Professional Documents
Culture Documents
Primary (Spontaneous) Upper Extremity Deep Vein Thrombosis
Uploaded by
Jazz ValeryCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Primary (Spontaneous) Upper Extremity Deep Vein Thrombosis
Uploaded by
Jazz ValeryCopyright:
Available Formats
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
OfficialreprintfromUpToDate
www.uptodate.com2016UpToDate
Primary(spontaneous)upperextremitydeepveinthrombosis
Author
KaoruGoshima,MD
SectionEditors
JohnFEidt,MD
JosephLMills,Sr,MD
DeputyEditor
KathrynACollins,MD,PhD,FACS
Alltopicsareupdatedasnewevidencebecomesavailableandourpeerreviewprocessiscomplete.
Literaturereviewcurrentthrough:Feb2016.|Thistopiclastupdated:Feb18,2016.
INTRODUCTIONPrimary,"spontaneous"upperextremitydeepveinthrombosisisrareandisdefinedas
thrombosisofthedeepveinsdrainingtheupperextremityduetoanatomicabnormalitiesofthethoracicoutlet
causingaxillosubclaviancompressionandsubsequentthrombosis.Thesyndromeisappropriatelytermedvenous
thoracicoutletsyndrome,butisalsoreferredtoasPagetSchroettersyndrome,andalternativelyaseffort
thrombosis[1].Ittypicallypresentsinyoung,otherwisehealthyindividualsassudden,severeupperextremity
painandswellingfollowingvigorousupperextremityactivity.Anaggressivetreatmentapproachthatincludes
anticoagulation,catheterdirectedthrombolysisandthoracicoutletdecompressionisaimedatrelievingacute
symptoms,andminimizingcomplicationsincludingrecurrentthromboembolismandpostthromboticsyndrome.
Theepidemiology,riskfactors,pathophysiology,clinicalfeatures,diagnosisandtreatmentofprimary
(spontaneous)upperextremityvenousthrombosiswillbereviewedhere.Catheterinducedupperextremityvenous
thrombosisandlowerextremitydeepveinthrombosisarediscussedelsewhere.(See"Catheterrelatedupper
extremityvenousthrombosis"and"Approachtothediagnosisandtherapyoflowerextremitydeepvein
thrombosis".)
UPPEREXTREMITYANATOMYTheupperextremityveinsaredividedintothesuperficialanddeepvenous
systems(figure1).
SuperficialveinsThemainsuperficialveinsoftheupperextremityincludethecephalic,basilic,median
cubital,andaccessorycephalicveins(figure1).Thebasilicveinisacommonaccesssiteforperformingdigital
subtractionvenography.
DeepveinsThedeepveinsoftheupperextremityincludethepairedulnar,radialandinterosseousveinsinthe
forearm,pairedbrachialveinsoftheupperarm,andaxillaryvein.Theaxillaryveinbecomesthesubclavianveinat
thelowerborderoftheteresmajormuscle(figure2).
ThoracicoutletanatomyThethoracicoutletisboundedbythebonystructuresofthespinalcolumn,firstribs,
andsternum(figure3A).Compressionofthevenousstructuresthattraversethethoracicoutletoccursintwo
distinctspaces:thescalenetriangleandthecostoclavicularspace.
ScalenetriangleTheanteriorborderofthescalenetriangleisformedbytheanteriorscalenemuscle,which
originatesfromthetransverseprocessesofthethirdthroughsixthcervicalvertebrae(C3C6)andinsertson
theinnerbordersandsuperiorsurfacesofthefirstrib.Theposteriorwallofthescalenetriangleisformedby
themiddlescalenemuscle,whicharisesfromthetransverseprocessesofthesecondthroughseventh
cervicalvertebrae(C2C7)andinsertsbroadlyontotheposterioraspectsofthefirstrib.Thesuperiorborder
ofthefirstribformsthebaseofthescalenetriangle.Thetrunksofthebrachialplexusandthesubclavian
arterypassbetweentheanteriorandmiddlescalenemuscles,whilethesubclavianveincourses
anteromedialtothescalenetriangle(figure3B).
CostoclavicularspaceThecostoclavicularspacecomprisestheareabetweenthefirstribandtheclavicle.
Thebrachialplexus,subclavianarteryandsubclavianveinpassthroughthisspace.Thesubclavianveinis
mostlikelytobecompressedatthissite.
PATHOGENESISPrimaryupperextremitydeepveinthrombosisisdefinedasthrombosisofthedeepveins
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
1/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
drainingtheupperextremityduetoanunderlyinganatomicanomalyatthethoracicoutletcausingcompressionor
repetitiveinjurytotheunderlyingaxillosubclavianvein[25].Primaryupperextremitydeepveinthrombosisisa
manifestationofvenousthoracicoutletsyndrome(vTOS).(See"Overviewofthoracicoutletsyndromes",section
on'VenousTOS'.)
Thrombosisoftheveinsdrainingtheupperextremitywasoriginallypostulatedtobethecauseofacutearmpain
andswellingbyPaget[6],andlaterVonSchroetterrelatedtheclinicalsyndromespecificallytotheaxillaryand
subclavianveins[7].ThisclinicalentitywasreferredtoasPagetSchroettersyndrome[8].Inthemid20thcentury,
thetermeffortthrombosiswascoined[9],duetothefactthatthesyndromeoftenoccurredinphysicallyactive
individualsafterunusuallystrenuoususeofthearmandshoulder[1012].Theterm"spontaneous"upperextremity
venousthrombosishasalsobeenusedhighlightingtheoftendramaticpresentationinanotherwisehealthy,young
individual.Forthepurposesofourdiscussion,wewillrefertothesyndromeasprimaryupperextremitydeepvein
thrombosistodistinguishitfromsecondarycauses,whichareassociatedwithincitingfactorssuchasindwelling
cathetersorprothromboticstates.(See"Catheterrelatedupperextremityvenousthrombosis".)
Anatomicabnormalitiesofthethoracicoutletthatresultincompressionoftheveincanbecongenitaloracquired.
Congenitalanomaliesconsistofcervicalribs,supernumerarymuscles,abnormaltendoninsertionsorabnormal
muscularortendinousbands[13,14].Acquiredabnormalitiesincludebonyovergrowthduetobonyfracture(eg,
clavicle,firstrib)[1518],orhypertrophyofanteriorscalenemuscleorsubclaviusmuscles,oftenrelatedto
repetitivelifting.Theabnormalitiesofthethoracicoutletareoftenbilateral,andbilateralprimaryupperextremity
deepveinthrombosishasbeenreported[19,20].Anatomicabnormalitiesnarrowthescalenetriangle,ormore
commonlythecostoclavicularspace,predisposingtheveintocompressionbetweenthefirstribandmuscleor
tendon(figure3AB),orbetweenanomaloustendoninsertions.Lesscommonly,compressionoftheveinbetween
theclavicleandacervicalribcanoccur,andpartialocclusionoftheveinbyacongenitalwebhasalsobeen
reported[13,14].(See'Thoracicoutletanatomy'above.)
Undersomecircumstances,itappearsthatananatomicabnormalityisnotnecessarytoproduceinjurytothevein.
Extremesinrangeofmotionoftheupperextremitycanleadtomovementoftheclaviclerelativetothefirstrib
sufficienttocausevenouscompression.Repetitiveoverheadarmmovementsorhyperabductionandexternal
rotationoftheshoulderaremostoftenimplicated[2123].Repetitiveinjurycausesperivenousfibrosis,which
eventuallyleadstothrombosis.Itisimportanttorecognizethatthepatientoftenpresentswithacuteonsetof
symptomsrelatedtothethrombosis,buttheunderliningproblemmaybeachronicrepetitiveinjurythathad
narrowedthevein.
EPIDEMIOLOGYANDRISKFACTORSUpperextremitydeepveinthrombosis(allcauses)represents1to4
percentofallcasesofdeepveinthrombosis[24].Primaryupperextremitydeepveinthrombosisisrarewithan
estimatedannualincidenceof1to2casesper100,000population[10,24].Themajorityofcasesofupper
extremitydeepveinthrombosisaresecondaryandrelatedtocentralvenouscannulation(eg,centralline,
pacemaker)orprothromboticstates(eg,thrombophilia,malignancy)[1,10,25,26](See"Catheterrelatedupper
extremityvenousthrombosis".)
Between60and80percentofpatientswithprimaryupperextremitydeepveinthrombosisreportahistoryof
exerciseorstrenuousactivityinvolvingusuallythedominantupperextremitypriortotheonsetofsymptoms.
Strenuousactivitiesincludeweightlifting,rowing,oractivitiesinvolvingrepetitiveoverheadarmmovements,
particularlyhyperabduction,suchaspitching[1,27,28].Theaverageageatpresentationisintheearlythirtiesand
themaletofemaleratiois2:1[1].Apredominanceofrighthandedindividualsmayexplainwhytheright
axillosubclavianveinismorecommonlyaffected.(See'Pathogenesis'above.)
RiskfactorsRiskfactorsforprimaryupperextremitydeepveinthrombosisincludethefollowing[1,10,2530]:
Youngerage
Athleticmuscularmale
Strenuousupperextremityactivity
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
2/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Repetitiveoverarmhyperabduction
Anatomicabnormalitiesofthethoracicoutlet(congenital,acquired)
Thrombophilia
CLINICALPRESENTATIONSPrimaryupperextremitydeepveinthrombosiscanpresentacutelywith
symptomsandsignsofupperextremitydeepveinthrombosisorpulmonaryembolism,orwithchronicor
intermittentsymptoms.
AcuteupperextremitydeepveinthrombosisAcutepresentationsareduetosuddenthrombosisofthe
axillosubclavianvein.
Theclassicpresentationisthatofayoung,athleticmalepresentingwithacuteonsetofupperextremitypainand
swellinginthedominantarmfollowingaparticularlystrenuousactivity[1,27,28].Strenuoususeofthearmpriorto
theonsetofextremityswellingorpainisrecalledin40to80percentofpatients,andsymptomsaregenerally
noticedwithin24hoursofthestrenuousactivity[10,11,23,31].Themajorityofpatients(70to80percent)manifest
withvariabledegreesofneck,shoulder,oraxillarydiscomfort,armheavinessandpainassociatedwithcomplaints
ofupperextremityswelling[32,33].Swellingandpaintypicallyimprovewithrestandelevationofthearmtothe
leveloftheheart,whereaselevationoftheextremityoverheadmayaggravatethesymptoms[34].
Physicalexaminationgenerallyrevealsedemaoftheaffectedextremity,oftenaccompaniedbycyanosisofthe
handandfingers.Thepatientmayalsohavealowgradefever.Apalpablevenouscord(superficial
thrombophlebitis)maybeapparentinassociatedsuperficialveins(eg,proximalcephalicvein).Dilated
subcutaneouscollateralveins,alsoknownasUrschelssign,maybenoticeableovertheupperchestandproximal
upperextremity,particularlyinthosewithanunderlyingchronicvenousstenosis[11,27,32].
