Professional Documents
Culture Documents
755 - Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
Uploaded by
zakCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
755 - Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
Uploaded by
zakCopyright:
Available Formats
Review Article
Perioperative Pain Control in
Pediatric Patients Undergoing
Orthopaedic Surgery
Abstract
Philip D. Nowicki, MD
Kelly L. Vanderhave, MD
Kathleen Gibbons, MD
Bishr Haydar, MD
Mark Seeley, MD
Kenneth Kozlow, MD
Kiran Bhoopal, MD
Virginia T. Gauger, MD
Management of perioperative pain is critical in the pediatric patient
undergoing orthopaedic surgery. A variety of modalities can be
used to manage pain and optimize recovery and patient
satisfaction, including nonopioid and opioid analgesia; local
anesthetic injection; and regional analgesia such as intrathecal
morphine, epidural therapy, and peripheral nerve blocks. Acute
pain management can be tailored based on the needs of the
patient, the surgical site, and the anticipated level of postoperative
pain. A preoperative discussion of the plan for perioperative pain
control with the patient, his or her parents, and the anesthesiologist
can help manage expectations and maximize patient satisfaction.
From the Department of
Orthopaedic Surgery, Western
Michigan University School of
Medicine, Kalamazoo, MI
(Dr. Nowicki and Dr. Kozlow), the
Departments of Orthopaedic Surgery
and Anesthesia, University of
Michigan Health System, Ann Arbor,
MI (Dr. Vanderhave, Dr. Gibbons,
Dr. Haydar, Dr. Seeley, and
Dr. Gauger), and the Department of
Anesthesia, Advocate Christ Medical
Center, Oak Lawn, IL (Dr. Bhoopal).
None of the following authors or any
immediate family member has
received anything of value from or
has stock or stock options held in a
commercial company or institution
related directly or indirectly to the
subject of this article: Dr. Nowicki,
Dr. Vanderhave, Dr. Gibbons,
Dr. Haydar, Dr. Seeley, Dr. Kozlow,
Dr. Bhoopal, and Dr. Gauger.
J Am Acad Orthop Surg 2012;20:
755-765
http://dx.doi.org/10.5435/
JAAOS-20-12-755
Copyright 2012 by the American
Academy of Orthopaedic Surgeons.
December 2012, Vol 20, No 12
espite modern diagnostic and
evaluative tools, pain remains
difficult to measure objectively.
Acute pain refers to pain of short duration (hours to days) and is typically associated with trauma, illness,
or surgery. Of particular concern to
the surgeon is evidence that suggests
that pain activates neuroendocrine
responses, thus increasing tissue metabolism that may ultimately impair
healing. Inadequate analgesia may
have deleterious effects on postoperative pulmonary function and increase the risk of morbidity and mortality.1 Therefore, the surgeon should
discuss postoperative pain management plans with the child and his or
her parents prior to surgery to set
appropriate expectations. This discussion is critical because poor pain
control in the pediatric patient can
lead to significant stress, prolonged
hospital stay, and decreased patient
satisfaction.2-9
Postoperative pain control in pediatric patients has received much
needed attention in the recent literature. Most pediatric hospitals now
have a dedicated acute pain service
whose primary focus is to assist with
pain management.2,3 Various options
are available for management of pain
following pediatric orthopaedic surgery and can be tailored based on the
needs of the patient, the surgical site,
and the anticipated severity of postoperative pain.
General Considerations
and Contraindications
Pharmacokinetic differences between
children and adults are significant
and have implications for the dosage
and intervals of analgesic medication. Most analgesics are lipophilic
substances and require transformation into water-soluble substances to
enable the body to excrete them in
the form of urine or bile. The medications volume of distribution is directly affected by body composition.
Compared with adults, infants and
755
Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
neonates have a higher total body
water content and lower levels of
plasma binding proteins, which have
opposing effects on drug dosing.
Opioids and local anesthetics, which
are highly protein bound, will be
present in a higher concentration in
children than in adults, increasing
the risk of toxicity.
Hepatic metabolism of drugs varies
with the childs age. Generally, drug
clearance in the 2- to 6-year age
group is higher than in adults because of the higher ratio of hepatic
mass to body weight as well as
smaller fat and muscle stores. These
factors should be taken into account
when planning for perioperative pain
management in the pediatric patient.
Pain scales such as the visual analog scale and the Faces Pain Scale are
especially useful for monitoring pain
control in children; routine use of
these assessment tools with all methods of pain control is strongly recommended.10 Child life specialists
specialize in various methods of child
and family support during pediatric
hospitalization and are useful in distracting children preoperatively and
postoperatively, resulting in improved patient cooperation with procedures and improved pain and anxiety control.11
Contraindications for nonopioid
analgesia include organ failure (hepatic failure due to acetaminophen
[APAP], renal failure due to nonsteroidal anti-inflammatory drugs
[NSAIDs]), gastrointestinal bleeding
(NSAIDs), asthma (NSAIDs; however, they may be used in patients
with asthma if a test dose does not
cause symptoms), and any previous
allergic reaction to the drug. Contraindications for opioid analgesia
include significant hepatic, pulmonary, or renal dysfunction and a history of allergic reaction to the drug.
Local anesthetic is contraindicated in
patients with hypersensitivity to the
drug, infection at the planned injec-
756
tion site, and uncontrolled bleeding
disorder. Regional analgesia is contraindicated in patients with sepsis,
infection at the insertion site, anatomic abnormalities (eg, sacral agenesis, myelomeningocele), and coagulopathy.
Extremity surgery in patients at
risk for compartment syndrome is a
relative contraindication for regional
analgesia. Dunwoody et al12 described the development of compartment syndrome in two patients who
underwent surgery with a continuous infusion of bupivacaine and fentanyl via an epidural catheter. This
combination provided excellent postoperative analgesia but predisposed
patients to injury because they were
unable to feel excessive pressure in
the operative limb. The authors concluded that an increased risk of compartment syndrome exists following
epidural use and that clinical vigilance is necessary for prevention.
Nonopioid Analgesia
APAP is the only over-the-counter
nonanti-inflammatory
analgesic
commonly available in the United
States, and it is the most common
nonopioid analgesic used in pediatric
patients. The drug acts as a weak inhibitor of cyclooxygenase-1 and -2 in
peripheral tissues, which accounts
for its lack of anti-inflammatory effect and more profound analgesic
and antipyretic properties. APAP has
the same indications as intermediatedose aspirin but is used preferentially
in children because of the lower risk
of side effects, especially Reye syndrome. APAP can be administered
orally, intravenously, or rectally and
is safe for use even in infants.
Intravenous (IV) APAP has the potential to fill an unmet need in inpatient treatment of pain and fever, especially if the patient cannot take
oral medication. Findings from the
initial report by Sinatra et al13 as well
as the results of a more recent expanded analysis14 support the safety
and efficacy of IV APAP for management of moderate to severe pain following major orthopaedic surgery.
NSAIDs are a group of agents that
differ in their antipyretic, analgesic,
and anti-inflammatory properties.
Their primary mechanism of action
is inhibition of cyclooxygenase, resulting in decreased formation of
prostaglandins, which are a major
component of the inflammatory response. NSAIDs are associated with
a risk of gastrointestinal disturbance
and renal damage, especially in patients with preexisting renal disease.
