Professional Documents
Culture Documents
Wozniacka2005 Optimal Use of Antimalarials in Treating
Uploaded by
l10n_assCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wozniacka2005 Optimal Use of Antimalarials in Treating
Uploaded by
l10n_assCopyright:
Available Formats
Am J Clin Dermatol 2005; 6 (1): 1-11
1175-0561/05/0001-0001/$34.95/0
THERAPY IN PRACTICE
2005 Adis Data Information BV. All rights reserved.
Optimal Use of Antimalarials in Treating
Cutaneous Lupus Erythematosus
Anna Wozniacka1 and Daniel P. McCauliffe2
1
2
Department of Dermatology, Medical University of Lodz, Krzemieniecka, Poland
Rutland Skin Center, Rutland, Vermont, USA
Contents
Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1. Brief Review of Lupus Erythematosus (LE)-Specific Skin Disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
2. Delayed Onset of Action . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3. Antimalarial Treatment Regimens . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.1 Inhibition of Antimalarial Efficacy by Cigarette Smoking . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.2 Antimalarial Treatment of LE-Nonspecific Skin Disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.3 Antimalarial Treatment in Children . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
3.4 Antimalarial Treatment in Pregnancy and in Breastfeeding Mothers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4. Antimalarial Adverse Effects . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4.1 Overdose Precautions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5. Potential Drug Interactions of Hydroxychloroquine and Chloroquine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6. Disorders that May be Worsened by Antimalarial Therapy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
7. Mechanisms by which Antimalarial Agents Provide Benefit . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8. Treatment Options When Standard Therapy Fails . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
9. Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Abstract
1
2
3
3
4
4
5
5
5
6
6
7
8
8
8
Antimalarials have been used to treat cutaneous and systemic lupus erythematosus (LE) for decades.
Although controlled studies comparing the efficacy of antimalarials versus placebo and other treatments are
generally lacking, many case reports and series support the therapeutic efficacy of these agents in treating both
LE-specific and -nonspecific skin lesions. Currently, the two most frequently used antimalarial agents are
chloroquine and hydroxychloroquine. There may be a delay of weeks to months in the onset of therapeutic
effects of antimalarials when treating LE. Smoking appears to inhibit the therapeutic efficacy of antimalarials
when treating cutaneous LE. Antimalarials have been associated with a number of potentially serious adverse
effects, including irreversible loss of vision. The aim of this review is to discuss the many facets of antimalarials
that will help clinicians optimally utilize these agents when treating cutaneous LE.
A review of the literature suggests that Payne[1] was the first to
report the use of antimalarials for treating cutaneous lupus, in
1894. He reported good results in 22 of 28 discoid lupus patients
treated with quinine, a natural alkaloid derived from the bark of the
Peruvian Cinchona tree.[1] During World War II, quinacrine, a
synthetic derivative of quinine, was used for treating malaria. It
was discovered that soldiers who had lupus and other rheumatic
disorders got better while taking quinacrine for malaria. This led to
research into the use of quinacrine and other antimalarials as
therapeutic agents for lupus erythematosus (LE) and additional
rheumatic disorders. Since that time many clinicians have successfully treated patients with systemic and cutaneous LE with antimalarials.[2] Almost all evidence to date on the benefits of antimalarial treatment for LE-specific and -nonspecific skin lesions is
based on case reports and case series. Unfortunately, good control
Wozniacka & McCauliffe
studies comparing antimalarials with placebo or other treatments
are generally lacking.
Currently, the two most frequently used 4-aminoquinoline antimalarial compounds are chloroquine and hydroxychloroquine.
Hydroxychloroquine differs chemically from chloroquine by only
one hydroxyl group and it is considered to be a less toxic analog of
chloroquine. These two drugs are very similar in pharmacokinetics,[3] action,[4] and metabolism.[5] With the advent of chloroquine and hydroxychloroquine, quinacrine has not been used as
frequently because of its more serious adverse effects,[6] although
it is still sometimes used in combination with chloroquine or
hydroxychloroquine when single antimalarial therapy fails.[6-8]
Chloroquine, hydroxychloroquine and quinacrine are water soluble and are readily absorbed from the gastrointestinal tract; plasma
concentration reaches a peak within approximately 8 hours.[9]
During treatment, plasma levels increase gradually to an equilibrium value after several weeks.[10]
1. Brief Review of Lupus Erythematosus (LE)-Specific
Skin Disease
Skin disease is a frequent manifestation of LE.[11] Cutaneous
lesions include both lupus-specific (clinically and histologically
diagnostic of LE) and lupus-nonspecific eruptions that can be
found in other clinical settings (table I).
There are three major LE-specific skin diseases according to
the Gilliam[12,13] classification: acute cutaneous LE, subacute cutaneous LE and chronic cutaneous LE. Usually one form of cutaneous LE predominates in any given patient, although less commonly a patient will have two or more forms of LE-specific skin
disease.[14]
Acute cutaneous LE lesions develop as erythematous and
edematous papules and plaques that are usually symmetrical and
found on sun-exposed areas such as the face, extensor arms, and
hands. A classic presentation is the malar (butterfly) distribution of
erythema over the central cheeks. Less commonly, acute cutaneous LE can present as a more generalized morbilliform eruption.
Acute cutaneous LE lesions virtually always present in a patient
with systemic LE.[14] For this reason, patients are often treated
more aggressively for systemic disease with systemic corticosteroids and other immunosuppressive agents (e.g. azathioprine,
cyclophosphamide). There is evidence that hydroxychloroquine
can provide corticosteroid-sparing effects, reduce flares and inhibit the development of acute cutaneous LE lesions, when treating
patients with systemic LE.[15-17] Antimalarial drugs are not recommended as a monotherapy for severe life-threatening systemic LE,
but may provide benefit for acute cutaneous LE as well as for
fatigue, arthralgias, myalgias, and serositis.
2005 Adis Data Information BV. All rights reserved.
Table I. Classification of lupus erythematosus (LE)-associated skin lesions
LE-specific skin lesions
Acute cutaneous LE
localized
generalized
Subacute cutaneous LE
annular
papulosquamous
Chronic cutaneous LE
discoid LE
localized (head and neck)
disseminated
hypertrophic LE
lupus profundus (panniculitis)
lupus tumidus
chilblain lupus
LE-nonspecific skin lesions
Photosensitivity
Oral ulcers
Alopecia
Urticaria
Vasculitis
Vesiculobullous lesions
Acral changes (pitting, nail and nailfold changes, Raynaud phenomenon)
Cutaneous mucinoses
Calcinosis cutis
Subacute cutaneous LE occurs most frequently in Caucasian
women.[18] Skin lesions are superficial, symmetrical and photodistributed. They are manifested mainly on the trunk and upper
extremities, less commonly on the face, and rarely below the
waist. The early erythematous scaly papules evolve into annular
plaques with central clearing, or into papulosquamous lesions that
are psoriasis-like with an overlying scale. Rarely do both patterns
appear in the same patient.[19] One-third to one-half of patients
with subacute cutaneous LE fulfill the American College of Rheumatology criteria for the diagnosis of systemic LE. Sun protection,
local corticosteroids and antimalarials are usually the first line of
treatment. Clinical observations indicate that in the majority of
patients subacute cutaneous LE responds to a single antimalarial
agent or combined antimalarial therapy.[20,21]
Chronic cutaneous LE can be subdivided into classic discoid
LE (the most common form of chronic cutaneous LE), hypertrophic LE, lupus profundus (panniculitis), lupus tumidus, and chilblain
lupus.[14] Although these lesions are usually more chronic (as the
name suggests) than those of acute cutaneous LE, they are not
Am J Clin Dermatol 2005; 6 (1)
Antimalarial Treatment of Cutaneous Lupus Erythematosus
necessarily any longer lasting than those of subacute cutaneous LE
and are similarly responsive to antimalarial therapy.[22]
3. Antimalarial Treatment Regimens
Discoid LE lesions usually start as flat or slightly elevated,
erythematous, sharply demarcated macules or papules with a scaly
surface. These early lesions slowly enlarge peripherally into larger
coin-shaped (discoid) plaques demonstrating adherent scale formation, follicular plugging, atrophic scarring and hyperpigmentation, usually followed by central hypopigmentation and telangiectasias. The vast majority of patients with discoid LE have facial,
neck, ear, and/or scalp involvement. Lesions on the trunk and
extremities (disseminated form) occur less frequently and are
more commonly associated with systemic LE than discoid LE
confined to the head and neck area (localized form). Because of
the potential for scarring associated with discoid LE lesions,
aggressive therapy is advocated. Delay in onset of the beneficial
effects of antimalarials is the reason why short-term, high-potency
topical, intralesional, or systemic corticosteroids might initially be
used.[17,23]
Most physicians use hydroxychloroquine as the antimalarial of
choice, as it seems to be generally accepted that hydroxychloroquine has fewer adverse effects than chloroquine and quinacrine.