Theupperextremityarterialvascularexaminationshouldbenormal.Reducedarterialbloodflowduetovenous
congestion(phlegmasiaceruleadolens)israreinthelowerextremityandevenmoresointheupperextremity
[35,36].However,ifpresent,itrepresentsanemergencyandindicatestheneedforemergenttreatment.(See
'Thrombolytictherapy'below.)
Coexistentsignsrelatedtobrachialplexuscompression(ie,neurogenicthoracicoutletsyndrome)maybepresent,
manifestingasparaesthesiasorpainintheulnarnervedistribution,tendernessoverthesupraclavicularfossa,and
wastingoftheintrinsichandmuscles.(See"Overviewofthoracicoutletsyndromes",sectionon'Clinical
evaluation'.)
AcutepulmonaryembolismInadditiontoupperextremityswellingandpain,upperextremitydeepvein
thrombosiscaninitiallypresentassymptomaticorasymptomaticpulmonaryembolism[12,28,33,3741].The
clinicalfeatures,diagnosisandtreatmentofpulmonaryembolismarediscussedindetailelsewhere.(See
"Overviewofacutepulmonaryembolisminadults".)
ChronicorintermittentsymptomsInpatientswithpartialthrombosisorchronicvenousstenosisdueto
repetitiveinjurythatcausesactivityrelatedobstruction,symptomsmaybeintermittentandlesssevere.Ifvenous
occlusiondevelopsoveraprotractedperiodoftime,edemaorpainmaybeminimal,andincreasedvenous
collateralflowoverthechest(Urschelssign)maybetheonlyclinicalsignthatisapparent[11,27,32,42].
DIAGNOSISAdiagnosisofupperextremityvenousoutflowobstruction(ie,deepveinthrombosisorvenous
stenosis)maybesuspectedbasedupontheclinicalpresentation,butshouldbeconfirmedwithimaging,typically
initiallyusingultrasound.Ddimerisusefulforexcludingthrombosisasanetiology,butwillnotexcludevenous
stenosiswithoutthrombosisasasourceofsymptoms.Onceadiagnosisofvenousoutflowobstructionis
established,aprimaryetiologyshouldbesoughttoidentifytheunderlyinganatomicabnormalitythatisthesource
oftheobstruction.Weobtainaplainchestradiographonallpatientstoidentifyanyobviousbonyabnormalities
however,moreadvancedimagingmaybeneededtodemonstrateabnormalmuscularattachments.Itisimportant
toassesscontralaterallimbinvolvementbecauseabouthalfofpatientswillhavesomedegreeofcontralateral
venousobstruction,evenintheabsenceofsymptoms.(See'Pathogenesis'above.)
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
3/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
DdimerPlasmaDdimer,whichisadegradationproductofcrosslinkedfibrin,maybeelevatedinpatients
withupperextremitydeepveinthrombosis,asinthosewithotherlowerextremitydeepveinthrombosisor
pulmonaryembolism.However,althoughaplasmaDdimer>500g/Lissensitiveforthrombosis,andhasahigh
negativepredictivevalue,itisnotspecificfortheanatomiclocationofthethrombosis,andwillnotexcludevein
compression/stenosisasasourceforsymptoms[43].
VenousoutflowobstructionBmodeultrasound,colorDopplerultrasound,andduplexultrasoundhavebeen
usedextensivelyinthediagnosisofdeepveinobstruction.NoncompressibilityoftheveinonBmodeultrasound
withorwithoutvisibleintraluminalthrombusisthemajorcriterionforthediagnosisofvenousthrombosis.Weuse
duplexultrasoundastheinitialtestfordiagnosingupperextremityvenousoutflowobstructionbecauseitis
noninvasive,inexpensive,andinobservationalstudies,hasanacceptablesensitivityandspecificityforthe
diagnosisofupperextremitydeepveinthrombosis[33,4451].Asystematicreviewevaluated17studies,
concludingthatcompressionultrasonographyisanacceptablealternativetostandardcontrastvenography[44].
Thesummaryestimatesofthesensitivityofcompression,Dopplerultrasound,andDopplerultrasoundwith
compressionwere97,84,and81percent,respectively,andspecificitieswere96,94,and93percent,
respectively.Disadvantagesofultrasoundarethatitistechniciandependent,andthatnonocclusivemural
thrombusandthrombusintheproximalsubclavianorinnominateveinsmaynotbeadequatelyseenasaresultof
acousticshadowingbytheoverlyingclavicleandsternum[50,52,53].However,proximalsubclavianvein
obstructionislesstypicalofprimarycausesofupperextremityvenousoutflowobstruction,whichtendtoaffect
themidtodistalsubclavian/proximalaxillaryveinatthethoracicoutlet.Whenacousticshadowingisaproblem,
venousthrombusorstenosismoreproximaltotheplacementoftheultrasoundprobecanbeinferredfrom
abnormalrespiratoryvariation,abnormalaugmentation,andabnormalDopplerflow.
Althoughstandardcatheterbased(digitalsubtraction)venographyprovidesthebestdefinitionofabnormalvenous
anatomyandisthestandardwithwhichothermodalitiesarecompared[44,54],itisgenerallynotneededto
establishadiagnosisofupperextremitydeepveinthrombosis.Venographyrequirescannulationofaperipheral
veinoftheaffectedupperextremity,whichcanbechallenginginthefaceofsignificantextremityedema,andthe
studyrequiresasubstantialintravenouscontrastload.Assuch,catheterbasedvenographyisgenerallyreserved
forsituationswherenoninvasivestudiesareequivocal,butclinicalsuspicionremainshighforaprimarycauseof
venousoutletobstruction[1].Forpatientswithintermittentorchronicsymptoms,extrinsiccompressionofthevein
canbedemonstratedduringcatheterbasedvenographybyperformingdynamicstudiesthatplacethearmin
variouspositionsduringthestudy.Thevenogrammaybenormalatrestbutabnormal(varyingdegreesofextrinsic
compressionwithnewvenouscollaterals)witharmabductionhowever,veincompressionwitharmabduction
canbeanormalvariant[55]Bonyabnormalitiesmayalsobeseenwithfluoroscopicimagingduringcatheterbased
venography,butabnormalfibrousbandsormuscleinsertionswillnot.
Lessinvasivemethodsofvenographyincludecomputedtomographic(CT)andmagneticresonance(MR)
venography[53,5658].Thesemodalitiesarenottypicallyusedtoestablishadiagnosisofupperextremityvenous
outflowobstruction.Rather,thesestudiesaremoreusefulforidentifyinganatomicabnormalitiesandother
secondarycausesfordeepveinthrombosis(eg,tumor).(See'Anatomicabnormalitiesofthethoracicoutlet'
below.)
CTvenographycanbeusedtoconfirmorexcludecentralveinthrombushowever,likecatheterbased
venography,substantialcontrastloadsarerequired.CTvenographyhasnotbeenstudiedsufficientlyto
determineitssensitivityandspecificity.Asmallstudyof18patientscomparedCTvenographyanddigital
subtractionvenographyfortheirabilitytodiscriminatetheseverityandextentofvenousobstruction,the
causeofupperextremitydeepveinthrombosis,andimplicationsfortheplanningoftreatment[58].CT
venographywasfelttoprovidemoreinformationthandigitalsubtractionvenography,andinhalfofthe
patients,thefindingsofCTvenographychangedthetreatmentplan.
ContrastenhancedMRimagingisveryspecificinitsabilitytoimagesubclavianveinthrombosis,butits
sensitivityforthrombosisistoolowtobeausefulscreeningmodality[53].However,withproperprotocol
anddynamicsequencing,contrastenhancedthreedimensional(3D)MRangiographyisanexcellent
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
4/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
noninvasivealternativetovenogram[59].Onemustrememberthatanatomiccompressionofvascular
structuresinthoracicoutletiscommonandpositivefindingsandthepresenceofpathologicalfindingsmust
beclinicallycorrelated.
AnatomicabnormalitiesofthethoracicoutletOnceadiagnosisofupperextremityvenousoutflow
obstructionisestablished,furtherimagingshouldbeperformedtoidentifyaprimarycauseforthrombosis,suchas
cervicalribs,supernumeraryribs,abnormalbandsorabnormalmuscleinsertions.Foranypatientsuspectedof
havingaprimarycauseforupperextremitydeepveinthrombosisorstenosis,weobtainaplainchestfilmto
identifyanybonyabnormalities[60].Ideally,theanatomicabnormalityshouldbeidentifiedpriortothoracicoutlet
decompressionhowever,thisisnotalwayspossible.Attimes,theanatomicabnormalitymaynotbeapparent
untilthetimeofsurgicalexploration.(See'Thoracicoutletdecompression'below.)
Althoughcomputedtomography(CT)andmagneticresonance(MR)imagingarelessappropriateinitialstudiesfor
screeningpatientssuspectedofhavingupperextremitydeepveinthrombosis,thesestudiesprovidemore
anatomicdetailandshowtherelationshipofvenousstructurestothesurroundingboneandmuscle.CTandMRI
alsoallowtheassessmentofcentralvenousstenosisorocclusion,whichcanbemissedbyultrasounddueto
acousticshadowingfromoverlyingbonystructures.Inaddition,lessobviousbonyabnormalitiescanbeseenon
thesestudies,andattimes,venouscompressionrelatedtobonyormuscularabnormalitiescanalsobeseen.
Intheabsenceofanobviousbonyanatomicabnormality,aprimarycauseforthethrombosisorvenousstenosis
canbepresumedintheyoung,otherwisehealthy,activeindividualwithaclassicpresentationwhodoesnothave
ahistoryofcentralvenousinstrumentationorothermedicalproblemsassociatedwithsecondaryetiologiesfor
venousoutflowobstruction.Thespecificabnormalitymaynotbedetermineduntilthetimeofsurgicalexploration.
(See'Approachtotreatment'below.)
DIFFERENTIALDIAGNOSISThedifferentialdiagnosisforupperextremityedemanotrelatedtoprimaryupper
extremitydeepveinthrombosisincludesedemarelatedtootheretiologies,secondarycausesofvenous
thrombosis,andlymphedema.
