Professional Documents
Culture Documents
Communicable Diseases
Uploaded by
jeshemaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Communicable Diseases
Uploaded by
jeshemaCopyright:
Available Formats
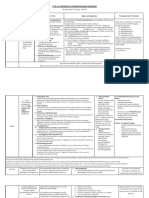
UNIVERSITY OF SANTO TOMAS
College of Nursing
COMMUNICABLE DISEASES NURSING
I.
Terminology
a. Communicable diseases can be transmitted through direct, indirect, break in the skin
integrity
i. Mode of transmission
1. Horizontal Transmission
a. Direct a person to person face to face encounter
i. Kissing
ii. Sexual contact
iii. Skin to skin contact
iv. Droplet VS Airborne(Indirect)
1. Source of infection
a. D- respiratory droplet droplet nuclei- sneezing,
coughing, singing
b. A respiratory droplet also
2. Size of source of infection:
a. D- bigger it remains in a surface
b. A smaller suspended in air
3. Distance to become infected
a. Dwithin 3 feet of the patient- AH1N1,
meningococcemia
b. A no limitation with regards to distance you
cannot stop the breeze of air
i. TB, measles, chickenpox
c. Airborne is more extensive than droplet
b. Indirect with intermediary object there is a bridge that connects
you to the individual
i. Vehicle borne- linens, catheter, bed pans, urinal inanimate
objects
ii. Vector borne insects, anthropods and rodents, rats living
things, non human
c. Break in skin integrity inoculation blood transfusion,
contaminated sharp and needles
d. Airborne
2. Vertical Transmission
a. Mother to child transmission perinatal transmission /
transplacental transmission
b. Infectious diseases there is a presence of living microbes in the body which may not
be transmitted through ordinary contact
c. Contagious diseases diseases that can easily be transmitted
d. All communicable diseases are infectious but not contagious.
i. Tetanus infectious only
ii. DHF communicable and infectious
e. Three factors to consider in epidemeologic triad
i. Host either man or animals > consider the susceptibility of the host pertaining
to the degree of resistance
1. If resistance is lowered prone to infection
2. Types
a. Patient individuals who are infected with signs and symptoms
least source of infection
b. Carrier who harbors the microbes but without signs and
symptoms- with higest potential to infect others
c. Suspect- whose medical history and symptoms that he may be
developing a specific infection
1
UNIVERSITY OF SANTO TOMAS
College of Nursing
f.
d. Contact with close association in contact or exposed to an
infected individual
ii. Agent microbes
1. Not all microbes possesses pathogenicity- capacity of the microbes to
cause an infection
2. Not all microbes possesses virulence strength and power of the microbes
to cause an infection
3. Most common- bacteria and virus
4. Virus only multiply in living things; very limited antiviral agent
a. Can pass thru filter in the body very very small
i. Blood brain barrier
ii. Placental barrier
1. German Measles fatal to the pregnant in 1 st to 2nd
trimester; more fatal in 1st trimester
b. Self limiting diseases kusang gumagaling
i. Colds adenovirus, rhinovirus
1. 2-3 days recovery
2. Watery nasal discharge
ii. Influenza
1. Recovery 7 days
2. If longer complication PNM
iii. Measles
1. Recovery 2 weeks
2. If longer complication- PNM or encephalitis
c. Permanent immunity
5. Bacteria
a. Can multiply in living and non living things
i. With specific antibiotics to specific bacteria
b. Easy to treat
c. Cannot thru filters in the body large molecules
i. Syphilis - Treponema pallidum can pass thru placental
barrier only after 16th week AOG second half of 2 nd
trimester third trimester; more fatal in third trimester
d. Temporary immunity
6. Protozoa
a. Plasmodium malaria
b. Amoebiasis
7. Fungi
a. Ring worm Tinea
i. Pedis feet
ii. Corporis body
iii. Capitis- head
iv. Crucis jock itch hadhad
v. Unguium onychomycosis nails
vi. Barbae barbers itch Beard
b. Tinea flavia or tinea versiculor malassezia furfur an-an
8. Rickettsia typhus fever proazeki, chuchuganami
iii. Environment conducive and favorable to the growth of microbes
1. C. tetani anaerobic
Immunity state of being resistant to infection and or free from infection
i. Natural inherent in the individuals body tissues and body fluid- innate, inborn
1. Race
ii. Acquired common, your body was able to produce antibodies or body was able
to get antibodies
2
UNIVERSITY OF SANTO TOMAS
College of Nursing
1. Active an actual participation of individuals body tissues and fluids in
producing immunity
a. PRODUCE antibodies yourself
b. Naturally acquired your body was able to produce the AB by
natural means, unintentionally
i. Situations to acquire: Previous infection , subclinical
immunity AB production due to constant exposure to
infection
c. Artificially acquired your body was able to produce the AB by
artificial means, intentionally done
i. Vaccines attenuated microbes avoid alcohol in cleaning
sites
ii. Toxoid attenuated or weakened toxins
2. Passive develop due to presence of antibodies within the serum not
coming from himself
a. GET ANTIBODIES
b. Naturally acquired by natural means, unintentional
i. Placental transfer of maternal antibodies 6 months
protection
1. 18 months stay of AB from the mother
ii. Breastmilk colostrums IgA transfer of IgA to the
colostrum
c. Artificially acquired artificial means, intentionally given
i. Anti serum
ii. Anti toxin
iii. Gammaglobulin
iv. Immunoglobulin
g. Immunization
i. Active to stimulate AB production
1. Weakened microbes
2. Weakened toxin
3. Effect: 4-7 days delayed production
4. Produce AB as long as you need it
5. Long lasting immunity
6. EPI vaccines anti rabies vaccine, tetanus toxoid,
ii. Passive
1. Give antibodies itself
2. Provide high titer of AB
3. Provide treatment
4. Effect: immediate
5. Short lived immunity
6. Anti rabies serum, tetanus antitoxin, anti tetanus serum, pertussis
immunoglobulin, heap B gammaglobulin
iii. TT and ATS IM deltoid, one in each area, separate syringe
iv. T. Toxoid given to pregnant
1. Effect to Baby: acquired, passive, natural
2. Effect to pregnant: active artificial
h. Chain of infectious process cycle
i. Causative agent microbes
1. DHF Dengue virus
2. Malaria Plasmodium
ii. Reservoir where it can multiply
1. Treponema pallidum Human
a. Genitals
2. Ah1n1 animals
3
UNIVERSITY OF SANTO TOMAS
College of Nursing
iii.
iv.
v.
vi.
vii.
viii.
ix.
3. Clostridium Tetani -soil
4. Measles human
a. Nasopharynx
5. Meningococcus human nasopharynx
6. Salmonella typhosa human intestines Peyers patches
Portal of exit way out to infect others; individuals body system
1. Measles- respiratory
2. T. pallidum- reproductive
3. Salmonella digestive
4. Meningococcemia respiratory
Modes of transmission- manner how the microbes is acquired -Means of
transportation; different from vehicle of transmission(source of infection)
1. Measles airborne
2. Rabies bites, scratch, licking of wound
3. Syphilis sexual contact
4. Typhoid fecal oral transmission/ ingestion
a. Vehicle feces, fomites, food
Portal of entry system; way to enter the individual
1. Measles- respiratory
2. Typhoid- GI
3. Syphilis- repro
4. Meningococcemia- respiratory
Susceptible host
In breaking any link mode of transmission is the weakest link
1. Fecal oral went from the anus >> went to the mouth
2. Oral fecal
3 factor to consider in caring the client
1. Know the Causative agent
2. Know the body secretion that harbors the microbes
3. Know the mode of transmission
General Nursing Care
1. Preventive you do not have infection yet
a. Health education change in knowledge, skills and attitude >>
change in behavior toward health
i. Person that is ultimately responsible for Health Education
MD
ii. Key provider RN we always remind the client
b. Immunization
i. Expanded Program Immunization PD 996 Marcos under
8 years old
ii. Cory Aquino UN goal universal child Proc No. 6 Under 6
years old
iii. Ramos- health for Filipinos Proc No. 46 under 5 years old
national immunity day
iv. Prevent 7 childhood diseases
1. BCG- TB
2. DPT
3. Measles
4. OPV
5. AMV
6. ***Cholera, Dysentery , Typhoid CDT given only
during epidemics gives only 6 months immunity
7. ***Anti- Rabies Vaccine given to animals bring to
barangay barangay captains
a. 2020 Philippines Rabies Fee
4
UNIVERSITY OF SANTO TOMAS
College of Nursing
b. 2010- Cebu rabies free
8. ***Flu vaccine give first to health workers >>
pregnant >> elderly , young children
9. ***not included in EPI but given free from health center
v. Contraindications
1. Permanent
a. Allergy
i. MMR eggs or Neomycin chick embryo
and neomycin
ii. HBV bakers yeast both have
saccharomyces
cerevisiae
>>
anaphylaxis
iii. Flu vaccine- chicken or chicken products
egg, feather, meat
iv. IPV inactivated polio vaccine SALK
vaccine
allergy
to
neomycin,
streptomycin
b. Encephalopathy without known cause or
convulsion within 7 days after pertussis vaccine
i. Convulsion indication of reaction in
pertussis component of drug DT vaccine
only; can cause permanent neurologic
disorder encephalopathy
ii. Encephalopathy 24 hours after DPT,
child is crying in consolably
2. Temporary resolve first the problem before giving
vaccine
a. Pregnancy
i. Cannot be given: live vaccines affect
fetal G and D MMR, OPV, BCG, Varivax
varicella vaccine; VZIG chickenpox if
with active infected house members
b. Very severe disease, severe febrile diseases
severe PNM
c. Immuno-compromised situation
i. Corticosteroids therapy
d. Recently received blood products- BT
i. Wait for 2-3 months before continuing
immunization
ii. MMR, AMV, Varivax
c. Environmental Sanitation
i. PD 856
1. Gonorrhea- 2x per month
2. Syphilis- 1x per month
ii. Proper disposal of garbage anti littering law PD 825
1. If throwing a litter- fine of2-5K and imprison from 6-12
months
d. Proper supervision of food handlers
i. Responsibility of DOH sanitary inspector inspects the
premises of food establishment
ii. FDA as of September 2009- food and drug association
2. Control there is infection; limit the spread of infection
a. Isolation separation of infected person during period of
communicability
5
UNIVERSITY OF SANTO TOMAS
College of Nursing
b.
c.
d.
e.
f.
g.
i. Strict Isolation protect other persons because microbes will
be within the patient
ii. Reverse Isolation / Protective Isolation protects the patient;
the microbes should be away from the patient
Quarantine limitation of freedom of movement of a well person
during the longest incubation period; separation of well yet exposed
individual
Disinfection- killing of pathogenic microbes by physical boiling,
washing- or chemical means;
i. Sterilization includes the spores
Disinfestations killing of undesirable small animal forms such as
arthropods and rodents by physical or chemical means
Fumimgation uses gaseous agents; kills the arthropods and
rodents
Medical asepsis handwashing most practical way and effective
to prevent spread of infection 10-15 seconds FRICTION- most
important factor of effective HW
i. Medical asepsis hands are lower than elbows
1. Use of barrier precautions PPE personal protective
equipment- use in direct contact with patient; use PRN
a. Sequence: gown > mask > goggles > gloves
b. Removing: gown > gloves > do hand washing >
goggles, mask > hand washing
2. Principle of Placarding signage in the bed
ii. Surgical asepsis hands are higher than elbows
Isolation precautions to prevent nosocomial infections
i. Category specific isolation first isolation precaution
conceptualized
1. Problem: you cannot implement if not diagnosed and
categorized
2. Respiratory
3. Enteric
4. Wound precautions
ii. Universal Blood and Body Fluid isolation Universal
Precautions implemented to patients with blood borne
precautions
iii. BSI Body substance isolations
iv. Revised isolation precaution
1. Standard precautions primary strategy used in
preventing nosocomial infection ; it has taken the
place of universal precaution
a. Applies to the following
i. All patients regardless of their diagnosis
ii. Blood and body fluids, excretions and
secretions except sweet
iii. Non intact skin
iv. Mucous membrane
b. Essential elements
i. Use barrier precaution used PRN
ii. Prevent
inadvertent
percutaneous
exposure needle stick and sharp ; DO
NOT recap, bend, manipulate, break
needles one hand recapping
iii. Immediate hand washing and washing of
other skin surface area
6
UNIVERSITY OF SANTO TOMAS
College of Nursing
2. Transmission based precaution- instituted to patients
infected with a highly transmissible infection
communicable disease
a. Precautions beyond those set forth in standard
precaution
b. Airborne precautions
i.