These drugs can cause reversible
platelet dysfunction and may worsen
hemostasis or cause bleeding in patients with preexisting coagulopathy.
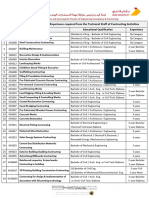
Guidelines for pediatric dosage of
several oral pain medications are
outlined in Table 1.
Ketorolac is a nonselective NSAID
that can be used for short-term (72
hours) management of pain; longer
administration is associated with
risks of gastrointestinal and renal
damage. The use of IV ketorolac in
pediatric orthopaedic surgery has increased dramatically over the past
decade. Studies have demonstrated
its efficacy and low risk of complications.15 In a placebo-controlled study
that compared the postoperative use
of IV ketorolac with morphine, patients in the ketorolac group were
discharged from the postanesthesia
care unit earlier than those in the
placebo group, and the incidence of
emesis was significantly lower in the
ketorolac group than in the morphine group.4 Eberson et al16 found
that administration of ketorolac and
opioid analgesia following long bone
osteotomies and complex foot procedures resulted in significantly shorter
hospital stays compared with administration of morphine alone. They
found that ketorolac reduced IV nar-
Journal of the American Academy of Orthopaedic Surgeons
Philip D. Nowicki, MD, et al
Table 1
Pediatric Dosage Guidelines for Commonly Used Oral Nonopioid Analgesics
Drug
Acetaminophen
Ibuprofen
Naproxen
Aspirind
Dose for
Patients <60
kg (mg/kg)
Dose for Patients
60 kg (mg)
1015
610
56b
1015b,d
6501,000
400600b
250375b
6501,000b
Interval (h)
Maximal Daily
Dose for Patients
<60 kg (mg/kg)
Maximal Daily
Dose for Patients
60 kg (mg)
4
6
12
4
100a
40b,c
24b,c
80b,c,d
4,000
2,400b
1,000b
3,600b
The maximal daily doses of acetaminophen for infants and neonates are a subject of current controversy. Provisional recommendations are
that daily dosing should not exceed 75 mg per kilogram per day for infants, 60 mg per kilogram per day for term neonates and preterm neonates of more than 32 weeks of postconceptional age, and 40 mg per kilogram per day for preterm neonates 28 to 32 weeks of postconceptional age. Fever, dehydration, hepatic disease, and lack of oral intake may all increase the risk of hepatoxicity.
b
Higher doses may be used in selected cases for treatment of rheumatologic conditions in children.
c
Dosage guidelines for neonates and infants have not been established.
d
Aspirin carries a risk of provoking Reye syndrome in infants and children. If other analgesics are available, aspirin should be restricted to
indications for which an antiplatelet or anti-inflammatory effect is required, rather than being used as a routine analgesic or antipyretic in neonates, infants, or children. Dosage guidelines for aspirin in neonates have not been established.
Reproduced with permission from Berde CB, Sethna NF: Analgesics for the treatment of pain in children. N Engl J Med 2002;347(14):10941103. http://www.massmed.org. Accessed October 19, 2012.
cotic requirements and decreased
narcotic-induced gastrointestinal distress with no increased bleeding risk.
Although the literature on multidose
use of ketorolac in infants is sparse,
ketorolac administration in infants
aged to 6 months should be minimal
if employed at all.17,18
Ketorolac has proved to be successful in controlling perioperative
pain associated with many types of
pediatric surgery, but its use in pediatric orthopaedic surgery has been
limited because of concern for potential detrimental effects on osseous
and soft-tissue healing. However,
Kay et al19 studied the use of ketorolac in 221 pediatric patients with
fractures treated surgically and
found no cases of delayed union,
malunion, and wound or bleeding
complications. The authors concluded that ketorolac was safe for
use with surgical fracture management and should be considered as an
adjunct for pain control in pediatric
patients.
Benzodiazepines can also be used
to assist with management of perioperative pain. These drugs are used to
control inflammation of the muscle,
which leads to spasm and pain. The
December 2012, Vol 20, No 12
most commonly used spasmolytic
medication in pediatric orthopaedics
is diazepam. Benzodiazepines act on
the central nervous system and skeletal muscle. These medications have
neither antipsychotic activity nor analgesic action and do not affect the
autonomic nervous system. Because
benzodiazepines lack analgesic properties, they should be used with
NSAIDs or opioids to provide adequate pain relief following orthopaedic procedures. Potential side effects
of spasmolytic medication include
impaired motor function, drug tolerance, and respiratory depression, especially when used in conjunction
with opioids. In the neuromuscular
patient, a combination of pain control therapies (eg, epidural analgesia,
opioids, benzodiazepines) is often
used to limit overmedication and
side effects.
Opioid Analgesia
Opioids are the most powerful drugs
available for pain relief, attenuating
both emotional and sensory aspects
of the pain experience. These drugs
act on receptors within the brain,
spinal cord, and peripheral tissues.
Administration via oral or IV routes
is most common, but opioids can
also be administered via the intrathecal (IT) or epidural spaces. In children, intramuscular injection of opioids is avoided because absorption is
unpredictable, and children dislike
injections. IV administration of opioids results in rapid onset of action
with a high level of efficacy for pain
relief. Table 2 lists several commonly
prescribed opioids as well as pediatric dosage guidelines.
Following orthopaedic surgery, the
amount of pain experienced by children with similar conditions varies
widely. Postoperative pain requirements fluctuate based on the activities being performed. In the perioperative period, a variety of options for
supplying opioid medication are
available. In adults and children
older than age 6 years, patientcontrolled analgesia (PCA) has been
shown to be an effective way to treat
varying levels of pain. PCA is safe,
effective, and highly satisfactory to
patients, families, and nursing staff.5
PCA by proxy (ie, nursing- and
parent-controlled analgesia) has been
shown to be safe and effective in
757
Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
Table 2
Guidelines for Pediatric Dosage of Oral and Intravenous Opioid Analgesicsa
Equianalgesic Dosesb
Typical Starting Intravenous or Subcutaneous
Doses and Intervals
Parenteral
Oral
Weight <50 kg
Weight 50 kg
Codeine
120 mg
200 mg
NR
NR
Morphine
10 mg
30 mg (long-term),
60 mg (single dose)
NA
10 mg
100 g (0.1 mg)
1520 mg
1020 mg
NA
1.52 mg
68 mg
75100 mg
300 mg
Drug
Oxycodone
Methadonec
Fentanyl
Hydromorphone
Meperidine (pethidine)d
Bolus: 0.1 mg/kg every
24 h
Infusion: 0.03 mg/kg/h
Bolus: 58 mg every 24 h
Infusion: 1.5 mg/h
NA
0.1 mg/kg every 48 h
Bolus: 0.51.0 g/kg every
12 h
Infusion: 0.52.0 g/kg/h
Bolus: 0.02 mg/kg every
24 h
Infusion: 0.006 mg/kg/h
Bolus: 0.81.0 mg/kg every
23 h
NA
58 mg every 48 h
Bolus: 2550 g every 12 h
Infusion: 25100 g/h
Bolus: 1 mg every 24 h
Infusion: 0.3 mg/h
Bolus: 5075 mg every
23 h
NA = not applicable, NR = not recommended
a
Doses are for patients over 6 months of age. In infants under 6 months, initial per-kilogram doses should begin at roughly 25% of the perkilogram doses recommended here. Higher doses are often required for patients receiving mechanical ventilation. All doses are approximate
and should be adjusted according to clinical circumstances. Recommendations are adapted from previous summary tables, including those of
a consensus statement from the World Health Organization and the International Association for the Study of Pain.
b
Equianalgesic doses refer to proportional drug doses when switching from intravenous to oral medication forms.
c
Methadone requires additional vigilance because it can accumulate and produce delayed sedation. If sedation occurs, doses should be withheld unitl sedation resolves. Thereafter, doses should be substantially reduced, the interval between doses should be extended to 8 to 12
hours, or both.
d
The use of meperidine should generally be avoided if other opioids are available, especially with long-term use, because its metabolite can
cause seizures.