Primaryupperextremitydeepveinthrombosiscanbedistinguishedfromsecondarycausesbytheabsenceof
venousinstrumentation,ayoung,otherwisehealthypatientdemographic,andamoretypicallysuddenonsetof
symptoms.Theclinicalfeaturesofupperextremitydeepveinthrombosisareotherwisesimilarandincludeupper
extremityedemaandpain,andcyanosisoftheskinduetovenouscongestion.Upperextremitydeepvein
thrombosisthatoccursintheabsenceofinstrumentationandwithnoidentifiableanatomicabnormalitiesorother
riskfactorsforvenousthrombosis(eg,oralcontraceptives)raisesaconcernofoccultmalignancy.Upto25
percentofpatientswillbediagnosedwithinoneyearofavenousthromboembolicevent[33,61].Ifaprimarycause
forupperextremitydeepveinthrombosisisnotimmediatelyapparentonimagingstudies,thepatienthasno
historyofinstrumentation,andthepatienthasnoneoftheriskfactorslistedaboveforprimaryupperextremity
deepvenousthrombosis,wesuggestamoreformallaboratoryevaluationtoruleoutsecondarycausesforupper
extremitydeepveinthrombosis,includingcoagulationstudies,whichshouldbedrawnpriortotheinitiationof
anticoagulation.(See"Screeningforinheritedthrombophiliainasymptomaticindividuals"and"Riskandprevention
ofvenousthromboembolisminadultswithcancer".)
Patientswithvenousthrombosisduetocompressionofstructuresofthethoracicoutletmayalsohavesymptoms
attributabletothearterialorneurologicstructuresthatpassthroughthisspace.Distinguishingbetween
neurogenic,arterial,andvenousthoracicoutletsyndromeisdiscussedelsewhere.(See"Overviewofthoracic
outletsyndromes",sectionon'Clinicalevaluation'.)
Therearemanycausesofextremityedemathatarenotrelatedtovenousobstruction.Themedicalhistorywill
usuallygiveaclueastothepotentialetiologyforedema(eg,historyofheartfailure).Althoughsystemicetiologies
typicallypresentwithbilateralextremityedema,thisfeatureisnothelpfulgiventhatanatomicabnormalitiesofthe
thoracicoutletarecommonandpatientswithprimaryupperextremitydeepveinthrombosiscanpresentwith
bilateralsymptoms.Routinelaboratorystudiestypicallyimportantintheevaluationofpatientswithextremity
edemaincludeacompletebloodcount,electrolytes,andliverfunctiontests.Thesestudiesmaypointtoan
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
5/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
alternativeetiologyforupperextremityedema.Thegeneralapproachtothepatientwithedemaisdiscussedin
detailelsewhere.(See"Pathophysiologyandetiologyofedemainadults"and"Clinicalmanifestationsand
diagnosisofedemainadults".)
Upperextremityarmswellingcanbeduetolymphedemahowever,swellingfromacutevenousthrombosishasa
moreabruptonsetandanantecedentriskfactorsuchasprioraxillarylymphnodedissectionislacking.(See
"Clinicalfeaturesanddiagnosisofperipherallymphedema".)
APPROACHTOTREATMENTThegoalsoftreatmentofprimaryupperextremitydeepveinthrombosisare
relievingsymptomsrelatedtovenousobstruction,preventingcomplicationsofdeepveinthrombosis,and
preventingrecurrentthrombosis[62].Treatmentoptionsincludeanticoagulation,thrombolysis,andsurgical
decompressionofthethoracicoutlet.Notreatmentorcombinationoftreatmentshasbeenrigorouslyevaluatedfor
thetreatmentofupperextremitydeepveinthrombosis.Asaresult,recommendationsarebaseduponavailable
retrospectivestudiesandindirectevidenceprovidedfromtheexperiencewithdeepveinthrombosisofthelower
extremity[1].
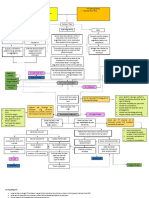
Ourapproachtotreatmentisasfollows:
WeagreewithguidelinesfromtheAmericanCollegeofChestPhysiciansthatrecommendanticoagulation
foraminimumofthreemonthsforallpatientsidentifiedwithupperextremitydeepveinthrombosis[63].(See
'Anticoagulation'below.)
Forpatientswithprimaryupperextremityaxillosubclaviandeepveinthrombosiswithsuddenonset,
moderatetosevereupperextremitysymptomsoflessthantwoweeksduration,wesuggestthrombolysisto
eliminatethrombustotheextentthatispossible.Lysisislesseffectivewhensymptomshavebeenpresent
formorethantwoweeks.(See'Thrombolytictherapy'below.)
Forgoodrisksurgicalpatientsidentifiedwithanatomicabnormalitiesofthethoracicoutletcausing
symptomaticvenouscompression,wesuggestthoracicoutletdecompression.Thespecificprocedureis
targetedtothetypeofabnormalityidentified.Forthoseinwhomaspecificabnormalityhasnotbeen
identified,weperformfirstribresection,providedthatasecondarycauseofupperextremityvenous
thrombosisisnotpresent.
Anticoagulationalone(nothrombolysis)withorwithoutthoracicoutletdecompressionmaybeappropriatefor
patientswithmildsymptoms,intermittentsymptoms,andthosewhopresentinadelayedmanner(>2
weeks).Thenaturalhistoryofthesepatientsisunclear.(See'Symptomaticcare'belowand'Anticoagulation'
below.)
RationaleforaggressivetreatmentAnaggressiveapproachthatincludesacombinationofthrombolysisand
thoracicoutletdecompressionwithorwithoutvenoplasty(percutaneous,open)appearstoimprovelongterm
outcomesinpatientswithprimaryupperextremitydeepveinthrombosis,particularlythosewithacute,moderate
toseveresymptoms[6485].Withanaggressiveapproach,successratesforreestablishingsubclavianvein
patencyarenearly100percentprovidedthatthrombolysisisperformedwithintwoweeksoftheonsetof
symptoms[8688].Althoughearlyinterventionisadvocated,patientswithprimaryupperextremitydeepvein
thrombosiswhopresentlaterthantwoweeksmayalsobenefitfromthoracicoutletdecompression(no
thrombolysis)giventhehighratesofrecurrentthrombosisandlongtermmorbidityassociatedwithanticoagulation
alone[3,22,89,90].
Inaworldwideclinicalseriesof606patientswithprimaryupperextremitydeepveinthrombosis,early
thrombolysisandfirstribresectionprovidedthebestoutcome,with95percentofthesurgicalcohortexperiencing
anexcellentclinicaloutcomecomparedwith29percenttreatedconservatively,whichconsistedofanticoagulation,
armelevation,andupperextremitycompression[27].Residualvenousobstructionwaspresentin78percentof
patients.Theclinicaloutcomesassociatedwithanticoagulationalonewereevaluatedinalaterseriesof54
patients,nearlyallofwhomweretreatedwithwarfarin[21].Afterameanfollowupoffiveyears,22percenthad
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
6/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
persistentseverevenousoutflowobstructiononfollowupultrasound.About50percentofthepatientswere
asymptomatic,but13percenthadsevereordisablingsymptoms.Subsequentpulmonaryembolismwas
documentedin26percentandwassymptomaticinonethirdofthepatients.Bycomparison,amongpatients
treatedwiththrombolysis(withoutthoracicoutletdecompression),76percentwereasymptomaticafteramean
followupof55months[21,86].Inotherretrospectivereviews,persistentsymptomsanddisabilityoccurredin41
to91percentofpatientstreatedconservatively[1,27].
Firstribresectionwithoutpreoperativethrombolysishasbeenproposedforthemanagementofprimarysubacute
venousthrombosis.Intheretrospectivereview,45of110patientsunderwentpreoperativethrombolysisaloneor
thrombolysisandballoonvenoplastypriortothoracicoutletdecompression.Theremaining65patientswere
treatedwithanticoagulationalonepriortothoracicoutletdecompression.Upto80percentofoccluded
axillosubclavianveinsrecanalizedduringthefollowupperiodintheanticoagulationgroup,andtheoverallratesof
venouspatencyweresimilarbetweenthegroups[89].
RecommendationsofothersOurrecommendationsareingeneralagreementwiththeguidelinesfromthe
AmericanCollegeofChestPhysicians(ACCP)however,theACCPsuggestsanticoagulanttherapyaloneover
thrombolysisforpatientswithacuteupperextremitydeepveinthrombosisthatinvolvestheaxillaryormore
proximalveins[63].Theyfurtherstatethatpatientsarelikelytochoosethrombolytictherapyoveranticoagulation
aloneiftheyaremorelikelytobenefitfromthrombolysis,haveaccesstocatheterbasedtherapy,attachahigh
valuetothepreventionofpostthromboticsyndrome,andattachalowervaluetotheinitialcomplexity,cost,and
riskofbleedingwiththrombolytictherapy.Thisrecommendationdoesnotdistinguishbetweenprimaryand
secondarycausesofupperextremitydeepveinthrombosisdirectlyhowever,giventhatpatientswithprimary
upperextremitydeepveinthrombosisaremorelikelytobenefitfromthrombolysiscomparedwithpatientswith
secondarycausesofdeepveinthrombosis,wesupportamoreaggressivetreatmentstrategy.(See'Rationalefor
aggressivetreatment'above.)
INITIALMANAGEMENTPatientswhoarediagnosedwithprimaryupperextremitydeepveinthrombosisare
initiallymanagedwithmeasurestoimprovetheircomfortandareanticoagulated.Anticoagulationhelpstomaintain
patencyofcollateralveinsandreducespropagationofthrombus.Anticoagulanttherapywithheparinorwarfarinis
alsoeffectiveinpreventingpulmonaryembolismwithlowerextremityvenousthrombosis,andbyextrapolation,
mayalsopreventembolismfromupperextremitydeepveinthrombosis[28,63].Thedecisiontoproceedwith
thrombolysisorthoracicoutletdecompressionisbaseduponsymptomseverityandthetypeofassociated
anatomicabnormality.(See'Approachtotreatment'above.)
SymptomaticcareSymptomaticcareofphlebiticsymptomsrelatedtoupperextremitydeepveinthrombosis
includesupperextremityelevation,andnonsteroidalantiinflammatorydrugs(NSAIDs)forpainmanagement.
Armelevationshouldhelpreduceupperextremityswelling.Graduatedcompressionstockingshavebeenshownto
reducetherateofpostthromboticsyndromeinpatientswithlowerextremitydeepveinthrombosis,andmayalso
bebeneficialinpatientswithupperextremitydeepveinthrombosis[33].However,compressionislikely
unnecessaryintreatedpatientsforwhomthelesioniscorrectedandedemahasresolved.
AnticoagulationWeagreewithguidelinesfromtheAmericanCollegeofChestPhysiciansthatrecommend
parenteralanticoagulation(eg,lowmolecularweightheparin,fondaparinux,intravenousunfractionatedheparin,
subcutaneousunfractionatedheparin)forallpatientswithaxillosubclavianveinthrombosis[63].Inourpractice,we
beginparenteralanticoagulationonceadiagnosisofdeepveinthrombosisismadebutafteranynecessary
laboratoryteststoevaluateforhypercoagulablestateshavebeenobtained.