Respiratory
protection
-particulate
respirator N95- ultra filtrable mask
ii. HEPA filter high efficiency particulate
airflow
iii. Ex: measles, TB, varicella, SARS, avian flu
or bird flu
c. Droplet precaution be sure for the microbes will
not have contact with conjunctiva and nasal or
oral mucosa
i. Goggles and mask
ii. Ex: meningitis, Hib infections, PNM,
leprosy, Ah1N1, influenza, DP, mumps
d. Contact precaution protect self when
performing activites that require physical
contact and contact with inanimate objects
gloves and gown
i. Gi infections- cholera, tyhoid, skin
infections, scabies, ring worm, herpes
zoster, STIs, ebola
II.
CNS Infections
a. Bacteria
i. Tetanus painful muscular spasm leg cramps
1. AKA: Lockjaw
2. CA: Clostridium tetani anaerobic soil
a. Normal habitat: intestines of herbivorous animals
b. Spore- formed when outside body should undergo sterilization
c. When in the body: transforms into a vegetative form destroyed by
oxygen
3. MOT: wound break in skin integrity any kind of wound
a. Tetanus neonatorum wound is in the stump of the UC due to
poor cord care
4. Releases toxin that will bring about systemic symptoms
a. Tetanolysin dissolves the RBC >> anemic
b. Tetanospasmin muscle spasms; acts of the myo-neural junctions
of the muscles and internuncial fibers of the spinal cord and the
brain spasm of all muscles of the person
5. Incubation period 3 days to 1 month
a. Shorter the IP, poorer prognosis
b. Initially, wound inflammation
i. Rubor, calor, dolor, tumor, FUNCTION LOSS
6. Signs and symptoms
a. Initially sigs of wound inflammation
b. Increased muscle tone near the wound
c. Tachycardia, profuse sweating
d. Low grade fever
e. Painful muscular spasms involuntary muscle contraction
f. Muscles affected:
i. Masseter muscle mastication muscle > low jaw / trismus
rigidity of jaw muscles
7
UNIVERSITY OF SANTO TOMAS
College of Nursing
ii. Facial muscle Risus Sardonicus Sardonic Smile Ngiting
aso- smiling with eyebrows raised
iii. Extensor muscles of the spine- opisthotonus position- arching
of the back - naka-liyad
1. Side lying position
7. Diagnostics: no specific; clinical observations and history of wound
a. Patient with rigidity of jaw muscle ask if she has wound, bluok na
ngipin or nagkaroon ng sugat
8. Medical management
a. Objective:
i. Neutralize the toxin
1. ATS- anti tetanus serum / TAT Tetanus anti toxin
a. Skin test
2. TIg tetanus immunoglobulin
a. Human serum
ii. Kill the microbes
1. Antiobiotic- PCN
2. Daily cleansing of the wound betadine with NSS,
hydrogen peroxide
a. Thin dressing
iii. Prevent and control spasm
1. Muscle relaxants
a. Parenteral Diazepam IVP or IV Drip
(regulation: according to frequency of spasm
more frequent, faster drip) should be always in
vein irritating to the vein
b. Tablet form
i. Methocarbamol Roboxin or Robaxisan
ii. Lioresal Baclofen
iii. Eperisone Myonal
9. Nursing care
a. Maintain adequate airway and ventilation
b. Maintain an IV line for emergency drugs
c. Monitor clients for signs of arrhythmia
d. Prevent client from having spasm reduce stimuli
i. Exteroceptive outside bright light and noise, air from
electric fans
ii. Interoceptive- within the patient flatulence, stress, pain
iii. Proprioceptive participation of patient and others- jarring
the bed, touching the pain, turning the patient
1. Gentle Handling the patient
2. Minimal handling of the patient avoid unnecessary
disturbing the patient
a. Organize and cluster care do all in one setting
e. Prevent client from injury
i. Falls- most common
ii. Never leave patient alone
iii. Padded side rails and call light
iv. Fracture
f. Provide comfort measures
10.Prevention
a. Immunization
i. DPT
1. 6 weeks after birth
2. 3 doses with 4 weeks interval
8
UNIVERSITY OF SANTO TOMAS
College of Nursing
3.
4.
5.
6.
7.
0.5 cc
IM Vastus Lateralis
Expect fever to set in
Observe for convulsions within 7 days
Apply warm compress immediately vasodilation to
enhance absorption
8. After 20 minutes- cold compress VC to decrease
swelling
9. If with local tenderness, VC first then after 24 hours
hot compress
ii. Tetanus toxoid
1. 2nd trimester pregnancy
2. 2 primary doses with 1 month interval
3. Booster doses depends on mother; every time she
gets pregnant
4. IM Deltoid
5. 0.5cc
6. First dose today
7. 2nd one month after
8. 3rd 6 months
9. 4th 1 year
10.5th 1 year
11.Low risk booster dose every 10 years
12.High risk BD every 5 years
b. Proper wound care
i. Wash- soap and running water
ii. Thin dressing
iii. Band aid and Mediplast are allowed
c. Avoid wounds
b. Meninigits- inflammation of meninges
i. CA:
1. Virus CMV Cytomegalovirus not pathogenic; opportunistic infections
2. Fungus Cryptococcal Meningitis Cryptococcus Neoformans excreta of
birds opportunistic infections
3. Bacteria
a. TB meningitis inflammation of meninges caused by tubercle bacilli
b. Staphylococcus aureus secondary to skin infection
c. Pneumococcal meningitits- S. pneumonia secondary to respi
infection
d. Meningococcal meningitis meningococcemia / Spotted fever
most fatal and highly contagious- caused by: N. meningitides
i. Only type of meningitis where in vascular system is affected
>> at risk for DIC >> intravascular bleeding >> vascular
collapse >> death
ii. Only 10% are dying
iii. Signs and symptoms: waterhouse friderichsen fulminant
type of meningococcemia >> 6-24 hours, patient die;
intravascular bleeding, uncontrolled
ii. MOT: Droplet Direct
iii. IC: 2-10 days
iv. Signs and symptoms Meningococcemia - petechiae and ecchymoses
1. Nasopharynx >> URTI >> colds, cough, body malaise >> Bloodstream
>> vascular system affectation >>
UNIVERSITY OF SANTO TOMAS
College of Nursing
a. >> Petechiae formation pin point red spots on the skin, parang
kagat ng langgam, apply pressure the redness disappears
insect bite; the redness remains petechiae
i. Tumbler test clear glass to chest for petechia, side of glass
applied to the suspected petechial formation
b. >> Ecchymosis blotchy purpuric lesions pantal pantal reddish
violet
2. >> meninges >> nuchal rigidity stiffening of the neck, you cannot flex,
hyperextend or turn to side to side the neck
a. >> Kernigs sign place the patient in supine position >> flex the
knees towards the abdomen >> extend the leg
i. Positive: patient will complain of pain or difficulty in
extending the legs after flexion of the knees pain on the
hamstring back of thigh
b. >> Brudzinski sign place patient in supine position >> Flex the
neck
i. Negative: no reaction
ii. Positive: involuntary drawing up of the extremity or the hips
upon flexion of the neck
3. >> increase ICP decreased absorption of CSF
a. Severe HA
b. Projectile vomiting 2-3 feet away
c. Altered VS cushings triad
i. ^temperature infection
ii. Dec RR and PR
iii. ^systolic, normal diastolic widening pulse pressure
d. Seizure and convulsion- altered pressure in the intracranial cavity
e. Diplopia choking of the optic disk double vision
i. Test using finger counting
f. ALOC
v. Diagnostics
1. Lumbar puncture aspiration of CSF
a. Color:
i. Yellowish, turbid, cloudy infection, bacterial etiology
ii. Clear CSF normal, may be viral
b. Laboratory exam:
i. Caused by bacterial: expect that the CSF will have increased
CHON, WBC and decreased sugar
ii. Viral: ^CHON, ^WBC, normal sugar
c. Culture and sensitivity to determine the specific microbes and the
appropriate drug
d. CIE- Counter Immuno Electrophoresis to determine if the
causative agent is a virus or protozoa
e. CI: highly increased ICP- could cause brain herniation >> death
2. Blood Culture microbes can travel to the bloodstream
vi. Medical Management
1. Antimicrobial therapy
2. Anti-inflammatory Corticosteroids
a. No prednisone does not cross BBB causes Na retention
b. Dexamethasone or Hydrocortisone (Solu-cortef)
3. Osmotic diuretic
a. Mannitol
i. Check I and O first
ii. Check BP- SE of mannitol is hypotension
4. Anticonvulsant short term
10
UNIVERSITY OF SANTO TOMAS
College of Nursing
a. Phenytoin - Dilantin
i. Per oral do frequent oral care and massage can cause
gingival hyperplasia- gum overgrowth
ii. Per IV Sandwich it with NSS
1. Crystallization of the drug in the IV tubing
b. Hydantoin
vii. Nursing care
1. Assess neurologic functions
2. Maintain adequate nutrition and elimination to prevent constipation
strain - ^ICP
3. Ensure clients comfort
a. HA diversional soft music; no reading and watching TV
i. Elevate HA of bed 20-30 angle
ii. Non stimulating environment dim and quiet room
iii. Gentle nursing massage- petrissage or friction index finger
and middle finger
4. Symptomatic and sypportive
viii. Prevention
1. Immunization BCG, Hiv
2. Proper disposal of nasopharyngeal secretions
a. Best way: swallowing
b. CMV and TB do not swallow can affect stomach
3. Covering nose and mouth when sneezing and coughing
c. Encephalitis- inflammation of brain and encephalon
i. AKA: brain fever
ii. CA: Arbovirus arthropod borne virus
iii. Classifications
1. Primary E. the virus affects the brain directly - communicable
a. St. Louise
b. Japanese B
c. Australian X
d. Equine Eastern and Western Encephalitis
e. MOT:
i. Mosquito bites
1. Aedes sollicitans
2. Culex tarsalis
ii. Ticks of horses
iii. Migratory Birds
2. Secondary E. before the brain was infected, there was a previous
infection
a. A complication of a certain disease measles, chickenpox, mumps,
post vaccine encephalitis anti Rabies vaccine
3. Toxic E not caused by virus, caused by metal poisoning mercury and
lead poisoning
iv. Manifestations: same as meningitis
1. Initially behavioral changes ALOC lethargy abnormally sleepy or
difficult to awaken
v. Diagnostics: same as meningitis
1. LP
a. Clears CSF
b. Increase CHON, increase WBC, normal glucose
2. EEG to determine extent of brain involvement
a. With residual epilepsy or brain damage
vi. Medical management: symptomatic
vii. Nursing Care: same as meningitis
11
UNIVERSITY OF SANTO TOMAS
College of Nursing
viii. Prevention
1. Eradicate mosquito - insecticide, insect repellant, screen windows
2. CLEAN
a. Chemically treated mosquito net permethrin solution soak for 12 days air dry for 2-3 days; can be used for 3-6 months
b. Larva eating fish larvivorous fishes
c. Environmental sanitation 4PM habit
d. Anti mosquito soap basil soap
e. Neem tree /Eucalyptus tree
d. Poliomyelitis
i. AKA:
1. Infantile paralysis
2. Acute Flaccid Paralysis pathogmnomonic sign
a. Soft, flabby and limp
3. Heine- Medins Disease
ii. CA: Poliovirus Legio Debilitans enterovirus
1. Type 1 Brunhilde causes permanent immunity
2. Type II- Lansing temporary immunity
3. Type III- Leon temporary immunity
iii. How to acquire and MOT:
1. Early: During the first 4 days of infection microbes can be found in
pharyngeal area- droplet direct
2. Late: 5th day onward- intestines fecal oral transmission
iv. 10 years old and below- more susceptible
v. Poliomyelitis >> 10 years old >>
1. Invasive stage or Abortive stage microbes will invades the body; patient
will recover, aborting the infection
a. >> nasopharynx >> tonsils >> respiratory infections symptoms
>> Sore throats, fever, chills, HA, body malaise
b. >> Mouth >> Payers patches >. GI symptoms >> abdominal pain
and anorexia, NV, diarrhea or congestion
2. Pre- paralytic stage patient has involvement with CNS but without
paralysis
a. >> CLN- cervical lymph node
b. >> MLN mesenteric lymph node
c. CLN and MLN >> blood stream >> CNS
i. >> severe muscle pain warm bath or warm compress;
narcotic analgesic Codeine does not involve respiratory
depression
ii. >>stiffness of hamstring
iii. >> Hoynes sign head drop lift should of patient when in
supine head will be lagging or dropping
iv. >> Poker Spine opisthotonus with head retraction - cannot
assume sitting position
v. >> Tripod position to assume sitting position use both
hands to support the back
3. Paralytic Stage
a. Types of paralysis
i. Bulbar cranial nerves- any of the 12 most fatal
1. Most affected: 9 and 10; vagus respiratory symptoms
ii. Spinal type- most common
1. Anterior horn cell motor function extremities
paralysis, either upper and lower, paralysis of
intercostals muscles
iii. Bulbo-spinal
12
UNIVERSITY OF SANTO TOMAS
College of Nursing
1. Anterior HC and CN
4. As long as the patient did not enter the paralytic stage, the prognosis is
good.