The administration schedule used in cutaneous lupus depends in
part on the extent of the skin lesions, the patients lean
bodyweight, and tolerance to the antimalarial. For the average size
adult with LE-specific skin disease, therapy with hydroxychloroquine is usually started at 400 mg/day (the recommended dosage
should not exceed 6.5 mg/kg lean bodyweight/day):
Antimalarials have also been effective in treating less common
forms of chronic cutaneous LE, such as lupus panniculitis,[24]
calcifying lupus panniculitis,[25] lupus tumidus,[2] hypertrophic
LE,[26,27] and chilblain lupus.[28]
If, after at least 2 months of hydroxychloroquine treatment,
there is no improvement, quinacrine 100 mg/day can be added.
Quinacrine hydrochloride is no longer available but quinacrine
dihydrochloride can be provided by compounding pharmacies.
Once the patient responds to this combination, one can consider
decreasing the hydroxychloroquine to 200 mg/day following 1
month of quinacrine initiation and also decreasing quinacrine
dosage during follow-up in order to minimize the adverse effects.
There is evidence that the combination of two antimalarial
agents is sometimes effective in the treatment of patients with
chronic cutaneous LE when a single agent fails.[6,7,29,30]
2. Delayed Onset of Action
It is important to allow enough time for antimalarials to provide
benefit. For systemic LE with concomitant skin lesions, Wallace[31] has observed that it can sometimes take hydroxychloroquine 3 months to improve not only skin rashes, but also fatigue,
arthralgias, myalgias, serositis, mucous membrane ulcerations,
and the patients sense of well-being. It is generally accepted that
the therapeutic effects of chloroquine and quinacrine treatment for
most cutaneous LE patients should begin to become apparent
within several weeks after starting treatment[10] and up to 2 months
after hydroxychloroquine treatment.[32]
Because it sometimes takes 12 months to begin seeing benefit
from antimalarials, 2 months might be considered the minimum
treatment period, and in some cases it might be prudent to wait
even longer before discontinuing antimalarial therapy. During this
initial treatment period, topical or intralesional corticosteroids and,
rarely, systemic corticosteroids, can be used temporarily to provide a more prompt improvement.[14]
2005 Adis Data Information BV. All rights reserved.
Lean bodyweight (men) = (1.10 weight [kg]) 128 weight2/
(100 height [m])2
Lean bodyweight (women) = (1.07 weight [kg]) 148
weight2/(100 height [m])2
The drug can be taken during or between meals, once daily, or
in divided doses.
Chloroquine is usually given in a dosage of 250500mg daily.
The dosage should not exceed 4 mg/kg lean bodyweight per day. If
the response is not satisfactory after at least 6 weeks, quinacrine
can be added at a dosage of 100 mg/day. Some patients may
respond to chloroquine but not hydroxychloroquine (figure 1), so
it might be beneficial to try chloroquine if hydroxychloroquine
fails.
Little has been published about combining antimalarials with
other non-antimalarial agents when treating cutaneous LE after
antimalarials alone have failed. In systemic LE, antimalarials are
often combined with other agents for greater therapeutic efficacy
when treating extracutaneous disease.
Antimalarial therapy is often continued for many months, if not
years, particularly in patients with systemic LE who gain additional non-cutaneous benefits from antimalarials therapy. In other
patients, even after the skin disease has resolved, it is common to
continue antimalarial treatment for additional months and gradually decrease the dosage to determine the minimal dose needed to
control the skin disease.[31,32]
Am J Clin Dermatol 2005; 6 (1)
Wozniacka & McCauliffe
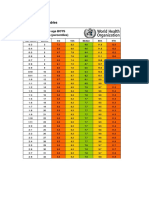
Fig. 1. (a) Patient with subacute cutaneous lupus erythematosus that failed to respond to hydroxychloroquine monotherapy for several months followed by
a combination of hydroxychloroquine and quinacrine. (b) Same patient 1 month after hydroxychloroquine was switched to chloroquine while quinacrine
therapy was maintained.
3.1 Inhibition of Antimalarial Efficacy by
3.2 Antimalarial Treatment of LE-Nonspecific Skin Disease
Cigarette Smoking
Two studies have demonstrated that smoking may interfere
with the efficacy of antimalarials in treating discoid LE and
subacute cutaneous LE.[33,34] One study found that discoid LE and
subacute cutaneous LE lesions were responsive to antimalarials in
91% of nonsmoking patients compared with only 40% of smokers.[34] This study also found that the cutaneous LE in patients who
smoked the most responded least well to antimalarials. It is therefore advisable that aggressive smoking cessation efforts be made
by smokers with cutaneous LE that is not responding well to
antimalarial treatment. The authors of this article have noted
dramatic improvement in patients with antimalarial-refractory discoid LE lesions after they stopped smoking while continuing on
antimalarial therapy.
How smoking might interfere with antimalarial efficacy is
uncertain. It is possible that nicotine might alter the metabolism of
aminoquinoline compounds by inducing hepatic microsomal enzymes.[35] Cigarette smoking may possibly interfere with the beneficial effects of antimalarials by blocking their uptake into
lysosomes[36] or by enhancing the metabolic clearance of antimalarials, as has been shown for quinine.[37] Compounds present
in the cigarette smoke might also be responsible for directly
exacerbating cutaneous lupus lesions. It is interesting to note that
there is some evidence that patients with discoid or systemic LE
are more likely to be smokers than age- and sex-matched controls.[34,38,39]
2005 Adis Data Information BV. All rights reserved.
Oral mucosal lesions are observed in 1524% of systemic LE
patients. Ulcerations of the oral and nasal mucosa are more often
seen in association with acute cutaneous LE lesions. Some oral
lesions may show LE-type histopathology when biopsied, particularly in discoid LE patients. There is some evidence that antimalarial agents are of benefit in treating mucosal lesions in LE
patients.[40]
Calcinosis cutis is less common in patients with lupus than in
patients with juvenile dermatomyositis and systemic sclerosis. It
has been reported in patients with discoid LE[41] and subacute
cutaneous LE.[42] In a patient with subacute cutaneous LE, Morgan
and Callen[25] described calcifying lupus panniculitis successfully
treated with chloroquine 500 mg/day and diltiazem 240mg twice a
day. After 10 months of treatment the calcinotic nodules broke
into several smaller nodules and improved considerably.
Patients with LE are more likely to complain of photosensitivity reactions than patients with other rheumatic disorders. Antimalarials may have some photoprotective effects. Chloroquine
was shown to increase the minimal erythema dose in patients after
3 months of treatment.[43]
Urticarial vasculitis lesions are purpuric and sometimes painful, and remain in the same location for at least several days, while
urticarial lesions (which rarely accompany lupus) tend to be pruritic, blanching, more evanescent and individual lesions should
resolve within 24 hours. The vasculitis lesions are often resistant
to antimalarial treatment and are more likely to resolve after
treatment with dapsone, systemic corticosteroids and/or cytotoxic
agents such as cyclophosphamide.[44]
Am J Clin Dermatol 2005; 6 (1)
Antimalarial Treatment of Cutaneous Lupus Erythematosus
Lupus patients, particularly those with very active systemic LE,
sometimes develop vesiculobullous eruptions called bullous systemic LE.[45] These lesions are usually treated with systemic
corticosteroids and dapsone.[46] Krim et al.[47] recently reported a
case of bullous LE induced by radiotherapy that was successfully
treated with hydroxychloroquine and topical corticosteroids. Rarely, vesiculobullous lesions may arise in acute and subacute cutaneous LE lesions.