Thechoiceofinitialparenteralagentforanticoagulationinpatientswithprimaryupperextremitydeepvein
thrombosisdependsupontheneedforfurthertreatmentintheformofthrombolysisorthoracicoutlet
decompression.Forpatientswithmild,intermittent,orchronicsymptomswhowillbemanagedonanoutpatient
basis,lowmolecularweightheparin(LMWH)orfondaparinuxcanbeinitiatedtobridgetolongtermtherapyina
similarfashionasthosewithlowerextremitydeepveinthrombosis[63,9193].(See"Overviewofthetreatmentof
lowerextremitydeepveinthrombosis(DVT)".)
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
7/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Whenthrombolysisisanticipated,weadministerunfractionatedheparin,andmaintaintherapeuticlevels(aPTT1.5
to2.5timescontrol)untilthrombolysisisinitiated.Duringthrombolysis,thedoseofheparinshouldbeloweredto
minimizebleedingcomplications,butoncethrombolysisiscompleted,fullanticoagulationcanberesumed[94,95].
Similarly,thedoseofheparinshouldbeloweredaroundthetimeofsurgicalintervention.Onceanynecessary
interventionsarecompleted,bridginganticoagulationcanbeusetotransitiontolongtermtherapyinanticipationof
discharge.(See"Perioperativemanagementofpatientsreceivinganticoagulants",sectionon'Bridging
anticoagulation'.)
AdmissionandreferralManypatientswithacute,severesymptomsrelatedtoprimaryupperextremitydeep
veinthrombosiswillrequireadmissiontomanagesymptomsandinanticipationofthrombolytictherapyand/or
surgicaldecompression.
Thereisno"onesizefitsall"approachtothetreatmentofprimaryupperextremitydeepveinthrombosis.
Individualizedcarerequiresateamofspecialistswithsufficientexperienceandreadilyavailableresourcesand
ancillarypersonnel.Suchteamsarerareoutsidetertiaryreferralcenters,andthus,referraltoavascularcenter
withsuchateamisappropriate[69,96].
Initialoutpatientanticoagulationandoutpatientreferralforpossiblefurthertreatmentmaybeappropriatefor
patientswith:
Minimalsymptoms
Delayedpresentationmorethantwoweeksaftertheonsetofsymptoms
Intermittentsymptomsduetovenousobstructionwithoutthrombosis
THROMBOLYTICTHERAPYTheaimofthrombolytictherapyispromptdissolutionofthrombustominimize
inflammationandendothelialinjuryandtorestoreveinpatency,whichreducesextremityedemaandassociated
symptoms[28,85,97,98].Thrombolytictherapyappearstohavethemostbenefitforpatientswhopresentwith
acute,moderatetoseveresymptomsrelatedtosuddenaxillosubclavianthrombosis.Inourexperience,thrombi
thathavebeensymptomaticforuptotwoweekshaveareasonablechanceoflysiswithcatheterdirectedinfusion
ofalteplasedirectedintothethrombus.Thrombolysisrestoresveinpatencyin64to84percentofpatients,with
betterpatencyratesassociatedwithearlierinitiationoflytictherapy[85].However,evenaftersuccessfullysis
thatrestoresveinpatency,uptoonethirdofpatientswillreocclude[1,85].(See'Rationaleforaggressive
treatment'above.)
Thegeneralcontraindicationstothrombolytictherapyaregiveninthetable(table1).Wedonotperform
thrombolysisinpatientswithonlypartialthrombosis,orthosewithmildacuteorchronic,intermittentsymptoms.
Symptomaticpatientswhopresentmorethantwoweeksaftertheonsetofsymptomsarelesslikelytobenefit
fromthrombolysisduetotheorganizednatureoftheclotandinflammatorychangesinthevein.
Observationalstudieshaveshownthatcatheterdirectedpharmacologicthrombolysis,whichinvolvesembedding
aninfusioncatheterintotheaxillosubclavianveinthrombus,achieveshigherratesofclotdissolutioncompared
withsystemicinfusionandrequiresanoveralllowerdoseandshorterdurationoflysis,whichreducesbleeding
complications[28,85,98].
Catheterdirectedpharmacologicupperextremitythrombolysisisperformedinthefollowingmanner:
Thebasilicveinoftheaffectedlimbisaccessedusingultrasoundguidance.
Aguidewireandcatheterareusedtotraversethethrombosedaxillosubclavianvein.
Amultisideholeinfusioncatheterisembeddedwithinthethrombusandinfusionofalteplaseinitiatedat0.01
mg/kg/hour[85,99].Alternatively,urokinase(notavailableintheUnitedStates)canbeused[100].
Thecatheterissuturedintoposition,andthepatienttransferredtoamonitoredsettingtomonitorforany
bleedingcomplications.Theprogressofthrombolysisisevaluatedbyperformingvenographyat12hours,
andagainat24hoursifnecessary.Atotaldoseof20to25mgalteplasecanbesafelyusedinmostcases.
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
8/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Forpatientsundergoingcatheterdirectedorsystemicthrombolysis,aspirinshouldbeadministeredalongwith
unfractionatedheparinduringinfusionofthethrombolyticagenttocounteractplateletactivationand
potentiallyincreasedthrombogenicitythatmaybeinducedwithlytictherapy[33].
Mechanicalthrombolysis(eg,AngioJet,EKOScatheter)isoftenusedincombinationwithpharmacologic
thrombolysis[101].Therearelimiteddatainvolvingtheuseofthesedevicestotreatupperextremitythrombosis.
However,baseduponavailableresultsforlowerextremitydeepveinthrombosis,thesetreatmentsmaybeuseful
inupperextremitythrombosistorapidlyextractalargeburdenofthrombusandreducetheoveralldoseand
durationoflytictherapy[102].
Oncevenouspatencyhasbeenreestablishedwithcatheterdirectedthrombolysis,itisimportanttoevaluatethe
residualaxillosubclavianveinforpersistentcompressionorstenosis.Occasionally,adjunctivepercutaneous
transluminalangioplasty(PTA)followingsuccessfulthrombolysisisneededtoopentheveinsufficientlysothat
anticoagulanttreatmentcanmaintainpatencyuntilthoracicoutletdecompressioncanbeperformed[1].(See
'Venoplasty'belowand'Thoracicoutletdecompression'below.)
THORACICOUTLETDECOMPRESSIONForpatientswithprimaryupperextremityaxillosubclaviandeep
veinthrombosis,andselectedpatientswithaxillosubclavianvenouscompression/stenosis,observationalstudies
supportsurgicaldecompressionofthethoracicoutlet,whichprovidesthelowerratesofrecurrent(orfuture)
thrombosis,andreducedlongtermmorbiditycomparedwithmoreconservativemanagement[1,27].(See
'Rationaleforaggressivetreatment'above.)
Thoracicoutletdecompression,whichmayincludeanyoneofacombinationoftheproceduresdiscussedbelow,
isindicatedforgoodrisksurgicalpatientswithanyofthefollowingpresentations[1,27,64,103,104]:
Patientswhopresentwithacute,moderatetoseveresymptomsduetoprimaryupperextremity
axillosubclavianthrombosis,followingthrombolysis.
Symptomaticpatients(intermittentorrecurrent)withathoracicoutletanatomicabnormalitycausingvenous
compression/stenosis.Objectiveevidenceofvenousthrombosismayormaynotbepresent.
Thoracicoutletdecompressionmaybeindicatedinpatientswithsymptomaticsubacute(>2weeks)or
symptomaticchronicthrombosis[89].
Followingsuccessfulthrombolysis,somecliniciansfavoranticoagulationforonetothreemonthstoallow
endothelialhealingandresolutionofacuteinflammationbeforethoracicoutletdecompression[64].However,given
theriskofrethrombosis,weagreewiththemajorityofsurgeonsinadvocatingsurgicaldecompressionduringthe
samehospitalizationasthrombolytictherapy[1,3,96].Regardlessofthetimingofsurgicaldecompression,
anticoagulationismaintaineduntilthesurgerycanbeperformed.(See'Anticoagulation'above.)
Forpatientswithresidualthrombusfollowingthrombolysisorthosewithchronicaxillosubclavianthrombosis,the
axillosubclavianveincanbereconstructedconcurrentwiththoracicoutletdecompressionoratalatertimeusing
openorendovasculartechniques,ifneeded.Inaseriesofpatientsundergoingfirstribresectionforchronic
symptomsrelatedtoprimarysubclavianveinthrombosis,subclavianveinthrombusresolvedin14of16patients
treatedwithongoinganticoagulation[105].(See'Venoplasty'below.)
Theaimofthoracicoutletdecompressionistoprovidemorespacethroughwhichtheneurovascularstructuresof
theupperextremitycanpass.Thoracicoutletdecompressionmayincludeanyoneoracombinationofthe
followingprocedures,thechoiceofwhichwilldependuponthespecificanatomicabnormalityidentified[22,105].
(See"Overviewofthoracicoutletsyndromes",sectionon'Pathogenesis'.)
Firstribresection
Cervicalribresection(lesscommonforvenousthoracicoutletsyndrome)
Divisionofanomalousbands
Divisionofanomalousmusculotendinousinsertions
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=sea
9/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Scalenectomy
Forpatientsidentifiedwithacervicalrib,cervicalribresectionmaybeallthatisrequired.However,whena
cervicalribisnotpresent,firstribresectioniscombinedwithdissectionanddivisionofstructuresidentifiedatthe
timeofsurgicalexplorationaspotentiallycausingcompressionontheneurovascularstructuresofthethoracic
outlet,whetherornotthesewereidentifiedasaspecificsourceofcompressiononpriorimagingstudies.
Threesurgicalapproachesareusedforthoracicoutletdecompression:thetransaxillary,supraclavicular,and
infraclavicularapproaches,eachwithadvantagesanddisadvantages.Therearenotrialscomparingsurgical
approachesfordecompression,andthereremainsnoexpertconsensusastowhichsurgicalapproachormethod
oftreatingtheinjuredvenoussegmentisbetter.Assuch,thesurgicalapproachdependslargelyuponthetypeof
anatomicabnormalitiesidentifiedandsurgeonpreference.Theseapproachesandthecomplicationsassociated
withthemarediscussedseparately.(See"Overviewofthoracicoutletsyndromes",sectionon'Thoracicoutlet
decompression'.)
Complicationsofthoracicoutletdecompressionincludehemopneumothorax,longthoracicnerveinjury,incomplete
ribresectionthatcanleadtorecurrentsymptoms,brachialplexusinjury,arterialinjury,lymphaticleak,and
surgicalsiteinfection.
VENOPLASTYAlthoughthereisuniformagreementthatthoracicoutletdecompressionshouldbeperformed
earlyinpatientswithacuteaxillosubclavianthrombosis[1],debateexistsoverthemanagementofthevein.
