Professional Documents
Culture Documents
SOAPNoteSOS MSBlankForm PDF
Uploaded by
NahjarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SOAPNoteSOS MSBlankForm PDF
Uploaded by
NahjarCopyright:
Available Formats
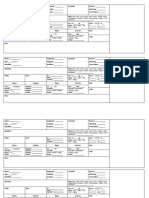
Outpatient Health Summary
Patients Name
Date of Birth
Marital Status:
M
Significant Others:
Sex
S
Family
History:
Employment
Tobacco
Phone Numbers:
DNR Status:
Resuscitate?
Next of Kin:
Religion:
Social
History:
wak SOS version 5:091102b
Date
Update:
Home
Work
Yes
Occupation
Qualifications:
Education
ETOH
M
F
No
Drugs
Siblings
Sex Hx
Others:
Past Medical History
CPT#
Start Date
Problem / Diagnosis
Medications
Start
Stop
Allergies, Adverse Drug Reactions:
Health Maintenance
Parameter
Dates
DPT/DT/TD
OPV
MMR
HIB
Influenza
Hepatitis
PPD/Tine
Pneumovax
H&P
Eye exam
Dental exam
PAP smear
Mammogram
Urinalysis
Hemoccult
Cholesterol
Sigmoidoscopy
Others
Funded by a grant from the Bureau of Research. 2002 American Academy of Osteopathy.
Designed to coordinate with the Established Outpatient Osteopathic SOAP Note Form. Recommended by American Association of Colleges of Osteopathic Medicine.
Past Surgical History
Date
Type
Consultants
Outpatient Osteopathic SOS History/Exam Form
Patients Name _______________________________
wak SOS version 5:091102b
Office of:
For office
use only:
Date________________
HISTORY
(See Outpatient Health Summary Form for details of history)
Patients Pain Analog Scale: � Not done
NO PAIN
WORST POSSIBLE PAIN
CC
E l e m e n t s
History of Present Illness
Status of 3 chronic
Location
Quality
Severity
_______________________
Duration
_______________________
Timing
_______________________
Context
Modifying factors
Assoc. Signs and Sx
OR
or inactive conditions
Review of Systems (Only ask / record those systems pertinent for this encounter.) � Not done
�
�
�
�
�
�
�
�
�
�
�
�
�
�
Level: ROS
Constitutional (Wt loss, etc.)
Eyes
Ears, nose, mouth, throat
Cardiovascular
Respiratory
Gastrointestinal
Genitourinary
Musculoskeletal
Integumentary (skin, breast)
Neurological
Psychiatric
Endocrine
Hematologic/lymphatic
Allergic/immunologic
Past Medical, Family, Social History
�
Past History / Trauma
�
�
Family History
Social History
�
II
None
III
1 system pertinent
to the problem
�
�
IV
V
2-9 systems
10 systems
Level: PFSH
II
None
�
III
IV 1 history area
�
2 history areas
V
�
� Not done
Overall History = Average of HPI, ROS or PFSH:
Level: HPI
II
1-3 elements reviewed
�
III
IV 4 elements OR status
�
V of 3 chronic conditions
II
( 1-3 HPI )
� III
( 1-3 HPI, 1 ROS )
� IV
(4+ HPI, 2-9 ROS, 1 PFSH)
(4+ HPI, 10+ ROS, 2+ PFSH)
Signature of transcriber: ______________________________
Signature of examiner: ___________________________________
Funded by a grant from the Bureau of Research. 2002 American Academy of Osteopathy.
Designed to coordinate with the Established Outpatient Osteopathic SOAP Note Form. Recommended by American Association of Colleges of Osteopathic Medicine.
(Page 1 of 3)
Outpatient Osteopathic SOS Musculoskeletal Exam Form
wak SOS version 5:091102b
� Not done
Patients Name ______________________
Date ________
Sex: Male �
Female �
Age _____
* Vital Signs (3 of 7)
Wt. ____________
Ht. ______________
Temp. _________
Reg. �
Pt. position for recording BP:
Resp. ____
Pulse ____
Irreg. �
Standing________ Sitting________ Lying__________
* Gait and Station:
Notes
Body
�
Endo.
Type:
Posture:
Excl. �
Gait: Symmetrical
Meso.
