Professional Documents
Culture Documents
Pediatric Nursing
Uploaded by
Wendy EscalanteCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Nursing
Uploaded by
Wendy EscalanteCopyright:
Available Formats
Growth
>Refers to quantitative changes-increases in size and structure
>As aOF
result
the growth
of FAMILY
the brain,(escalante-saac)
the child has a greater capacity for learning,
1 PEDIATRIC NURSING: CARE
THEofCHILD
AND
for remembering, and for reasoning. He grows mentally as well as physically
Development
>refers to qualitative changes
>its used to denote an increase in skill and ability to function
>it is a progressive series or orderly coherent changes
Progressive
>changes are directional
Orderly
>suggests that there is a relationship between a given stage and the stages which
precedes or follow
Principles of Growth and Development
1. Growth and Development are continuous processes from conception until death
2. Growth and Development proceeds in an orderly sequence
a) Cephalo- caudal
b) Proximal- distal
3. Different children pass at different rates
All body systems does not develop at same rate
There is an optimum time for initiation of experiences in learning
Primitive reflexes must be lost before development can proceed
A great deal of skill and behavior is learned by practice
Factors influencing Growth and Development
Genetic influences
Race and nationality
Sex
Intelligence level
Health
Environmental influences
HAVIGHURSTS developmental task for childhood
Birth to 6 years
Learning to walk
Learning to take solid foods
Learning to talk
Learning to control the
elimination
Achieving physiological
stability
Forming simple concepts
Learning to relate oneself
emotionally
Learning to distinguish right
and wrong
Learning physical skills
6-12 years
necessary for ordinary
games
Building wholesome attitude
toward oneself as a growth
organization
Learning to get along with
age mates
Learning an appropriate
masculine or feminine sex
roles
Developing fundamental
skills in reading writing
calculations
Developing conscience,
mortality, and as scale of
values
Achieving personal
independence
Computation of the weight and height of infants and children
From 1-6 years
Weight in pounds(lbs.) = age in years x 5 + 17
From 6-12 years
Weight in pounds(lbs.)= age in years x 7 +5
For infants below 6 months of age
Weight in grams= age in months x 600 + birth weight (300 grams)
For 6-12 months
Weight in grams= age in months x 500 + birth weight (300 grams)
Usual changes in weight at different age
At 4-5 months -------------------------------------------------------------- 2 x birth weight
At 1 year --------------------------------------------------------------------- 3 x birth weight
At 2 years -------------------------------------------------------------------- 4 x birth weight
At 3 years---------------------------------------------------------------------5 x birth weight
At 5 years -------------------------------------------------------------------- 6 x birth weight
At 7 years -------------------------------------------------------------------- 7 x birth weight
2 PEDIATRIC NURSING: CARE OF THE CHILD AND FAMILY (escalante-saac)
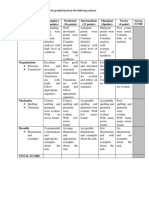
CRITERIA
Appearance(color)
Pulse, HR,
Grimace(reflexes)
Activity(muscle tone)
Respiration
0
Pale
Absent
No response
Flaccid
Absent
1
Blue
<100 bpm
Grimace
Some flexion
Weak
2
Pink
>100bpm
Cough/ sneeze
Well flexed
Good cry
TEMP REGULATION
-In utero, its increased than mothers temp
-Heat loss/unit body wt is 4x than that of adult due to its greater surface are in relation to the BW.
-Temp should be taken/rectum
PE
Color, respiration, cry is lusty, vigorous
Skin
Pink tinged and warm to
-Increased concentration of RBC in the blood vessels and SQ fats
touch
-White cheese like substance w/c serves as skin lubricant
Vernix caseosa
-Vasomotor disability
Acrocyanosis
-When lying skin appears red on the dependent side
Harlequin sign
-Plugged sebaceous glands
Milia
-Bluish black pigmentation
Mongolian spots
-Breakdown of RBC at birth, inc lvl of bilirubin leads to jaundice
Physiologic jaundice
HEAD
Inc ICP
Bulging fontanelles, fontanelle tenses
Diamond shape(2-3 cm
Anterior fontanelle
width, 2-4 cm length)
Triangular shaped
Posterior
Molding
Assymetrical
Caput succedaneum
Localized soft are of scalp
Cephalhematoma
Collection of blood resulting from ruptured blood vessels bet surfaces of cranial base
and periosteum
Signs of bone pathology:
*Microcephaly
*Craniotabes
POSTURE
Fit are dorsiflexed, flexed body and will offer resistance when extremities are
straightened
Chest
Bell shaped and <HC
Face and neck
Tongue is large-cretinism
High palatine arch- small head and mental retardation
Laxity and webbing of neck- Down/turner syndrome
Abdomen
Cardiac sphincter not well developed
Umbilical stump 6-10 days healed slough off
Omphalocele-esophageal atresia
Liver is palpable 2-3 cm below right costal arc
Genitalia
-Undesceded testes
-Slightly swollen owing to hormone activites w/ mother
Skeletal
Bones are soft- Compose of cartilage
Feet is flat- plantar fat pads
Blood coagulation
The majority of newborns are born w/ prolonged coagulation time because there
blood levels of vit K are lower than normal
Vit K is synthesized to the action of intestinal flora
A newborn intestine is sterile @ birth unless membranes were ruptured >24 hrs of
delivery
Flora must therefore accumulate before Vit K be synthesized
Autoimmune system
The newborn infant has difficulty antibodies against invading antigens until he
reaches 2mos of age
This is why immunization against childhood dx are not given to babie <2mos old
Neuromuscular system
Limpness or total absence of muscular responses to manipulation is never normal
and suggests narcosis, shock or cerebral injury
Blink reflex
Protects the eye from any objects coming near it by rapid eye closure
Rooting reflex
Newborn check is brushed/stroke near the corner of his mouth, the child turns his
head in that direction. Serves help baby find the food.