vi. Diagnostic exam
1. Lumbar puncture- same as encephalitis
2. Throat washing or throat culture limitation: only in the 1 st 4 days
3. Stool exam 5th day onwards
vii. Medical management
1. Symptomatic and supportive
2. If with respiratory paralysis MV Iron Lung Machine Negative Pressure
breathing
a. No upper clothing- check for rise and fall of chest
viii. Nursing care
1. Supportive
2. Psychological care
ix. Prevention:
1. Immunization
a. OPV Sabin
i. 6 weeks after birth
ii. 3 doses with 4 weeks interval
iii. 2-3 gtts/ orem
iv. No feeding for 30 minutes
v. If vomited repeat vaccine
vi. If with diarrhea, give the vaccine but do not count it as a
dose
vii. Be careful in handling the stool only vaccine that the virus
will be eliminated in the stool
viii. If with immune-compromised family member, do not give the
vaccine= leukemia, steroid therapy- to protect the other
family members to be infected
1. Instead give IPV (Salk)
a. 6 weeks after birth
b. 0.5cc
c. IM
2. Avoid MOT
e. Rabies disease of a low form of animal warm blooded animals dogs, cats, raccoon,
skunk ,bat accidentally transmitted to man
i. AKA: hydrophobia, Lyssa, La Rage
ii. CA: Rhabdo virus (neurotropic- high affinity to neurons)
iii. MOT: Contact with saliva of a rabid animal
iv. Pathway of virus
1. Rhabdo virus >> peripheral nerves >> central nervous system >> Negri
Bodies pathologic lesions that are formed as microbes multiply ; if there
is no multiplication no Negri bodies
2. Rhabdo virus >>efferent nerves>> salivary gland where saliva is
produced
v. IP
1. Animals 3-8 weeks
a. Dumb stage complete change in disposition or behavior either
becomes withdrawn - stays in one corner, stays quiet OR very
affectionate walks in and fro manic
b. Furious stage animal is easily agitated >> easily bite >> vicious
look, drooling of saliva, animal will die
2. Humans 10 days-year; 21 years; average : 1-3 months
a. Invasive stage vague symptoms
13
UNIVERSITY OF SANTO TOMAS
College of Nursing
i. Bite will be numb, itchy or painful
ii. Flu like symptoms fever, sore throat
iii. Marked insomnia
iv. Restless, apprehensive, irritable
v. Kapag bite palang, not capable of infecting others
b. Excitement stage
i. Aerophobia
ii. Hydrophobia
iii. Can cause pharyngo-laryngospasm = painful
iv. Swallowing can cause spasms painful
v. Drooling of saliva
vi. Maniacal behavior rabid animal easily agitated, violent,
climb the walls and jump in the window
1. Antipsychotic agents
a. Haloperidol Haldol -IM
b. Benadryl sedative hypnotic effect IM
c. Paralytic Stage
i. No spasms
ii. Paralysis will set it rapid and progressive paralysis from
toes going up
vi. Within 24-72, patient will die after the symptoms appear
vii. Diagnostics done before signs and symptoms appear; all done to animals
1. Brain biopsy presence of Negri bodies
2. DFA test- Direct Fluorescent antibody test for rabies- confirmatory
3. Observation of animals (10 days)
a. If dog died within 10 days animal is rabid
b. Factors if dog will be observed
i. Site of the bite 3 mm per hour ; if waist up, no need for
observation
ii. Extent of the bite big bite, deep bite, multiple bite no
need to observe, instead vaccine
iii. Reason for the bite flight or fight response of the dog
1. Was the dog provoked or unprovoked?
a. Provoked- no need to worry
b. Unprovoked WORRY!
viii. Medical management post exposure prophylaxis lessens chances of
developing rabies but not 100% guarantee
1. Active immunization anti rabies vaccine
a. PVRV Purified Vero Cell Vaccine Verorab 0.5ml
b. PDEV Purified Duck Embryo Vaccine Lyssavac 1cc/ vial
c. PCEV Purified chick embryo vaccine Rabipur 1cc / vial
d. Given per IM
i. Do skin testing
e. Given per intradermal no need for skin testing
f. Site:
i. Adult: Deltoid area IM or ID
ii. Child: Vastus lateralis
g. Schedule
i. 3 doses
ii. Day 0, day 7, day 21 always add from the first dose
iii. IM
1. Day 0 2 vials one for each side
2. Day 7- 1 vial
3. Day 21 1 vial
14
UNIVERSITY OF SANTO TOMAS
College of Nursing
4. If completed 3 doses immunity for 3 years; if bitten
give only booster doses
5. If dog got lost, killed finish the 3 doses + booster
doses
6. Booster dose day 90 1 vial
iv. ID
1. 0.1cc
on
each
site
(Verorab)
/
0.2
cc
(Lyssabac/Rabipur)
a. D0
b. D3
c. D7
2. 01 cc on 1 site / 0.2 cc (Lyssabac/Rabipur)
a. D28-30
b. D90
2. Passive immunization
a. Coming from animal serum
b. ERIg equine Rabies Immunoglobulin
i. ARS anti Rabies Serum
ii. HyperRab
iii. Favirab
iv. Skin test before giving
1. If positive, provide human serum
a. HRIg- human rabies immunoglobulin
i. Imogram
ii. Rabuman
c. Dosage is computed according to BW the more wt, the more
amount
i. 0.2cc/kg BW animal serum
1. ARS
2. HyperRab
3. Imogam
ii. 0.133cc / kg BW human serum
1. Imogram
2. Rabuman
d. Given only within 7 days
e. Given IM ventrogluteal
i. If with deep, multiple and big bite divide the dose then one
is given ventrolgluteal; other is injected around the bite 4
point site injection
1. Neck up bite MD
2. Neck down bite RN
ix. Nursing Care
1. Keep water out of site
2. Symptomatic and supportive
3. Dim and quiet environment photosensitive and easily agitated
4. Room should be away from sub utility room where we wash articles
5. Restrain the patient before maniacal behavior sets in
6. Provision of comfort measures let patient die with dignity and comfort
x. Prevention
1. Be a responsible pet owner
2. Have the animals immunized
3. If one dog is rabid in a community give ARV to all dogs in the community
4. Keep away from stray animals greater chance of exposure to virus
5. Keep animals caged or chained
xi. Virus can die after 60C heat for 35 seconds.
15
UNIVERSITY OF SANTO TOMAS
College of Nursing
III.
Circulatory System
a. Virus DHF
b. Protozoa Malaria
c. DHF
i. Not the same as hemorrhagic fever
ii. CA: Arbovirus arthropod borne virus
1. Dengue Virus 1,2,3,4
2. Onyongyong Virus
3. Chikungunya Virus
4. West Nile
5. Flavivirus epidemic in the Philippines
iii. MOT: mosquito bite
1. Aedes Aegypti biological transmitter after 8-11 days, the mosquito can
spread the virus nagiging part na ng system ng lamok yung virus
2. Life span of mosquito: 4 months
3. Even the larva contains the virus
4. Day biting no specific time of the day
5. Clear stagnant water
6. Low flying mosquito
7. Geographical location urban areas; any part of the Philippines is a
Dengue risk area
iv. Virus >> blood stream >> multiply >> multiple lesions in blood stream
1. >> increased capillary fragility >> easy bleeding decreased
thrombocytes
2. >> increased capillary permeability >> allow fluid shift >> edema >>
ascites >> plasma leakage blood is concentrated hemoconcentration
v. Manifestations
1. Dengue without warning signs Dengue grade 1
a. High grade fever 3-5 day
i. Antipyretics RTC- decline in Temperature, gradual
b. Pain HA, retro-orbital pain behind eyes, joints and bone pains,
abdominal pain
c. Nausea and vomiting
d. Petechiae formation / Herman sign generalized redness of the
skin, generalized flushing
e. DENGUE FEVER ONLY no actual bleeding DANDY fever,
BREAKBONE fever
2. Dengue with warning signs with actual bleeding
a. Nose epistaxis, gum bleeding
b. Hematemesis, melena
c. Hematocchezia
3. Presence of severe DHF
a. Signs of circulatory failure
i. Cold clammy skin
ii. Cold extremities
iii. Prolonged capillary refill 3 seconds or more sluggish
1. Normal 1-2 seconds; less than 3 seconds
iv. VS
1. Decrease BP
2. Rapid but weak pulse thread
3. Rapid respiration
4. Dengue shock syndrome
a. Hypovolemic shock
vi. Diagnostic:
16
UNIVERSITY OF SANTO TOMAS
College of Nursing
1. Tourniquet or Rumpel Leede Test test for capillary fragility; presumptive
test
a. Check on BP of patient
b. Add S and D
c. Divide by 2
d. Quotient amount of inflation of the BP cuff
e. Inflate for
i. Children 5 minutes
ii. Adult 10 minutes
f. Deflate
g. Assess for presence of petechiae formation
h. Count petechiae in one square inch
i. More than or equal to 20 petechiae in one square inch
positive result
i. Criteria before performing Tourniquet Test:
i. Age of patient is 6 months or older with protection against
infection
ii. Fever of more than 3 days
iii. No other signs of DHF fever is the only complain
2. Blood Exam platelet count low confirmatory
a. Hematocrit hemoconcentration high
vii. Management
1. Symptomatic
a. No aspirin anti platelet
b. Provide coagulants
i. Vitamin K - methadione
c. Increase OFI
d. Oresol to maintain Intravascular volume
viii. Nursing care
1. Prevention and control of bleeding
2. Increase body resistance
3. No dark colored foods
4. Avoid red meat in preparation for occult blood test- 3 days before exam
a. Beef and liver
ix. Prevention
1. Eradicate mosquito
2. CLEAN Program
d. Malaria
i. AKA: ague
ii. King of tropical diseases
iii. CA: Protozoan plasmodium
1. Vivax- common in Philippines
2. Falciparum most fatal microbe which has a tendency to multiply very
rapidly; common in Philippines
3. Ovale
4. Malariae
iv. MOT:
1. mosquito bite Anopheles mosquito female sucks blood for
reproduction; biological transmitter
a. Night biting sunset to sunrise
b. Clear slow flowing water rural areas mountainous and forested
areas
i. 73 provinces- endemic in malaria
2. Blood transfusion
3. Contaminated sharps and needles
17
UNIVERSITY OF SANTO TOMAS
College of Nursing
v. Plasmodium >> Bloodstream >>
1. RBC where some microbes will be reproducing >> ruptures after
reproduction >> anemia; rupturing = chills >> fever microbes will be
back to the BS
2. Liver will not destroy the liver, wait for the liver to release RBC for them
to penetrate
a. not all microbes will penetrate the RBC; tambay lang yung iba- can
live for 3-5 years
vi. Manifestations - chills before fever
1. Stages
a. Cold Stage 10-15 minutes
i. Chilling sensation shaking of the body or shattering of the
lips
ii. Keep the patient warm blanket, hug, provide warm drinks,
expose patient to drop light, application of hot water bag in
the soles
b. Hot Stage 4-6 hours
i. Presence of fever
1. HA, abdominal pain and vomiting
ii. NR: lower down the body temperature TSB, cold compress,
light loose clothing, fluids you cannot immediately increase
the fluid intake of patient; if with neurologic sign, no need >>
increase ICP; antipyretics
c. Wet stage
i. Excessive sweating, feeling of weakness
ii. NR:
1. Make patient comfortable rest
2. Keep patient warm and dry
3. Increase OFI
2. Fever normal or subnormal
a. Other infectious diseases high fever
3. Severe anemia
4. Cerebral hypoxia
a. Restlessness, confusion, delirium, LOC, coma, convulsions
5. Black water Fever passing out black urine or dark red urine rapid
destruction of RBC- falciparum
vii. Diagnostics
1. Malarial Smear- before fever
2. QBC Quantitative Buffy Coat- rapid test for malaria- immediately extract
blood
viii. Medical management
1. Anti malarial
a. Chloroquine mainstay drug for treatment
b. Primaquine
c. Fansidar
d. Atabrine
e. Quinine very first developed; reserved drug given only if in
severe stage
i. If with resistance, give Artemesia Annua
f. Artemether from artemesia annua- first line of anti malarial
agents- IMCI
g. Abortifacient agents
i. Cautiously used for pregnant women
ii. Not a contraindication
iii. Neonatal malaria child from an untreated malarial mother
18
UNIVERSITY OF SANTO TOMAS
College of Nursing
IV.