Concurrentwiththoracicoutletdecompression,somefeelthatvenolysisorvenoplasty(percutaneoustransluminal
oropen)issufficientwhileothersadvocateveinrepair(patchvenoplasty,interpositionveingraft,veinbypass,
jugularturndown)[27,80,106].Thereareinsufficientdatatosupportoneapproachoveranother.
Occasionally,percutaneoustransluminalangioplasty(PTA)isneededtokeeptheveinopenfollowingthrombolysis
untilthoracicoutletdecompressioncanbeaccomplished[1].However,priortothoracicoutletdecompression,
stentingshouldbeavoided[42,86,107109].Shouldermovementssubjectthestenttorepetitivecompressionthat
canleadtostentfracture.Inonesmallobservationalstudy,stentusewasfoundtobeanindependentriskfactor
forupperextremityrethrombosis[86].Oncethoracicoutletdecompressionhasbeenperformed,whetherornota
veinpatchrepairorbypasswasperformed,residualorrecurrentstenosismaywarrantPTAandpossiblystenting,
withacceptableclinicaloutcomes[1,22].
FOLLOWUPWeobtainaDuplexultrasoundinthepostsurgicalperiodtoconfirmpatencyofaxillosubclavian
vein.Ifthepatientexperiencesrecurrentsymptoms,weagreewithothersinadvocatinganimmediatevenogram
toevaluatethepatencyoftherepairedvenoussegment[105].
DurationofanticoagulationInpatientswithprimaryupperextremitydeepveinthrombosis,anticoagulation
shouldbecontinuedforaminimumofthreemonthsfollowingtheinitialthromboticevent,withalongerdurationof
therapyindicatedforthosewhohavehadarecurrentevent[63,110].Wemaintainanticoagulationregardlessof
whetherintervention(thrombolysis,thoracicoutletdecompression)wasperformed.
PERIOPERATIVEMORBIDITYANDMORTALITYMortalityrelatedtoprimaryupperextremitydeepvein
thrombosisisoveralllow,duetotherelativelyyoungpopulationofpatientswhoaretypicallyaffected.By
comparison,mortalityrelatedtosecondarycausesofupperextremitydeepveinthrombosisishigher,rangingfrom
15to50percentreflectingunderlyingcomorbiditiessuchasmalignancy,renalfailure,andmultiorganfailure[12].
RecurrentthromboembolismRecurrentupperextremitydeepveinthrombosis(allcauses)occursin2to8
percentofpatientsfollowingtreatment[28,111,112].Theseratesaresignificantlylowerthanrecurrenceratesfor
lowerextremitydeepveinthrombosis,whichinonelongtermstudywas30percentateightyears[113].
Ahypercoagulablestateneedstobeconsideredinpatientswhodeveloprecurrentthromboembolism[12].Higher
ratesofthrombophiliahavebeenreportedinpatientswithrecurrentupperextremitydeepveinthrombosis[30,114
117].Inonestudy,90percentofpostoperativecomplicationswereassociatedwithsomeformofthrombophilia
[115].Theevaluationofthrombophiliaisdiscussedelsewhere.(See"Evaluatingpatientswithestablishedvenous
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
10/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
thromboembolismforacquiredandinheritedriskfactors".)
PostthromboticsyndromePostthromboticsyndromereferstothedevelopmentofsymptomsorsignsof
chronicvenousinsufficiencyrelatedtoapriordeepveinthrombosis.Postthromboticsyndromeisdiscussedin
detailelsewhere.(See"Postthrombotic(postphlebitic)syndrome".)
Qualityoflifeisreducedinpatientswithpostthromboticsyndrome,particularlyifthedominantarmisaffected.
Severeupperextremitysymptomswithskinulcerationarerare,butpostthromboticsyndromeaffectingtheupper
extremitycanresultinoccupationaldisabilityinpatientswhosejobrequiresmanuallabor.Eveninpatientswhose
occupationdoesnotinvolvethevigoroususeofthearms,symptomsofpostthromboticsyndromecanlimitother
activitiesandadverselyimpactqualityoflife.
Theincidenceofpostthromboticsyndromefollowingupperextremitydeepveinthrombosis(allcauses)ranges
from7to44percentbutappearstobemoreprevalentfollowingprimarycomparedwithsecondaryetiologies
[12,28].Sinceprimaryupperextremitydeepveinthrombosisgenerallyaffectsyoung,otherwisehealthyindividuals
withanactivelifestyleandlonglifeexpectancy,oneoftheaimsofearlyaggressivetreatmentisminimizing
symptomsofpostthromboticsyndrome.(See'Rationaleforaggressivetreatment'above.)
Inpatientswithprimaryupperextremitydeepveinthrombosis,upto53percentofpatientstreatedwith
anticoagulationalonehistoricallydevelopedpostthromboticsyndromeat5years[27,103].Withaggressive
therapythatincludesanticoagulation,thrombolysis,andthoracicoutletdecompression,theincidenceofresidual
symptomsrangesfrom12to25percent[1,27].Theriskofdevelopingpostthromboticsyndromemaybegreaterin
patientswhohaveresidualveinobstruction.However,inonestudy,noassociationbetweenultrasoundfindings
andthedevelopmentofpostthromboticsyndromewasfound[118].
SUMMARYANDRECOMMENDATIONS
Primary,"spontaneous"upperextremitydeepveinthrombosisisestimatedtorepresentbetween1and4
percentofallcasesofupperextremitydeepveinthrombosis,withsecondarycausesofthrombosisrelatedto
centralveincannulation(eg,centralline,pacemaker)orprothromboticstates(eg,thrombophilia,malignancy)
muchmorecommon.(See'Introduction'above.)
Primaryupperextremitydeepveinthrombosisisdefinedasthrombosisofthedeepveinsdrainingtheupper
extremity(axillary,subclavian)duetoanunderlyinganatomicanomalyatthethoracicoutletcausing
compressionorrepetitivevenousinjury.Thesyndromeisappropriatelytermedvenousthoracicoutlet
syndrome,butisalsoreferredtoasPagetSchroettersyndromeandeffortthrombosis.Anatomic
abnormalitiescanbecongenitaloracquired.Congenitalanomaliesconsistofcervicalribs,supernumerary
muscles,abnormaltendoninsertions,orabnormalmuscularortendinousbands.Acquiredabnormalities
includebonyovergrowthduetobonyfracture(usuallyoftheclavicle),orhypertrophyofanteriorscalene
muscleorsubclaviusmuscles,oftenrelatedtorepetitivelifting.(See'Pathogenesis'above.)
Primaryupperextremitydeepveinthrombosistypicallypresentsinyoung,otherwisehealthyindividualsas
sudden,severearmswelling.Althoughmorecommonlyassociatedwithlowerextremitydeepvein
thrombosis,pulmonaryembolismfromupperextremitydeepveinthrombosis(primaryandsecondary)occurs
in4to10percentofpatients.Theclinicianshouldhaveahighindexofsuspicionforthisdisorderwhena
youngpatientwithnoincitingfactorspresentswithsignsofupperextremityvenousthrombosis,or
pulmonaryembolismintheabsenceoflowerextremitysymptoms.(See'Clinicalpresentations'above.)
Adiagnosisofupperextremityvenousoutflowobstruction(ie,deepveinthrombosisorvenousstenosis)may
besuspectedbasedupontheclinicalpresentation,butshouldbeconfirmedwithimaging,typicallyinitially
usingultrasound.Ddimerisusefulforexcludingthrombosisasanetiology,butwillnotexcludevein
compression/stenosiswithoutthrombosisasasourceofsymptoms.Onceadiagnosisofvenousoutflow
obstructionisestablished,aprimaryetiologyshouldbesoughttoidentifytheunderlyinganatomic
abnormalitythatisthesourceoftheobstruction.Weobtainaplainchestradiographonallpatientstoidentify
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
11/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
anyobviousbonyabnormalities.Moreadvancedimagingmaybenecessarytodemonstrateabnormal
muscularattachmentsordynamicvenouscompression.(See'Diagnosis'above.)
Treatmentofprimaryupperextremitydeepveinthrombosisisaimedatpreventingpulmonaryembolism,
recurrentvenousthrombosisandpostthromboticsyndrome.Forpatientswithacutelysymptomaticprimary
upperextremitydeepveinthrombosis,werecommendanticoagulationovernosuchtherapy(Grade1B).
Anticoagulationhelpstomaintainpatencyofcollateralveins,reducespropagationofthrombus,andis
effectiveforpreventingpulmonaryembolism.Weprefertouseunfractionatedheparintofacilitaterapiddose
adjustmentinpatientswhowillundergootherinterventionssuchasthrombolysisandthoracicoutlet
decompression.
Forpatientswithmoderatetosevereacutesymptomswhoarediagnosedwithprimaryupperextremitydeep
veinthrombosis,wesuggestthrombolysisoveranticoagulationalone(Grade2C).Followingthrombolysis,
wesuggestthoracicoutletdecompression,ratherthannodecompression(Grade2C).Thisapproach
decreasestheriskforrecurrentthrombosisandpostthromboticsyndrome.Anticoagulationalonemaybe
adequateforminimallysymptomaticorintermittentlysymptomaticpatients.Forthosewhopresentina
delayedmanner(>2weeksfromtheonsetofsymptoms),decompressionofthoracicoutletinadditionto
anticoagulationmaybebeneficial.(See'Approachtotreatment'aboveand'Rationaleforaggressive
treatment'above.)
WeagreewithAmericanCollegeofChestPhysicianswhorecommendaminimumofthreemonthsof
anticoagulationfollowinganinitialthromboticevent.Wemaintainanticoagulationforaminimumofthree
monthsregardlessofwhetherintervention(thrombolysis,thoracicoutletdecompression)wasperformed.
(See'Approachtotreatment'above.)
UseofUpToDateissubjecttotheSubscriptionandLicenseAgreement.
REFERENCES
1.IlligKA,DoyleAJ.AcomprehensivereviewofPagetSchroettersyndrome.JVascSurg201051:1538.
2.AllaVM,NatarajanN,KaushikM,etal.Pagetschroettersyndrome:reviewofpathogenesisandtreatment
ofeffortthrombosis.WestJEmergMed201011:358.
3.AzizS,StraehleyCJ,WhelanTJJr.Effortrelatedaxillosubclavianveinthrombosis.Anewtheoryof
pathogenesisandapleafordirectsurgicalintervention.AmJSurg1986152:57.
4.BahmJ.Criticalreviewofpathophysiologicmechanismsinthoracicoutletsyndrome(TOS).ActaNeurochir
Suppl2007100:137.
5.MustafaS,SteinPD,PatelKC,etal.Upperextremitydeepvenousthrombosis.Chest2003123:1953.
6.Paget,J.Clinicallecturesandessays.LongmenGreenandCo,1875.
