Professional Documents
Culture Documents
Terapia de Oxigeno en Ems
Uploaded by
Julisa FernandezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Terapia de Oxigeno en Ems
Uploaded by
Julisa FernandezCopyright:
Available Formats
5/2/2012
Can Oxygen Really Be Bad?
Keith Wesley, MD
Medical Director
HealthEast Medical Transportation
St. Paul, MN
Oxygen
Oxygen administration is the most
common treatment in prehospital care.
Typically it is the first drug that EMS
providers are taught to administer.
All providers should be highly
proficient with oxygen delivery
equipment.
Tradition
EMS providers administer oxygen during
the initial assessment of patients with
suspected ACS. However, there is
insufficient evidence to support its routine
use in uncomplicated ACS. If the patient is
dyspneic, hypoxemic, or has obvious signs
of heart failure, providers should titrate
therapy, based on monitoring of
oxyhemoglobin saturation, to 94% (Class I,
LOE C).
Oxygen
Less well taught, is the fact that oxygen
is a drug.
Indications
Contraindications
Adverse effects
A dose
An intended duration of administration
Chemistry Warning
I remember being taught as a young
medical student to administer oxygen for
everything from nausea and vomiting to
lower limb fractures.
I was even told at one point that it had
analgesic properties.
I will highlight some research on
supplemental oxygen use in the
prehospital care and discuss
controversies that are arising from the
research.
5/2/2012
Oxygen
Not all chemicals
are bad. Without
chemicals such as
hydrogen and
oxygen, for
example, there
would be no water, a
vital ingredient for
beer.
-Dave Barry
Oxygen
Oxygen is essential
for animal life.
Oxygen
Oxygen
Oxygen:
Diatomic gas
Atomic weight =
15.9994 g-1
Colorless
Tasteless
Third most abundant
element in the
Universe.
Present in Earths
atmosphere at
20.95%.
Oxygen
Oxygen therapy has
always been a major
component of
prehospital care.
Oxygen
In medical school,
in 1983, we only
received a 1 hour
presentation in Year
1 biochemistry on
reactive oxygen
species.
5/2/2012
Oxygen
Now, there are
shelves of
textbooks on the
subject.
The Chemistry of Oxygen
Oxygen is a highly
reactive substance.
It shares electrons
between two atoms
in order to maintain
stability.
Overall, diatomic
oxygen has 2
unpaired electrons.
The Chemistry of Oxygen
Free Radicals:
An atom or group of atoms
that has at least one
unpaired electron and is
therefore unstable and
highly reactive. In animal
tissues, free radicals can
damage cells and are
believed to accelerate the
progression of cancer,
cardiovascular disease,
and age-related diseases.
Oxygen
We are learning that
oxygen is a twoedged sword.
It can be beneficial.
It can be harmful.
The Chemistry of Oxygen
Molecules/atoms
with unpaired
electrons are
extremely unstable
and highly-reactive.
The Chemistry of Oxygen
Reactive oxygen
species (ROS) are a
normal byproduct of
the normal
metabolism of
oxygen.
American Heritage Dictionary
5/2/2012
The Chemistry of Oxygen
The Chemistry of Oxygen
Free radicals, in normal concentrations,
are important in intracellular bacteria
and cell-signaling.
Most important free radicals:
Superoxide (O2-)
Hydroxyl radical (OH)
The Chemistry of Oxygen
The Chemistry of Oxygen
Oxygen produces numerous freeradicalssome more reactive than
others:
Superoxide free radical (O2-)
Hydrogen peroxide (H2O2)
Hydroxyl free radical (OH)
Nitric oxide (NO)
Singlet oxygen (1O2)
Ozone (O3)
The Chemistry of Oxygen
How are free-radicals produced?
Normal respiration and
metabolism.
Exposure to air
pollutants.
Sun exposure.
Radiation
Drugs
Viruses
Bacteria
Parasites
Dietary fats
Stress
Injury
Reperfusion
5/2/2012
The Chemistry of Oxygen
Most cells receive
approximately
10,000 free-radical
hits a day.
Enzyme systems
can normally
process these.