1. Severely anemic >> die
ix. Prevention: Eradicate the mosquito
Integumentary System
a. Bacteria
i. Leprosy
b. Virus Eruptive Fever manifested by eruptions and rashes
i. Measles
ii. German Measles
iii. Chicken pox
iv. Herpes Zoster
v. If eruptions are found in mucous membrane enanthem
vi. Eruptions of skin exanthema
vii. Eruptions - characteristics
1. Macule flat rashes
2. Papule elevated rashes
3. Vesicle elevated rashes filled with fluid
4. Pustule- elevated rashes filled with pus
c. Leprosy
i. AKA: Hansens Diseases / Hansenosis
ii. Hansenites affected with leprosy
iii. CA: acid fast bacilli Mycobacterium leprae
iv. MOT:
1. Prolonged intimate skin to skin contact
2. Droplet high concentration in respiratory secretions
v. IC: 5.5 months 8 years
vi. Cardinal signs
1. Peripheral nerve enlargement
2. Loss of sensation not all body parts
3. Positive skin smear test for mycobacterium leprae
vii. Types:
1. Paucibacillary type- tuberculoid
a. Non infectious- less tendency to infect
b. Benign type mild manifestations; recovery is good ; good
prognosis
c. Mild
d. 1-5 skin patches and nodules
2. Multibacillary lepromatous type
a. Infectious- highly communicable
b. Malignant type
c. Severe manifestations >> Could cause death
d. More than 5 skin patches or nodules
3. Regardless of type- same manifestations
viii. Signs and Symptoms
1. Early
a. Color changes in skin that do not disappear even with treatment
hypopigmentation namumuti yung balat ng patien; mistaken for
an-an
b. Skin lesions that does not heal even with treatment ring worm like;
mistaken for fungal infection
c. Pain and redness of the eyes
d. Muscle weakness and paralysis of the extremities
e. Nasal obstruction and nose bleeding
f. Affected area
i. Loss of sensation
ii. Loss of hair growth
19
UNIVERSITY OF SANTO TOMAS
College of Nursing
iii. Anhydrosis
2. Late
a. Lagopthlamus- inability to close the yelids tulog na pero dilat
parin yung mata or half open
b. Madarosis loss of eyebrows / eyelashes
c. Sadlle-nose Deformity - Sinking of the bridge of the nose
i. As part of the disease process- there is absorption of the
small bones bridge of the nose, cartilage of the ears,
fingers and toes >> they undergo natural amputation no
need to bring to OR it comes by nature, no pain (loss of
sensation)
d. Leonine face resembling a face of a lion no eyebrows, triangle
nose
e. Contracture clawing of the fingers and the toes
f. Chronic skin ulcers
i. Problem: skin infections
g. Male: with gynecomastia enlargement of the breast
ix. Diagnosis
1. Skin Smear Test
2. Skin Lesion Biopsy to rule out malignancy
3. Lepromin test
a. Just like skin testing
i. Inject the antigen in the arm >> see the reaction of the
patient
b. To determine type of leprosy
4. Blood exam
a. Wassermann Reaction test
x. Medical Management
1. Multiple Drug Therapy (MDT)
a. Principle: combination of drugs
i. it would prevent drug resistance;
ii. it would hasten recovery;
iii. to lessen period of communicability (after 2 weeks of
treatment, patient will be non communicable)
b. Approaches
i. Paucibacillary Treatment
1. Rifampicin Once a month
2. Lamprene OD
3. 6-9 months
ii. Multibacilalry Treatment
1. Rifampicin once a month
2. Dapsone OD
3. Lamprene OD
4. 12-18 months
c. Should go to the health center every 28 days DOH
d. Patient should be patient enough to go to the health center.
e. Expected side effects that are considered to be harmless
i. Rifampicin orange urine, tears, saliva, sweat, stool
ii. Lamprene hyperpigmentation of the skin darkening of the
skin
f. Expected side effects because of the toxin released by the death of
microbes
i. Leprae reaction microbes are starting to die
1. Do not discontinue the drug
2. Go to HC to treat symptoms symptomatically
20
UNIVERSITY OF SANTO TOMAS
College of Nursing
3. Mild REST
a. Reddening in and around the nodule
b. Edema
c. Sudden increase in number of lesions
d. Tenderness and pain on the nerves
4. Severe -ISA
a. Iritis inflammation of the iris
b. Sudden acute paralysis
c. Acute orchitis inflammation of testes
ii. Management symptomatic treatment
g. Side effects that would warrant discontinuance of drug
i. Rifampicin hepatotoxicity
ii. Dapsone generalized rashes or itchiness
iii. Lamprene dryness or flaking of the skin
xi. Nursing Care
1. Psychological aspect of care low self esteem, altered body image, social
stigma
2. Skin care
3. Provide or Encourage physical exercise to strengthen muscles and
prevent contracture
4. Provide drug information
xii. Does not cross the placental barrier just delay the treatment- wait for the
mother to deliver because drugs have teratogenic effect
xiii. Prevention
1. Immunization BCG
2. Avoid MOT
d. Measles
i. AKA: Rubeola, Morbili, Hard Measles, Little Red Disease, 7 day measles, 9 day
measles, 1st disease
1. 6 common rash forming diseases in US
a. 1- Measles*
b. 2- Scarlet fever / Scarlatina strawberry tongue
c. 3- German measles*
d. 4- Dukes Disease / Filatov Disease
e. 5- Hungarian Measles / Slapped Cheek Disease/ Erythema
Infectiosum
f. 6- Roseola Infantum / Exanthem Criticum / Exanthem Subitum /
Tigdas Hangin children 6 months up to 3 years old *
g. * - common in Philippines
ii. CA: Paranaso virus- ruveola virus
iii. MOT: airborne
iv. Stages
1. Pre-eruptive
a. Before rashes appears
b. High grade fever for 3-4 days
c. 3Cs
i. Cough
ii. Colds
iii. Conjunctivitis inflammation of the conjunctiva puffiness of
eyelids, excessive nasolacrimal discharge (muta)
d. Photosensitivity
e. Koplick spots fine red spot with bluish white spots at the center
Pathogmnomonic sign; seen in inner cheek, just beside the molar
tabi ng bagang
i. After 24 hours > Eruptive stage
21
UNIVERSITY OF SANTO TOMAS
College of Nursing
2. Eruptive Stage
a. Maculo-papular rashes reddish in color, blotchy appearance
pantal pantal
i. Follow the hair line first in behind the ears, face ,neck
,trunk extremities Cephalocaudal
ii. When to appear: 3 day of illness
1. Within to 2-3 days entire body will have rashes
3. Post eruptive stage
a. Rashes will disappear by having a fine, branny desquamation from
red > brown > peel off
i. Only the rashes will be peeling off, not the whole skin
b. In the road to recovery
v. Diagnostics: Clinical Observation
vi. Management: Symptomatic
1. Antibiotics treat or prevent secondary bacterial infections
a. Complication:
i. broncho PNM can cause death
ii. encephalitis
iii. otitis media
vii. Nursing care: Symptomatic and Supportive
1. Maintain and increase body resistance of patient
a. Adequate nutrition
2. Keep patient warm and dry to prevent complications like PNM
3. Prevent exposure to draft- hamog
4. Can still bathe the patient
viii. When communicable: 4 days before and 5 days after appearance of rashes
ix. Highly communicable: before appearance of rashes
x. Prevention:
1. Immunization
a. AMV 9 months
i. 0.5cc
ii. SQ Deltoid
iii. May develop fever give antipyretic
iv. After 3-4 days the child may experience mild rash formation
normal reaction to the vaccine good reaction, childs body
was stimulated to antibody reaction
b. MMR
i. 12-15 months
ii. SQ
iii. Deltoid- 0.5cc
iv. Can be given to adult and adolescent
v. If female of childbearing age- no pregnancy for 3 months >>
can cause congenital defect
c. During epidemic give AMV or MMR at the age of 6 months but the
child would have to be revaccinated at age of 15 months- booster
dose
2. Proper disposal of NP secretions
e. German Measles
i. AKA: 3 day disease, Rubella, Roteln
ii. CA: Pseudoparamyxovirus Toga or Rubella Virus
iii. MOT: Droplet
iv. Stages
1. Pre eruptive
a. Presence or absence for fever if present, only for 1-2 days
b. 2Cs- cough and colds
22
UNIVERSITY OF SANTO TOMAS
College of Nursing
f.
c. Enanthem Forscheimers spot fine red spots or petechial spots
soft palate
i. If seen > patient will develop eruptive stage
2. Eruptive Stage
a. Presence of rashes macula popular rashes are pinkish in color and
discreet appearance smaller than in measles
i. Where: appears in cephalocaudal
1. Face > neck > trunk > extremities
ii. 24 hours entire body
b. Enlargement of lymph nodes one factor to differentiate M and GM;
differential diagnosis
i. Suboccipatal lymph node
ii. Posterior auricular LN
iii. Posterior cervical LN
3. Post Eruptive
a. Rashes disappears on the 3rd day of illness
b. Road to recover
c. Enlarged LN gradually subsides
v. Diagnostic exam: same as measles
vi. Medical management same as measles
vii. Nursing care same as measles
viii. Prevention same as measles
ix. Communicable: during entire course of disease
x. Fatal only if in pregnant women during 1 st 2nd trimester >> Congenital defects
1. Microcephaly
2. Congenital heart defect TOF, VSD, PDA
3. Congenital cataract could lead to blindness
4. Deafness and mutism
5. Exposure only can also predispose your child to these congenital defects
a. Receive gammaglobulin within 72 hours or 3 days
Chicken Pox
i. AKA: Varicella
ii. CA: Varicella Zoster Virus
1. Can be found on the nasopharyngeal secretions and secretions of the
rashes
2. Can cause infection if it enters the nasopharynx
3. Skin to skin contact- cannot acquire chickenpox
iii. MOT: Airborne
iv. Manifestations
1. For 24-48 hours mild manifestations
a. Presence or absence of low grade fever prior to rashes
appearance
b. HA, body malaise, muscle pain
2. Vesiculo-pustular or vesiculo-papular rashes
a. Earlier: 5-10 rashes that are flat muna- macule >> elevated
papule with another set of macule >> vesicle >> pustules
b. Itchy
i. Must tell patient to take a bath daily
1. Luke warm water bathe katamtamang lamig ng tubig
c. Rupture: Could develop into boil - pigsa, puruncle- big boil ,
carbuncle- dikit dikit na pgsa, cellulitis skin infection, gangrene
d. Permanent scarring > Pock marks
e. How distributed: generalized
i. Covered parts of the body first to appear Trunk and scalp
23
UNIVERSITY OF SANTO TOMAS
College of Nursing
f.
V.