Patients with LE may develop several types of alopecia in
addition to that arising from scarring discoid LE lesions. Antimalarials may help prevent the progression of hair loss but cannot
reverse the alopecia caused by scarring discoid LE.[40]
Cutaneous mucinoses presents in patients with LE as papular,
plaque-like, and nodular cutaneous lesions resulting from dermal
mucin deposition.[48] They typically occur on the trunk and arms
and may be responsive to antimalarial or prednisone therapy.[49]
3.3 Antimalarial Treatment in Children
Hydroxychloroquine is considered to have a good safety profile
and be well tolerated in children, if recommended dosage limits
are not exceeded. Fox et al.[50] described two girls in whom lupus
profundus occurred at 3.5 and 8 years of age. They were both
successfully treated with hydroxychloroquine for 4 years and 1
year, respectively. There are also several reports of using chloroquine in children with cutaneous lupus with the dosage not exceeding 4 mg/kg lean body mass per day.[51,52]
3.4 Antimalarial Treatment in Pregnancy and in
Breastfeeding Mothers
Although some authors have advocated the withdrawal of antimalarial treatment when a patient becomes pregnant, more recent
reports indicate that antimalarials not only have a good safety
profile but are helpful in suppressing LE flares that sometime
occur during pregnancy.[53-55] Levy et al.,[54] in the first randomized, placebo-controlled study of patients with lupus, not only
revealed the absence of teratogenic effects after a 3-year follow-up
of children but also observed a lower frequency of LE flares
during pregnancy. It is even suggested that hydroxychloroquine,
but not quinacrine, can be initiated during pregnancy for lupus
flares.[54]
Hydroxychloroquine and chloroquine bind avidly to various
tissues, so stopping these agents at the first sign of pregnancy
means that it will still take several months for them to be completely eliminated from the bound tissues.[10,56] Hydroxychloroquine
may be safer than chloroquine during pregnancy as it binds less
avidly to tissues, is less toxic and has a lesser ability to cross the
placenta than chloroquine.[54] Hydroxychloroquine may have an
2005 Adis Data Information BV. All rights reserved.
additional benefit in treating antiphospholipid antibody syndrome
in pregnancy.[57] The safety of hydroxychloroquine, chloroquine,
and quinacrine in breastfeeding mothers has not been established.
4. Antimalarial Adverse Effects
Adverse effects with antimalarials occur in <10% of patients.[31] Gastrointestinal reactions are probably the most common
but they are transient and can be diminished by lowering the dose
of the drug. Most patients complaints concern abdominal cramps,
nausea, vomiting, or diarrhea. Quinacrine causes these symptoms
more often than chloroquine and hydroxychloroquine and in up to
30% of treated patients.[32]
The most common visual problems encountered in antimalarial
treated patients include difficulty in reading, photophobia, blurred
distance vision, visual field defects, and light flashes.[58-61]
Hydroxychloroquine and chloroquine can induce irreversible retinal damage, so patients are advised to have a baseline ophthalmologic evaluation before starting therapy to document any preexisting retinal changes. It appears that the risk of retinal toxicity is
minimized when the total daily dose of hydroxychloroquine does
not exceed 6.5 mg/kg lean bodyweight per day and chloroquine
does not exceed 34 mg/kg lean bodyweight per day. Several
studies have found that retinal toxicity in hydroxychloroquinetreated patients is quite rare. In a retrospective review of 1207
hydroxychloroquine-treated patients, only one patient (0.08%) had
definite toxicity, and this patient had received a dosage greater
than the recommended upper limit of 6.5 mg/kg/day.[62] Patients
taking hydroxychloroquine for greater than 6 years or who have
renal disease may be at greater risk of developing retinal toxicity.[63] Daily dose and keratopathy have been associated with a risk
of developing chloroquine retinopathy.[64]
There have been reports that resistant skin lesions are sometimes successfully treated with the combination of hydroxychloroquine (or chloroquine) and quinacrine, without any increase in eye
toxicity.[6,29,30] However, one report raises some concern about
increased retinal toxicity when these antimalarials are combined.[7]
Despite the rarity of this adverse effect, cases of irreversible
retinal damage continue to be reported in patients on long-term
therapy. Thus, many physicians still recommend that patients have
ophthalmologic evaluations at 6- to 12-month intervals while
receiving therapy. This evaluation should include a funduscopic
examination, visual field testing (including central fields with a
red object), and visual acuity testing. Electro-oculograms may
have less value in screening for antimalarial-induced retinal toxicity.[65] A recent article has indicated that red Amsler grid screening
helps identify patients more likely to have hydroxychloroquineAm J Clin Dermatol 2005; 6 (1)
induced ocular toxicity, but an abnormal screening is in itself an
unreliable predictor of toxicity.[66]
It should be remembered that retinal lesions have been associated with systemic LE, unrelated to antimalarial therapy. Antimalarials usually take years to induce retinal pathology, so complaints of visual symptoms weeks after starting therapy might be
related to other causes, including concomitant corticosteroid treatment.
Both chloroquine and hydroxychloroquine may be deposited in
the corneal epithelium and can be detected on slit lamp examination. Some patients with these corneal deposits may complain of
halos around light sources and photophobia. However, visual
acuity is not reduced.[59] Corneal deposits are transient and disappear with drug discontinuation.[60] It is worth noting that since the
recommended dose of chloroquine has decreased over the years,
corneal abnormalities are now rarely observed.[61] Quinacrine appears to have insignificant adverse ocular effects compared with
hydroxychloroquine and chloroquine.
Although there have been descriptions in the medical literature
of hematologic and hepatic adverse effects during hydroxychloroquine or chloroquine treatment, some authors advocate that pretreatment and follow-up laboratory testing are not necessary,
particularly for hydroxychloroquine.[63,67,68] Sontheimer[68] reviewed the literature on this matter recently and found that this
stance is supported by the fact that these adverse effects are
exceedingly rare, particularly when current dosage guidelines are
followed. The current American college of Rheumatology guidelines for the use of hydroxychloroquine in patients with rheumatoid arthritis state that baseline and follow-up laboratory testing
are not necessary or recommended.[67] However, it seems prudent
to obtain baseline and periodic blood counts and hepatic function
tests in patients who have pre-existing hepatic or hematologic
disease or in patients at increased risk of developing hematologic
or hepatic diseases.
Hematologic function should be evaluated during quinacrine
therapy or combined treatment. Aplastic anemia following quinacrine treatment was described after the drug was introduced during
World War II, and was mostly related to overdoses or concomitant
treatment with other bone marrow suppressant drugs.[69] At lower
doses quinacrine is less likely to cause serious problems.[68,70,71]
Quinacrine is more likely to induce hemolysis in patients deficient
in glucose-6-phosphate dehydrogenase than chloroquine or
hydroxychloroquine.[72]
Antimalarials rarely induce neuromuscular toxicity. Neurotoxicity was a problem in the past when much higher doses of
antimalarials were used. Very little has been published in recent
years about the occurrence of psychiatric disorders due to antimalarial therapy. There are some literature reports that chloro 2005 Adis Data Information BV. All rights reserved.
Wozniacka & McCauliffe
quine, hydroxychloroquine, and quinacrine can cause depression,
claustrophobia, feelings of inferiority, loss of sleep from bad
dreams, suspiciousness, loss of affection, and toxic psychosis, but
these adverse effects were usually associated with higher dosages
than are currently prescribed.[73-75] Antimalarials may rarely predispose susceptible individuals to seizures.[76]
Antimalarial drugs can induce skin dryness, pruritus, and urticaria.[77,78] Blue-black skin pigmentation sometimes develops in
sun-exposed areas and also on the palate and nails.[32] Bleaching of
the hair has rarely been described.[32] Hydroxychloroquine and
chloroquine have rarely been reported to precipitate acute generalized exanthematous pustulosis, erythema multiforme, and toxic
epidermal necrolysis.[79,80]
During quinacrine treatment diffuse yellowing of the skin,
sclerae and bodily secretions can occur but these changes resolve
after treatment stops.[81] Quinacrine has also been associated with
a lichenoid drug eruption, which may be a harbinger of bone
marrow toxicity.[32]
Although antimalarials have sun-protective properties, paradoxical photosensitivity has been described.[82] Pelle and Callen[83]
reported that adverse cutaneous reactions to hydroxychloroquine
are more common in patients with dermatomyositis than in patients with several types of cutaneous LE.
There are several case reports of cardiac conduction defects
(atrioventricular block) after chloroquine treatment.[84] Therefore,
some authors advocate not prescribing antimalarials in patients
with pre-existing conduction defects.[84]
4.1 Overdose Precautions
Adverse effects can occur from taking too high a dose of
antimalarials. Hydroxychloroquine overdose has been associated
with visual disturbances, headache and drowsiness, and
seizures.[85] Chloroquine overdose has been associated with nausea, vomiting, headache, drowsiness, seizures, vision changes, low
blood pressure (causing dizziness or fainting), respiratory difficulties, heartbeat irregularities, and cardiac arrest.[86] Marquardt and
Albertson[87] described tachycardia, hypotension, CNS depression,
and conduction defects that occurred within 30 minutes of ingesting a handful of hydroxychloroquine 200mg pills. Quinacrine
overdose has been associated with fainting, seizures, and heart
rhythm irregularities. It is very important to keep antimalarial
medications out of reach of small children.