Fair
�
Ecto.
Poor
�
Asymmetrical
I
N
Ant./Post. Spinal Curves:
Cervical Lordosis
�
�
Thoracic Kyphosis
�
�
Lumbar Lordosis
�
�
I = increased; N = normal; D = decreased
*1
*2
*3
*4
*5
*6
�
�
�
Skin:
Head / neck
Trunk
N
�
�
Reflexes:
Biceps L
R
Triceps L
R
Brachio- L
Radialis R
0
�
�
�
�
�
�
Methods Used For
Examination
All T
A
R
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
L. upper extremity
R. upper extremity
1
�
�
�
�
�
�
T
�
�
�
�
�
�
�
�
�
�
�
�
�
�
2
�
�
�
�
�
�
3
�
�
�
�
�
�
4
�
�
�
�
�
�
�
�
�
�
Patella
Horizontal Planes
�
�
Ab
�
�
L
R
Achilles L
R
Babinski L
R
Key to the
Severity Scale
Region
Evaluated
Head and Face
Neck
Thoracic T1-4
T5-9
T10-12
Ribs
Lumbar
Sacrum / Pelvis
Pelvis / Innom.
Abd ./ Other
Upper
R
Extremity L
Lower
R
Extremity L
Signature of transcriber: ________________________
* Gen. Appearance:
�
�
D
�
�
Ab
�
�
For office
use only:
Scoliosis (Lateral Spinal Curves):
None
Sitting
�
Functional
Standing
�
Mild
Prone/Supine
�
Moderate
Unable to Examine
�
Severe
�
Right: 1/8 �
Short leg?
Equal �
Left: 1/8 �
N
�
�
Office of:
N
�
�
L. lower extremity
R. lower extremity
0
�
�
�
�
up
up
1
�
�
�
�
�
�
2
3
�
�
�
�
�
�
�
�
down
down
4
�
�
�
�
�
�
Ab
�
�
Motor:
C5 L
R
C6 L
R
C7 L
R
C8 L
R
1
�
�
�
�
�
�
�
�
2
�
�
�
�
�
�
�
�
3
�
�
�
�
�
�
�
�
4
�
�
�
�
�
�
�
�
Normal
�
*Cardiovascular
Observation normal
�
Palpation normal
�
*Lymphatics
No palpable nodes
�
*Neurologic and Psychiatric:
Coordination intact
�
Sensory intact
�
Mental status
Oriented:
In time
�
In person
�
In place
�
Good mood/ affect
�
Level of SOS
�
�
II
III
1-5 elements
IV
12+ elements for
musculoskeletal Exam
Perform all * elements
5
�
�
�
�
�
�
�
�
T1 L
R
L4 L
R
L5 L
R
S1 L
R
1
�
�
�
�
�
�
�
�
2
�
�
�
�
�
�
�
�
3
�
�
�
�
�
�
�
�
4
�
�
�
�
�
�
�
�
__________________________________________________
Funded by a grant from the Bureau of Research. 2002 American Academy of Osteopathy.
Designed to coordinate with the Established Outpatient Osteopathic SOAP Note Form. Recommended by American Association of Colleges of Osteopathic Medicine.
�
�
�
�
�
�
�
6+ elements
0 = No SD or background (BG) levels
2 = Obvious TART (esp. R and T), +/- symptoms
1 = More than BG levels, minor TART
3 = Key lesions, symptomatic, R and T stand out
Severity
Somatic Dysfunction and Other Systems
MS / SNS / PNS / LYM. / CV / RESP. / GI / FAS. / etc.
0 1
2 3
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
Signature of examiner:
�
�
(Page 2 of 3)
5
�
�
�
�
�
�
�
�
Outpatient Osteopathic Assessment and Plan Form
A
Patients Name
Dx No.
________________________________
739.0
739.1
739.2
739.8
739.3
Dx No.