Abundantly found in covered parts than in exposed parts of the
body
g. With unifocular appearance- one focus appears one at a time but
never fuses together
i. Kapag nagdikit dikit Herpes Zoster
h. Rashes could also be seen in mucous membrane buccal, vagina
i. When recovering: rashes will star to crust (dry), falls off (peel off)
by itself
v. Diagnostic- clinical examination
vi. Medical management Symptomatic
1. Antiviral agent- decrease duration of illness
a. Zovirax - Acyclovir 5x per day 7 - 10 days
i. Cream: prevent skin infections not the pock marks
2. Antipruritic agents
vii. Nursing care
1. Supportive
a. Skin care
b. Adequate nutrition and rest
viii. Communicable: until all rashes have crusted and dried
ix. Prevention:
1. Immunization
a. Varicella vaccine - Varivax
i. 12-18 months
ii. 0.5cc SQ Deltoid
iii. If less than 13 years old single dose only
iv. 13 and above 2 doses with 1 month interval
v. Fever
vi. After 3-4 days, mild rash formation normal reaction to
vaccine
2. Proper disposal of nasopharyngeal secretion
g. Herpes Zoster dormant type of chicken pox; inactive type you cannot acquire HZ
unless you have had CP
i. Usually infected: adults
ii. AKA: Singles, Zona, Acute Posterior Ganglionitis ganglion of posterior nerve
roots
iii. CA: Varicella Zoster Virus
iv. MOT: Direct Droplet
v. Manifestations
1. Same as chicken pox
2. Vesiculo-papular rashes
a. Painful
b. Itchy
c. Even patient has recovered, pain may persist up to 2 months
d. No generalized distribution
e. With unilateral distribution rashes follows the nerve pathway
longitudinal, vertical
f. Appears in cluster
g. Not only in the skin- can be on mucous membrane hard palate
vi. Diagnostics: Clinical Observation
vii. Medical Management: symptomatic
viii. Nursing care: supportive
ix. Prevention: same as chicken pox
Respiratory System
a. Bacteria
i. Diphtheria
24
UNIVERSITY OF SANTO TOMAS
College of Nursing
ii. Pertussis
iii. Pneumonia
iv. Tuberculosis
b. Virus
i. Colds
ii. Influenza
c. Diphtheria contagious disease
i. Affects all age groups
ii. Causes generalized toxemia
iii. CA: Corynebacterium diphtheria klebs Leoffler Bacillus
iv. MOR: Direct droplet
v. Manifestations
1. Nasal type
a. Irritating nasal discharge sero-sanguinous secretions with foul
mousy odor
b. Upper lip and nasal excoriation
c. Pseudomembrane is found in nasal septum needs nasal speculum;
covered by irritating nasal discharge
i. Grayish white membrane ash like
2. Pharyngeal / faucial
a. Sore throat
b. Dysphagia
c. Appreciated Pseudomembrane soft palate, uvula, pillars of tonsils
d. Neck edema anterior upper aspect of the neck: Bull Neck
Appearance
i. Inflammation of cervical LN
3. Laryngeal MOST FATAL
a. Affects voice box
b. Hoarseness of voice, aphonia (loss of voice) temporary
c. DOB, dyspnea; to compensate: use of accessory muscles chest
retractions, chest indrawing
d. Barking, dry metallic, croupy, dry husky cough
e. Respiratory distress or arrest
vi. Diagnostics
1. Nose and throat swab confirmatory test
2. Schick test to determine immunity or susceptibility to Diphtheria
3. Moloney Test to determine hypersensitivity to Diphtheria antitoxin
vii. Medical Management
1. Objectives:
a. Neutralize the toxin
i. Give anti diphtheria serum (ADS)
b. Kill the microbes
i. Antibiotic PCN
c. Prevent respiratory obstruction
i. Emergency tracheostomy
ii. ET tube may damage larynx stenosis respiratory
damage
viii. Nursing care
1. Provide client CBR to prevent the complication: myocarditis
a. Toxin released has special affinity to the heart muscle
b. Manifestations of myocarditis
i. Marked facial pallor
ii. Very irregular pulse rate
iii. Hypotension
iv. Chest pain
25
UNIVERSITY OF SANTO TOMAS
College of Nursing
v. Epigastric pain
vi. Notify MD ASAP to treat myocarditis
2. Maintain airway patent
a. Independent nursing:
i. Proper positioning folwers, upright position to maintain
adequate lung expansion
ii. Increase OFI liquefy secretions
iii. Encourage DBCE to aid in the expulsion of repspiratou
secretions
iv. CPT to loosen and mobilize secretions
v. Frequent turning to the sides every two hours to prevent
pooling of secretions
b. Dependent nursing:
i. Inhalation therapy
1. Oxygenation, nebulization, steam inhalation
ii. Suctioning as ordered
iii. Postural drainage
3. Provide adequate nutrition
a. Soft diet to lessen dysphagia
4. Provide comfort measures
ix. Prevention
1. Immunization
2. Proper disposal of secretions
3. Never kiss the patient
4. Cover the nose and mouth when sneezing and coughing
d. Pertussis
i. AKA: whooping cough, Chin cough
ii. Unlike D, pertussis affects children 6 years old and below
iii. CA: Bordetella pertussis, Hemophilus Pertussis both aerobic and anaerobic
iv. IP: 7-10 days
v. MOT: direct Droplet
vi. Manifestations
1. Catarrhal Stage highly communicable
a. Usually 1 week
b. Cold, fever, nocturnal coughing
c. Tiredness and listlessness (matamlay) opposite of restlessness
2. Paroxysmal stage / spasmodic stage
a. Pathogmnomonic sign: 5-10 successful forceful coughing, which
ends in a prolonged Inspiratory phase or a whoop
b. Congested face maga yung mukha
c. Congested tongue- purple in color
d. Teary red eyes with protrusion of eye balls
e. Distention of face and neck veins
f. Involuntary micturition and defecation
g. Abdominal hernia- pressure exerted on abdominal wall when
coughing
h. Chokes on mucus vomiting
i. F and E imbalance
3. Convalescent
a. Patient is no longer communicable
b. Signs and symptoms subside
c. On the road to recovery
vii. Diagnostics
1. Nasal swab
a. Recommended only in catarrhal stage many discharges
26
UNIVERSITY OF SANTO TOMAS
College of Nursing
2. Confirmatory test: naso-pahryngeal culture
a. Three cultures to be done
i. Bordet Gengou
ii. Agar Plate
iii. Cough Plate
viii. Medical management
1. DOC: Erythromycin PCN
2. Pertussis Immuneglobulin
3. F and E replacement
4. Codeine with mild sedation antitussive effect, suppress cough
ix. Nursing Care
1. Provide patient adequate rest conserve energy of patient, decrease
oxygen demand and consumption
2. Maintain F and E balance
3. Provide adequate nutrition but with SAP
a. Upright position
b. Patient experiences cough, hold the feeding
c. Nipples in bottle feeding should only have small holes medicine
dropper
4. Provide abdominal binder to prevent abdominal hernia
x. No permanent immunity but second attacks are rare below 6 years old
xi. Prevention
1. Same as diphtheria
e. Pneumonia hard sponge
i. Inflammation of the lung parenchyma
ii. CA:
1. Not highly pathogenic affects low body resistance individuals;
opportunistic infections to suffering people with AIDS
a. Virus - CMV
b. Protozoa
i. PCP Pneumocystic Carinii Pneumonia
2. Bacteria most common
a. CAP common type of PNM streptococcus PNM
b. HAP hospital acquired PNM staphylococcus PNM, Gram negative
bacteria (Pseudomonas, Klebsiella)
3. Inhalation of noxious substances
a. Aspiration PNM
b. Lipid PNM
i. Oil oil based lubricant
iii. MOT Direct droplet
iv. Manifestations
1. Fever
a. Onset: gradual or abrupt
2. Shaking chills Rigor
3. Productive cough
4. Sputum production
a. Rusty CAP
b. Creamy yellow Staphylococcus
c. Currant Jelly Klebsiella
d. Greenish Pseudomonas
e. Clear no infection
i. With PNM but no infection
ii. Aspiration or lipid PNM
5. Chest pain or pleuritic pain friction between pleural layers
a. Aggravated by coughing
27
UNIVERSITY OF SANTO TOMAS
College of Nursing
f.
b. Application of chest binder to prevent friction of lung layers
c. Apply pillow or splinting into the chest walls to lessen chest pain
d. Turn patient to side affected side to splint
i. IMCI: assess PNM
1. RR
a. 1 week 2 months 60bpm
b. 2 months 12 months 50 bpm
c. 12 months 5 years old 40bpm
2. Stridor harsh breath sound inspiration
3. Chest indrawing
4. Wheezing expiration
v. Diagnostics:
1. CXR definitive to check if there is stiffness in the lungs
a. Lung Consolidation
b. Patchy Infiltrates
2. Sputum Exam in the morning; first thing in the morning; upon rising
plenty of respiratory secretion, copious
a. 5-10ml of sputum
b. Deep breathing 3 times hold breath forceful expectoration
from the lungs
c. Done forcefully
d. Put tongue at the back of the lower teeth
vi. Medical management
1. Antibiotics
2. Inhalation therapy to loosen respiratory secretion for easy expectoration
vii. Nursing Care
1. Maintain airway patent airway Ineffective airway clearance
2. Provide adequate rest
3. Provide adequate nutrition
4. Provide comfort measures
viii. Preventive
1. Immunization
2. Same as diphtheria
Tuberculosis
i. AKA: Kochs infection, Phthisis Greek word for TB, Galloping Consumption, PTB
ii. CA: AFB
1. Mycobacterium Tuberculosis hominis- human ;
2. Bovis- cattles (inefficiently pasteurized cattle milk);
3. Avis birds MAC- Mycobacterium Avium Complex opportunistic
infections in patient who are suffering with AIDS particularly in abroad
iii. After 4-8 weeks symptomatic
iv. MOT: Airborne
v. Manifestations
1. Low grade fever, night sweats
2. Anorexia, weight loss, fatigability
3. Body malaise, chest pain and back pain
4. Productive cough, hemoptysis and dyspnea
5. Hemoptysis erosion of lung capillaries no CPT!; blood tinged sputum
bloody sputum
vi. Diagnostic exam
1. Tuberculin testing screening test for TB;
a. Positive result exposure to TB
b. Consistently positive developed sensitivity to the microbes
c. 4 things to know
i. PPD purified CHON derivative
28
UNIVERSITY OF SANTO TOMAS
College of Nursing
ii. ID
iii. Interpreted after 48-27 hours take 72 hours
iv. Positive more than 10mm induration
v. With HIV- 5mm positive
d. Techniques
i. Mantoux test ordinary skin test PPD 48 to 72 hours
1. Most accurate way of tuberculin testing; less pain;
easy to perform
ii. Tine Test / Multi- Puncture Test
1. Get a sterile needle soak needle in PPD for 3-4
hours puncture patient in circular manner for 6-8
times
2. Tine test kit- syringe; at tip, you have 4-6 needles
iii. Vollmer and Pirquet Test / Skin Scratch / Skin Patch Test
1. Get a sterile needle to make a scratch in your skin
get a gauze that is soaked in a PPD apply to the
scratch keep for 72- 96 hours after 72-96 hours,
remove gauze over scratch, wait for 48 to 72 hours
before you can have the result
a. Result: 5-7 days
2. Sputum exam presence of AFB diagnostic test
3. CXR determine extent of disease
a. Minimal PTB
b. Moderately advanced PTB
c. Far advanced PTB
vii. Medical management
1. Anti TB agents SCC Short Course Chemotherapy
a. To prevent resistance
b. RIPES
i. Rifampicin- hepatotoxic monitor liver enzymes, avoid
alcohol
1. Orange urine, tears
2. Before starting ask if with contact lens; remove
contact les, use eye glasses could permanently stain
with orange
ii. Isoniazid- hepatotoxic also
1. SE: peripheral neuritis
a. B6- Pyridoxine to counteract peripheral neuritis
iii. Pyrazinamide
1. SE: hyperuricemia gout and kidney stones
2. To promote excretion of UA: alakalinize the urine
increase OFI, increase milk intake, increase vegetable
intake
iv. Ethambutol
1. SE: optic neuritis irreversible
2. Observe for visual disturbances notify MD
3. Eye problems:
a. Color blindness most common
i. Difficulty differentiating red and green
v. Streptomycin
1. SE: ototoxicity 8th cranial damage; nephrotoxic
2. Observe for vertigo and tinnitus
3. Monitor I and O
4. Monitor Creatinine and BUN
viii. Nursing Care - DDR
29
UNIVERSITY OF SANTO TOMAS
College of Nursing
VI.
1. Provide adequate rest
2. Provide adequate nutrition
a. Small frequent feeding
b. Highly nutritious
3. Encourage drug compliance most important
a. DOTS
ix. Prevention
1. Immunization
a. BCG
i. At birth 1 dose 0.05ml
1. ID deltoid Right
ii. Do not massage spill the drug
iii. There will be abscess formation which will heal and develop a
scar
1. 2-3 months
iv. If with abscess 4 months Indolent abscess Kochs
Phenomenon
1. Reasons
a. Wrong technique of administration
b. Exposure to a person who is actively infected
with TB
2. Bring patient in HC I and D;
a. Prophylaxis: ID- 6 months; child 9 months;
immunocompromised 12 months
v. No booster doses School entrants BCG developed clinical
immunity
2. Proper disposal of secretion
3. Same with other respiratory infections
Gastrointestinal System
a. Bacteria
i. Typhoid
ii. Leptospirosis
iii. Bacillary dysentery
iv. Cholera
b. Protozoa amebiasis
c. Metazoan- schistosomiasis
d. Virus hepatitis
e. Helminthes- parasitism
f. Typhoid
i. CA: Salmonela typhi can be found on urine or stoll of an individual
1. Sources:
a. Fingers
b. Feces
c. Food
d. Fly
e. Fomites
ii. MOT: Fecal Oral
iii. Manifestations
1. Fever, dull HA, abdominal pain
2. Vomiting, diarrhea/ constipation
3. Payers patches- target organ of ST
4. Clinical features
a. Ladder like fever
b. Presence of rose spots found in abdomen or face (children)
i. Can have ulceration bleeding
30
UNIVERSITY OF SANTO TOMAS
College of Nursing
c.
iv. Diagnostics
1. Blood
a.
b.