5. Potential Drug Interactions of
Hydroxychloroquine and Chloroquine
Antimalarials may interact with other drugs. Chloroquine has
antiarrhythmic potential and can inhibit ventricular ectopy, similar
Am J Clin Dermatol 2005; 6 (1)
Antimalarial Treatment of Cutaneous Lupus Erythematosus
to amiodarone and chlorpromazine. This raises some concerns
about prescribing these medicines together.[88]
Simultaneous treatment with chloroquine decreases the bioavailability of ampicillin[81] and methotrexate.[89] Kaolin reduces
the effectiveness of chloroquine.[90] Cimetidine impairs the elimination of chloroquine in healthy subjects.[91]
Cultured HeLa cells grown in the presence of chloroquine
retained more digoxin and digitoxin in their lysosomes than did
cells grown in the absence of chloroquine.[92] The clinical implications of this finding are uncertain.
Because antimalarials adversely affect both the pre- and postsynaptic aspects of neuromuscular transmission at concentrations
close to those employed in clinical practice, they should not be
used, or should be used with caution, in the company of other
drugs or disorders that compromise neuromuscular transmission.[93]
To our knowledge there are no known food interactions with
hydroxychloroquine, chloroquine, or quinacrine.
6. Disorders that May be Worsened by
Antimalarial Therapy
Certain disorders may be worsened by antimalarial therapy
(table II). The doses of chloroquine and hydroxychloroquine that
are used to treat cutaneous LE and related rheumatic skin diseases
will predictably produce acute hepatitis in individuals who have
porphyria cutanea tarda. Even low doses of antimalarials (e.g.
hydroxychloroquine >100mg twice weekly) can cause toxic hepatitis[94] in patients with porphyria cutanea tarda. This very severe
hepatic reaction can simulate an acute surgical abdomen, which
occurs within several days of treatment. There is a single report of
two cases of idiosyncratic fatal hepatotoxic effects occurring within 2 weeks of starting hydroxychloroquine therapy at a common
daily dose of 400 mg/day.[95]
Serious idiosyncratic anemia and hepatotoxic effects of antimalarials related to glucose-6-phosphate dehydrogenase deficiency are very rare. Because of the uncommonness of both porphyria
cutanea tarda and glucose-6-phosphate dehydrogenase deficiency,
Table II. Disorders that may be worsened by antimalarial therapy
Porphyria cutanea tarda
Psoriasis
Hepatic disease
Glucose-6-phosphate dehydrogenase deficiency-associated anemia
Hematologic disease
Ocular disease
Neuromuscular disorders
Psychiatric disturbances
2005 Adis Data Information BV. All rights reserved.
routine screening of all patients before starting antimalarial therapy is not considered necessary by some.[68] There is general
agreement that antimalarial compounds should be used with caution in patients with hepatic disease or alcoholism. Patients at risk
of hepatic disease should have routine liver function tests before
and periodically while receiving antimalarial agents. When antimalarials are used according to the treatment guidelines (hydroxychloroquine 6.5 mg/kg/day, chloroquine 4 mg/kg/day and
quinacrine 100 mg/day) they are unlikely to cause hepatic injury
in healthy individuals.[68] The data in the literature suggests that
hydroxychloroquine is even protective against elevated liver function test results in patients with rheumatoid arthritis receiving
aspirin or methotrexate.[96] As antimalarials can cause adverse
ocular effects, they are contraindicated in patients with pre-existing retinopathy, visual field defects, or maculopathy.[97]
There are conflicting opinions concerning the necessity for
periodic complete blood cell counts in patients during antimalarial
treatment. In the authors opinion periodic testing is still advisable
during treatment, particularly in patients who have or are at risk of
developing hematologic disease. Antimalarials should be discontinued if any severe blood disorder appears. It is worth mentioning
that many studies did not reveal hematologic abnormalities during
routine antimalarial treatment.[49,96,98] Although quinacrine produced serious hematologic adverse effects when taken in dosages
of >100 mg/day in the past, hematologic reactions are so unlikely
when current dosage guidelines are followed that it is not cost
effective to frequently check hematologic function during treatment.[81]
There are conflicting data in the literature concerning the use of
antimalarials in psoriatic patients. Some authors claim that in
contrast to lithium and -blockers, antimalarials do not induce
psoriasis de novo but only worsen already existing disease.[99]
As antimalarials can be neurotoxic and myotoxic, special care
is required when treating patients with neuromuscular disorders.
Caucasians and patients with concomitant renal failure may be at
increased risk of developing proximal myopathy, peripheral
neuropathy, and cardiac myotoxicity while taking hydroxychloroquine.[100]
Although the incidence of antimalarial psychosis is small, close
observation of patients during therapy is recommended, especially
when any behavioral changes are noted.[75] It is unlikely that
hydroxychloroquine could worsen schizophrenia. In fact, hydroxychloroquine was once considered as a useful adjunct therapy for
the treatment of schizophrenia, but the results of studies performed
on 61 randomized patients with schizophrenia did not show significant differences between general symptoms in patients treated
with standard antipsychotic drugs combined with hydroxychloroquine compared with antipsychotics combined with placebo.[101]
Am J Clin Dermatol 2005; 6 (1)
Wozniacka & McCauliffe
7. Mechanisms by which Antimalarial Agents
Provide Benefit
Although antimalarials have been used for decades in treating
cutaneous LE, the precise mechanisms by which they provide
therapeutic benefit are not well defined. These mechanisms have
been more extensively reviewed elsewhere by the authors of this
article.[102] Potential effects include a number of interrelated antiinflammatory[103] and immunosuppressive effects[104] that include
photoprotection,[105] lysosomal stabilization,[106] suppression of
antigen presentation,[107] and inhibition of prostaglandin[108] and
cytokine synthesis.[109] Antimalarials may inhibit tumor necrosis
factor (TNF)- expression. This is of particular interest as thalidomide, an agent that appears to be efficacious in treating cutaneous
LE, may act by opposing the effects of TNF.[110]
8. Treatment Options When Standard Therapy Fails
The standard treatment for most patients with cutaneous LE
includes photoprotection, topical corticosteroids and antimalarials
(figure 2). There are other therapeutic options when standard
therapy fails.
Dapsone, a sulfone that is used in the primary treatment of
dermatitis herpetiformis and as an antibacterial drug for leprosy,
has been successfully administered in bullous eruptions,[116] subacute cutaneous LE,[117] and discoid LE lesions.[118]
Systemic corticosteroids are useful not only in refractory systemic LE but also during the initiation of antimalarial therapy in
Begin treatment with photoprotective measures and consider topical
or intralesional corticosteroids, tacrolimus, pimecrolimus or imiquimod1
Begin hydroxychloroquine up to 6.5 mg/kg lean bodyweight per day
If a smoker, encourage methods for smoking cessation
If no response by 8 weeks, add quinacrine 100 mg/day
If no response in a further 4 weeks switch from hydroxychloroquine
to chloroquine up to 4 mg/kg lean bodyweight per day while
continuing quinacrine 100 mg/day
If no response after several weeks, try a retinoid or clofazimine.
Alternatively, dapsone can be used (dapsone might be tried before
antimalarials in bullous LE)
If still no response, consider thalidomide or gold therapy
If all of the above fail or could not be tolerated, consider
immunosuppressive agents including short-term systemic
corticosteroids, methotrexate, azathioprine, mycophenolate mofetil, or
cyclosporine (ciclosporin)
Fig. 2. Treatment algorithm for lupus erythematosus (LE)-specific cutaneous LE, based mostly on data from reports on subacute cutaneous LE and
discoid LE. 1 Use of tacrolimus, pimecrolimus and imiquimod based on
recent limited case reports.[111-115]
2005 Adis Data Information BV. All rights reserved.
scarring cutaneous disease while waiting for the delayed benefit of
antimalarials. Long-term systemic corticosteroids are not advisable in patients whose clinical disease is limited to the skin.