7.vonSchroetter,L.ErkrankungenderGefasse.In:NathnagelHandbuchderPathologieundTherapie,
AnonymousWein,Holder,1884.
8.HUGHESES.VenousobstructionintheupperextremityPagetSchroetter'ssyndromeareviewof320
cases.SurgGynecolObstet194988:89.
9.DrapanasT,CurranWL.Thrombectomyinthetreatmentof"effort"thrombosisoftheaxillaryandsubclavian
veins.JTrauma19666:107.
10.LindbladB,TengbornL,BergqvistD.Deepveinthrombosisoftheaxillarysubclavianveins:epidemiologic
data,effectsofdifferenttypesoftreatmentandlatesequelae.EurJVascSurg19882:161.
11.HorattasMC,WrightDJ,FentonAH,etal.Changingconceptsofdeepvenousthrombosisoftheupper
extremityreportofaseriesandreviewoftheliterature.Surgery1988104:561.
12.FlintermanLE,VanDerMeerFJ,RosendaalFR,DoggenCJ.Currentperspectiveofvenousthrombosisin
theupperextremity.JThrombHaemost20086:1262.
13.SwintonNWJr,EdgettJWJr,HallRJ.Primarysubclavianaxillaryveinthrombosis.Circulation1968
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
12/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
38:737.
14.FisherJB,GransonMA.Congenitalvenouswebcausingsubclavianveinobstruction:acasereport.JVasc
Surg198910:460.
15.JohansenKH,ThomasGI.Latethoracicoutletsyndromesecondarytomalunionofthefracturedclavicle:
casereportandreviewoftheliterature.JTrauma200252:607.
16.JainS,MonbaliuD,ThompsonJF.Thoracicoutletsyndromecausedbychronicretrosternaldislocationof
theclavicle.Successfultreatmentbytransaxillaryresectionofthefirstrib.JBoneJointSurgBr2002
84:116.
17.DuaneTM,O'ConnorJV,ScaleaTM.Thoracicoutletsyndromeresultingfromfirstribfracture.JTrauma
200762:231.
18.PeivandiMT,NazemianZ.Clavicularfractureandupperextremitydeepvenousthrombosis.Orthopedics
201134:227.
19.StevensonIM,ParryEW.Radiologicalstudyoftheaetiologicalfactorsinvenousobstructionoftheupper
limb.JCardiovascSurg(Torino)197516:580.
20.MachlederHI.Thrombolytictherapyandsurgeryforprimaryaxillosubclavianveinthrombosis:current
approach.SeminVascSurg19969:46.
21.HronE,LozinguezO,EmmerichJ,etal.Longtermsequelaeofspontaneousaxillarysubclavianvenous
thrombosis.AnnInternMed1999131:510.
22.UrschelHCJr,RazzukMA.PagetSchroettersyndrome:whatisthebestmanagement?AnnThoracSurg
200069:1663.
23.DiFeliceGS,PalettaGAJr,PhillipsBB,WrightRW.Effortthrombosisintheelitethrowingathlete.AmJ
SportsMed200230:708.
24.IsmaN,SvenssonPJ,GottsterA,LindbladB.Upperextremitydeepvenousthrombosisinthepopulation
basedMalmthrombophiliastudy(MATS).Epidemiology,riskfactors,recurrencerisk,andmortality.
ThrombRes2010125:e335.
25.EngelbergerRP,KucherN.Managementofdeepveinthrombosisoftheupperextremity.Circulation2012
126:768.
26.KucherN.Clinicalpractice.Deepveinthrombosisoftheupperextremities.NEnglJMed2011364:861.
27.UrschelHCJr,PatelAN.SurgeryremainsthemosteffectivetreatmentforPagetSchroettersyndrome:50
years'experience.AnnThoracSurg200886:254.
28.JoffeHV,GoldhaberSZ.Upperextremitydeepveinthrombosis.Circulation2002106:1874.
29.HendlerMF,MeschengieserSS,BlancoAN,etal.Primaryupperextremitydeepveinthrombosis:high
prevalenceofthrombophilicdefects.AmJHematol200476:330.
30.MartinelliI,BattaglioliT,BucciarelliP,etal.Riskfactorsandrecurrencerateofprimarydeepvein
thrombosisoftheupperextremities.Circulation2004110:566.
31.AdamsJT,DeWeeseJA."Effort"thrombosisoftheaxillaryandsubclavianveins.JTrauma197111:923.
32.PrandoniP,BernardiE.Upperextremitydeepveinthrombosis.CurrOpinPulmMed19995:222.
33.JoffeHV,KucherN,TapsonVF,etal.Upperextremitydeepveinthrombosis:aprospectiveregistryof592
patients.Circulation2004110:1605.
34.OzakarL,DnmezG,YrbulutM,etal.PagetSchroettersyndromeforerunningthediagnosesofthoracic
outletsyndromeandthrombophilia.ClinApplThrombHemost201016:351.
35.BolithoDG,ElwoodET,RobertsF.Phlegmasiaceruleadolensoftheupperextremity.AnnPlastSurg2000
45:644.
36.PetritschB,WendelF,HahnD,GoltzJP.Phlegmasiaceruleadolensofthearm.JVascAccess2012
13:399.
37.KucherN,TapsonVF,GoldhaberSZ,DVTFREESteeringCommittee.Riskfactorsassociatedwith
symptomaticpulmonaryembolisminalargecohortofdeepveinthrombosispatients.ThrombHaemost
200593:494.
38.MuozFJ,MismettiP,PoggioR,etal.Clinicaloutcomeofpatientswithupperextremitydeepvein
thrombosis:resultsfromtheRIETERegistry.Chest2008133:143.
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
13/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
39.SteinPD,MattaF,MusaniMH,DiaczokB.Silentpulmonaryembolisminpatientswithdeepvenous
thrombosis:asystematicreview.AmJMed2010123:426.
40.MaiC,HuntD.Upperextremitydeepvenousthrombosis:areview.AmJMed2011124:402.
41.InoueK,SaitoJ,MiyazakiM,etal.AKendoplayerwithhaemoptysis.Lancet2004364:814.
42.UrschelHCJr,PatelAN.PagetSchroettersyndrometherapy:failureofintravenousstents.AnnThorac
Surg200375:1693.
43.MerminodT,PellicciottaS,BounameauxH.LimitedusefulnessofDdimerinsuspecteddeepvein
thrombosisoftheupperextremities.BloodCoagulFibrinolysis200617:225.
44.DiNisioM,VanSluisGL,BossuytPM,etal.Accuracyofdiagnostictestsforclinicallysuspectedupper
extremitydeepveinthrombosis:asystematicreview.JThrombHaemost20108:684.
45.KerrTM,LutterKS,MoellerDM,etal.Upperextremityvenousthrombosisdiagnosedbyduplexscanning.
AmJSurg1990160:202.
46.KnudsonGJ,WiedmeyerDA,EricksonSJ,etal.ColorDopplersonographicimagingintheassessmentof
upperextremitydeepvenousthrombosis.AJRAmJRoentgenol1990154:399.
47.SajidMS,AhmedN,DesaiM,etal.Upperlimbdeepveinthrombosis:aliteraturereviewtostreamlinethe
protocolformanagement.ActaHaematol2007118:10.
48.PrandoniP,PolistenaP,BernardiE,etal.Upperextremitydeepveinthrombosis.Riskfactors,diagnosis,
andcomplications.ArchInternMed1997157:57.
49.BaarslagHJ,vanBeekEJ,KoopmanMM,ReekersJA.Prospectivestudyofcolorduplexultrasonography
comparedwithcontrastvenographyinpatientssuspectedofhavingdeepvenousthrombosisoftheupper
extremities.AnnInternMed2002136:865.
50.MustafaBO,RathbunSW,WhitsettTL,RaskobGE.Sensitivityandspecificityofultrasonographyinthe
diagnosisofupperextremitydeepveinthrombosis:asystematicreview.ArchInternMed2002162:401.
51.ChinEE,ZimmermanPT,GrantEG.Sonographicevaluationofupperextremitydeepvenousthrombosis.J
UltrasoundMed200524:829.
52.HbschPJ,StiglbauerRL,SchwaighoferBW,etal.Internaljugularandsubclavianveinthrombosiscaused
bycentralvenouscatheters.EvaluationusingDopplerbloodflowimaging.JUltrasoundMed19887:629.
53.HaireWD,LynchTG,LundGB,etal.Limitationsofmagneticresonanceimagingandultrasounddirected
(duplex)scanninginthediagnosisofsubclavianveinthrombosis.JVascSurg199113:391.
54.DesjardinsB,RybickiFJ,KimHS,etal.ACRAppropriatenessCriteriaSuspectedupperextremitydeep
veinthrombosis.JAmCollRadiol20129:613.
55.MatsumuraJS,RillingWS,PearceWH,etal.Helicalcomputedtomographyofthenormalthoracicoutlet.J
VascSurg199726:776.
56.KroenckeTJ,TaupitzM,ArnoldR,etal.Threedimensionalgadoliniumenhancedmagneticresonance
venographyinsuspectedthromboocclusivediseaseofthecentralchestveins.Chest2001120:1570.
57.BaarslagHJ,VanBeekEJ,ReekersJA.Magneticresonancevenographyinconsecutivepatientswith
suspecteddeepveinthrombosisoftheupperextremity:initialexperience.ActaRadiol200445:38.
58.KimH,ChungJW,ParkJH,etal.RoleofCTvenographyinthediagnosisandtreatmentofbenignthoracic
centralvenousobstruction.KoreanJRadiol20034:146.
59.ErsoyH,SteignerML,CoynerKB,etal.Vascularthoracicoutletsyndrome:protocoldesignanddiagnostic
valueofcontrastenhanced3DMRangiographyandequilibriumphaseimagingon1.5and3TMRI
scanners.AJRAmJRoentgenol2012198:1180.
60.SandersRJ,HammondSL,RaoNM.Diagnosisofthoracicoutletsyndrome.JVascSurg200746:601.
61.GirolamiA,PrandoniP,ZanonE,etal.Venousthrombosesofupperlimbsaremorefrequentlyassociated
withoccultcancerascomparedwiththoseoflowerlimbs.BloodCoagulFibrinolysis199910:455.
62.BeckerDM,PhilbrickJT,WalkerFB4th.Axillaryandsubclavianvenousthrombosis.Prognosisand
treatment.ArchInternMed1991151:1934.
63.KearonC,AklEA,ComerotaAJ,etal.AntithrombotictherapyforVTEdisease:AntithromboticTherapyand
PreventionofThrombosis,9thed:AmericanCollegeofChestPhysiciansEvidenceBasedClinicalPractice
Guidelines.Chest2012141:e419S.
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
14/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
64.MachlederHI.EvaluationofanewtreatmentstrategyforPagetSchroettersyndrome:spontaneous
thrombosisoftheaxillarysubclavianvein.JVascSurg199317:305.