Reproduced with permission from Berde CB, Sethna NF: Analgesics for the treatment of pain in children. N Engl J Med 2002;347(14):10941103. http://www.massmed.org. Accessed October 19, 2012.
children younger than age 6 years
and in cognitively impaired children.6 Its efficacy is due to maintenance of opioid concentrations
within a narrower range than that of
intermittent injections, with lower
peak and higher trough levels.
Continuous IV opioid infusion can
be used in patients in whom PCA
is contraindicated because of age,
physical disability, or cognitive impairment. The advantage of continuous infusion over intermittent opioid
administration is the attainment of
stable plasma opioid levels without
wide fluctuations. However, constant
infusion will not cover breakthrough
incident pain; therefore, rescue doses
of opioid are still needed. Continu-
758
ous infusion of an opioid must be
carefully monitored because respiratory depression can occur with excessive drug accumulation. The infusion rate should be reduced in
children at risk of central nervous
system depression or respiratory depression.
Local Anesthetic Injection
Local anesthetics have been shown
to be effective for management of
postoperative pain by temporarily
blocking conduction of the pain signal along nerve fibers. Herrera et al20
examined the efficacy of hematoma
block in pediatric patients with iso-
lated femoral fractures treated with
flexible elastic intramedullary nailing. Thirteen patients (37%) received
a hematoma block with 0.5% bupivacaine at the end of the procedure;
22 patients (63%) with similar fractures did not receive a block. The authors found that 36% of patients in
the control group versus 8% in the
block group required opioid administration within the first 2 hours
postoperatively. The authors concluded that hematoma block is a safe
and effective adjunct for pain control
following elastic intramedullary nailing for femoral fractures. In a
double-blind randomized control
trial of 40 pediatric patients who underwent extremity surgery, Bulut
Journal of the American Academy of Orthopaedic Surgeons
Philip D. Nowicki, MD, et al
Table 2 (continued)
Guidelines for Pediatric Dosage of Oral and Intravenous Opioid Analgesicsa
Typical Starting Oral Doses and Intervals
Parenteral:Oral Dose Ratio
Weight 50 kg
Weight <50 kg
1:2
0.51.0 mg/kg every 34 h
3060 mg every 34 h
1:3 (long-term)
1:6 (single dose)
Immediate release: 1520 mg every 34 h
Sustained release: 3045 mg every 812 h
NA
1:2
NA
Immediate release: 0.3 mg/kg every 34 h
Sustained release: 2035 kg: 1015 mg every
812 h
3550 kg: 1530 mg every 812 h
0.10.2 mg/kg every 34 h
0.10.2 mg/kg every 48 h
NA
1:4
0.040.08 mg/kg every 34 h
24 mg every 34 h
1:4
23 mg/kg every 34 h
100150 mg every 34 h
510 mg every 34 h
510 mg every 48 h
NA
NA = not applicable, NR = not recommended
a
Doses are for patients over 6 months of age. In infants under 6 months, initial per-kilogram doses should begin at roughly 25% of the perkilogram doses recommended here. Higher doses are often required for patients receiving mechanical ventilation. All doses are approximate
and should be adjusted according to clinical circumstances. Recommendations are adapted from previous summary tables, including those of
a consensus statement from the World Health Organization and the International Association for the Study of Pain.
b
Equianalgesic doses refer to proportional drug doses when switching from intravenous to oral medication forms.
c
Methadone requires additional vigilance because it can accumulate and produce delayed sedation. If sedation occurs, doses should be withheld unitl sedation resolves. Thereafter, doses should be substantially reduced, the interval between doses should be extended to 8 to 12
hours, or both.
d
The use of meperidine should generally be avoided if other opioids are available, especially with long-term use, because its metabolite can
cause seizures.
Reproduced with permission from Berde CB, Sethna NF: Analgesics for the treatment of pain in children. N Engl J Med 2002;347(14):10941103. http://www.massmed.org. Accessed October 19, 2012.
et al21 compared 20 patients who received 0.5% bupivacaine via subfascial catheters postoperatively with
20 who received normal saline. Initially, no difference was found between the groups in terms of pain
scores, but a substantial decrease in
postoperative pain was reported in
the local anesthetic group at hours 4
to 48. The authors reported few
complications in both groups and
concluded that catheter administration of local anesthetic was effective
and prolonged postoperative analgesia.
Preoperative or intraoperative injection of botulinum toxin A into selected muscle groups can aid in preDecember 2012, Vol 20, No 12
venting postoperative spasms in
neuromuscular patients. Use of this
injection has been shown to be beneficial in patients undergoing adductor release.22
Regional Analgesia
Regional anesthesia offers several
benefits for pain control following
pediatric orthopaedic surgery, including decreased need for opioid
medications, earlier return of postoperative gastrointestinal function, and
attenuation of the stress response
caused by surgical procedures.23 Several cohort series have confirmed
that regional anesthesia is safe for
use in children. A prospective 1-year
study of more than 24,000 anesthetics (including regional blocks) reported that the overall incidence of
complications associated with regional blocks was 0.9 in 1,000
blocks.7 In most cases, these complications involved either failure to
place an effective block or failure of
the block to provide adequate analgesia postoperatively. More serious
complications, such as peripheral
nerve injury and local anesthetic toxicity, were rare.24 Placing these blocks
in deeply sedated or anesthetized patients, as is often necessary in pediatric patients, was found to be safe.7
759
Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
Intrathecal Morphine
Injection
Injection of preservative-free morphine into the IT space can provide
up to 24 hours of pain control following extremity surgery.25 Spinal injections can be performed following
the induction of general anesthesia
and before the surgical incision is
made. Alternatively, morphine can
be injected directly into the dura in
patients undergoing spinal fusion.26,27
As with IV morphine, side effects
associated with IT morphine injection include nausea, pruritus, and
urinary retention. However, the most
concerning side effect is respiratory
depression, which can occur up to 24
hours after injection. Therefore, respiratory monitoring (continuous
pulse oximetry) and limited use of
other respiratory depressants are recommended following this technique.
A recent study evaluated the use of
low-dose IT morphine following a
variety of surgical procedures in 187
children and found that 81% of patients did not require opioid rescue
medication in the first 8 hours postoperatively and that 37% of patients
had sustained pain relief 24 hours after the spinal injection.28 Thus, IT
morphine is ideally suited for patients who are expected to transition
to oral analgesics shortly after surgery.