Retinoids seem to be effective in hypertrophic discoid LE[119]
and also in other forms of cutaneous lupus, as shown in a randomized, double-blind, multicenter study.[120] Thalidomide, an antiinflammatory agent and immunomodulator that inhibits the production of TNF, is beneficial for LE-specific skin lesions. However, adverse effects that include birth defects, irreversible neuropathy, and rapid relapse following withdrawal, limit the utility of
this drug.[110]
Clofazimine has been reported to be beneficial for some cutaneous LE patients.[121] It should be remembered that adverse effects
such as nausea and diarrhea or orange-pink skin pigmentation and
bodily secretion discolorations occur, especially during long-term
treatment.[121]
Immunosuppressive agents such as azathioprine,[122] methotrexate,[123,124] and cyclosporine (ciclosporin)[125] are sometimes used
in patients with severe disease unresponsive to other types of
therapy. The improvement of lupus skin lesions has also been
reported after gold therapy.[126] Unfortunately, this drug frequently
induces mucocutaneous, hematologic, renal, and pulmonary adverse effects that requires its discontinuation. Additionally, recent
case reports indicate that topical tacrolimus, pimecrolimus, and
imiquimod might provide benefit for cutaneous LE.[111-115]
9. Conclusions
Although there is a lack of well controlled studies to show the
benefit of antimalarials in cutaneous LE, there is much evidence to
support their efficacy in treating LE-specific skin disease. They
also have utility in treating some forms of LE-nonspecific skin
disease. It is important that clinicians allow ample time for the
antimalarials to begin working as there may be a lag time of
several weeks to 2 months before improvement is noted. Cigarette smokers with cutaneous LE that is unresponsive to antimalarial agents should stop smoking, as there is evidence that
smoking interferes with antimalarial efficacy. Hydroxychloroquine appears to have a good safety profile for use in children and
during pregnancy, but its safety in breastfeeding mothers is uncertain. Although antimalarials for the most part are well tolerated
with little risk of serious adverse effects when dosage guidelines
are followed, patients with certain disorders or on certain medications may be at increased risk of antimalarial adverse effects. The
frequency at which laboratory and ophthalmologic testing should
be performed is debatable.
Am J Clin Dermatol 2005; 6 (1)
Antimalarial Treatment of Cutaneous Lupus Erythematosus
Acknowledgments
No sources of funding were used to assist in the preparation of this
manuscript. The authors have no conflicts of interest that are directly relevant
to the content of this review.
References
1. Payne JF. A postgraduate lecture on lupus erythematosus. Clin J 1894; 4: 223-9
2. Tsakonas E, Joseph L, Esdaile JM, et al. A long-term study of hydroxychloroquine
withdrawal on exacerbations in systemic lupus erythematosus: the Canadian
Hydroxychloroquine Study Group. Lupus 1998; 7: 65-7
3. Ritschel WA, Hammer GV, Thompson GA. Pharmacokinetics of antimalarials and
proposals for dosage regimens. Int J Clin Pharmacol Biopharm 1978; 16:
395-401
4. Laaksonen AL, Koskiahde V, Juva K. Dosage of antimalarial drugs for children
with juvenile rheumatoid arthritis and systemic lupus erythematosus. Scand J
Rheumatol 1974; 3: 103-8
5. McChesney EW, Rothfield NF. Comparative metabolic studies of chloroquine and
hydroxychloroquine. Arthritis Rheum 1964; 7: 328-9
6. Feldmann R, Salomon D, Saurat JH. The association of the two antimalarials
chloroquine and quinacrine for treatment-resistant chronic and subacute cutaneous lupus erythematosus. Dermatology 1994; 189: 425-7
7. Lipsker D, Piette JC, Cacoub P, et al. Chloroquine-quinacrine association in
resistant cutaneous lupus. Dermatology 1995; 190: 257-8
8. Toubi E, Rosner I, Rozenbaum M, et al. The benefit of combining hydroxychloroquine with quinacrine in the treatment of SLE patients. Lupus 2000; 9: 92-5
9. Koranda FC. Antimalarials. J Am Acad Dermatol 1981; 4: 650-5
10. Sjolin-Forsberg G, Berne B, Blixt C, et al. Chloroquine phosphate: a long-term
follow up of drug concentration in skin suction blister fluid and plasma. Acta
Derm Venereol 1993; 73: 426-9
11. Hochberg MC, Boyd RE, Ahearn JM, et al. Systemic lupus erythematosus: a
review of clinico-laboratory features and immunogenetic markers in 150 patients with emphasis on demographic subsets. Medicine 1985; 64: 285-95
12. Gilliam JN, Sontheimer RD. Distinctive cutaneous subsets in the spectrum of lupus
erythematosus. J Am Acad Dermatol 1981; 4: 471-5
13. Gilliam JN, Sontheimer RD. Skin manifestations of SLE. Clin Rheum Dis 1982; 8:
207-18
14. McCauliffe DP. Cutaneous lupus erythematosus. Semin Cutan Med Surg 2001; 20:
14-26
15. The Canadian Hydroxychloroquine Study Group. A randomized study of the effect
of withdrawing hydroxychloroquine sulfate in systemic lupus erythematosus.
N Engl J Med 1991; 324: 150-4
16. The Canadian Hydroxychloroquine Study Group. A long-term study of hydroxychloroquine withdrawal on exacerbations in systemic lupus erythematosus.
Lupus 1997; 7: 80-5
17. Sontheimer RD, Provost TT. Cutaneous manifestations of lupus erythematosus. In:
Wallace DJ, Hahn BH, editors. Dubois lupus erythematosus. 5th ed. Baltimore
(MD): Williams & Wilkins, 1997: 569-23
18. Sontheimer RD, Thomas JR, Gilliam JM. Subacute cutaneous lupus erythematosus. Arch Dermatol 1979; 115: 1409-15
19. Cardinali C, Caproni M, Baenacchi E, et al. The spectrum of cutaneous manifestations in lupus erythematosus: the Italian experience. Lupus 2000; 9: 417-23
20. Furner BB. Treatment of subacute cutaneous lupus erythematosus. Int J Dermatol
1990; 29: 542-7
21. Ruzicka T, Bieber T, Meurer M. Subacute cutaneous lupus erythematosus: clinical
aspects, immunology and therapy. Wien Klin Wochenschr 1987; 99: 802-7
22. Jessop S, Whitelaw D, Jordan F. Drugs for discoid lupus erythematosus. Cochrane
Database Syst Rev 2001; 1: CD 002954
23. Callen JP. Chronic cutaneous lupus erythematosus. Clinical, laboratory therapeutic, and prognostic examination of 62 patients. Arch Dermatol 1982; 118: 412-6
24. Chung HS, Hann SK. Lupus panniculitis treated by a combination therapy of
hydroxychloroquine and quinacrine. J Dermatol 1997; 24: 569-72
25. Morgan KW, Callen JP. Calcifying lupus panniculitis in a patient with subacute
cutaneous lupus erythematosus: response to diltiazem and chloroquine. J Rheumatol 2001; 28: 129-32