Sucking reflex
Infant lip is touched makes sucking motion
Extrusion reflex
Any substance is placed in the anterior portion of infants tongue, he will extrude it.
Its a protective reflex to prevent infant from swallowing inedible substances.
Disappears in 4mos of age
Palmar grasp reflex
When object is placed in newborns palm, child will grasp it by closing fingers on it;
disappears 6 wks-3 mos
Plantar grasp reflex
When an object touches the sole of newborns foot at the base of toes, his toes grasp
in some manner as his fingers; disappears 3 mos
Lies on his back, his head turns to other side; the arm and leg on the side to w/c his
head turns extend and the opposite arm and leg contrasts; disappear 2 nd-3rd mos of
life
Moro reflex
Startling the infant by loud noise or jumping his bassinet, the infant abducts and
extends his arm and leg; his fingers assume atypical C-position
Babinski reflex
When the side of sole of newborns foot is stroked in J curve from the heel upward,
3 PEDIATRIC NURSING: CARE OF THE CHILD AND FAMILY (escalante-saac)
Magnet reflex
Landau reflex
Step in place reflex
INFANT CARE CONCERS
1. Bathing
2. Diaper area care
3. Clothing
4. Care of teeth
5. Exercise
6. Sleep
HEALTH PROBS IN INFANT
1. Constipation
Ribbon like stools
Bouts of diarrhea
Failure to meet dvptal
milestone
Congenital hypothyroidism
2. Loose stools
Loose stools, distended
abdomen, def. in fat soluble
vitamins
3. Lactose intolerance
4. Colic
5. Spitting up
6. Miliaria
the newborn fans his toes in contrast w/ adult; occurs because of immaturity of
nervous system; fade 3 mos of age
If pressure is applied to soles of ft of infant in supine pos, he pushed back against
pressure
When newborn is hel in prone pos w/ hand underneath him supporting his trunk, he
should demonstrate some muscle tone
Newborn in vertical pos, his ft touches a hard surface, he will take few quick
alternating steps, disappear 3 mos
Helps infant learn different textures and sensations and provide opportunity to
exercise and kick
A good time for parent to spend time talking to child and communicating
Dont allow infant to wear a lengthy period of time
Frequently changed every 4hrs
Easily laundried
Not be binding dapat
Teach parents to begin brushing an infant as 1st tooth arise
Use soft brush and water once a day to prevent plaque from forming
2 wks- expose skin to sunlight, it provides natural source of vit D, no >3-5min if 1 st
day
Best time-11 am and after 3 pm
Suggestion to eliminate or at least cope w/ night walking
Delay bedtime 1 hr shorten an afternoon sleep period dont respond immediately to
the child at night to be certain that baby wont fall asleep again
Because stools tend to be loose
Stools infrequent in formula fed infants if diet is too high in protein, fat/ deficient in
fuid
If it persists beyond 5-6 mos- add food w/ bulk such as foods/veges such as
increased fluid intake
Prune juice maybe given but too much may cause diarrhea
Infants w/ hx of constipation for >1 wk should be examined for anal fissure/ tight
anal sphincter
SX OF HIRSCHPRUNGS DISEASE
Chronic constipation may occur in children w/ _
Stools of breast fed infants are generally softer than those who are formula fed
infants
May begin w/ introduction of solid foods such as fruits
Malabsorption syndrome/celiac disease or inability to digest fats may manifest itself
1st by:
Inquire about duration of loose stools:
*The number os stools/day
*Color and consistency
*any mucus ot blood in tehm
*Associated fever cramping & vomiting
Lactose is broken down in the intestines by the enzyme lactase
Sx:
Abdominal pain, flatulence, bloating, diarrhea
Paroxysysmal abd pain that generally occur in infancts under 3 mos of age
Sx:
Infants cries loudly and pulls leg up against abdomen
Face is red and flush
Fist clenched
Abdomen is tense
-major prob for parents because its frightening
-The infant appears to be in acute pain and the distress persist for hrs usually in
middle of night
BASIC RULE:
-Avoid heat in case appendicitis is developing
-Hot water bootles and heating pads shouldnt be used because eof the possibility of
burning the delicate skin of infants and young children
Ask pts to describe how they burp the infant, sicne burping thoroughly often helps
limit spitting up
They may put infant in an infant chair for half an hr after feeding
Reassure parents that it decreases in amt as baby can better coordinate swallowing
and digestive process
Or prickly heat- rash occurs most often in warm weather or when babies are
overdressed or in overheated rooms
SX:
Cluster of pinpoint
Reddened papules w/ occasional vesicles and pustules surrounded by erythema
4 PEDIATRIC NURSING: CARE OF THE CHILD AND FAMILY (escalante-saac)
-Bathing infants 2x a day during hot weather is added to bathwater- may improve
rash
CHILD REARING CONCERNS
1. Teething
High fever, convulsions, vomiting, diarrhea and earache are never normal
signs of teething.