Epidural Therapy
Injecting local anesthetics and/or
opioids into the epidural space can
provide effective analgesia for thoracic, pelvic, and lower extremity
surgery. Advantages of epidural therapy include decreased intraoperative
blood loss, prolonged pain control,
and minimal sedation required postoperatively. Side effects associated
with epidural injections include pruritus, urinary retention, and nausea.29 Additionally, depending on the
concentration of local anesthetic
760
used, varying degrees of motor block
can occur with epidural infusions.
A single injection into the epidural
space via the sacral hiatus, commonly known as a caudal injection,
may provide several hours of postoperative analgesia for pelvic and lower
extremity surgery and is a useful
technique for outpatient procedures.
For patients who are scheduled to be
admitted, epidural catheters can be
placed into the lumbar or thoracic
regions for continuous administration of local anesthetics and/or opioids. These catheters can be maintained for several days, and the
concentration and volume of the infusion can be altered to optimize
pain control.
Peripheral Nerve Block
This technique involves placement of
local anesthetic near a peripheral
nerve to block conduction of the
pain signal to the central nervous
system. A successful peripheral nerve
block requires minimal amounts of
anesthesia and opioid and provides
excellent postoperative pain control.
Nerve blocks can be performed as a
single injection, or catheters can be
placed in proximity to relevant
nerves to provide prolonged pain relief following surgery.
Ultrasonography can be used to
aid in the placement of peripheral
nerve blocks and, as a result, the use
of these blocks has expanded in recent years. Real-time imaging of the
relevant nerve and vascular structures facilitates precise needle placement such that smaller amounts of
local anesthetic can be used, thereby
limiting the risk of local anesthetic
toxicity.30
Implementation of various approaches to the brachial and to the
lumbar and sciatic plexuses can effectively anesthetize the nerves of
the upper and lower extremities, respectively, providing excellent post-
operative analgesia. Additionally, the
complication rate associated with peripheral nerve blocks has been
shown to be small. DeVera et al31 retrospectively reviewed 1,657 nerve
blocks placed in patients (age range,
2 months to 20 years) over a 5-year
period following induction of general anesthesia. In this large series,
only two self-limiting nerve injuries
were reported. The ability to target
the specific innervation of the surgical site using a minimal amount of
local anesthesia to avoid the side
effects of systemic opioids makes peripheral nerve block an integral technique for providing effective analgesia for orthopaedic procedures.
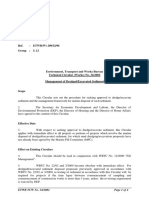
Pain Control Following
Spine Surgery
A growing body of literature regarding
pain control following spine surgery
has evolved over the past 10 years (Table 3). Traditional treatment regimens
include APAP, NSAIDs, and PCA or
nurse-controlled IV analgesia with opioids and benzodiazepines to treat muscle spasms. Recent studies have examined the role of regional analgesia in
the context of perioperative control of
pain associated with spine surgery. Applicable techniques include IT injection
of opioids or continuous epidural analgesia (CEA) and patient-controlled
epidural analgesia with local anesthetics, opioids, or both.
We have addressed the use of
APAP and NSAIDS in pediatric orthopaedic surgery; however, the use
of ketorolac in spinal surgery must
be discussed specifically. NSAID use
following spinal fusion has been discouraged in the adult population due
to concerns regarding postoperative
bleeding and pseudarthrosis.15 Multiple studies have demonstrated the efficacy and low risk of complications
associated with IV ketorolac following pediatric spine fusion.15,33 In one
Journal of the American Academy of Orthopaedic Surgeons
Philip D. Nowicki, MD, et al
Table 3
Regimens for Pain Control Following Pediatric Spine Surgery
Study
Route
Medication/Dosage
Dadure et al32
IV
Munro et al33
IV
Ketoprofene 2 mg/kg IV every 12 h and paracetamol 15 mg/kg IV/PO
every 6 h
Ketorolac 0.5 mg/kg every 6 h for 36 h w/morphine PCA (maximum
ketorolac dose 15 mg for weight <50 kg)
0.25% bupivacaine 0.51 mL/kg, clonidine 1 g/kg, epinephrine
1:200,000 if >6 months of age (single injection)
1% lidocaine 0.51 mL/kg bolus, then 0.10.2 mL/kg/h (continuous
injection)
Morphine 5 g/kg followed by morphine PCA
Morphine 919 g/kg followed by continuous IV morphine infusion
0.0050.06 mg/kg/h
Morphine 919 g/kg
Morphine 45 g/kg
Hydromorphone 20 g/mL and 0.1% bupivacaine at 0.10.2 mL/kg/h
Hydromorphone/fentanyl/morphine and 0.0625 to 0.125% bupivacaine at 28 mL/h
Fentanyl 1 g/mL and 0.4% lidocaine at 0.10.35 mL/kg/h
0.1% bupivacaine and hydromorphone 10 g/mL at 8 mL/h
0.0625% to 0.125% bupivacaine with morphine 510 g/kg at 410
mL/h
0.1% ropivacaine and hydromorphone 10 g/mL at 0.2 mL/kg/h
0.2% ropivacaine 1.6 mL/h with 2 mL every 10 min (patientcontrolled epidural)
Khoury et al34
Peripheral nerve block
Dadure et al35
Peripheral nerve block
Gall et al26
Poe-Kochert et al36
Intrathecal
Intrathecal
Tripi et al37
Ganesh et al28
Sucato et al38
Shaw et al29
Intrathecal
Intrathecal
Epidural
Epidural
Reinoso-Barbero et al39
Gauger et al40
Arms et al2
Epidural
Epidural
Epidural
Lowry et al41
Antok et al42
Epidural
Epidural
IV = intravenous, PCA = patient-controlled analgesia, PO = oral
study, 35 patients received a bolus of
either ketorolac or saline at the end
of their spinal fusion and then every
6 hours for 36 hours.33 Patients in
the ketorolac group consistently
rated their pain lower than did those
in the placebo group up to the afternoon of the second postoperative
day. Fourteen patients were followed
for a minimum of 2 years and no
pseudarthrosis was found in either
group. Sucato et al15 compared 158
patients who received ketorolac following posterior spinal fusion and
instrumentation for adolescent idiopathic scoliosis with 161 patients
who did not receive ketorolac and
found no difference between the two
groups in terms of the rate of pseudarthrosis (1.9% versus 3.1%) as well
as no increased risk of other surgical
complications. Despite these supportive studies, there continues to be
December 2012, Vol 20, No 12
a reluctance to use ketorolac in this
patient population. Hayes et al43 surveyed a group of international anesthesiologists regarding the use of
NSAIDs in pediatric patients following spine fusion and found that there
continues to be a wide discrepancy in
the use of these drugs in this population despite the fact that postoperative NSAIDs can reduce morbidity
associated with opioid consumption,
specifically respiratory depression.
In 1988, Dalens and Tanguy44 published their results of the use of IT
morphine in 20 pediatric patients
who underwent spinal fusion. The
authors found that IT morphine (25
g/kg) administered at the lumbar
level before the start of the surgical
procedure was safe and provided 36
hours of analgesia. Although IT morphine has been found to be beneficial, current protocols vary regarding
time of administration (beginning or
end of surgical procedure), dosage (2
to 25 g/kg), additives, volume of injectant, outcome variables measured,
and documented side-effect profile.