Presence of splenomegaly
exam
Blood culture first week only 1 week only in bloodstream
Widals Test presence of antigen
i. AgO Somatic Antigen presently infected
ii. AgH Flageller antigen has been previously been exposed
to TF; had immunizations
c. Typhidot- detects antibodies
i. IgM- present infection
ii. IgG- recovery period and some form of immunity
v. Medical Management
1. Antibiotic Therapy
a. DOC: Chloramphenicol
2. F and E replacement
vi. Nursing Care
1. Maintain F and E balance
a. I and O
b. Signs of DHN
i. Before 48 hours: #1 indicator weight loss
1. 70% of body is fluid
2. Provide adequate nutrition
a. Limit oily and fatty foods aggravate diarrhea
b. Small frequent feeding if vomiting
c. If pediatric placed on NPO 4-8 hours to rest the GI tract then
clear liquids general liquids full diet
d. No NPO for adult clients
3. Provide patient comfort measures
vii. Prevention:
1. Immunization CDT
2. Avoid the five Fs
a. Handwashing
b. Food
i. Preparation
ii. Handling
iii. Storage
c. Eradicate flies
d. Do not put anything in your mouth
g. Leptospirosis
i. AKA: Mud Fever, Canicola Fever, Swamp Fever, Pre-tibial Fever, Icterohemorrhagica Disease, Weils Disease, Swineherds Disease
ii. Farm animals dog, cats, sheep, goat, rats (not given immunizations)
iii. Source of infection: Urine of rats
iv. CA: spirochete- Leptospira
v. MOT: Skin penetration, mucous membrane no need for wound can enter
pores of the skin
vi. Organism enter blood stream affects organs of the body striated muscles,
liver and kidneys (with special affinity with kidney cells) high risk for kidney
failure
vii. Incubation period: 2 days- 4 weeks; average: 5-6 days
viii. Manifestations
1. Fever, HA, vomiting, anorexia, body malaise
2. Muscle tenderness and pain calf muscles gastrocnemius does not
like to walk nor stand up
3. Jaundice with hemorrhage orange eyes and skin
31
UNIVERSITY OF SANTO TOMAS
College of Nursing
ix. Diagnostics
1. Blood exam
a. Leptospira Agglutination Test LAT
b. Leptospira Antigen Antibody Test LAAT
c. Microscopic Agglutination Test MAT - advanced
x. Medical Management
1. Antibiotic therapy Tetracycline
xi. Nursing care
1. Supportive
a. Monitor UO of patient
i. Consistency
ii. Frequency
iii. Amount
iv. Any Change Notify MD
xii. Prevention
1. Eradicate the source of infection rats
a. Rat poison
h. Dysentery
i. Types:
Bacillary
Violent- one after the other Amebic
diarrhea
Synonym
Shigellosis
Cholera, eltor
Amebiasis
Bloody Flux
CA
Shigella Dysenteriae Vibrio Cholerae before Protozoa
before SHIGA
Vibrio
Comma
(comma Entamoeba hystolitca
Strains:
shaped)
Stages:
- Flexneri
- Ogawa
- Inactive: Cyst
- Boydii
- Inaba
- Active: Trophozoites
- Sonnei
- Eltor
When outside the body:
cyst
MOT
Fecal Oral thru ingestion
Signs and Mucoid Stool, could be Rice, watery stool one after Mucopurulent
blood
symptoms
blood
streak
when the other: pathogmnomonic streak stools with foul
severe endotoxins sign
smell dissolves the
released
thus,
intestinal tissue
destroying
the Fishy odor stool
intestinal wall
Foul smell: because of pus
Enters the BS release
vibriolytic
substances
stimulate
peristalsis
diarrhea
No bloodstreak does not
destroy the intestinal wall
Rapid DHN manifested in
skin
integrity
Washerwomans
hand:
wrinkled, poor skin turgor,
dry skin
Waten bed special bed;
with hole and pail under the
bed
32
UNIVERSITY OF SANTO TOMAS
College of Nursing
Diagnostics
Stool exam
Rectal swab
Stool exam
Rectal swab
Medical
Manageme
nt
Antibiotics: Cotrimoxazole
ORT
Stool exam
Rectal swab
Antibiotics: Tetracycline
IVT continuous peristalsis
nothing per orem
Fresh within 30 minutes
trophozoites
(30
minutes to 1 hour)
transform into cyst
Antiamebic:
Metronidazole
or
Chloroquine
(anti
protozoan)
ORT
Nursing
Same as typhoid
Care
Prevention
Same as typhoid
i. Schistosomiasis
i. AKA: Snail fever, Bilharziasis
ii. CA: Schistosoma
1. Japonicum intestinal symptoms- affects man and animal
2. Mansoni intestine- intestina symptoms - man
3. Haematobium urinary symptoms- urinary bladder- man
iii. MOT: skin penetration / mucous membrane no need for wound
iv. Enter body of man in pairs male and female
1. Male with canal in the middle gynecoporic canal where female will
enter when they will copulate female will stay inside until she is ready
to lay her eggs after laying eggs go to portal circulation to find other
partner to lay eggs
v. Snail- intermediate host
vi. Feces with eggs rupture Larvae (Miracidium) not yet ready to infect man
or animal; 24 to 48 hours to find snail snail (incubator) Oncomelania Quadrasi;
stay in snail for 4-8 week if the microbes is now ready to infect man or animal
get out of the snail thru respiratory tract of the snail in the form of larva
(Cercariae) skin penetration / mucous membrane of man or animal
vii. Manifestation
1. Itchiness at site of entrance of the parasite
2. Fever infection
3. Calf and muscle pain
4. Dysentery-like symptoms (bacillary dysentery)
a. Mucoid
5. Emaciation payatot;
6. Abdominal distention(late sign)
a. if palpated, splenomegaly and hepatomegaly
7. lymph adenopathy
viii. Diagnostic exam
1. stool exam determine egg of parasite
2. confirmatory:
a. Blood exam
i. Circum Ova Precipitin Test COPT egg of parasite
ii. ELISA test
b. Rectal biopsy
ix. Medical Management
1. Antiblood Fluke Agent
a. Praziquantel, Fuadin
x. Nursing care: symptomatic and supportive
33
UNIVERSITY OF SANTO TOMAS
College of Nursing
j.
1. Poor prognosis in the Philippines
xi. Prevention
1. Snail control
a. Molluscides snail poison
b. Proper irrigation and cultivation of land destroy breeding places of
snail
c. Create fish ponds snail eating fish bangus
2. Environmental sanitation
a. Proper excreta disposal
b. Keep all animals caged or chained
c. Built foot bridges no need to cross a snail infested water
d. Proper wearing of foot wears boots
3. Health Education
Hepatitis inflammation of liver
i. Causes
1. Alcoholism
2. Drug intoxication
3. Chemical intoxications arsenic
4. Microbes
5. Virus
ii. Viral Type can be transferred to another
1. ABCDEG
2. Hepatitis A
a. AKA: Infectious Hepatitis / Catarrhal / jaundice/ epidemic Hepatitis
b. CA: Hepatitis A virus (RNA)
c. MOT: Fecal Oral
i. Food handlers
ii. Children
iii. Practices anal oral sex
d. IP: 2-6 weeks
3. Hepatitis B
a. AKA: Serum / Homologous / Viral (most fatal and deadliest)
b. CA: Hepa B Virus (DNA)
i. Blood and other body fluids- tears, saliva, sweat, milk,
semen, cervical fluid, pericardial fluid: Source of Infection
c. MOT:
i. Parenteral
1. BT, contaminated sharps and needles
ii. Oral to oral
1. Saliva, frequent kisses- 6-8 gallons of saliva
iii. Sexual contact
1. Seminal and cervical fluid
iv. Vertical
1. Infected mother to born child during the child birth
process
d. IP: 6-weeks 6 months
e. At risk:
i. Drug addicts
ii. Promiscuous individuals
iii. Health workers
4. Hepatitis C
a. AKA: Post Transfusion Hepatitis
b. CA: Hepa C virus
i. Blood
c. MOT: Parenteral contaminated sharps and needles
34
UNIVERSITY OF SANTO TOMAS
College of Nursing
d. At risk
i. Drug addicts
ii. Blood recipients
iii. Health workers
e. IP: 5-12 weeks
5. Hepatitis D
a. Dormant Type of Hepa B
b. CA: Delta Virus / Hepa D virus
i. Note: Delta virus cannot multiply by itself in order to
multiply, it needs the presence of Hepa B virus
ii. Once you developed Hepa B, even recovered there will be
left dormant virus help Hepa D virus to multiply
c. IP: 3-13 weeks
6. Hepatitis E
a. Enteric hepatitis
b. CA: Hepatitis E virus
i. feces
c. MOT: fecal oral
d. IP: 3-6 weeks
7. Hepatitis G
a. CA: Hepa G
i. Source of infection: blood
b. MOT: same as hepatitis C
c. IP: unknown
8. Partnership in MOT
a. A-E
b. B-D
c. C-G
iii. Manifestations
1. Pre-icteric- before jaundice appears; lesser degree
a. Fever- infection
b. RUQ pain inflammation, infiltration of liver
c. Fatigability, weight loss, body malaise inability of the liver to
convert glucose to glycogen (stored source of energy)
i. CHON amino acid should be de-aminase by the liver
ii. Fats
d. Anorexia, nausea, vomiting inability to deaminase the CHON
e. Anemia decrease life span of RBC (120 days)
2. Icteric phase
a. Jaundice inability of the liver to remove the normal amount of
bilirubin
b. Accumulation of bile salts on the skin pruritus / itchiness
c. Tea- colored urine / brown urine due to excess bilirubin thrown
out by the kidney to the urine
d. Acholic stool no color; clay colored stool
i. Unconjugated bilirubin (BS)
1. some will go to liver conjugated bilirubin
intestine to give rise for color of stool
2. Some will go to kidney urine color
3. Post icteric stage
a. Jaundice will subside
b. Signs and symptoms subsides
c. Energy level of patient increases; it would take 3-4 months for the
liver to recover or regenerate: Complete liver recovery REST;
avoid alcoholic beverages and OTC drugs for at least 1 year
35
UNIVERSITY OF SANTO TOMAS
College of Nursing
iv. Diagnosis
1. Liver enzyme test
a. ALT Alamine Aminotransferase SGPT
i. #1 indicator of liver problem
b. AST Aspartate Aminotransferase SGOT
i. Increases only upon onset of jaundice
c. ALP Alkaline Phosphatase
i. Increased obstructive jaundice / obstructive hepatitis
d. GGT Gamma Glutamyl Transferase
i. Increased Toxic Hepatitis caused by: alcohol, drugs or
chemicals
e. LDH- Lactic Dehydrogenase
i. Increased liver damage
2. Serum antigen antibody test what virus causing infection, chronic or
acute hepatitis
a. HBsAG acute hepatitis B
b. HBcAg- chronic Hepa B Increasing HBsAg
c. HBeAg
d. HAsAg exposure to the virus 2 weeks after
e. AntiHAV
i. IgG presently infected
ii. IgM
f. AntiHBS while recovering, it increases
g. Anti HBe
h. AntiHBc
3. Urinary exam
4. PT exam
5. UTZ of liver
v. Medical management
1. Symptomatic
a. Hepatic protectors phospholipid, vitamins and mineral
supplement liver will not exert effort to metabolize allow liver
for recovery
i. Essentiale / Silymarin
ii. Pedia: Jetipar
b. Chronic Hepa B
i. antiviral agent
1. Lamivudine
a. OD for one year
ii. Immune stimulant injectable
1. Interferon
a. 2-3x per week for 6 months
vi. Nursing Care
1. Rest to decrease metabolism decrease load of liver liver relax liver
recovery
2. Nutrition
a. Low fat no enough bile released by liver
b. High CHO to spare CHON metabolism
i. CHON amino acid ammonia encephalopathy
ii. Butterball Diet any hard candy but not chocolates because
it contains fats
c. CHON for tissue repair
i. If the patient is infected moderate CHON
ii. If patient is recovery high CHON
iii. If patient with complication Low CHON
36
UNIVERSITY OF SANTO TOMAS
College of Nursing
vii. NO PERMANENT IMMUNITY
viii. Prevention
1. Immunization
a. Hepa B vaccine
i. 3 doses
ii. 0.5cc IM
iii. Early infancy: vastus lateralis
iv. Late infancy : deltoid
v. Never given in gluteus muscles adipose tissues
decrease absorption
vi. 0-6-14 weeks
vii. If the birth weight is less than 2kg extra dose 10 th weeks
2. Avoid the MOT
k. Parasitism
i. Helminths
1. Ingestion
a. Enterobiasis
i. Pinworm infestation, seatworm
ii. Oxyuriasis
iii. Enterobis Vermicularis
iv. Nocturnal ani itchiness at night
1. Well fitted underwear at night
v. Only parasitism that cannot be diagnosed by stool exam
vi. Diagnostics
1. Scotchtape test / Cellophane tape test- morning
a. Glass slide with tape
b. Ascariasis
i. AKA: giant intestinal roundworm ascaris lumbricoides
ii. Manifestations
1. Vomiting and passing out of worms
2. Intestinal obstruction
c. Trichuriasis
i. Whipworm latigo
ii. Trichuris Trichiuria
d. Trichinosis
i. Round worm
ii. Trichiniasis
iii. Trichinellosis
iv. Trichinella Spiralis
v. Ingestion of raw meat, half cooked
e. Taeniasis
i. Tapeworm
ii. Ingestion of half cooked foods
iii. Taenia saginata beef tapeworm medium rare, half cook
iv. Taenia solium pork
v. Diphyllobothrium latum fish tapeworm sushi, sashimi
vi. Hymenolepsis Nana dwarf tapeworm
1. Person to person; hand to mouth transmission
vii. With segments could regenerate
f. Paragonimiasis
i. Flatworm
ii. Oriental Lung fluke
iii. Paragonimus westermani
iv. Insufficiently cooked of crab or crayfish
v. Productive cough and hemoptysis
37
UNIVERSITY OF SANTO TOMAS
College of Nursing
2.