2005 Adis Data Information BV. All rights reserved.
26. Harvey S, Pineda R, Shore JW, et al. Hypertrophic discoid lupus erythematosus of
conjunctiva. Am J Ophthalmol 1999; 127: 604-5
27. Donzis PB, Insler MS, Buntin DM, et al. Discoid lupus erythematosus involving
the eyelids. Am J Ophthalmol 1984; 98: 32-6
28. Pock L, Petrovska P, Becvar R, et al. Verrucous form of chilblain lupus erythematosus. J Eur Acad Dermatol Venereol 2001; 15: 448-51
29. Dubois EL. Antimalarials in the management of discoid and systemic lupus
erythematosus. Semin Arthritis Rheum 1978; 8: 33-51
30. Werth V, Franks A. Treatment of discoid skin lesions with azathioprine. Arch
Dermatol 1986; 122: 746-7
31. Wallace DJ. Antimalarials: the real advance in lupus. Lupus 2001; 10: 385-7
32. Wallace DJ. Antimalarial therapies. In: Wallace DJ, Hahn BH, editors. Dubois
lupus erythematosus. 5th ed. Baltimore (MD): Williams & Wilkins, 1997:
1117-40
33. Rahman P, Gladmann DD, Urowitz MB. Efficacy of antimalarial therapy in
cutaneous lupus in smokers versus non-smokers. J Rheumatol 1998; 25: 1716-9
34. Jewell ML, McCauliffe DP. Patients with cutaneous lupus erythematosus who
smoke are less responsive to antimalarial treatment. J Am Acad Dermatol 2000;
42: 983-7
35. Miller RG. Cigarettes and drug therapy: pharmacokinetic and pharmacodynamic
considerations. Clin Pharm 1990; 9: 125-35
36. Polet T. The effects of lysosomotrophic amines on protein degradation, migration
of nonhistone proteins to the nucleus, and cathepsin D in lymphocytes. J Cell
Physiol 1985; 122: 415-23
37. Wanwimolruk S, Wong SM, Coville PF, et al. Cigarette smoking enhances the
elimination of quinine. Br J Clin Pharmacol 1993; 36: 610-4
38. Hardy CJ, Palmer BP, Muir KR, et al. Smoking history, alcohol consumption, and
systemic lupus erythematosus: a case-control study. Ann Rheum Dis 1998; 57:
451-5
39. Nagata C, Fujita S, Iwata H, et al. Systemic lupus erythematosus: a case-control
epidemiologic study in Japan. Int J Dermatol 1995; 34: 333-7
40. Wallace DJ. Antimalarial agents and lupus. Rheum Dis Clin North Am 1994; 20:
243-63
41. Johansson E, Kanerva L, Niemi KM, et al. Diffuse soft tissue calcifications
(calcinosis cutis) in patient with discoid lupus erythematosus. Clin Exp Dermatol 1988; 13: 193-6
42. Marzano AV, Kolesnikova LV, Gasparini G, et al. Dystrophic calcinosis cutis in
subacute cutaneous lupus. Dermatology 1999; 90: 90-2
43. Wozniacka A, Robak E, Sysa-Jedrzejowska A, et al. The influence of chloroquine
treatment on minimal erythema dose measurements in systemic lupus erythematosus patients [abstract]. J Invest Dermatol 2002; 3: 763
44. Nishijima C, Hatta N, Inaoki M, et al. Urticarial vasculitis in systemic lupus
erythematosus: fair response to prednisolone/dapsone and persistent hypocomplementemia. Eur J Dermatol 1999; 9: 54-6
45. Malcangi G, Brandozzi G, Giangiacomi M, et al. Bullous SLE: response to
methotrexate and relationship with disease activity. Lupus 2003; 12: 63-6
46. Yung A, Oakley A. Bullous systemic lupus erythematosus. Australas J Dermatol
2000; 41: 234-7
47. Krim E, Noblesse I, Beylot Barry M, et al. Bullous localization of a lupus
erythematosus induced by radiotherapy. Ann Dermatol Venereol 2002; 129:
1307-9
48. Fowler Jr JF, Callen JP. Cutaneous mucinosis associated with lupus erythematosus.
J Rheumatol 1984; 11: 380-3
49. Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus; a
neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch
Dermatol 2000; 136: 1033-41
50. Fox JN, Klapman MH, Rowe L. Lupus profundus in children: treatment with
hydroxychloroquine. J Am Acad Dermatol 1987; 16: 839-44
51. Ziering CL, Rabinowitz LG, Esterly NB. Antimalarials for children: indications,
toxicities, and guidelines. J Am Acad Dermatol 1993; 28: 634-70
52. Magana-Garcia M. Antimalarials for children [letter]. J Am Acad Dermatol 1994;
3: 510
53. Khamashta MA, Buchanan NM, Hughes GR. The use of hydroxychloroquine in
lupus pregnancy: the British experience. Lupus 1996; 5: S65-6
54. Levy RA, Vilela VS, Cataldo MJ, et al. Hydroxychloroquine (HCQ) in lupus
pregnancy: double blind and placebo-controlled study. Lupus 2001; 10: 401-4
Am J Clin Dermatol 2005; 6 (1)
10
55. Costedoat-Chalumeau N, Amoura Z, Duhaut P, et al. Safety of hydroxychloroquine in pregnant patients with connective tissue diseases: a study of one
hundred thirty-three cases compared with a control group. Arthritis Rheum
2004; 50: 3056-7
56. Tett SE, Cutler DJ, Day RO, et al. A dose-ranging study of the pharmacokinetics of
hydroxychloroquine following intravenous administration to healthy volunteers. Br J Clin Pharmacol 1988; 26: 303
57. Petri M. Thrombosis and systemic lupus erythematosus; the Hopkins Lupus Cohort
perspective. Scand J Rheumatol 1996; 25: 191-3
58. Rynes RI. Antimalarials: is re-evaluation needed? J Clin Rheumatol 1998; 4: 50-1
59. Hobbs HE, Eadie SP, Somerville F. Ocular lesions after treatment with chloroquine. Br J Ophthalmol 1961; 45: 284-97
60. Maksymowych W, Russell AS. Antimalarials in rheumatology: efficacy and safety. Semin Arthritis Rheum 1987; 16: 206-21
61. Lozier JR, Friedlaender MH. Complications of antimalarial therapy. Int
Ophthalmol Clin 1989; 29: 172-8
62. Levy GD, Munz SJ, Paschal J, et al. Incidence of hydroxychloroquine retinopathy
in 1207 patients in a large multicenter outpatient practice. Arthritis Rheum
1997; 40: 1482-6
63. Mavrikakis I, Mavrikakis E. Are evidence-based guidelines being followed for the
monitoring of ocular toxicity of hydroxychloroquine? A nationwide survey of
practice amongst consultant rheumatologists and implications for clinical governance. Rheumatology 2004; 43: 1057-8
64. Araiza-Casillas R, Cardenas F, Morales Y, et al. Factors associated with chloroquine-induced retinopathy in rheumatic diseases. Lupus 2004; 13: 621
65. Neubauer AS, Samari-Kermani K, Schaller U, et al. Detecting chloroquine
retinopathy: electro-oculogram versus colour vision. Br J Ophthalmol 2003; 87:
902-8
66. Pluenneke AC, Blomquist PH. Utility of red Amsler grid screening in a rheumatology clinic. J Rheumatol 2004; 31: 1754-5
67. American College of Rheumatology Ad Hoc Committee on Clinical Guidelines.
Guidelines for monitoring drug therapy in rheumatoid arthritis. Arthritis Rheum
1996; 39: 723-31
68. Sontheimer RD. Questions answered and a $1 million question raised concerning
lupus erythematosus tumidus. Arch Dermatol 2000; 136: 1044-9
69. Trenholme GM, Carson PE. Therapy and prophylaxis of malaria. JAMA 1978;
240: 2293-5
70. Custer RP. Aplastic anemia in soldiers treated with Atabrine (quinacrine). Am J
Med Sci 1946; 212: 211-24
71. Zuehlke RL, Lillis PJ, Tice A. Antimalarial therapy for lupus erythematosus: an
apparent advantage of quinacrine. Int J Dermatol 1981; 20: 57-61
72. Schmid I, Anasetti C, Petersen FB, et al. Marrow transplantation for severe
aplastic anemia associated with exposure to quinacrine. Blut 1990; 61: 52-4
73. Ward WQ, Walter-Ryan WG, Shehi GM. Toxic psychosis: a complication of
antimalarial therapy. J Am Acad Dermatol 1985; 12: 863-5
74. Evans RL, Khalid S, Kinney JL. Antimalarial psychosis revisited. Arch Dermatol
1984; 120: 765-7
75. Genel F, Erermis S, Aksu G, et al. Quinacrine-induced psychiatric disturbances in
a child with common variable immunodeficiency and chronic giardiasis. Hum
Psychopharmacol 2002; 17: 357-9
76. Tristano AG, Falcon L, Wilson M, et al. Seizure associated with chloroquine
therapy in a patient with systemic lupus erythematosus. Rheum Int 2004; 24:
315-6
77. Holme SA, Holmes SC. Hydroxychloroquine-induced pruritus. Acta Derm Venereol 1999; 79: 333
78. Jimenez-Alonso J, Tercedor J, Reche I. Antimalarial drugs and pruritus in patients
with lupus erythematosus [letter]. Acta Derm Venereol 2000; 80: 458
79. Evans CC, Bergstresser PR. Acute generalized exanthematous pustulosis precipitated by hydroxychloroquine. J Am Acad Dermatol 2004; 50: 650-1
80. Litt JZ. Litts drug eruption manual. 9th ed. New York: Parthenon Publishing,
2003: 91, 92, 219, 220
81. Wallace DJ. The use of quinacrine (Atabrine) in rheumatic diseases: a re-examination. Semin Arthritis Rheum 1989; 18: 282-97
82. Metayer I, Balguerie X, Courville P, et al. Photodermatosis induced by hydroxychloroquine: 4 cases. Ann Dermatol Venereol 2001; 128: 729-31