Despite the benefits associated
with IT morphine (eg, reduced intraoperative blood loss, decreased pain
scores 24 hours postoperatively), its
use is hindered by the side-effect profile. The hydrophilic nature of this
opioid allows cephalad migration
within the cerebrospinal fluid, where
morphine can act upon the brain
stem, resulting in respiratory depression, pruritus, nausea, and vomiting.45 Because the incidence of these
side effects is thought to be dosedependent, current studies are designed to determine the optimal dosing regimen. Eschertzhuber et al46
compared the effects of low- and
high-dose IT morphine (5 g/kg and
761
Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
15 g/kg, respectively) combined
with a fixed dose of sufentanil with
those of the control group. The lowdose regimen provided an excellent
blood-sparing effect and sufficient
postoperative analgesia, with a sideeffect profile comparable to that of
the control group. The high-dose
regimen showed no statistical advantages over the low-dose regimen.
Similarly, Tripi et al37 compared the
use of IT morphine in three groups
(no dose, moderate dose [9 to
19 g/kg], high dose [20 g/kg]) of
patients undergoing posterior spinal
fusion for idiopathic scoliosis. The
authors found that higher doses of
morphine did not result in significantly better analgesia compared
with moderate doses and that higher
doses were associated with greater
frequency of respiratory depression.
Given the side-effect profile and
limited duration of analgesia provided by a single injection of IT morphine, some orthopaedic surgeons
may prefer the use of epidurals in pediatric patients. Behar et al47 first reported the efficacy of epidural morphine in patients with severe acute or
chronic pain; however, Amaranath
et al48 were the first to report its successful use in pediatric spine surgery.
In patients who receive epidural analgesia, the catheter is inserted under
direct visualization at the end of the
surgical procedure.29 For single catheter techniques, the catheter is placed
at the middle of the incision. For
dual catheter techniques, one catheter is placed in the proximal incision
and the other is placed in the distal
incision.49 Following a thorough neurologic examination, the catheters
are then typically dosed with a combination of local anesthetic (eg, ropivacaine, bupivacaine) and narcotic
(eg, fentanyl, morphine, hydromorphone).
In the only randomized, doubleblind study of epidural analgesia administered following pediatric spinal
762
fusion, OHara et al50 compared the
use of IV morphine with that of epidural bupivacaine plus fentanyl in
patients with idiopathic scoliosis and
found no difference in analgesic effectiveness. However, in the largest
study to date, Sucato et al38 evaluated 613 patients who received either
CEA or PCA following spine fusion
and found that average and overall
pain scores in the first 48 hours were
significantly lower in the CEA group.
In addition to epidural safety and
efficacy, other postoperative parameters have been evaluated. Van
Boerum et al51 compared epidural infusion with PCA and found pain
control to be comparable; however,
patients in the epidural group tolerated full diet earlier and were discharged an average of 0.5 days
sooner than those in the PCA group.
Cassady et al52 found that the safety
and efficacy of CEA were comparable to that of PCA, with a more
rapid return of bowel sounds in patients treated with CEA.
Concerns regarding the adequacy
of epidural analgesia in this patient
population center on catheter placement and leakage of the solution
from the epidural space. Turner
et al53 studied epidural catheter
placement in 14 patients who underwent spinal fusion. The authors injected an omnipaque contrast agent
into the catheter before obtaining a
postoperative radiograph of the
chest. Contrast medium was visualized in the spinal canal in seven patients who reported satisfactory analgesia; however, no contrast was seen
within the spinal canal or paravertebral gutter space in five (36%) who
had inadequate analgesia. Lavelle
et al54 evaluated pain control with
epidural analgesia in patients who
had spine procedures that violated
the epidural space. The authors compared 29 patients who received epidurals with 26 patients who received
PCA following Smith-Petersen os-
teotomies and instrumentation using
multiple sublaminar wires. The authors found that epidural analgesia
resulted in lower pain scores during
the first 24 hours postoperatively.
Counterintuitively, patients with violated canals had lower pain scores
than those with an intact epidural
space.
To date, only one study has compared the three most common methods of postoperative pain control in
pediatric patients treated with posterior spinal fusion. Milbrandt et al55
compared the efficacy and side-effect
profile of PCA alone (41 patients),
IT morphine injection with PCA (42
patients), and epidural catheter infusion (55 patients) for pain control
following posterior spinal fusion and
segmental spinal instrumentation for
adolescent idiopathic scoliosis. Although IT morphine with PCA provided better immediate pain control
than did the other modalities, patients who received epidural catheter
infusion had the lowest pain scores
for the longest period of time, with
faster return to solid foods and significantly less vomiting, but more
pruritus.
Complications
Postoperative pain control modalities have a wide range of adverse effects. The most common side effects
of opioid analgesia include itching,
nausea, and sedation. Pruritus can be
irritating and can prevent adequate
patient comfort. The incidence of
pruritus associated with the use of
peripheral nerve blocks has been
found to be low (0.9% to 8%)32,35
and is higher with morphine PCA
(11% to 17%).38,55 Following IT
morphine or epidural injection, the
incidence of pruritus has been reported to be as high as 37%28 and
49%,55 respectively.
Postoperative nausea and vomiting
Journal of the American Academy of Orthopaedic Surgeons
Philip D. Nowicki, MD, et al
(PONV) causes discomfort in the recovery period and prevents appropriate oral intake. PONV is dependent
on both the type of anesthetic and
the postoperative pain regimen. In a
large retrospective study, 13% of patients treated with continuous IV
morphine infusion had PONV,36
whereas up to 54% of patients
treated with CEA in a separate study
had nausea.38 In a prospective study
of 60 children who received regional
and general anesthesia for orthopaedic surgery, the risk for PONV dramatically diminished (6.7%) with
the use of regional analgesia.34
Respiratory depression is a dangerous and potentially fatal complication in the postoperative period that
is often dependent on postoperative
opioid use and the route of administration. Multiple studies have demonstrated a decreased risk of respiratory depression with the use of IT
morphine, especially when given in
low doses.28,37,55 This risk is transient
and typically subsides without the
need for reintubation.55 Moreover, it
has been suggested that patients
treated with IT morphine postoperatively can be safely monitored on
regular surgical hospital floors.5 The
use of epidural opioids also may
cause respiratory depression.39 One
study reported that the risk of respiratory depression associated with
epidural analgesia with opioids was
as high as 58%;38 other studies demonstrated no significant difference in
the risk of respiratory depression associated with epidural analgesia and
PCA.40
Neurologic deficit following spinal
fusion can be either transient or permanent and is a major concern. Postoperative pain modalities that can
mask this dangerous morbidity
should be avoided.38 To avoid motor
block, some authors have advocated
against the use of local anesthetic in
the epidural solution and have
switched from bupivacaine to ropiDecember 2012, Vol 20, No 12
vacaine due to the decreased incidence of motor block associated with
the latter.3,42 Several studies have proposed that following spinal fusion,
an epidural bolus should not be
given until the postoperative neurologic examination has been documented.9,38,40,41,54,55
1.