� All not done
Region
739.4
739.5
739.9
739.7
739.6
First visit
Y
�
�
�
�
�
�
�
�
�
�
�
�
N
�
�
�
�
�
�
�
�
�
�
�
�
Resolved
OMT
Head and Face
Neck
Thoracic T1-4
T5-9
T10-12
Ribs
Lumbar
Sacrum
Pelvis
Abdomen/Other
Upper Extremity
Lower Extremity
Written Diagnosis
ICD Code
Somatic Dysfunction of Head and Face
Somatic Dysfunction of Neck
Somatic Dysfunction of Thoracic
Somatic Dysfunction of Ribs
Somatic Dysfunction of Lumbar
Physicians evaluation of patient prior to treatment:
___________________________
Date
Written Diagnosis
ICD Code
wak SOS version 5: 5:091102b
Office of:
For office
use only:
Somatic Dysfunction of Sacrum
Somatic Dysfunction of Pelvis
Somatic Dysfunction of Abd / Other
Somatic Dysfunction of Upper Extremity
Somatic Dysfunction of Lower Extremity
�
Improved
Unchanged
Treatment Method
ART
BLT
�
�
�
�
�
�
�
�
�
�
�
�
CR
�
�
�
�
�
�
�
�
�
�
�
�
CS
�
�
�
�
�
�
�
�
�
�
�
�
Response
DIR
FPR
HVLA
IND
INR
LAS
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
Meds:
PT:
Exercise:
Other:
Worse
ME
MFR
�
�
�
�
�
�
�
�
�
�
�
�
ST
�
�
�
�
�
�
�
�
�
�
�
�
VIS
�
�
�
�
�
�
�
�
�
�
�
�
OTH
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
�
R
�
�
�
�
�
�
�
�
�
�
�
�
I
�
�
�
�
�
�
�
�
�
�
�
�
U
�
�
�
�
�
�
�
�
�
�
�
�
W
�
�
�
�
�
�
�
�
�
�
�
�
Nutrition:
Complexity / Assessment / Plan (Scoring) *Default to level 2same criteria
Problems
Self-limiting
Established problem improved / stable
Establishedworsening
Newno workup
New additional workup
Level I
Risk: (Presenting problem(x), diagnostic procedures(s), and
management options)
Minimal = Min.
Low
Moderate = Mod.
High
Minimal = Min.
1 (2 max.)
1
2
3 (1 max.)
4
Level II
Level III
Level IV
Level V
1 pt.
�
2 pt.
�
3 pt.
�
4 pt.
�
Requires 3 of above 3 (problems, risk and data).
Level I
Level II
Level III
Level IV
Level V
Min.
�
Low
�
Mod.
�
High
�
Data
Lab
Radiology
Medicine
Discuss with performing physician
Obtain records or Hx from others
Review records, discuss with physician
Visualization of tracing, specimen
Level I
Level II
Level III
1 pt.
�
2 pt.
�
Level IV
Maximum Points
1
1
1
1
1
2
2
Level V
3 pt.
�
4 pt.
�
Level of complexity = average of included areas.
Optional MethodCoding by Time
Traditional MethodCoding by Components
When majority of the encounter is counseling / coordinating, the level is determined by total time
History
Examination
Complexity /
Assessment Plan
II
III
IV
II
III
IV
Final level of service
II
III
IV
New patients (minutes)
10
15
25
40
60
OMT performed as Above:
0 areas
CPT Codes:
Other Procedures
Written Dx:
Performed:
E/M Code:
New
�
�
�
Write 992 plus . . .
02
03
04
�
Follow-up:
1-2 areas
�
05
IV
45
60
10
15
25
40
Dictate total time and counseling / coordinating time plus a brief description of topics discussed
>60
III
30
Final level of service
All three areas required. Average of the three equals level of service.
Minutes spent
with the patient:
II
20
Outpatient patients (minutes)
I
10
EST
...
Signature of transcriber: _________________________________
�
11
10
11
12
3-4 areas
�
12
�
13
Signature of examiner:
5-6 areas
�
14
�
15
Units:
7-8 areas
Consults
...
�
41
PRN
9-10 areas
�
42
�
43
�
44
�
45
____________________________________________
Funded by a grant from the Bureau of Research. 2002 American Academy of Osteopathy.
Designed to coordinate with the Established Outpatient Osteopathic SOAP Note Form. Recommended by American Association of Colleges of Osteopathic Medicine.