VII.
Through the skin of the feet walking bare footed
a. Ancylostomiasis
i. Hookworm
ii. Ancylostoma Duodenale
iii. Necatus Americanus
iv. Seeps blood 50ml of blood is lost per day
b. Stongyloidiasis
i. Threadworm
ii. Strongyloide Stercoralis
ii. Manifestations
1. Voracious appetite
2. Weakness, pot belly, anemia
3. When young: stunted growth
iii. Diagnostics
1. Stool exam except for pinworm
iv. Medical Management
1. Antihelminthic
a. Mebendazole
b. Albendazole
c. Thiabendazole
d. Commercially prepared: Pyrantel Pamoate Combantrin
v. Nursing Care: symptomatic and supportive
vi. Prevention
1. Personal hygiene
2. Proper preparation of food
Genito-urinary system
a. Gonorrhea
i. AKA: Clap, Strain, Jack, GC, Gleet, Morning Drop - tulo
ii. CA: Neisseria Gonorrhea
iii. MOT: Sexual Contact
iv. IP: 3-21 days
v. Manifestations
1. Female: cervix no affectations of the urethra
2. Male: urethral involvement
a. Urethritis, dysuria
b. Redness and edema of urethral meatus
c. Purulent urethral discharge - morning
d. Frequent gonorrhea: formation of scar in the epididymis obstruct
sperm flow sterility
3. Female:
a. Asymptomatic
b. Signs and symptoms if cervix is affected PID
c. If urethra is affected same as males
d. Frequent: narrowing of the fallopian tube sterility / ectopic
pregnancy
4. Systemic Gonococcal septicemia
a. Gonococcal rashes tender papillary skin lesions (pustular,
hemorrhagic and necrotic)
b. Migratory polyarthralgia, polyarthritis, tenosynovitis
vi. Diagnostic
1. C and S mucosal scraping
a. They scrape the discharges coming from the urethral mucosa of the
patient
b. If no discharge cervical smear- Pap Smear
vii. Medical management
38
UNIVERSITY OF SANTO TOMAS
College of Nursing
1. Antibiotic
a. PCN Benzathine Pen G Penadur never given per IV; IM use only
i. If given per IV death
ii. Gauge 16-19 fast push; drug easy to clog
iii. ATB also for RHD prophylaxis against infection Penadur
b. Cephalosporin
i. Ceftriaxone
ii. Cefuroxime
c. If PCN and cephalosporin treatment is not effective patient may
have gonorrhea and chlamydial infection
i. Chlamydia trachomatis- with resistance with PCN and
Cephalosporing
ii. treat with Tetracycline Doxycline
1. Chlamydia clear discharge
viii. Nursing Care
1. Outpatient Basis
2. Psychological Care
a. Low self esteem
3. Health education
ix. Prevention
1. Safe sex practices according to CDC
a. No sex
b. Long term mutually monogamous relationship
c. Mutual masturbation without direct contact
d. According to Flavier - ABC
i. Abstinence
ii. Be Faithful
iii. Condom
2. Education and counseling
3. Behavior modification
4. Use of condoms
a. Preventive only; not a part of safe sex
x. Effect to child during pregnancy
1. Ophthalmia neonatorum blindness
a. Credes Prphylaxis
b. Syphilis
i. AKA: Pox, Lues, Bad Blood Disease(minimal amounts of microbes in the blood)
ii. CA: Spirochete Treponema Pallidum
1. Can pass thru placenta after 16th week
iii. MOT: Sexual Contact; blood transfusion
iv. IP: 10-90 days
1. Average: 21 days
v. Manifestations
1. Primary Stage chancre
a. Chancre
i. Painless, moist ulcer that heals spontaneously with or
without treatment (3-6 weeks)
ii. Usually found in genitals, face, lips, tongue, under the breast,
fingers
b. Presence of regional adenopathy
2. Secondary stage infectious stage
a. Highly communicable
b. Flu-like symptoms
i. Fever, HA, body malaise, sore throat
c. Skin rashes painful Condylomata lata / condyloma lata
39
UNIVERSITY OF SANTO TOMAS
College of Nursing
i. Lesions that are fused together, highly infectious, found
under the breast and on the genitals
d. Oral lesion- oral mucous patches
e. Changes in hair growth patchy alopecia
f. Thinning of pubic hair
g. Generalized lymph adenopathy
3. Latent Phase
a. Asymptomatic for 1-2 years
4. Tertiary / late stage
a. No longer communicable
b. Lesions Gumma infiltrating tumor (skin, bone, liver) seems
like the body to be decaying; found any part of the individual
c. CV changes
i. Aortitis and aneurysm
ii. reason for death
d. CNS degeneration
i. Paresthesia, psychosis, dementia, abnormal reflexes,
shooting pains
vi. Diagnostics
1. Dark Field microscope
2. Blood Exams
a. FTA ABS fluorescent Treponema Antibody Absorption Test
confirmatory
b. VDRL Venereal Disease Research Laboratory
c. RPR Rapid Plasma Reagin
vii. Medical Management same as gonorrhea
viii. Nursing Care same as gonorrhea
ix. Prevention same as gonorrhea
x. Dangerous if pregnant woman 3rd trimester
1. Possible defects:
a. Mother may have a stillbirth
b. Mother may give birth to a syphilitic baby placenta is bigger than
the baby
i. Baby will resemble like an old man; with linear scar at the
angles of the mouth; have persistent vesicular eruptions and
nasal discharges
c. Mother may give birth with late manifestations of syphilis
i. Normal but change 2 years after birth
1. Hutchinsons teeth- saw like teeth
2. Anterior bowing of the tibia
3. Dactylitis finger inflammation
4. Saddle nose with high palate horse like
5. Deafness
d. Mother may give birth with normal baby only after 2 years
c. HIV infection /AIDS
i. HIV is not AIDS
ii. HIV infection infected by a virus; initial stage of AIDS
iii. AIDS- infected with virus with group of signs and symptoms and with
incompetent immune system; late stage of HIV
iv. CA: Virus Human Immunodeficiency Virus retrovirus
1. Very fragile can be easily destroyed by alcohol 70%, chlorine, 56C, Na
hypochloride (Zonrox, Chlorox, Purex) no need to be concentrate (1 Na
Hypochoride: 10 Water)
2. Capable outside the body: 4 hours
3. Goes outside the body with blood virus is alive; up to 12 hours
40
UNIVERSITY OF SANTO TOMAS
College of Nursing
v.
vi.
vii.
viii.
ix.
a. If ordinary body fluid 4 hours
4. Death because of AIDS: As long as the body is humid virus is alive no
embalming
a. Cremated / directly buried within 24 hours
MOT:
1. Blood transfusion
a. Single exposure: 90%
2. Sexual contact
a. Single exposure: .1-1% to be infected
3. Exposure to contaminated blood products or tissue
a. Single exposure: .1-.5%
4. Perinatal or vertical exposure
a. No treatment: 30%
b. With Treatment: 5%
5. Contaminated sharps and needles
a. Single exposure: .1-.5%
Normal immune response:
1. Microorganism detected macrophage Alert T cells Stimulates B
cells release of antibodies destroy the microbes
a. Antigen- antibody reaction signs and symptoms
2. Cell mediated Immunity
a. Involves the T cells;
i. T cells serves as the backbone of immune system
responsible for secreting the lymphocytes first line against
infections
ii. Killer T cells / Cytotoxic cells tracks down infected human
cell to destroy
iii. Helper T cells inuutusan to stimulate B cells
iv. Suppressor T Cells when the infection is under control, the
STC tells the killer T cells to stop
3. Humoral Immunity
a. Involves the B cells
i. Produces the antibodies
ii. Stimulated by the Helper T cells
In HIV, defective T cells no immune defense
HIV virus has affinity with T cells did not detect macrophage, so did not alert
the T cells reverse transcriptase resemble the T cells
Well Worried Person infected with HIV remains asymptomatic takes time
to produce AB after 6 weeks to 6 months positive HIV infection production
of antibodies (Window Period- time between infection to the production of
antibodies) - ARC( AIDS related complex) symptoms AIDS
1. ARC:
a. fever with night sweats without a cause
b. enlargement of the lymph nodes without a cause (cervical, inguinal,
axillary)
c. memory loss + altered sleeping patterns + altered gait
2. AIDS: months to years
a. AIDS defining illness/ disease
i. Major signs
1. Fever- persistent 1 month and above pabalik balik
2. Chronic diarrhea- 1 month and above pabalik balik
3. 10% weight loss
4. For pedia: stunted growth
ii. Minor signs
1. Persistent cough 1 month and above
41
UNIVERSITY OF SANTO TOMAS
College of Nursing
x.
xi.
xii.
xiii.