Haller G, Laroche T, Clergue F:
Morbidity in anaesthesia: Today and
tomorrow. Best Pract Res Clin
Anaesthesiol 2011;25(2):123-132.
2.
Arms DM, Smith JT, Osteyee J, Gartrell
A: Postoperative epidural analgesia for
pediatric spine surgery. Orthopedics
1998;21(5):539-544.
3.
Lnnqvist PA, Morton NS: Postoperative
analgesia in infants and children. Br J
Anaesth 2005;95(1):59-68.
4.
Watcha MF, Jones MB, Lagueruela RG,
Schweiger C, White PF: Comparison of
ketorolac and morphine as adjuvants
during pediatric surgery. Anesthesiology
1992;76(3):368-372.
5.
Berde CB, Lehn BM, Yee JD, Sethna NF,
Russo D: Patient-controlled analgesia in
children and adolescents: A randomized,
prospective comparison with
intramuscular administration of
morphine for postoperative analgesia.
J Pediatr 1991;118(3):460-466.
6.
Monitto CL, Greenberg RS, Kost-Byerly
S, et al: The safety and efficacy of
parent-/nurse-controlled analgesia in
patients less than six years of age. Anesth
Analg 2000;91(3):573-579.
7.
Giaufr E, Dalens B, Gombert A:
Epidemiology and morbidity of regional
anesthesia in children: A one-year
prospective survey of the FrenchLanguage Society of Pediatric
Anesthesiologists. Anesth Analg 1996;
83(5):904-912.
8.
Taenzer AH, Clark C: Efficacy of
postoperative epidural analgesia in
adolescent scoliosis surgery: A metaanalysis. Paediatr Anaesth 2010;20(2):
135-143.
9.
Tobias JD: A review of intrathecal and
epidural analgesia after spinal surgery in
children. Anesth Analg 2004;98(4):956965.
10.
von Baeyer CL: Childrens self-reports of
pain intensity: Scale selection, limitations
and interpretation. Pain Res Manag
2006;11(3):157-162.
11.
Brewer S, Gleditsch SL, Syblik D,
Tietjens ME, Vacik HW: Pediatric
anxiety: Child life intervention in day
surgery. J Pediatr Nurs 2006;21(1):1322.
12.
Dunwoody JM, Reichert CC, Brown KL:
Compartment syndrome associated with
bupivacaine and fentanyl epidural
analgesia in pediatric orthopaedics.
J Pediatr Orthop 1997;17(3):285-288.
13.
Sinatra RS, Jahr JS, Reynolds LW,
Viscusi ER, Groudine SB, PayenChampenois C: Efficacy and safety of
single and repeated administration of 1
gram intravenous acetaminophen
injection (paracetamol) for pain
management after major orthopedic
Summary
A variety of safe and effective options are available for management
of perioperative pain following pediatric orthopaedic surgery. Regional
analgesia such as peripheral nerve
blocks and epidural analgesia can
provide excellent pain control with
low risk of complications and few
side effects. Following pediatric orthopaedic surgery, IV ketorolac is an
excellent adjunct for pain control
that is associated with low morbidity. The plan for management of
perioperative pain in the pediatric orthopaedic patient is best orchestrated
in the preoperative period. Discussion among the patient, caregivers,
anesthesiologist, and surgeon is critical to set expectations and maximize
patient satisfaction.
References
Evidence-Based Medicine: Levels of
evidence are described in the table of
contents. In this article, references 5,
11, 13, 14, 21, 26, 40, 46, 52 and
are level I studies. References 4, 7, 8,
23, 27, 30, 33, 34, 40, 41, 44, 47,
49, and 50 are level II studies. References 6, 15, 16, 18-20, 29, 31, 32,
35, 38, 48, 51, 54, and 55 are level
III studies. References 2, 3, 9, 28, 34,
42, 45, and 53 are level IV studies.
References 1, 10, 17, 22, 24, 25, and
43 are level V expert opinion.
References printed in bold type are
those published within the past 5
years.
763
Perioperative Pain Control in Pediatric Patients Undergoing Orthopaedic Surgery
surgery. Anesthesiology 2005;102(4):
822-831.
14.
Sinatra RS, Jahr JS, Reynolds LW, et al:
Intravenous acetaminophen for pain
after major orthopedic surgery: An
expanded analysis. Pain Pract 2012;
12(5):357-365.
26.
Gall O, Aubineau JV, Bernire J, Desjeux
L, Murat I: Analgesic effect of low-dose
intrathecal morphine after spinal fusion
in children. Anesthesiology 2001;94(3):
447-452.
15.
Sucato DJ, Lovejoy JF, Agrawal S,
Elerson E, Nelson T, McClung A:
Postoperative ketorolac does not
predispose to pseudoarthrosis following
posterior spinal fusion and
instrumentation for adolescent idiopathic
scoliosis. Spine (Phila Pa 1976) 2008;
33(10):1119-1124.
27.
Goodarzi M: The advantages of
intrathecal opioids for spinal fusion in
children. Paediatr Anaesth 1998;8(2):
131-134.
28.
Ganesh A, Kim A, Casale P, Cucchiaro
G: Low-dose intrathecal morphine for
postoperative analgesia in children.
Anesth Analg 2007;104(2):271-276.
16.
Eberson CP, Pacicca DM, Ehrlich MG:
The role of ketorolac in decreasing
length of stay and narcotic complications
in the postoperative pediatric
orthopaedic patient. J Pediatr Orthop
1999;19(5):688-692.
17.
American Academy of Pediatrics
Committee on Fetus and Newborn;
American Academy of Pediatrics Section
on Surgery; Canadian Paediatric Society
Fetus and Newborn Committee; Batton
DG, Barrington KJ, Wallman C:
Prevention and management of pain in
the neonate: An update. Pediatrics 2006;
118(5):2231-2241.
18.
19.
20.
21.
Aldrink JH, Ma M, Wang W, Caniano
DA, Wispe J, Puthoff T: Safety of
ketorolac in surgical neonates and
infants 0 to 3 months old. J Pediatr Surg
2011;46(6):1081-1085.
Bulut T, Yilmazlar A, Yavascaoglu B,
Sarisozen B: The effect of local
anaesthetic on post-operative pain with
wound instillation via a catheter for
paediatric orthopaedic extremity surgery.
J Child Orthop 2011;5(3):179-185.
22.
Nolan J, Chalkiadis GA, Low J, Olesch
CA, Brown TC: Anaesthesia and pain
management in cerebral palsy.
Anaesthesia 2000;55(1):32-41.
23.
Rubin K, Sullivan D, Sadhasivam S: Are
peripheral and neuraxial blocks with
ultrasound guidance more effective and
safe in children? Paediatr Anaesth 2009;
19(2):92-96.
24.
25.
764
Sucato DJ, Duey-Holtz A, Elerson E,
Safavi F: Postoperative analgesia
following surgical correction for
adolescent idiopathic scoliosis: A
comparison of continuous epidural
analgesia and patient-controlled
analgesia. Spine (Phila Pa 1976) 2005;
30(2):211-217.
39.