An excess of freeradicals damages
cells and is called
oxidative stress.
The Chemistry of Oxygen
Diseases associated with free-radicals:
Arthritis
Cancer
Atherosclerosis
Parkinsons disease
Alzheimers disease
Diabetes
ALS
Neonatal diseases:
Intraventricular
hemorrhage
Periventricular
leukomalacia
Chronic lung disease /
bronchopulmonary
dysplasia
Retinopathy of
prematurity.
Necrotizing enterocolitis.
The Chemistry of Oxygen
1.8
H2O2 Leakage from
Cardiomyocytes
1.2
1
0.8
The Chemistry of Oxygen
Many of the
changes associated
with aging are
actually due to the
effects of freeradicals.
As we age, the
antioxidant enzyme
systems work less
efficiently.
The Chemistry of Oxygen
So, what does all
this crap mean to
me as an EMS
provider?
1.6
1.4
The Chemistry of Oxygen
Rat
Parakeet
Canary
Lifespan =
3.5 years
0.6
0.4
0.2
0
Lifespan =
21 years
Lifespan =
24 years
5/2/2012
The Chemistry of Oxygen
Oxidative stress
occurs primarily
during reperfusion
not during hypoxia.
Flooding previously
ischemic cells with
oxygen during
reperfusion worsens
oxidative stress.
Reperfusion Injury
Reperfusion injury occurs when
oxygen is reintroduced to ischemic
tissues.
Organs most affected:
REPERFUSION INJURY
Reperfusion Injury
When tissues are reperfused with
oxygen, free-radical species are
produced.
Heart
Kidney
Liver
Lung
Intestine
Reperfusion Injury
Reperfusion injury is particularly
problematic in:
Stroke
Acute coronary syndrome
Trauma
Carbon monoxide poisoning
Cyanide poisoning
STROKE
5/2/2012
Stroke
Reperfusion injury
in stroke:
Free-radical release.
Leukocyte adhesion
and infiltration.
Neuronal breakdown
(leading to more
free-radicals).
Stroke
The brain in stroke is vulnerable to
oxidative stress:
It contains more fatty acids.
It has few antioxidants.
It has high oxygen consumption.
It has high levels of iron and ascorbate
(worse oxidative stress).
Dopamine and glutamine oxidation.
Stroke
Stroke
Lactic acid accumulates in the neurons
as a consequence of ischemic stroke.
The acidic environment has a prooxidant effect:
In 1994, the American Heart
Association Stroke Council concluded
that there were no data to support the
routine use of supplemental oxygen in
patients who had a stroke.
More recently, supplemental oxygen
has been suggested to be potentially
detrimental.
Increased H2O2 conversion.
Superoxide anion converted to
hydroperoxyl radical (HO2).
Increases iron availability for free radical
formation.
Panciolli AM, et al. Supplemental oxygen use in ischemic
stroke patients: does utilization correspond to need for
oxygen therapy. Arch Intern Med. 2002;162:49-52.
Stroke
Stroke
In non-hypoxic patients with minor or
moderate strokes, supplemental
oxygen is of no clinical benefit.
Supplemental oxygen should not
routinely be given to non-hypoxic
stroke victims with minor to moderate
strokes.
Further evidence is needed to give
conclusive advice concerning oxygen
supplementation for patients with
severe strokes.
Portier de la Morandiere KP, Walter D. Oxygen therapy in
acute stroke. Emergency Medicine Journal. 2003;20:547553
Ronning OM, Guldvog B. Should Stroke Victims Routinely Receive Supplemental Oxygen?
A Quasi-Randomized Controlled Trial. Stroke. 1999;30:2033-2037.
5/2/2012
Stroke
Prehospital concerns:
Determine time of onset
(if possible).
Determine glucose
level.
Administer dextrose
ONLY if hypoglycemia
is verified.
Determine oxygenation
status with pulse
oximetry.
Administer
supplemental oxygen if
SpO2 is < 95%.
Avoid IV fluids
(especially dextrosecontaining).
Do not attempt to lower
blood pressure.
Acute Coronary Syndrome
In acute uncomplicated MI, there is no
evidence that supplemental oxygen
reduces mortality. However, there is no
evidence of harm. Further research is
required before changes in clinical
practice should be recommended.