2. Persistent generalized lymph adenopathy
3. Generalized pruritic dermatitis
4. Oropharyngeal candidiasis
5. Recurrent Herpes Zoster
6. Progressive dessiminated Herpes Simplex
iii. Adult: 2 major, 1 minorh
iv. Children: 2 major, 2 minor
b. Common Opportunistic Organisms months to years death
i. CMV, PCP
ii. Kaposi sarcoma blood vessel wall malignancy manifested in
the skin
1. Pink or purple painless spots on the skin
2. Leopard Look
iii. Candidiasis Oral Lesions
iv. OHR oral hairy leukoplakia
Diagnostics
1. ELISA test screening test
a. 2 positive WB
2. Western Blot confirmatory
3. Blood Test: HIV Viral Load shows the replication activity of the virus
4. CD4 cell count: determine if the stage of infection is AIDS or HIV
a. Normal: 1200 cells
b. More than or equal to 200 HIV
c. Less than 200 AIDS
5. For pedia:
a. Blood culture for HIV detect the microbes
b. Immune Complex Dissociated 24 Assay detect presence of
antigen
Medical management
1. Symptomatically
2. Giving of anti retroviral agents in combinations 4 groups Cocktail Drugs
a. 21 tablets per day
b. Does not allow the virus to multiply
c. NRTI Nucleoside reverse transcriptase inhibitor- terminates viral
replication
i. AZT- Azidothymidine, Zidovudine, Retrovir
1. Check CBC SE: agranulocytosis AZT
d. NNRTI Non Nucleoside reverse transcriptase inhibitor blocks the
DNA activity of the virus
i. Nevirapine Viramune
e. Protease inhibitor for the maturation of virus- inhibits
i. Saquinavir Invirase
ii. Indinavir Crixivan
iii. Ritonavir Novir
f. Fusion inhibitor
i. Prevents fusion of the virus to human cell
ii. Enfuvirtide Fuzeon
g. If with hepatotoxicity and nephrotoxicity stop treatment for
awhile
Nursing Care
1. Symptomatic and supportive
2. Counseling- better understanding and knowledge of disease process;
a. Promote quality of life
b. Provide self care and comfort
Prevention
42
UNIVERSITY OF SANTO TOMAS
College of Nursing
1. Same with other STIs
xiv. Can be in saliva- 6-8 gallons
43
You might also like
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Expanded Program On ImmunizationDocument15 pagesExpanded Program On ImmunizationReygie MarsadaNo ratings yet
- CD HandoutDocument20 pagesCD HandoutiandameNo ratings yet
- Communicable Disease NursingDocument50 pagesCommunicable Disease NursingGreggy Ventura100% (1)
- CHN Final TopicsDocument52 pagesCHN Final TopicsMary Ann SacramentoNo ratings yet
- Infectious DiseasesDocument10 pagesInfectious DiseasesAgnes Marie RendonNo ratings yet
- Nle Test Plan For July 2012 Nle: Nursing Practice IDocument7 pagesNle Test Plan For July 2012 Nle: Nursing Practice IPhilip AdallaNo ratings yet
- Pharmacology ReviewerDocument15 pagesPharmacology ReviewerKathrynne MendozaNo ratings yet
- NP1 BulletsDocument17 pagesNP1 BulletsJea VesagasNo ratings yet
- Communicable Disease 2Document12 pagesCommunicable Disease 2Bianca CordovaNo ratings yet
- Dec2012nletips MCHN 121021230343 Phpapp01 PDFDocument7 pagesDec2012nletips MCHN 121021230343 Phpapp01 PDFJessamine Rochelle Reyes EsbertoNo ratings yet
- Np1 CHN HandoutsDocument61 pagesNp1 CHN HandoutsRiezah EncisaNo ratings yet
- CD 1Document13 pagesCD 1Don MarcusNo ratings yet
- Palmer Set 4Document8 pagesPalmer Set 4Karen Mae Santiago AlcantaraNo ratings yet
- Board Exam 4Document20 pagesBoard Exam 4Kira100% (9)
- Professional Adjustment Final 2Document41 pagesProfessional Adjustment Final 2lielani_martinezNo ratings yet
- Nle Test Plan: Nursing Practice IDocument14 pagesNle Test Plan: Nursing Practice IericNo ratings yet
- Psychiatric Nursing ReviewerDocument7 pagesPsychiatric Nursing ReviewerJay Soriano0% (1)
- Disaster Nursing (Midterm)Document3 pagesDisaster Nursing (Midterm)Farrah SalcedoNo ratings yet
- Practice Test 4Document15 pagesPractice Test 4Kira100% (9)
- Sexually Transmitted DiseasesDocument5 pagesSexually Transmitted Diseasesreghpineda28No ratings yet
- Professional Adjustment and Nursing JurisprudenceDocument65 pagesProfessional Adjustment and Nursing JurisprudenceJAY LAPAZ ANDRES, RN, BSN, MAN (C), MAEd.. (C)100% (2)
- Perioperative Nursing: Rose Delia P. Ocariza, RN, MANDocument66 pagesPerioperative Nursing: Rose Delia P. Ocariza, RN, MANDeva HiyasNo ratings yet
- Preoperative Surgical NursngDocument271 pagesPreoperative Surgical NursngPaw PawNo ratings yet
- Fundamentals of Nursing Gladys Bautista Jaime 2010Document10 pagesFundamentals of Nursing Gladys Bautista Jaime 2010Clarissa GuifayaNo ratings yet
- CD HandoutsDocument27 pagesCD HandoutsricogonzzzNo ratings yet
- Medical Surgical Nursing TionkoDocument40 pagesMedical Surgical Nursing TionkojeshemaNo ratings yet
- Professional Adjustment and ResearchDocument26 pagesProfessional Adjustment and ResearchjeshemaNo ratings yet
- PA and ResearchDocument36 pagesPA and ResearchjeshemaNo ratings yet
- Communicable Disease Nursing Study BulletsDocument12 pagesCommunicable Disease Nursing Study Bulletsoh_chamieNo ratings yet
- Pre Board ResultsDocument28 pagesPre Board ResultsMichael MontañoNo ratings yet
- CHNDocument7 pagesCHNRichard GeeNo ratings yet
- CHN HandiesDocument23 pagesCHN HandiesFreeNursingNotesNo ratings yet
- Community Health Nursing Part 1Document64 pagesCommunity Health Nursing Part 1Jim Ryan PauloNo ratings yet
- Pnle Answer and Explantion 4Document12 pagesPnle Answer and Explantion 4Lloyd rafaelNo ratings yet
- NP1 BulletsDocument17 pagesNP1 BulletsJea VesagasNo ratings yet
- Communicable DiseasesDocument20 pagesCommunicable DiseasesKILLUANo ratings yet
- Sample Nursing Exams-BudekDocument4 pagesSample Nursing Exams-BudekLj FerolinoNo ratings yet
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument20 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- Maternal and Child Health Nursing CompressDocument15 pagesMaternal and Child Health Nursing CompressRy Llanes100% (1)
- Pediatric NursingDocument29 pagesPediatric NursingjeshemaNo ratings yet
- PHC II - Sample ExamDocument35 pagesPHC II - Sample ExamMelvin VillasNo ratings yet
- CHN Reviewer Mock ExamDocument6 pagesCHN Reviewer Mock ExamLorenz CapacioNo ratings yet
- Community Health Nursing - REVIEWERDocument45 pagesCommunity Health Nursing - REVIEWERmary navalNo ratings yet
- Goal 3: Good Health and Well-: Placed in The Center of The Public Health BagDocument26 pagesGoal 3: Good Health and Well-: Placed in The Center of The Public Health BagHed KcamNo ratings yet
- Prelims Pedia 102Document10 pagesPrelims Pedia 102quidditch07No ratings yet
- HeheezjghDocument7 pagesHeheezjghDemiar Madlansacay QuintoNo ratings yet
- Communicable and Infectious Disease Nursing-NewDocument15 pagesCommunicable and Infectious Disease Nursing-NewShandz de RosasNo ratings yet
- Nutrition 1Document6 pagesNutrition 1jeshemaNo ratings yet
- Communicable DiseaseDocument41 pagesCommunicable DiseaseMrz AlzNo ratings yet
- NP2Document49 pagesNP2Edward Nicko GarciaNo ratings yet
- Gapuz Communicable Disease NursingDocument46 pagesGapuz Communicable Disease NursingBJ DUQUESANo ratings yet
- Nle Tips For OrthopedicDocument2 pagesNle Tips For OrthopedicCharie OcampoNo ratings yet
- CD HandoutsDocument80 pagesCD HandoutsMayflor GuiyabNo ratings yet
- Answer and Rationale Communicable Disease NursingDocument17 pagesAnswer and Rationale Communicable Disease NursingCharles Gerard B. BeluanNo ratings yet
- Philippine Nurses Licensure ExaminationDocument18 pagesPhilippine Nurses Licensure ExaminationHenry ApolNo ratings yet
- CDN IntroDocument40 pagesCDN Intro01 TONGOL, LAILANI B.No ratings yet
- Communicable Disease Prevention and ControlDocument197 pagesCommunicable Disease Prevention and Controldennisjamesbartz100% (1)
- Communicable Diseases Part 12Document23 pagesCommunicable Diseases Part 12Kenneth Reigne ArguidasNo ratings yet
- Tomas Lao Vs NLRCDocument6 pagesTomas Lao Vs NLRCjeshemaNo ratings yet
- Traders Royal Bank Vs CADocument8 pagesTraders Royal Bank Vs CAjeshemaNo ratings yet
- CIR Vs NortonDocument4 pagesCIR Vs NortonjeshemaNo ratings yet
- RF Sugay Vs ReyesDocument3 pagesRF Sugay Vs ReyesjeshemaNo ratings yet
- Umali Vs CADocument9 pagesUmali Vs CAjeshemaNo ratings yet
- Musculoskeletal Problems Rev 11.21.07Document191 pagesMusculoskeletal Problems Rev 11.21.07jeshemaNo ratings yet
- Boyer-Roxas Vs CADocument8 pagesBoyer-Roxas Vs CAjeshemaNo ratings yet
- Musculoskeletal Problems Rev 11.21.07Document103 pagesMusculoskeletal Problems Rev 11.21.07jeshemaNo ratings yet
- Francisco Motors Vs CADocument6 pagesFrancisco Motors Vs CAjeshemaNo ratings yet
- VITAMINSDocument31 pagesVITAMINSjeshemaNo ratings yet
- Medical Surgical Nursing Review 1Document422 pagesMedical Surgical Nursing Review 1jeshemaNo ratings yet
- Protein Energy MalnutritionDocument38 pagesProtein Energy Malnutritionjeshema100% (2)
- Research 2Document78 pagesResearch 2jeshemaNo ratings yet
- High Risk NewbornDocument68 pagesHigh Risk NewbornjeshemaNo ratings yet
- Prelims Lecture BNP RevisedDocument65 pagesPrelims Lecture BNP RevisedjeshemaNo ratings yet
- Medical Surgical Nursing Review 1Document31 pagesMedical Surgical Nursing Review 1jeshemaNo ratings yet
- Nutrition - Vitamins Part 2Document29 pagesNutrition - Vitamins Part 2jeshemaNo ratings yet
- Unit 1 Introduction To Nutrition: Anita A. Cabezon RN, MPHDocument47 pagesUnit 1 Introduction To Nutrition: Anita A. Cabezon RN, MPHjeshemaNo ratings yet
- GastrointestinalDocument63 pagesGastrointestinaljeshema100% (2)
- Macro MineralsDocument56 pagesMacro Mineralsjeshema100% (3)
- Eyes and Ears DisordersDocument36 pagesEyes and Ears Disordersjeshema100% (4)
- Care of Clients With Integumentary ProblemsDocument26 pagesCare of Clients With Integumentary ProblemsjeshemaNo ratings yet
- Gastrointestinal and HepatobiliaryDocument54 pagesGastrointestinal and Hepatobiliaryjeshema100% (2)
- BurnsDocument31 pagesBurnsjeshema100% (1)
- The Ten Lepers SkitDocument6 pagesThe Ten Lepers SkitPastor JeanneNo ratings yet
- Lorenzo v. Director of HealthDocument1 pageLorenzo v. Director of HealthYeyen M. EvoraNo ratings yet
- Giorgio Agamben - MetropolisDocument3 pagesGiorgio Agamben - MetropolisJackNo ratings yet
- A Lesson Plan On Field Visit: Holy Family College of Nursing Subject: Nursing EducationDocument15 pagesA Lesson Plan On Field Visit: Holy Family College of Nursing Subject: Nursing EducationShivani SrivastavaNo ratings yet
- Leprosy in Pregnancy: Devi Noviana Saputri Surya DoriskaDocument15 pagesLeprosy in Pregnancy: Devi Noviana Saputri Surya DoriskaHardi SetiyoNo ratings yet
- Immunology in LeprosyDocument17 pagesImmunology in LeprosyDr Daulat Ram DhakedNo ratings yet
- Health Problems MyselfDocument54 pagesHealth Problems MyselfKrishnaveni Murugesh100% (2)
- IntroductionDocument10 pagesIntroductionNareman Alaa50% (2)
- Lorenzo Vs Director of HealthDocument2 pagesLorenzo Vs Director of HealthJessamine OrioqueNo ratings yet
- FNCP LeprosyDocument7 pagesFNCP LeprosyChristian Eduard de DiosNo ratings yet
- Pathophysiology: Mycobacterium Leprae/ Mycobacterium LepromatosisDocument2 pagesPathophysiology: Mycobacterium Leprae/ Mycobacterium LepromatosisAkeroNo ratings yet
- cmr00057 0094 PDFDocument19 pagescmr00057 0094 PDFSadam_fasterNo ratings yet
- 2024-Article Text-6560-1-10-20230128Document4 pages2024-Article Text-6560-1-10-20230128Adniana NareswariNo ratings yet
- Manual: Federal Ministry of Health EthiopiaDocument196 pagesManual: Federal Ministry of Health Ethiopiaalfonso delgadoNo ratings yet
- The History of Bacteriology Bullock 1938Document476 pagesThe History of Bacteriology Bullock 1938Andersinclair AndersinclairNo ratings yet
- 2.01 Medieval Period and Renaissance: OutlineDocument5 pages2.01 Medieval Period and Renaissance: OutlineManila MedNo ratings yet
- Communicable DiseaseDocument193 pagesCommunicable DiseaseLuvastranger Auger100% (2)
- Leprosy & Pregnancy: DR Y Sri HarshaDocument53 pagesLeprosy & Pregnancy: DR Y Sri HarshaBhawna Joshi100% (1)
- Different Types of Disabilities: List of 21 DisabilitiesDocument6 pagesDifferent Types of Disabilities: List of 21 DisabilitiesjasonNo ratings yet
- Cte #2: Matrix of Communicable DiseasesDocument7 pagesCte #2: Matrix of Communicable Diseasesjoannamae molagaNo ratings yet
- D.Pharm 1 Year ER20-15T-Social Pharmacy: LeprosyDocument46 pagesD.Pharm 1 Year ER20-15T-Social Pharmacy: LeprosyPriyanshu SharmaNo ratings yet
- The Origin and Spread of Leprosy: Historical, Skeletal, and Molecular DataDocument30 pagesThe Origin and Spread of Leprosy: Historical, Skeletal, and Molecular DataNaeNo ratings yet
- Term 2 Nur 153 Answer KeyDocument14 pagesTerm 2 Nur 153 Answer KeyMargie BalunesNo ratings yet
- 150 - Mycobacterium LepraeDocument83 pages150 - Mycobacterium LepraeNirav PatelNo ratings yet
- Leprosy - Mumal BakliwalDocument13 pagesLeprosy - Mumal BakliwalAni SharmaNo ratings yet
- Derma Trans Clerks Review 2019Document22 pagesDerma Trans Clerks Review 2019anonymousNo ratings yet
- Nadopod 2004Document21 pagesNadopod 2004Jin Yi LimNo ratings yet
- 4.22 - Quiz LeprosyDocument32 pages4.22 - Quiz LeprosyEdo LiawandiNo ratings yet
- MF3 - LeprosyDocument25 pagesMF3 - LeprosyAnnbe BarteNo ratings yet
- Erythema Nodosum LeprosumDocument23 pagesErythema Nodosum LeprosumSulfia SuhardiNo ratings yet