Reinoso-Barbero F, Saavedra B, Hervilla
S, de Vicente J, Tabars B, GmezCriado MS: Lidocaine with fentanyl,
compared to morphine, marginally
improves postoperative epidural
analgesia in children. Can J Anaesth
2002;49(1):67-71.
40.
Gauger VT, Voepel-Lewis TD, Burke
CN, et al: Epidural analgesia compared
with intravenous analgesia after pediatric
posterior spinal fusion. J Pediatr Orthop
2009;29(6):588-593.
41.
DeVera HV, Furukawa KT, Matson
MD, Scavone JA, James MA: Regional
techniques as an adjunct to general
anesthesia for pediatric extremity and
spine surgery. J Pediatr Orthop 2006;
26(6):801-804.
Lowry KJ, Tobias J, Kittle D, Burd T,
Gaines RW: Postoperative pain control
using epidural catheters after anterior
spinal fusion for adolescent scoliosis.
Spine (Phila Pa 1976) 2001;26(11):
1290-1293.
42.
Dadure C, Pirat P, Raux O, et al:
Perioperative continuous peripheral
nerve blocks with disposable infusion
pumps in children: A prospective
descriptive study. Anesth Analg 2003;
97(3):687-690.
Antok E, Bordet F, Duflo F, et al:
Patient-controlled epidural analgesia
versus continuous epidural infusion with
ropivacaine for postoperative analgesia
in children. Anesth Analg 2003;97(6):
1608-1611.
43.
Hayes J, Pehora C, Bissonnette B: The
use of NSAIDs in pediatric scoliosis
surgery: A survey of physicians
prescribing practice. Paediatr Anaesth
2009;19(8):756-763.
44.
Dalens B, Tanguy A: Intrathecal
morphine for spinal fusion in children.
Spine (Phila Pa 1976) 1988;13(5):494498.
45.
Rathmell JP, Lair TR, Nauman B: The
role of intrathecal drugs in the treatment
of acute pain. Anesth Analg 2005;101(5
suppl):S30-S43.
Shaw BA, Watson TC, Merzel DI,
Gerardi JA, Birek A: The safety of
continuous epidural infusion for
postoperative analgesia in pediatric spine
surgery. J Pediatr Orthop 1996;16(3):
374-377.
30.
Tsui BC, Pillay JJ: Evidence-based
medicine: Assessment of ultrasound
imaging for regional anesthesia in
infants, children, and adolescents. Reg
Anesth Pain Med 2010;35(2 suppl):S47S54.
31.
32.
33.
34.
Munro HM, Walton SR, Malviya S,
et al: Low-dose ketorolac improves
analgesia and reduces morphine
requirements following posterior spinal
fusion in adolescents. Can J Anaesth
2002;49(5):461-466.
Khoury CE, Dagher C, Ghanem I,
Naccache N, Jawish D, Yazbeck P:
Combined regional and general
anesthesia for ambulatory peripheral
orthopedic surgery in children. J Pediatr
Orthop B 2009;18(1):37-45.
35.
Dadure C, Bringuier S, Raux O, et al:
Continuous peripheral nerve blocks for
postoperative analgesia in children:
Feasibility and side effects in a cohort
study of 339 catheters. Can J Anaesth
2009;56(11):843-850.
46.
Eschertzhuber S, Hohlrieder M, Keller C,
Oswald E, Kuehbacher G, Innerhofer P:
Comparison of high- and low-dose
intrathecal morphine for spinal fusion in
children. Br J Anaesth 2008;100(4):538543.
36.
Poe-Kochert C, Tripi PA, Potzman J,
Son-Hing JP, Thompson GH:
Continuous intravenous morphine
infusion for postoperative analgesia
following posterior spinal fusion for
idiopathic scoliosis. Spine (Phila Pa
1976) 2010;35(7):754-757.
47.
Behar M, Magora F, Olshwang D,
Davidson JT: Epidural morphine in
treatment of pain. Lancet 1979;1(8115):
527-529.
48.
Amaranath L, Andrish JT, Gurd AR,
Weiker GG, Yoon H: Efficacy of
intermittent epidural morphine following
posterior spinal fusion in children and
Dalens B: Regional Anesthesia in Infants,
Children and Adolescents. London,
United Kingdom, Williams & Wilkins
Waverly Europe, 1995.
Cot CJ Lerman J, Todres IDA Practice
38.
29.
Kay RM, Directo MP, Leathers M,
Myung K, Skaggs DL: Complications of
ketorolac use in children undergoing
operative fracture care. J Pediatr Orthop
2010;30(7):655-658.
Herrera JA, Wall EJ, Foad SL:
Hematoma block reduces narcotic pain
medication after femoral elastic nailing
in children. J Pediatr Orthop 2004;
24(3):254-256.
Son-Hing JP, Thompson GH: Intrathecal
morphine for postoperative analgesia in
patients with idiopathic scoliosis undergoing posterior spinal fusion. Spine
(Phila Pa 1976) 2008;33(20):22482251.
of Anesthesia for Infants and Children.
Philadelphia, PA, Saunders, 2009.
37.
Tripi PA, Poe-Kochert C, Potzman J,
Journal of the American Academy of Orthopaedic Surgeons
Philip D. Nowicki, MD, et al
adolescents. Clin Orthop Relat Res
1989;(249):223-226.
49.
Tobias JD, Gaines RW, Lowry KJ, Kittle
D, Bildner C: A dual epidural catheter
technique to provide analgesia following
posterior spinal fusion for scoliosis in
children and adolescents. Paediatr
Anaesth 2001;11(2):199-203.
50.
OHara JF Jr, Cywinski JB, Tetzlaff JE,
Xu M, Gurd AR, Andrish JT: The effect
of epidural vs intravenous analgesia for
posterior spinal fusion surgery. Paediatr
Anaesth 2004;14(12):1009-1015.
51.
Van Boerum DH, Smith JT, Curtin MJ:
A comparison of the effects of patient-
December 2012, Vol 20, No 12
controlled analgesia with intravenous
opioids versus Epidural analgesia on
recovery after surgery for idiopathic
scoliosis. Spine (Phila Pa 1976) 2000;
25(18):2355-2357.
52.
53.
Cassady JF Jr, Lederhaas G, Cancel DD,
Cummings RJ, Loveless EA: A
randomized comparison of the effects of
continuous thoracic epidural analgesia
and intravenous patient-controlled
analgesia after posterior spinal fusion in
adolescents. Reg Anesth Pain Med 2000;
25(3):246-253.
Turner A, Lee J, Mitchell R, Berman J,
Edge G, Fennelly M: The efficacy of
surgically placed epidural catheters for
analgesia after posterior spinal surgery.
Anaesthesia 2000;55(4):370-373.
54.
Lavelle ED, Lavelle WF, Goodwin R,
et al: Epidural analgesia for
postoperative pain control after
adolescent spinal fusion procedures
which violated the epidural space.
J Spinal Disord Tech 2010;23(5):347350.
55.
Milbrandt TA, Singhal M, Minter C,
et al: A comparison of three methods of
pain control for posterior spinal fusions
in adolescent idiopathic scoliosis. Spine
(Phila Pa 1976) 2009;34(14):14991503.