Discourage use of OTC drugs because they may contain bentocaine and if applied
too far back in the throat may interfere with gag reflex
Acetaminophen is the best treatment
2. Thumb sucking
Parents should be taught that thumb sucking is normal and does not deform the jaw
line as long as it stops by school age
Be sure the infant has adequate sucking pleasure and then ignore thumb sucking
3. Pacifier
A baby who has colic craves sucking and enjoys pacifiers because his abdomen
hurts and interprets this as hunger sensation
EFFECTS OF SEPARATION FROM PARENTS
Kind of parenteral care
Factors
Kind of person
Maternal deprivation
Term used for an infants lack of warm relationship
EFFECTS OF DEPRIVATION (1ST 6 MONTHS)
1. Becomes emotionally isolated from adults
2. Retarded mental development
3. Cry great deal
4. Poor motor development
5. Will refuse contact with adults
EFFECTS OF DEPRIVATION (2nd 6 MONTHS)
Period of analyctic depression occurs
1. Depressed infants
2. Look sad cry a great deal
3. Withdrawn in their relationship with adults
4. May refuse to eat, loose weight
5. Respiratory disturbance
Walks alone
The 15 month old (toddlerhood)
Creeps upstairs
Build a tower of 2 blocks
Holds a cup with fingers
around it
Grasps spoon but spills
content
Pat pictures in book
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fundamentals in NursingDocument9 pagesFundamentals in NursingWendy EscalanteNo ratings yet
- Degenerative Joint DiseaseDocument35 pagesDegenerative Joint DiseaseWendy EscalanteNo ratings yet
- Recognition Day Script: Maunlad Na Kinabukasan"Document2 pagesRecognition Day Script: Maunlad Na Kinabukasan"Argel Cochico100% (6)
- High School Newsletter October2Document8 pagesHigh School Newsletter October2api-102758902No ratings yet
- KINESIOTHERAPHYDocument40 pagesKINESIOTHERAPHYJeyarajasekar TtrNo ratings yet
- Assessment of Kidneys PDFDocument1 pageAssessment of Kidneys PDFWendy EscalanteNo ratings yet
- PATHODocument2 pagesPATHOWendy EscalanteNo ratings yet
- NCP 2 MiDocument16 pagesNCP 2 MiWendy EscalanteNo ratings yet
- NCPDocument3 pagesNCPWendy EscalanteNo ratings yet
- Drug StudyDocument14 pagesDrug StudyWendy EscalanteNo ratings yet
- Nasogastric Tube Management and CareDocument21 pagesNasogastric Tube Management and CareWendy EscalanteNo ratings yet
- Caring For The Bedridden PatientDocument1 pageCaring For The Bedridden PatientWendy EscalanteNo ratings yet
- Concept Map of CKD Gastrointestinal SymptomsDocument4 pagesConcept Map of CKD Gastrointestinal SymptomsWendy Escalante0% (1)
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendDocument2 pagesModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- 02 Orig Art 02 PDFDocument3 pages02 Orig Art 02 PDFWendy EscalanteNo ratings yet
- Assessment of KidneysDocument1 pageAssessment of KidneysWendy EscalanteNo ratings yet
- Concept Map of Carotid Artery DiseaseDocument2 pagesConcept Map of Carotid Artery DiseaseWendy EscalanteNo ratings yet
- Acid-Ash DietDocument10 pagesAcid-Ash DietWendy Escalante0% (1)
- At DietDocument8 pagesAt DietWendy EscalanteNo ratings yet
- Brat DietDocument8 pagesBrat DietWendy EscalanteNo ratings yet
- Pediatric NursingDocument16 pagesPediatric NursingWendy Escalante100% (1)
- Therapeutic DietDocument3 pagesTherapeutic DietWendy EscalanteNo ratings yet
- Drug Study FinalDocument8 pagesDrug Study FinalWendy EscalanteNo ratings yet