65.RathbunSW,StonerJA,WhitsettTL.Treatmentofupperextremitydeepveinthrombosis.JThromb
Haemost20119:1924.
66.ThompsonJF,WinterbornRJ,BaysS,etal.VenousthoracicoutletcompressionandthePagetSchroetter
syndrome:areviewandrecommendationsformanagement.CardiovascInterventRadiol201134:903.
67.StoneDH,ScaliST,BjerkAA,etal.Aggressivetreatmentofidiopathicaxillosubclavianveinthrombosis
providesexcellentlongtermfunction.JVascSurg201052:127.
68.LeeWA,HillBB,HarrisEJJr,etal.Surgicalinterventionisnotrequiredforallpatientswithsubclavianvein
thrombosis.JVascSurg200032:57.
69.MelbySJ,VedanthamS,NarraVR,etal.Comprehensivesurgicalmanagementofthecompetitiveathlete
witheffortthrombosisofthesubclavianvein(PagetSchroettersyndrome).JVascSurg200847:809.
70.StrangeVognsenHH,HauchO,AndersenJ,StruckmannJ.Resectionofthefirstrib,followingdeeparm
veinthrombolysisinpatientswiththoracicoutletsyndrome.JCardiovascSurg(Torino)198930:430.
71.deLenRA,ChangDC,HassounHT,etal.Multipletreatmentalgorithmsforsuccessfuloutcomesin
venousthoracicoutletsyndrome.Surgery2009145:500.
72.UrschelHCJr,RazzukMA.ImprovedmanagementofthePagetSchroettersyndromesecondarytothoracic
outletcompression.AnnThoracSurg199152:1217.
73.DonayreCE,WhiteGH,MehringerSM,WilsonSE.Pathogenesisdetermineslatemorbidityof
axillosubclavianveinthrombosis.AmJSurg1986152:179.
74.AbuRahmaAF,SadlerD,StuartP,etal.Conventionalversusthrombolytictherapyinspontaneous(effort)
axillarysubclavianveinthrombosis.AmJSurg1991161:459.
75.SkalickaL,LubandaJC,JiratS,etal.Endovasculartreatmentcombinedwithstratifiedsurgeryiseffective
inthemanagementofvenousthoracicoutletsyndromecomplications:alongtermultrasoundfollowup
studyinpatientswiththromboticeventsduetovenousthoracicoutletsyndrome.HeartVessels2011
26:616.
76.LeeMC,GrassiCJ,BelkinM,etal.Earlyoperativeinterventionafterthrombolytictherapyforprimary
subclavianveinthrombosis:aneffectivetreatmentapproach.JVascSurg199827:1101.
77.GloviczkiP,KazmierFJ,HollierLH.Axillarysubclavianvenousocclusion:themorbidityofanonlethal
disease.JVascSurg19864:333.
78.PrandoniP,BernardiE,MarchioriA,etal.Thelongtermclinicalcourseofacutedeepveinthrombosisofthe
arm:prospectivecohortstudy.BMJ2004329:484.
79.PovlsenB,BelzbergA,HanssonT,DorsiM.Treatmentforthoracicoutletsyndrome.CochraneDatabase
SystRev2010:CD007218.
80.MolinaJE,HunterDW,DietzCA.ProtocolsforPagetSchroettersyndromeandlatetreatmentofchronic
subclavianveinobstruction.AnnThoracSurg200987:416.
81.UrschelHCJr,RazzukMA.Neurovascularcompressioninthethoracicoutlet:changingmanagementover
50years.AnnSurg1998228:609.
82.HrubJ,SemrdM,VidimT,etal.[Outcomesofcombinedsurgicalandendovasculartreatmentofthe
venousthoracicoutletsyndromeduring20002007intheIIndSurgicalClinicoftheVFN(GeneralFaculty
Hospital)and1.LFUK(FirstMedicalFaculty,CharlesUniversity)inPrague].RozhlChir201089:69.
83.KearonC,KahnSR,AgnelliG,etal.Antithrombotictherapyforvenousthromboembolicdisease:American
CollegeofChestPhysiciansEvidenceBasedClinicalPracticeGuidelines(8thEdition).Chest2008
133:454S.
84.AngleN,GelabertHA,FarooqMM,etal.Safetyandefficacyofearlysurgicaldecompressionofthethoracic
outletforPagetSchroettersyndrome.AnnVascSurg200115:37.
85.VikA,HolmePA,SinghK,etal.Catheterdirectedthrombolysisfortreatmentofdeepvenousthrombosisin
theupperextremities.CardiovascInterventRadiol200932:980.
86.LeeJT,KarwowskiJK,HarrisEJ,etal.Longtermthromboticrecurrenceafternonoperativemanagementof
PagetSchroettersyndrome.JVascSurg200643:1236.
87.MolinaJE,HunterDW,DietzCA.PagetSchroettersyndrometreatedwiththrombolyticsandimmediate
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
15/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
surgery.JVascSurg200745:328.
88.SchneiderDB,DimuzioPJ,MartinND,etal.Combinationtreatmentofvenousthoracicoutletsyndrome:
opensurgicaldecompressionandintraoperativeangioplasty.JVascSurg200440:599.
89.GuzzoJL,ChangK,DemosJ,etal.Preoperativethrombolysisandvenoplastyaffordsnobenefitinpatency
followingfirstribresectionandscalenectomyforsubacuteandchronicsubclavianveinthrombosis.JVasc
Surg201052:658.
90.TilneyML,GriffithsHJ,EdwardsEA.Naturalhistoryofmajorvenousthrombosisoftheupperextremity.
ArchSurg1970101:792.
91.vanDongenCJ,vandenBeltAG,PrinsMH,LensingAW.Fixeddosesubcutaneouslowmolecularweight
heparinsversusadjusteddoseunfractionatedheparinforvenousthromboembolism.CochraneDatabase
SystRev2004:CD001100.
92.KarabayO,YetkinU,OnolH.Upperextremitydeepveinthrombosis:clinicalandtreatmentcharacteristics.
JIntMedRes200432:429.
93.SavageKJ,WellsPS,SchulzV,etal.Outpatientuseoflowmolecularweightheparin(Dalteparin)forthe
treatmentofdeepveinthrombosisoftheupperextremity.ThrombHaemost199982:1008.
94.EndenT,SandvikL,KlwNE,etal.CatheterdirectedVenousThrombolysisinacuteiliofemoralvein
thrombosistheCaVenTstudy:rationaleanddesignofamulticenter,randomized,controlled,clinicaltrial
(NCT00251771).AmHeartJ2007154:808.
95.SchulmanS,BeythRJ,KearonC,etal.Hemorrhagiccomplicationsofanticoagulantandthrombolytic
treatment:AmericanCollegeofChestPhysiciansEvidenceBasedClinicalPracticeGuidelines(8thEdition).
Chest2008133:257S.
96.CaparrelliDJ,FreischlagJ.Aunifiedapproachtoaxillosubclavianvenousthrombosisinasinglehospital
admission.SeminVascSurg200518:153.
97.AleshI,KayaliF,SteinPD.Catheterdirectedthrombolysis(intrathrombusinjection)intreatmentofdeep
venousthrombosis:asystematicreview.CatheterCardiovascInterv200770:143.
98.ShahAD,BajakianDR,OlinJW,LooksteinRA.PowerpulsespraythrombectomyfortreatmentofPaget
Schroettersyndrome.AJRAmJRoentgenol2007188:1215.
99.OkluR,WickyS.Catheterdirectedthrombolysisofdeepvenousthrombosis.SeminThrombHemost2013
39:446.
100.WickyST.Acutedeepveinthrombosisandthrombolysis.TechVascIntervRadiol200912:148.
101.KimHS,PatraA,PaxtonBE,etal.Catheterdirectedthrombolysiswithpercutaneousrheolytic
thrombectomyversusthrombolysisaloneinupperandlowerextremitydeepveinthrombosis.Cardiovasc
InterventRadiol200629:1003.
102.DasariTW,PappyR,HennebryTA.Pharmacomechanicalthrombolysisofacuteandchronicsymptomatic
deepveinthrombosis:asystematicreviewofliterature.Angiology201263:138.
103.UrschelHCJr.Managementofthethoracicoutletsyndrome.NEnglJMed1972286:1140.
104.MolinaJE.Surgeryforeffortthrombosisofthesubclavianvein.JThoracCardiovascSurg1992103:341.
105.ChangKZ,LikesK,DemosJ,etal.Routinevenographyfollowingtransaxillaryfirstribresectionand
scalenectomy(FRRS)forchronicsubclavianveinthrombosisensuresexcellentoutcomesandveinpatency.
VascEndovascularSurg201246:15.
106.FeugierP,AleksicI,SalariR,etal.LongtermresultsofvenousrevascularizationforPagetSchroetter
syndromeinathletes.AnnVascSurg200115:212.
107.MeierGH,PollakJS,RosenblattM,etal.Initialexperiencewithvenousstentsinexertionalaxillary
subclavianveinthrombosis.JVascSurg199624:974.
108.OderichGS,TreimanGS,SchneiderP,BhirangiK.Stentplacementfortreatmentofcentralandperipheral
venousobstruction:alongtermmultiinstitutionalexperience.JVascSurg200032:760.
109.MaintzD,LandwehrP,GawendaM,LacknerK.FailureofWallstentsinthesubclavianveinduetostent
damage.ClinImaging200125:133.
110.SchulmanS,LindmarkerP,HolmstrmM,etal.Postthromboticsyndrome,recurrence,anddeath10years
afterthefirstepisodeofvenousthromboembolismtreatedwithwarfarinfor6weeksor6months.JThromb
Haemost20064:734.
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
16/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
111.HeitJA,MohrDN,SilversteinMD,etal.Predictorsofrecurrenceafterdeepveinthrombosisandpulmonary
embolism:apopulationbasedcohortstudy.ArchInternMed2000160:761.
112.MolinaJE.ReoperationsafterfailedtransaxillaryfirstribresectiontotreatPagetSchroettersyndrome
patients.AnnThoracSurg201191:1717.
113.FlintermanLE,vanHylckamaVliegA,RosendaalFR,DoggenCJ.Recurrentthrombosisandsurvivalafter
afirstvenousthrombosisoftheupperextremity.Circulation2008118:1366.
114.GabrielF,PortolsO,LabisM,etal.Usefulnessofthrombophiliatestinginvenousthromboembolic
disease:findingsfromtheRIETEregistry.ClinApplThrombHemost201319:42.
115.CassadaDC,LipscombAL,StevensSL,etal.TheimportanceofthrombophiliainthetreatmentofPaget
Schroettersyndrome.AnnVascSurg200620:596.