2005 Adis Data Information BV. All rights reserved.
Wozniacka & McCauliffe
83. Pelle MT, Callen JP. Adverse cutaneous reactions to hydroxychloroquine are more
common in patients with dermatomyositis than in patients with cutaneous lupus
erythematosus. Arch Dermatol 2002; 138: 1231-3
84. Verny C, Gennes C, Sebastien P, et al. Heart conduction disorders in long-term
treatment with chloroquine: two new cases. Presse Med 1992; 21: 800-4
85. Physicians desk reference. 59th ed. Montvale (NJ): Thomson PDR, 2005: 3008
86. Physicians desk reference. 59th ed. Montvale (NJ): Thomson PDR, 2005: 2984
87. Marquardt K, Albertson TE. Treatment of hydroxychloroquine overdose. Am J
Emerg Med 2001; 19: 420-4
88. Harris L, Downar E, Shaikh NA, et al. Antiarrhythmic potential of chloroquine:
new use for an old drug. Can J Cardiol 1988; 4: 295-300
89. Seidman P, Albertioni F, Beck O, et al. Chloroquine reduces the bioavailability of
methotrexate in patients with rheumatoid arthritis. Arthritis Rheum 1994; 37:
830-3
90. McElnay JC, Sidahmed AM, DArcy PF. Examination of the chloroquine-kaolin
drug absorption interaction using the buccal partitioning model. J Clin Hosp
Pharm 1982; 7: 269-73
91. Ette EI, Brown-Awala EA, Essien EE. Chloroquine elimination in humans: effect
of low-dose cimetidine. J Clin Pharmacol 1987; 27: 813-6
92. Algharably N, Owler D, Lamb JF. The rate of uptake of cardiac glycosides into
human cultured cells and the effects of chloroquine on it. Biochem Pharmacol
1986; 35: 3571-81
93. Sieb JP, Milone M, Engel AG. Effects of the quinoline derivatives quinine,
quinidine, and chloroquine on neuromuscular transmission. Brain Res 1996;
712: 179-89
94. Shieh S, Cohen JL, Lim HW. Management of porphyria cutanea tarda in the setting
of chronic renal failure: a case report and review. J Am Acad Dermatol 2000;
42: 645-52
95. Makin AJ, Wendon J, Fitt S, et al. Fulminant hepatic failure secondary to
hydroxychloroquine. Gut 1994; 35: 569-70
96. Fries JF, Singh G, Lenert L, et al. Aspirin, hydroxychloroquine, and hepatic
enzyme abnormalities with methotrexate in rheumatoid arthritis. Arthritis
Rheum 1990; 33: 1611-9
97. Browning DJ. Hydroxychloroquine and chloroquine retinopathy: screening for
drug toxicity. Am J Opthalmol 2002; 133: 649-56
98. Fox R, Dixon R, Guarrasi V, et al. Treatment of primary Sjogrens syndrome with
hydroxychloroquine: a retrospective, open-label study. Lupus 1996; 5: S31-6
99. Wolf R, Ruocco V. Triggered psoriasis. Adv Exp Med Biol 1999; 455: 221-5
100. Stein M, Bell MJ, Ang LC. Hydroxychloroquine neuromyotoxicity. J Rheumatol
2000; 27: 2927-31
101. Desta M, Tadesse A, Gebre N, et al. Controlled trial of hydroxychloroquine in
schizophrenia. J Clin Psychopharmacol 2002; 22: 507-10
102. Wozniacka A, Carter A, McCauliffe DP. Antimalarials in cutaneous lupus erythematosus: mechanisms of therapeutic benefit. Lupus 2002; 11: 71-81
103. Landewe RB, Miltenburg AM, Breedveld FC, et al. Cyclosporine and chloroquine
synergistically inhibit the interferon-gamma production by CD4 positive and
CD8 positive synovial T cell clones derived from a patient with rheumatoid
arthritis. J Rheumatol 1992; 19: 1353-7
104. Salmeron G, Lipsky PE. Immunosuppressive potential of antimalarials. Am J Med
1983; 18: 19-24
105. Sjolin-Forsberg G, Berne B, Eggelte TA, et al. In situ localization of chloroquine
and immunohistological studies in UVB-irradiated skin of photosensitive patients. Acta Derm Venereol 1995; 75: 228-31
106. Olczyk K, Drozdz M, Kucharz E, et al. Studies on the activity of selected
lysosomal exoglycosidases in patients with systemic lupus erythematosus. Med
Interne 1984; 22: 221-5
107. Fox R. Anti-malarial drugs: possible mechanisms of action in autoimmune disease
and prospects for drug development. Lupus 1996; 5: S4-S10
108. Ruzicka T, Printz M. Arachidonic acid metabolism in guinea pig skin: effects of
chloroquine. Agents Actions 1982; 12: 527-9
109. Sperber K, Quraishi H, Kalb TH, et al. Selective regulation of cytokine secretion
by hydroxychloroquine: inhibition of interleukin 1 alpha (IL-1) and IL-6 in
human monocytes and T cells. J Rheumatol 1993; 20: 803-8
110. Housman TS, Jorizzo JL, McCarty MA, et al. Low-dose thalidomide therapy for
refractory cutaneous lesions of lupus erythematosus. Arch Dermatol 2003; 139:
50-4
Am J Clin Dermatol 2005; 6 (1)
Antimalarial Treatment of Cutaneous Lupus Erythematosus
111. Kanekura T, Yoshii N, Terasaki K, et al. Efficacy of topical tacrolimus for treating
the malar rash of systemic lupus erythematosus. Br J Dermatol 2003; 148: 3536
112. Yoshimasu T, Ohtani T, Sakamoto T, et al. Topical FK506 (tacrolimus) therapy
for facial erythematous lesions of cutaneous lupus erythematosus and dermatomyositis. Eur J Dermatol 2002; 12: 50-2
113. Gerdsen R, Wenzel I, Uerlich M, et al. Successful treatment of chronic discoid
lupus erythematosus of the scalp with imiquimod. Dermatology 2002; 205:
416-8
114. Lampropoulos CE, Sangle S, Harrison P, et al. Topical tacrolimus therapy of
resistant cutaneous lesions in lupus erythematosus: a possible alternative.
Rheumatology (Oxford) 2004; 43 (11): 1383-5
115. Kreuter A, Gambichler T, Breuckmann F, et al. Pimecrolimus 1% cream for
cutaneous lupus erythematosus. J Am Acad Dermatol 2004; 51 (3): 407-10
116. Hall RP, Lawley TJ, Smith HR, et al. Bullous eruption of systemic lupus
erythematosus: dramatic response to dapsone therapy. Ann Intern Med 1982;
97: 165-70
117. Tsutsui K, Imai T, Hatta N, et al. Widespread pruritic plaques in a patient with
subacute cutaneous lupus erythematosus and hypocomplementemia: response
to dapsone therapy. J Am Acad Dermatol 1996; 35: 313-5
118. Neri R, Mosca M, Bernacchi E, et al. A case of SLE with acute, subacute and
chronic cutaneous lesions successfully treated with Dapsone. Lupus 1999; 8:
240-3
119. Shornick JK, Formica N, Parke AL. Isotretinoin for refractory lupus erythematosus. J Am Acad Dermatol 1991; 24: 49-52
2005 Adis Data Information BV. All rights reserved.
11
120. Ruzicka T, Sommerburg C, Goerz G, et al. Treatment of cutaneous lupus
erythematosus with acitretin and hydroxychloroquine. Br J Dermatol 1992;
127: 513-8
121. Arbiser JL, Moschella SL. Clofazimine: A revive of its medical uses and mechanisms of action. J Am Acad Dermatol 1995; 32: 241-7
122. Tsokos GC, Caughman SW, Kleppel JH. Successful treatment of generalized
discoid skin lesions with azathioprine. Arch Dermatol 1985; 121: 1323-5
123. Boehm IB, Boehm GA, Bauer R. Management of cutaneous lupus erythematosus
with low-dose methotrexate: indication for modulation of inflammatory mechanisms. Rheumatol Int 1998; 18: 59-62
124. Bohm I, Uerlich M, Bauer R. Rapid improvement of subacute cutaneous lupus
erythematosus with low-dose methotrexate. Dermatology 1997; 194: 307-8
125. Peter RU, Ruzicka T. Cyclosporin A in the therapy of inflammatory dermatoses.
Hautarzt 1992; 43: 687-4
126. Dalziel K, Going G, Cartwright PH, et al. Treatment of chronic discoid lupus
erythematosus with an oral gold compound (auranofin). Br J Dermatol 1986;
115: 211-6
Correspondence and offprints: Dr Daniel P. McCauliffe, Rutland Skin
Center, 3 Mahoney Avenue, Rutland, VT 05701, USA.