Mackway-Jones K. Oxygen in uncomplicated myocardial infarction. Emerg Med J.
2004;21:75-81.
Myocardial Infarction
There was a non-significant trend
toward increased mortality in the group
that received oxygen.
A caveat of this study is that it took
place in the era before
revascularization therapy.
There have been further studies that
also indicate that there may be limited
benefit from oxygen use.
ACUTE CORONARY
SYNDROME
Myocardial Infarction
In 1976, a randomized controlled trial was
published in the British Medical Journal in
which 157 patients with uncomplicated MI
were randomized to receive either
supplemental oxygen or air for the first 24
hours following onset of symptoms.
There were no significant difference in the
primary outcome of death or the
secondary outcomes of ventricular
dysrhythmia or pain requiring analgesia.
Myocardial Infarction
In 2010-2011 a Cochrane review gave a
strong indication that oxygen may be
harmful in uncomplicated MI.
The review analyzed the 1976 paper
and two other studies from 1997 and
2004, and concluded that the limited
evidence available showed no benefit
and potential harm from oxygen use.
5/2/2012
Myocardial Infarction
On the basis of the Cochrane review,
the AHA recommended in the 2010
Guidelines that supplemental oxygen
no longer be administered to patients
with uncomplicated cardiac chest pain
who have an oxygen saturation greater
than 94%.
POST-CARDIAC ARREST
Post-Cardiac Arrest
Cardiac Arrest
Post-cardiac arrest brain injury is a
common cause of morbidity and
mortality.
68% of out-of-hospital cardiac arrests
23% of in-hospital cardiac arrests
Causes:
Limited tolerance of ischemia
Unique response to reperfusion
Cardiac Arrest
They were stratified into:
Hypoxia (PaO2 less than 60 mmHg)
Normoxia (PaO2 61-299 mmHg)
Hyperoxia (PaO2 greater than 300 mmHg)
The Journal of the American Medical
Association published a study looking
at the partial pressure of oxygen (PaO2)
in arterial blood of patients brought to
the ED following successful
resuscitation by EMS.
The patients were stratified based on
an arterial blood gas taken within 24
hours of hospital admission.
Cardiac Arrest
The study was multicenter and quite large
Enrolled 6,326 patients over five years
Primary outcome was survival to hospital
discharge.
Hyperoxia was a significant independent risk
factor for in-hospital mortality.
The odds ratio for death was 1.8 (95% CI 1.52.2) in the hyperoxia group compared with the
normoxia group.
This was even higher than the odds ratio for
death in the hypoxia group.
5/2/2012
Cardiac Arrest
Correlation does not equal causation
There is a plausible mechanism by which
hyperoxia could cause increased
mortality in patients following cardiac
arrest, and the chance of causation is
great enough to consider limiting the
amount of oxygen given to patients
following cardiac arrest to a sufficient
amount to keep arterial oxygen saturation
94-96%.
RECOMMENDATIONS FROM
THE BRITISH THORACIC
SOCIETY
British Thoracic Society
British Thoracic Society
Do all breathless patients benefit from
oxygen therapy?
Can the routine administration of highdose oxygen to all sick patients have
any harmful effects?
Amongst healthcare professionals there is a widespread
belief that oxygen relieves breathlessness, yet there is no
evidence that this is the case, providing that oxygen levels
in the blood are normal (which is true in many serious
illnesses, even if breathlessness is present). In fact, giving
oxygen when blood saturation levels are normal will
produce hyperoxia which may stimulate reflexes that
actually reduce the blood flow to organs such as the heart
and might therefore reduce the delivery of oxygen to these
vital organs.
Unnecessary oxygen therapy can hinder the
efforts of healthcare professionals by delaying the
recognition of patient deterioration due to the
false reassurance that can be provided by a high
oxygen saturation reading. Additionally, patients
with some lung diseases, such as COPD, are
sensitive to oxygen and an excess can have
harmful consequences.
British Thoracic Society
British Thoracic Society
Oxygen is a treatment for hypoxaemia,
not breathlessness. (Oxygen has not
been shown to have any effect on the
sensation of breathlessness in nonhypoxaemic patients.)