116.LeebeekFW,StadhoudersNA,vanSteinD,etal.Hypercoagulabilitystatesinupperextremitydeepvenous
thrombosis.AmJHematol200167:15.
117.HronE,LozinguezO,AlhencGelasM,etal.Hypercoagulablestatesinprimaryupperextremitydeepvein
thrombosis.ArchInternMed2000160:382.
118.PerssonLM,ArnhjortT,LrfarsG,RosforsS.Hemodynamicandmorphologicevaluationofsequelaeof
primaryupperextremitydeepvenousthrombosestreatedwithanticoagulation.JVascSurg200643:1230.
Topic8211Version10.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
17/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
GRAPHICS
Anteriorviewsuperficialveinsoftheupper
extremity
Thecephalicveinoriginatesattheradialaspectofthewrist
traversingtheradialborderoftheforearm.Itreceivestributaries
fromboththeventralanddorsalsurfaces.Attheantecubitalfossa
itprovidesatributarytothemediancubitalvein.Intheupperarm,
ittravelsinthegroovebetweenthepectoralismajoranddeltoid
muscles.Itpiercesthecoracoclavicularfasciaand,crossingthe
axillaryartery,endsintheaxillaryveinjustbelowtheclavicle.
Sometimesitcommunicateswiththeexternaljugularveinbya
branchwhichascendsanteriortotheclavicle.
Thebasilicveinoriginatesintheulnaraspectofthewrist
traversingtheulnarsideoftheforearmtotheantecubitalfossa
whereitisjoinedbythemediancubitalvein.Itascendsinthe
groovebetweenthebicepsbrachiiandpronatorteres,crossesthe
brachialarteryattheelbowandcontinuescephaladalongthe
medialborderofthebicepsbrachii.Itperforatesthedeepfasciaof
theupperarmandjoinsthebrachialvein.
Graphic55596Version7.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
18/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Deepveinsoftheupperextremity
Thedeepveinsoftheupperextremityincludethepairedulnar,radial
andinterosseousveinsintheforearm,pairedbrachialveinsoftheupper
arm,andaxillaryvein.Theaxillaryveinoriginatesatthelowerborderof
theteresmajormuscleincontinuitywiththebrachialveins.Thebasilic
andcephalicveins,whicharesuperficialveins,contributetotheaxillary
vein,thoughmanyanatomicvariationsoccur.Afterpassingtheouter
marginofthefirstrib,theaxillaryveincontinuesasthesubclavianvein.
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
19/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Graphic61941Version4.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
20/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Anatomyofthethoracicoutlet
Thethoracicoutletreferstotheconfinedspacebetweentheclavicleand
firstrib.Structuresthatpassthroughthisregionincludethenervesofthe
brachialplexus,thesubclavianarteryandsubclavianvein.
Graphic59433Version5.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
21/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Cervicalribcausingthoracicoutletsyndrome
Thoracicoutletsyndromesareduetocompressionofanyofthestructures
(brachialplexus,subclavianartery,subclavianvein)thattraversethe
confinedspacebetweentheclavicleandfirstrib.Anatomicabnormaliaties
suchasacervicalrib(shown),musculotendinousabnormalitiesorscarring
cancontributetothepathology.
Graphic50430Version5.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
22/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Contraindicationstofibrinolytictherapyfordeepvenousthrombosis
oracutepulmonaryembolism
Absolutecontraindications
Priorintracranialhemorrhage
Knownstructuralcerebralvascularlesion
Knownmalignantintracranialneoplasm
Ischemicstrokewithinthreemonths(excludingstrokewithinthreehours*)
Suspectedaorticdissection
Activebleedingorbleedingdiathesis(excludingmenses)
Significantclosedheadtraumaorfacialtraumawithinthreemonths
Relativecontraindications
Historyofchronic,severe,poorlycontrolledhypertension
Severeuncontrolledhypertensiononpresentation(SBP>180mmHgorDBP>110mmHg)
Historyofischemicstrokemorethanthreemonthsprior
Traumaticorprolonged(>10minute)CPRormajorsurgerylessthanthreeweeks
Recent(withintwotofourweeks)internalbleeding
Noncompressiblevascularpunctures
Recentinvasiveprocedure
Forstreptokinase/anistreplasePriorexposure(morethanfivedaysago)orpriorallergic
reactiontotheseagents
Pregnancy
Activepepticulcer
Pericarditisorpericardialfluid
Currentuseofanticoagulant(eg,warfarinsodium)thathasproducedanelevatedinternational
normalizedratio(INR)>1.7orprothrombintime(PT)>15seconds
Age>75years
Diabeticretinopathy
SBP:systolicbloodpressureDBP:diastolicbloodpressureCPR:cardiopulmonaryresuscitation.
*TheAmericanCollegeofCardiologysuggeststhatselectpatientswithstrokemaybenefitfrom
thrombolytictherapywithin4.5hoursoftheonsetofsymptoms.
ReproducedwithpermissionfromtheAmericanCollegeofChestPhysicians.KearonC,AklEA,Comerota
AJ,etal.AntithrombotictherapyforVTEdisease:AntithromboticTherapyandPreventionofThrombosis,
9thed:AmericanCollegeofChestPhysiciansEvidenceBasedClinicalPracticeGuidelines.Chest2012
141:e419S.Copyright2012.
Graphic95035Version2.0
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
23/24
3/6/2016
Primary(spontaneous)upperextremitydeepveinthrombosis
Disclosures
Disclosures:KaoruGoshima,MDNothingtodisclose.JohnFEidt,MDNothingtodisclose.JosephLMills,Sr,MD
Grant/Research/ClinicalTrialSupport:NIHInstituteofAging(abdominalaorticaneurysmstudy).Consultant/AdvisoryBoards:AnGes
(criticallimbischemia)CescaTherapeutics(criticallimbischemia).Speaker:Gore(bypasssummit[Polytetrafluoroethylene]).Other
financialinterests:Elsevier(vascularsurgerytextbooks).KathrynACollins,MD,PhD,FACSNothingtodisclose.
Contributordisclosuresarereviewedforconflictsofinterestbytheeditorialgroup.Whenfound,theseareaddressedbyvettingthrougha
multilevelreviewprocess,andthroughrequirementsforreferencestobeprovidedtosupportthecontent.Appropriatelyreferenced
contentisrequiredofallauthorsandmustconformtoUpToDatestandardsofevidence.
Conflictofinterestpolicy
http://www.uptodate.com/contents/primaryspontaneousupperextremitydeepveinthrombosis?topicKey=SURG%2F8211&elapsedTimeMs=1&source=se
24/24
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 3003-322 L3 Logbook Downloadable Unit v1Document12 pages3003-322 L3 Logbook Downloadable Unit v1Juan Francisco La Rosa MendozaNo ratings yet
- Chapter 101. Primary Hip Arthroplasty - I. Total Hip ArthroplastyDocument65 pagesChapter 101. Primary Hip Arthroplasty - I. Total Hip ArthroplastyVanessa Yvonne GurtizaNo ratings yet
- Abdominoplasty Classic Principles and TechniqueDocument18 pagesAbdominoplasty Classic Principles and TechniqueJonathan Zenteno JiménezNo ratings yet
- Dynamis User ManuelDocument123 pagesDynamis User ManuelStephen Chu100% (1)
- Holidays After StrokeDocument8 pagesHolidays After StrokeRifki YulianNo ratings yet
- Data Interpretation For Medical Students, 2e (Pastest)Document642 pagesData Interpretation For Medical Students, 2e (Pastest)Test MRCP100% (1)
- May ThurnerDocument1 pageMay ThurnerIoanaTNo ratings yet
- Vascular Board Questions NumberedDocument60 pagesVascular Board Questions NumberedAudrey Schlembach100% (6)
- Fungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportDocument5 pagesFungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportIJAR JOURNALNo ratings yet
- ClexaneDocument19 pagesClexaneahmadNo ratings yet
- SUCCEESSFULLY Navigating The First Year of Surgical ResidencyDocument56 pagesSUCCEESSFULLY Navigating The First Year of Surgical ResidencyYoya LawiNo ratings yet
- Effect of Fondaparinux Prophylaxis On Anti-Factor Xa Concentrations in Patients With Morbid ObesityDocument8 pagesEffect of Fondaparinux Prophylaxis On Anti-Factor Xa Concentrations in Patients With Morbid ObesityIdan LeviNo ratings yet
- Medic Hand Over 18 TH, 2011Document68 pagesMedic Hand Over 18 TH, 2011ikhoNo ratings yet
- Concept MapDocument4 pagesConcept MapDud AccNo ratings yet
- Clinical Questions and PICO 2012Document18 pagesClinical Questions and PICO 2012Gogularaajan RajendranNo ratings yet
- Emergency Internal Medicine: Rizal HafizDocument104 pagesEmergency Internal Medicine: Rizal HafizMotivation VoiceNo ratings yet
- Recall April 19 DR MominDocument7 pagesRecall April 19 DR MominShariq ShaNo ratings yet
- MS 2 NCP Deep Vein ThrombosisDocument4 pagesMS 2 NCP Deep Vein ThrombosisRosaree Mae PantojaNo ratings yet
- Emergency Medicine 1st Edition - DR - Waleed (101 Papers)Document101 pagesEmergency Medicine 1st Edition - DR - Waleed (101 Papers)Mokhtar Moh100% (1)
- Ethinylestradiol 15mcg + Gestodene 60mcg (Minesse)Document17 pagesEthinylestradiol 15mcg + Gestodene 60mcg (Minesse)asdwasdNo ratings yet
- Vaginal Hysterectomy and Vaginal Repair: Women's ServiceDocument16 pagesVaginal Hysterectomy and Vaginal Repair: Women's Serviceintan yulia safarinaNo ratings yet
- Reporting & Documenting Client Care: A Communication Skills ModuleDocument13 pagesReporting & Documenting Client Care: A Communication Skills Modulefarhan anwarNo ratings yet
- Naplex ReviewDocument63 pagesNaplex Reviewdivinevalley100% (7)
- A ObstetricsDocument87 pagesA ObstetricsGeraldine PatayanNo ratings yet
- 5 Deep Vein Thrombosis Nursing Care PlansDocument7 pages5 Deep Vein Thrombosis Nursing Care PlansSubhranil MaityNo ratings yet
- A Pulmonary EmbolismDocument11 pagesA Pulmonary EmbolismMonica Damayani SusiloNo ratings yet
- NICE 2010 Guidelines On VTEDocument509 pagesNICE 2010 Guidelines On VTEzaidharbNo ratings yet
- Air TravelDocument6 pagesAir TravelGulfishan HaqNo ratings yet
- Thrombosis Research: Full Length ArticleDocument6 pagesThrombosis Research: Full Length ArticleCarol GomezNo ratings yet
- Concept Map For EndocarditisDocument3 pagesConcept Map For EndocarditisSavanna ChambersNo ratings yet