha Ida BagusNo ratings yet
- Initial Evaluation and Referral Guidelines For Management of Pelvic Ovarian MassesDocument6 pagesInitial Evaluation and Referral Guidelines For Management of Pelvic Ovarian Massesjhon heriansyahNo ratings yet
- Antenatal Treatment of Hydrocephalus via Ventriculoamniotic ShuntingDocument2 pagesAntenatal Treatment of Hydrocephalus via Ventriculoamniotic ShuntingRendra Artha Ida BagusNo ratings yet
- Fetal Ventriculomegaly: Postnatal Management: Special Annual IssueDocument3 pagesFetal Ventriculomegaly: Postnatal Management: Special Annual IssueRendra Artha Ida BagusNo ratings yet
- Breech Za NigeriaqDocument10 pagesBreech Za NigeriaqRendra Artha Ida BagusNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument8 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyRendra Artha Ida BagusNo ratings yet
- RCOG Cardiac Disease and Pregnancy PDFDocument18 pagesRCOG Cardiac Disease and Pregnancy PDFSteven SetioNo ratings yet
- Articles: BackgroundDocument9 pagesArticles: BackgroundRendra Artha Ida BagusNo ratings yet
- Mouritsen 20Document7 pagesMouritsen 20Rendra Artha Ida BagusNo ratings yet
- The Presence and Location of Estrogen and Progesterone Receptors in The Human Pelvic Cardinal LigamentsDocument3 pagesThe Presence and Location of Estrogen and Progesterone Receptors in The Human Pelvic Cardinal LigamentsRendra Artha Ida BagusNo ratings yet
- 4Document11 pages4Rendra Artha Ida BagusNo ratings yet
- HypertensionPregnancy (1) AcogDocument7 pagesHypertensionPregnancy (1) AcogFelipe LlanosNo ratings yet
- NejDocument9 pagesNejRendra Artha Ida BagusNo ratings yet
- Book OgDocument37 pagesBook OgRendra Artha Ida BagusNo ratings yet
- OvarianDocument5 pagesOvarianRendra Artha Ida BagusNo ratings yet
- RCOG Cardiac Disease and Pregnancy PDFDocument18 pagesRCOG Cardiac Disease and Pregnancy PDFSteven SetioNo ratings yet
- Second Trimester Maternal Dimeric Inhibin-A in The Multiple-Marker Screening Test For Down's SyndromeDocument5 pagesSecond Trimester Maternal Dimeric Inhibin-A in The Multiple-Marker Screening Test For Down's SyndromeRendra Artha Ida BagusNo ratings yet
- Meconeum Peritonitis Case ReportDocument2 pagesMeconeum Peritonitis Case ReportRendra Artha Ida BagusNo ratings yet
- Presentase Lemak Tubuh Dengan Preeklampsia Pada Awal KehamilanDocument7 pagesPresentase Lemak Tubuh Dengan Preeklampsia Pada Awal KehamilanNovela VeronaNo ratings yet
- HypertensionPregnancy (1) AcogDocument7 pagesHypertensionPregnancy (1) AcogFelipe LlanosNo ratings yet
- Abnormal BleedingDocument20 pagesAbnormal BleedingratnacantikNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Exploring Perfect PostureDocument8 pagesExploring Perfect Posturesquishyware100% (1)
- CME BodyGuard 323 - User Manual PDFDocument80 pagesCME BodyGuard 323 - User Manual PDFCristian Andres ValenciaNo ratings yet
- ArrhythmiasDocument48 pagesArrhythmiasHarshan JeyakumarNo ratings yet
- UTIDocument4 pagesUTIVagabond RabbyNo ratings yet
- GAD Thought Record SheetDocument1 pageGAD Thought Record SheetpanickedchickNo ratings yet
- The Ashtavaidya Medical Tradition of KeralaDocument5 pagesThe Ashtavaidya Medical Tradition of Keralahari haraNo ratings yet
- Framework For Professional PracticeDocument26 pagesFramework For Professional PracticeAdvait GulatiNo ratings yet
- ABCs of Psychiatric MedicinesDocument41 pagesABCs of Psychiatric Medicines아이닠텓No ratings yet
- Farmakopunktur Pada KankerDocument15 pagesFarmakopunktur Pada KankerYoshua ViventiusNo ratings yet
- Terapii ExperiențialeDocument14 pagesTerapii ExperiențialeCretu IleanaNo ratings yet
- Clinical Audit: Pain Management in Total Knee Replacement Aadhar Hospital January - July 2018Document29 pagesClinical Audit: Pain Management in Total Knee Replacement Aadhar Hospital January - July 2018Relacy Healthcare100% (2)
- Outcomes of Masking and Habituation Therapy With The Implementation of A New Sound Therapy ProtocolDocument7 pagesOutcomes of Masking and Habituation Therapy With The Implementation of A New Sound Therapy ProtocolGöksel TurhalNo ratings yet
- MJ SolisDocument3 pagesMJ SolisBaltazar MarcosNo ratings yet
- Brevital (Methohexital) PIDocument1 pageBrevital (Methohexital) PIBrian HarrisNo ratings yet
- Goodman and Gilman39s Manual of Pharmacology and Therapeutics Latest EditionDocument3 pagesGoodman and Gilman39s Manual of Pharmacology and Therapeutics Latest EditionLinda0% (1)
- Proceeding Liver Update 2015Document268 pagesProceeding Liver Update 2015Bambang Prasetio100% (2)
- Model Curriculum Handbook RadiotDocument157 pagesModel Curriculum Handbook RadiotYuda FhunkshyangNo ratings yet
- Endocrine NursingDocument2 pagesEndocrine NursingUnclePorkchop94% (34)
- The Alexander TechniqueDocument27 pagesThe Alexander Techniquedaniyal.az100% (1)
- Freedom at Your FingertipsDocument30 pagesFreedom at Your FingertipsLucian Grec100% (1)
- The How and Why of The Movement System As The Identity of Physical TherapyDocument8 pagesThe How and Why of The Movement System As The Identity of Physical TherapyValeria Javalera BatNo ratings yet
- Wim Hof MethodDocument4 pagesWim Hof MethodAdiMulahasanovicNo ratings yet
- Literature Review: Periodontal AnatomyDocument68 pagesLiterature Review: Periodontal AnatomyRoshna NarayanNo ratings yet
- Positioning Techniques in Long-Term Care - Self-Directed Learning Package For Health Care Providers PDFDocument41 pagesPositioning Techniques in Long-Term Care - Self-Directed Learning Package For Health Care Providers PDFAde Risaldi TangdilianNo ratings yet
- Atomic HabitsDocument31 pagesAtomic HabitsRafaelOliveira100% (23)
- CASE STUDY-Chris SizemoreADocument2 pagesCASE STUDY-Chris SizemoreAMatthew Karl Cuenco GatdulaNo ratings yet
- Hypnotism Secret 8Document5 pagesHypnotism Secret 8parasNo ratings yet
- Jacques Lacan BiographyDocument2 pagesJacques Lacan Biographysantanu6No ratings yet
- Lower Extremity DisordersDocument14 pagesLower Extremity DisordersJameson87No ratings yet
- Halcyon Brochure RAD10443B 092417Document14 pagesHalcyon Brochure RAD10443B 092417Anonymous 0TOLgQWuHvNo ratings yet