The essence of this guideline can be
summarized simply as a requirement
for oxygen to be prescribed according
to a target saturation range and for
those who administer oxygen therapy
to monitor the patient and keep within
the target saturation range.
10
5/2/2012
British Thoracic Society
The guideline suggests aiming to
achieve normal or near-normal oxygen
saturation for all acutely ill patients
apart from those at risk of hypercapnic
respiratory failure or those receiving
terminal palliative care.
British Thoracic Society
Generally, try to
keep SpO2 between
92-96%.
Treat only
documented
hypoxemia unless
patient critically ill.
Prehospital Implications
PREHOSPITAL
IMPLICATIONS
This presentation has presented
current and cutting edge information
on oxygen usage and oxidative stress.
We dont know where subsequent
science will take us.
Always follow local protocols and
policies in regard to patient care!
Prehospital Implications
Prehospital Implications
Action
WhatCondition
is the status ofStatus
these issues:
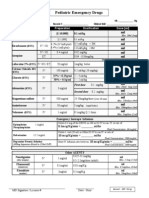
Neonatal Resuscitation
AHA Standard
Room air unless failure after 90
seconds
Stroke
Flux
Use oximetry to guide care
Myocardial infarction
Flux
Use oximetry to guide care
Post-resuscitation management
Flux
Use oximetry to guide care
Trauma
Carbon monoxide
Inadequate Evidence
Flux
Use pulse oximeters
to determine the
need for
supplemental
oxygen and to
monitor oxygen
levels during care.
Practice unchanged. Use pulse
oximetry to guide care
Time dependent
11
5/2/2012
Take Home Message
Oxygen should be
treated like any other
drug.
It has benefits and
risks.
Empiric use is not a
good practice.
Use oximetry to guide
care.
Take Home Message
As this evolves, I
suspect that the
usage of oxygen will
be curtailed in
prehospital care.
It is time to change
from empiric
therapy to focused
therapy.
docwesley@gmail.com
QUESTIONS?
12
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Herman Gendered Restrooms and Minority Stress June 2013Document16 pagesHerman Gendered Restrooms and Minority Stress June 2013Julisa FernandezNo ratings yet
- Campus Sexual Violence - Statistics - RAINNDocument6 pagesCampus Sexual Violence - Statistics - RAINNJulisa FernandezNo ratings yet
- Hands Only CPRDocument7 pagesHands Only CPRJulisa FernandezNo ratings yet
- Validate Rendering Fidelity by Referencing The 1 MV ECG Calibration SignalsDocument1 pageValidate Rendering Fidelity by Referencing The 1 MV ECG Calibration SignalsJulisa FernandezNo ratings yet
- Disrythmia Recognition ACLS ASHIDocument127 pagesDisrythmia Recognition ACLS ASHIJulisa FernandezNo ratings yet
- PediatricResuscMeds HOPUDocument1 pagePediatricResuscMeds HOPUJulisa FernandezNo ratings yet
- Technical Search Considerations - Listening TechniquesDocument41 pagesTechnical Search Considerations - Listening TechniquesJulisa FernandezNo ratings yet
- Technical Search Considerations - Search MarkingsDocument24 pagesTechnical Search Considerations - Search MarkingsJulisa FernandezNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Brachial Plexus InjuryDocument10 pagesBrachial Plexus InjurySanditya FadliNo ratings yet
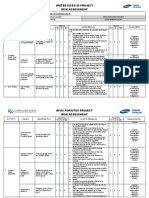
- Apoc Risk Assessment Format - Sesa-Bfim-Ra-Cs-001Document11 pagesApoc Risk Assessment Format - Sesa-Bfim-Ra-Cs-001Abdul WasayNo ratings yet