765
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- eMRCS - GI ParasitologyDocument3 pageseMRCS - GI ParasitologyzakNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Operating Theatre Design: Department of Medical HistoryDocument4 pagesOperating Theatre Design: Department of Medical HistoryzakNo ratings yet
- Miklós Szendrői Franklin H. Sim (Eds.) Color Atlas of Clinical OrthopedicsDocument9 pagesMiklós Szendrői Franklin H. Sim (Eds.) Color Atlas of Clinical OrthopedicszakNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Tello+User+Manual+v1.0 EN 2.12Document22 pagesTello+User+Manual+v1.0 EN 2.12Dhafin Aufa SajidNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- ACCOLADE II SurgicalDocument11 pagesACCOLADE II Surgicaltrinh thanhNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Ranson Criteria PDFDocument1 pageRanson Criteria PDFzakNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Results of Traction Injuries of CPNDocument5 pagesThe Results of Traction Injuries of CPNzakNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Surgical Release of Iliopsoas Tendon For Groin Pain After Total Hip ArthroplastyDocument3 pagesSurgical Release of Iliopsoas Tendon For Groin Pain After Total Hip ArthroplastyzakNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Psychometric Success Spatial Ability - Practice Test 1 PDFDocument12 pagesPsychometric Success Spatial Ability - Practice Test 1 PDFsalica4gbNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- BMJ Case Reports 2013 Whately BCR 2013 010480Document7 pagesBMJ Case Reports 2013 Whately BCR 2013 010480zakNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Exeter V40: Femoral Stem Using Exeter BroachDocument20 pagesExeter V40: Femoral Stem Using Exeter BroachzakNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Plab Themes EmqsDocument22 pagesPlab Themes EmqsnaeamzNo ratings yet
- Alternative Approach For Lumbar Transforaminal Epidural Steroid InjectionsDocument12 pagesAlternative Approach For Lumbar Transforaminal Epidural Steroid InjectionsIk Soo KimNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 481 - The Use of Dual-Mobility Components in Total Hip ArthroplastyDocument6 pages481 - The Use of Dual-Mobility Components in Total Hip ArthroplastyzakNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- AnglesDocument1 pageAngleszakNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Platelat Rich PlasmaDocument9 pagesPlatelat Rich PlasmazakNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- 10-2-13 830am Treatment of Anterior Knee Pain Anne Rex-TorzokDocument17 pages10-2-13 830am Treatment of Anterior Knee Pain Anne Rex-TorzokzakNo ratings yet
- Alternative Approach For Lumbar Transforaminal Epidural Steroid InjectionsDocument12 pagesAlternative Approach For Lumbar Transforaminal Epidural Steroid InjectionsIk Soo KimNo ratings yet
- Eye Muscle Surgery 2Document8 pagesEye Muscle Surgery 2zakNo ratings yet
- Pectoralis Major RuptureDocument5 pagesPectoralis Major RupturezakNo ratings yet
- Arab Board 1Document1 pageArab Board 1zakNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ped Med HandbookDocument27 pagesPed Med HandbookSoad Shedeed0% (1)
- AMC Recall 1999 To 2008 (Magdi)Document243 pagesAMC Recall 1999 To 2008 (Magdi)zak67% (6)
- The Management of Nerve InjuriesDocument22 pagesThe Management of Nerve InjuriesAnnie JoNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Badminton ReviewerDocument10 pagesBadminton ReviewerHailsey WinterNo ratings yet
- Goa Daman & Diu Factory Rules PDFDocument141 pagesGoa Daman & Diu Factory Rules PDFmrudang1972100% (1)
- Conceptual Artist in Nigeria UNILAGDocument13 pagesConceptual Artist in Nigeria UNILAGAdelekan FortuneNo ratings yet
- AS and A Level: ChemistryDocument11 pagesAS and A Level: ChemistryStingy BieNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Quartile1 PDFDocument2 pagesQuartile1 PDFHanifah Edres DalumaNo ratings yet
- Metal Workers BizHouse - UkDocument3 pagesMetal Workers BizHouse - UkAlex BekeNo ratings yet
- DP November 2017 Examination Schedule en PDFDocument4 pagesDP November 2017 Examination Schedule en PDFSuperlucidoNo ratings yet
- Test 2 Sku3023 A201 QuestionDocument8 pagesTest 2 Sku3023 A201 QuestionHafiz HafizanNo ratings yet
- 9A02502 Transmission of Electric PowerDocument6 pages9A02502 Transmission of Electric PowersivabharathamurthyNo ratings yet
- Haldex-Barnes 2-Stage Pump For Log SplittersDocument2 pagesHaldex-Barnes 2-Stage Pump For Log SplittersPer Akkamaan AgessonNo ratings yet
- 2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticeDocument40 pages2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticebbNo ratings yet
- Kaged Muscle Magazine Issue 1Document41 pagesKaged Muscle Magazine Issue 1hashimhafiz1100% (1)
- AIR Conditioner: Owner'S ManualDocument52 pagesAIR Conditioner: Owner'S Manualashley diazNo ratings yet
- G10Mapeh Exam First QuaterDocument8 pagesG10Mapeh Exam First QuaterJonas LamcisNo ratings yet
- 2nd APJ Abdul Kalam Essay Writing CompetitionDocument2 pages2nd APJ Abdul Kalam Essay Writing CompetitionANURAG SINGHNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 5 Contracting Activity and Technical Staff RequirementsDocument2 pages5 Contracting Activity and Technical Staff RequirementsDaniyar KussainovNo ratings yet
- Test7 PointersDocument16 pagesTest7 PointersPratibha DwivediNo ratings yet
- 3397 - Ciat LDC 300VDocument71 pages3397 - Ciat LDC 300VPeradNo ratings yet
- Carinthia Katalog DownloadDocument16 pagesCarinthia Katalog DownloadOperator_010100% (2)
- TheBasicsofBrainWaves - RS PDFDocument4 pagesTheBasicsofBrainWaves - RS PDFOnutu Adriana-LilianaNo ratings yet
- Metaphysics of LucretiusDocument6 pagesMetaphysics of LucretiusChristopher BennettNo ratings yet
- Coding DecodingDocument21 pagesCoding DecodingAditya VermaNo ratings yet
- Kelas ChondrichtyesDocument15 pagesKelas ChondrichtyesanitagustinawatiNo ratings yet
- 8-General Rules For Erection ProcedureDocument4 pages8-General Rules For Erection ProcedurePrijin UnnunnyNo ratings yet
- Technical Data Sheet: LPI HVSC PlusDocument2 pagesTechnical Data Sheet: LPI HVSC PlusNguyễn TấnNo ratings yet
- The Spirit Controlled Life Ebook PDF 1Document184 pagesThe Spirit Controlled Life Ebook PDF 1Okesola AbayomiNo ratings yet
- MMW ReviewerDocument3 pagesMMW ReviewerMarcSaloj NeryNo ratings yet
- Course Code:TEX3021 Course Title: Wet Processing Technology-IIDocument20 pagesCourse Code:TEX3021 Course Title: Wet Processing Technology-IINakib Ibna BasharNo ratings yet
- Management of DredgedExcavated SedimentDocument17 pagesManagement of DredgedExcavated SedimentMan Ho LamNo ratings yet
- Danika Cristoal 18aDocument4 pagesDanika Cristoal 18aapi-462148990No ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)