E-mail: dpmccauliffe@juno.com
Am J Clin Dermatol 2005; 6 (1)
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Vedic Astrology OverviewDocument1 pageVedic Astrology Overviewhuman999100% (8)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Development of The FaceDocument76 pagesDevelopment of The Facedr parveen bathla100% (1)
- Vital Signs Reference Chart - 1Document1 pageVital Signs Reference Chart - 1l10n_assNo ratings yet
- Lubchenco Curve PDFDocument1 pageLubchenco Curve PDFWarren Lie25% (4)
- Surface Roughness Measurement - MitutoyoDocument2 pagesSurface Roughness Measurement - MitutoyoSelvaraj BalasundramNo ratings yet
- Schneider Power Supply PhaseoDocument26 pagesSchneider Power Supply PhaseoScott EnnisNo ratings yet
- Manual de Uso Ecografo GE Logiq e PDFDocument192 pagesManual de Uso Ecografo GE Logiq e PDFDaniel CortesNo ratings yet
- Hart Transmitter Calibration: Application NoteDocument8 pagesHart Transmitter Calibration: Application NoteThulasi Raman KowsiganNo ratings yet
- Specimen 1 ValuationDocument17 pagesSpecimen 1 ValuationLight BearerNo ratings yet
- Analytical Methods To Measure The Constants of Fats and OilsDocument5 pagesAnalytical Methods To Measure The Constants of Fats and OilsPenicillium Notatum67% (3)
- Toaz - Info Chemtech Reviewer PRDocument1 pageToaz - Info Chemtech Reviewer PRchristy janioNo ratings yet
- Callen2009 Clinically Relevant InformationDocument4 pagesCallen2009 Clinically Relevant Informationl10n_assNo ratings yet
- BMI Chart for Boys Ages 5-19Document1 pageBMI Chart for Boys Ages 5-19Justitia LantuNo ratings yet
- Beverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug InteractionsDocument1 pageBeverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug Interactionsl10n_assNo ratings yet
- Classification of Cutaneous LupusDocument5 pagesClassification of Cutaneous Lupusl10n_assNo ratings yet
- TABLE Boys 3mo To 5yr TRICEPSage PercentileDocument2 pagesTABLE Boys 3mo To 5yr TRICEPSage Percentilel10n_assNo ratings yet
- Jurnal Kriteria Baru SleDocument10 pagesJurnal Kriteria Baru SleDr Edi HidayatNo ratings yet
- Callen2004 Update On The Management of Cutaneous Lupus ErythematosusDocument6 pagesCallen2004 Update On The Management of Cutaneous Lupus Erythematosusl10n_assNo ratings yet
- Boeck Ler 2009Document5 pagesBoeck Ler 2009l10n_assNo ratings yet
- Z Score BMI 5-19yearsold Label GirlDocument1 pageZ Score BMI 5-19yearsold Label GirlVienny Widhyanti RosaryaNo ratings yet
- F E T C: Luid AND Lectrolyte Herapy IN HildrenDocument12 pagesF E T C: Luid AND Lectrolyte Herapy IN HildrenHartantoRezaGazaliNo ratings yet
- Temperature MeasurementDocument5 pagesTemperature Measurementl10n_ass100% (1)
- NPPA040112 DecisiontreeDocument1 pageNPPA040112 Decisiontreel10n_assNo ratings yet
- Weight gain by birth weight and age groups for boysDocument1 pageWeight gain by birth weight and age groups for boysl10n_assNo ratings yet
- Bmi For Age Z-ScoreDocument1 pageBmi For Age Z-ScoreTisha Patricia OedoyNo ratings yet
- Bmifa Boys Z 5 19 LabelsDocument1 pageBmifa Boys Z 5 19 LabelssufigueiraNo ratings yet
- GCS PDFDocument1 pageGCS PDFFrincia100% (1)
- CSFDocument1 pageCSFl10n_assNo ratings yet
- PDFDocument1 pagePDFl10n_assNo ratings yet
- CHT Acfa Boys Z 3 5Document1 pageCHT Acfa Boys Z 3 5Rivadin NurwanNo ratings yet
- PDFDocument1 pagePDFl10n_assNo ratings yet
- CSFDocument1 pageCSFl10n_assNo ratings yet
- Dahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory EpilepsyDocument11 pagesDahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory Epilepsyl10n_assNo ratings yet
- Cunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic DietDocument5 pagesCunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic Dietl10n_assNo ratings yet
- Cross2013 New Research With Diets and EpilepsyDocument6 pagesCross2013 New Research With Diets and Epilepsyl10n_assNo ratings yet
- Brodie2005 Diagnosing and Predicting Refractory EpilepsyDocument4 pagesBrodie2005 Diagnosing and Predicting Refractory Epilepsyl10n_assNo ratings yet
- Best2000 Cardiac Complications in Pediatric Patients On The Ketogenic DietDocument3 pagesBest2000 Cardiac Complications in Pediatric Patients On The Ketogenic Dietl10n_assNo ratings yet
- Bough2007 Anticonvulsant Mechanisms of The Ketogenic DietDocument16 pagesBough2007 Anticonvulsant Mechanisms of The Ketogenic Dietl10n_assNo ratings yet
- ParikalpDocument43 pagesParikalpManish JaiswalNo ratings yet
- Operational Transconductance Amplifier ThesisDocument6 pagesOperational Transconductance Amplifier ThesislaurahallportlandNo ratings yet
- Student Pilot GuideDocument13 pagesStudent Pilot GuideAŞKIN FIRATNo ratings yet
- MC BreakdownDocument5 pagesMC BreakdownThane SnymanNo ratings yet
- DOCUMENT guides the way with VLB-44 LED Marine BeaconDocument4 pagesDOCUMENT guides the way with VLB-44 LED Marine BeaconbenNo ratings yet
- 3-Ph Induction MotorDocument246 pages3-Ph Induction MotorAn00pgadzillaNo ratings yet
- 43-101 Technical Report Quimsacocha, February 2009Document187 pages43-101 Technical Report Quimsacocha, February 2009Marco Vinicio SotoNo ratings yet
- Motherboards Tuf z270 Mark 2Document70 pagesMotherboards Tuf z270 Mark 2Jonah HexNo ratings yet
- ElectrochemistryDocument24 pagesElectrochemistryZainul AbedeenNo ratings yet
- Unchained MelodeeDocument93 pagesUnchained MelodeeRafael Cornholio RodriguezNo ratings yet
- Nordtest Method NT Fire 049Document16 pagesNordtest Method NT Fire 049mail2021No ratings yet
- Masterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyDocument35 pagesMasterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyDemerson CamposNo ratings yet
- Resultados de La Web: GDDS - Traducción Al Español - Ejemplos Inglés - Reverso ..Document3 pagesResultados de La Web: GDDS - Traducción Al Español - Ejemplos Inglés - Reverso ..Jo PaterninaNo ratings yet
- Personal Care Na Hair GuideDocument8 pagesPersonal Care Na Hair GuideIsabellaNo ratings yet
- Discrete Variable Probability Distribution FunctionsDocument47 pagesDiscrete Variable Probability Distribution FunctionsJanine CayabyabNo ratings yet
- Mast Bending Stress Calculation: Antenna 1Document6 pagesMast Bending Stress Calculation: Antenna 1Vinay KumarNo ratings yet
- WIP CaseStudyDocument3 pagesWIP CaseStudypaul porrasNo ratings yet
- Pitfalls of HIV Infection - Dr. Rizqi Amalia, Sp.ADocument46 pagesPitfalls of HIV Infection - Dr. Rizqi Amalia, Sp.AandreknhNo ratings yet
- 2017 Scoring Materials Math g6Document119 pages2017 Scoring Materials Math g6KRANo ratings yet
- Sing 2Document64 pagesSing 2WindsurfingFinnNo ratings yet
- 5 - Flight Recorder - OcrDocument19 pages5 - Flight Recorder - OcrtmhoangvnaNo ratings yet