- Ma Gui Ba Gua Sample Exercise DocumentDocument14 pagesMa Gui Ba Gua Sample Exercise Documentshmoopiebear50% (2)
- Inbound 7714832539582663562Document17 pagesInbound 7714832539582663562Julesbon ParsaliganNo ratings yet
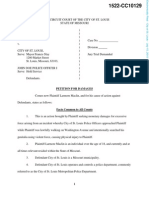
- Maclin SuitDocument5 pagesMaclin Suitnicholas.phillipsNo ratings yet
- 4.b. Medical For Athletes 2Document2 pages4.b. Medical For Athletes 2Mark Era Acson De LunaNo ratings yet
- Pe & Health 6-25-14 PDFDocument432 pagesPe & Health 6-25-14 PDFRomeo D Belnas0% (1)
- Peripheral Nervous System NotesDocument9 pagesPeripheral Nervous System NotesSaoirseNo ratings yet
- Easy Care 2100 User ManualDocument8 pagesEasy Care 2100 User ManualJim BurkeNo ratings yet
- Cerebral HemorrhageDocument10 pagesCerebral HemorrhageJayd Lorenz Vicente ChuanNo ratings yet
- Pathophysiology: A Clinical Approach (2nd Ed.) - Braun Anderson (Chapter 3)Document8 pagesPathophysiology: A Clinical Approach (2nd Ed.) - Braun Anderson (Chapter 3)Mcat NotensionNo ratings yet
- Resume "Something The Lord Made"Document2 pagesResume "Something The Lord Made"Jennifer OngkoNo ratings yet
- Assessment and Management of Unconscious PatientDocument10 pagesAssessment and Management of Unconscious PatientDebasis SahooNo ratings yet
- Chymoral PlusDocument3 pagesChymoral PlusNeha SureshNo ratings yet
- Muscle Activity During The Gait CycleDocument3 pagesMuscle Activity During The Gait CycleMarjorie Walker100% (1)
- Susan Aikens Vs BBC Worldwide Reality Productions (Life Below Zero)Document32 pagesSusan Aikens Vs BBC Worldwide Reality Productions (Life Below Zero)Kyle Hopkins100% (1)
- M/DN MIS Intramedullary Femoral Fixation Surgical TechniqueDocument32 pagesM/DN MIS Intramedullary Femoral Fixation Surgical TechniqueVamby SabidoNo ratings yet
- Damage Control Orthopaedics (DC O: Presented by Specialist of Orthopedic& Traumatology Al-Mahmoudia General HospitalDocument52 pagesDamage Control Orthopaedics (DC O: Presented by Specialist of Orthopedic& Traumatology Al-Mahmoudia General HospitalpaswordnyalupaNo ratings yet
- Flail Chest MP Shah - CcuDocument29 pagesFlail Chest MP Shah - CcuMARTINNo ratings yet
- Gravaboi Codes and NumbersDocument18 pagesGravaboi Codes and NumbersHenrii Arias0% (1)
- Blyton Enid Now For A Story 1948Document193 pagesBlyton Enid Now For A Story 1948athinapolos100% (1)
- Autologous Platelet-Rich Plasma inDocument6 pagesAutologous Platelet-Rich Plasma innoor hidayahNo ratings yet
- Spinal Cord InjuriesDocument17 pagesSpinal Cord InjuriesspinalcordNo ratings yet
- International General Certificate Candidate's Observation Sheet Igc3 - The Health and Safety Practical ApplicationDocument7 pagesInternational General Certificate Candidate's Observation Sheet Igc3 - The Health and Safety Practical Applicationsubhanmusadiq60% (10)
- Spartacus 2x05 - ReckoningDocument52 pagesSpartacus 2x05 - ReckoningJavier de PascualNo ratings yet
- Manual of Neurologic TherapeuticsDocument534 pagesManual of Neurologic TherapeuticsDefault User100% (1)
- The Girl Who Would Be King Chapters 15 16Document6 pagesThe Girl Who Would Be King Chapters 15 16Waddle DeeNo ratings yet
- Case Study On Open Tibial FractureDocument48 pagesCase Study On Open Tibial FractureOmotosho AlexNo ratings yet
- People v. Dalag y Custodio 402 SCRA 254 PDFDocument27 pagesPeople v. Dalag y Custodio 402 SCRA 254 PDFfelix camerinoNo ratings yet
- PLC InjuryDocument5 pagesPLC InjuryTeng HanNo ratings yet