- Nursing Care For Patient With Neurological DiseaseDocument8 pagesNursing Care For Patient With Neurological DiseaseWendy EscalanteNo ratings yet
- FNCP CommunityDocument4 pagesFNCP CommunityWendy EscalanteNo ratings yet
- Case Presentation: Group 2Document30 pagesCase Presentation: Group 2Wendy EscalanteNo ratings yet
- DM Report1Document16 pagesDM Report1Wendy EscalanteNo ratings yet
- Integrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsDocument78 pagesIntegrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsWendy EscalanteNo ratings yet
- Diabetes MellitusDocument5 pagesDiabetes MellitusWendy EscalanteNo ratings yet
- Jesse Balaban-Feld - CVDocument4 pagesJesse Balaban-Feld - CVapi-337804038No ratings yet
- EN3NG03 Soft Skills IDocument2 pagesEN3NG03 Soft Skills IsourabhNo ratings yet
- B2 Use of English Test 01-Pages-2-5Document4 pagesB2 Use of English Test 01-Pages-2-5ThivennyaNo ratings yet
- Impulse Control DisorderDocument22 pagesImpulse Control DisorderAhmad AltarefeNo ratings yet
- Mid Test PsycholinguisticsDocument4 pagesMid Test Psycholinguisticsnurul rifaaNo ratings yet
- Air-in-Line Alarms: Decreasing Alarms Through Antisiphon Valve ImplementationDocument3 pagesAir-in-Line Alarms: Decreasing Alarms Through Antisiphon Valve ImplementationSjis11362No ratings yet
- Pavan Kumar ResumeDocument3 pagesPavan Kumar ResumeThirumalamohan KotaNo ratings yet
- In Lak'ech, The Chicano Clap, and FearDocument24 pagesIn Lak'ech, The Chicano Clap, and FearLuntyChanNo ratings yet
- 04 Circular 2024Document17 pages04 Circular 2024dwivediayush926No ratings yet
- Guru Tattva - Freedom VidyaDocument4 pagesGuru Tattva - Freedom VidyaRavan SharmaNo ratings yet
- Rubric For StorytellingDocument2 pagesRubric For Storytellingapi-298487060No ratings yet
- IEEE STD C37.14-1992 - IEEE Standard For Low-Voltage DC Power Circuit Breakers Used in EnclosuresDocument46 pagesIEEE STD C37.14-1992 - IEEE Standard For Low-Voltage DC Power Circuit Breakers Used in EnclosuresnovitopoNo ratings yet
- My ResumeDocument3 pagesMy ResumeKc Velle Pagangpang ReginaldoNo ratings yet
- Propst ReportDocument5 pagesPropst ReportJosh Bean0% (1)
- 76th Peterborough Kiwanis Music Festival ProgramDocument16 pages76th Peterborough Kiwanis Music Festival ProgramPeterborough ExaminerNo ratings yet
- Action Plan in MathDocument4 pagesAction Plan in MathRoselyn Catubig Vidad Jumadla100% (4)
- Trudell - 7th Grade Concert ProgramDocument1 pageTrudell - 7th Grade Concert Programapi-663957641No ratings yet
- Key Point Slides - Ch5Document21 pagesKey Point Slides - Ch5Nuzul DwiNo ratings yet
- CSS - TGDocument150 pagesCSS - TGJenniferBanogonNo ratings yet
- 0 Title 1Document12 pages0 Title 1RODJHEN ANNE P. BARQUILLANo ratings yet
- Regents Exam ScheduleDocument1 pageRegents Exam ScheduleSaraNo ratings yet
- WFA Competency LevelsDocument5 pagesWFA Competency LevelsTroy Lyons DunowNo ratings yet
- You Will Learn How To: Introduce Yourself. Ask People About Some Specific InformationDocument4 pagesYou Will Learn How To: Introduce Yourself. Ask People About Some Specific InformationPaula Valentina Hernandez RojasNo ratings yet
- 20 Points RubricsDocument1 page20 Points RubricsJerome Formalejo,No ratings yet
- AirWatch Device Features Summary v8 - 1Document3 pagesAirWatch Device Features Summary v8 - 1Razvan CristeaNo ratings yet
- The Abington Journal 02-01-2012Document20 pagesThe Abington Journal 02-01-2012The Times LeaderNo ratings yet