(Page 3 of 3)
You might also like
- All My Test Results are Normal: A Smart Guide to Testing for Chronic Fatigue SyndromeFrom EverandAll My Test Results are Normal: A Smart Guide to Testing for Chronic Fatigue SyndromeRating: 2.5 out of 5 stars2.5/5 (2)
- Physician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideFrom EverandPhysician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideNo ratings yet
- Nursing Care Plan FormatDocument4 pagesNursing Care Plan Formatprince242653100% (1)
- 2.physical E, HISTORY NCPDocument13 pages2.physical E, HISTORY NCPمريم حجيNo ratings yet
- Patient Assessment FormDocument26 pagesPatient Assessment FormjajsdjajdaNo ratings yet
- 2017 Certificate of Health 1Document2 pages2017 Certificate of Health 1herman syahNo ratings yet
- Medical FormDocument2 pagesMedical FormJane WilliamNo ratings yet
- IDCAP Clinical Assessment ToolsDocument4 pagesIDCAP Clinical Assessment ToolsIDCAP2011100% (1)
- Pre-Employment Medical FormDocument2 pagesPre-Employment Medical FormSourin NandiNo ratings yet
- Medical Certificate of Fitness: To Be Filled by CandidateDocument2 pagesMedical Certificate of Fitness: To Be Filled by CandidatevenkatNo ratings yet
- ANTENATAL Assessment FINALDocument12 pagesANTENATAL Assessment FINALM. jehovah Nissie YeshalomeNo ratings yet
- Ministry of Higher Education Malaysia Medical Report Part 1: Health Declaration Part 2: Medical Examination FormDocument5 pagesMinistry of Higher Education Malaysia Medical Report Part 1: Health Declaration Part 2: Medical Examination FormSantiago MoranNo ratings yet
- Nurse Report Sheet OriginalDocument2 pagesNurse Report Sheet Originalhvera01No ratings yet
- Graduate SOAP NOTE TEMPLATEDocument7 pagesGraduate SOAP NOTE TEMPLATEMiley MunozNo ratings yet
- 01.17bmQT10 Health Examination ReportDocument6 pages01.17bmQT10 Health Examination ReportKita 09No ratings yet
- History and Physical Examination Checklist PDFDocument10 pagesHistory and Physical Examination Checklist PDFgietsche_gelNo ratings yet
- Neuroscience Physical Therapy Evaluation FormDocument7 pagesNeuroscience Physical Therapy Evaluation FormTaral PatelNo ratings yet
- Mini SBAR Report SheetDocument3 pagesMini SBAR Report Sheetthe201girlsNo ratings yet
- 355 - 132243 - 2012-2013 Application-FullDocument3 pages355 - 132243 - 2012-2013 Application-FullElie ShalhoubNo ratings yet
- MED-F-018 OPD-Dentist Assessment PEADSDocument3 pagesMED-F-018 OPD-Dentist Assessment PEADSdrakmalik71No ratings yet
- Medical Fitness Form PDFDocument4 pagesMedical Fitness Form PDFKartikeya BagraNo ratings yet
- Graduate PDFDocument2 pagesGraduate PDFTrieu LeNo ratings yet
- Clinical Log BookDocument14 pagesClinical Log Booklecturio100% (2)
- Patients ChartDocument1 pagePatients ChartLovely HackeyNo ratings yet
- Physical Examination Form: Return by July 17ThDocument1 pagePhysical Examination Form: Return by July 17ThFlorian Ananias ByarugabaNo ratings yet
- Clinical Paperwork 2014-2015Document8 pagesClinical Paperwork 2014-2015AmandaNicholsNo ratings yet
- Nursing Health Assessment Guide: San Pedro CollegeDocument3 pagesNursing Health Assessment Guide: San Pedro CollegeRue Cheng MaNo ratings yet
- Nursing Health Assessment Guide: San Pedro CollegeDocument3 pagesNursing Health Assessment Guide: San Pedro CollegeKim ZNo ratings yet
- Initial Patient Assessment FormDocument3 pagesInitial Patient Assessment FormFrederickKalangieNo ratings yet
- Lasustech Medical FormDocument2 pagesLasustech Medical FormAl MubarakNo ratings yet
- Ghid de AnamnezaDocument5 pagesGhid de AnamnezaOtilia PavalNo ratings yet
- DAAD - Health CertificateDocument2 pagesDAAD - Health Certificaterosenrot1100% (2)
- Physical Examination Form: Return by July 15Th:: ThisDocument1 pagePhysical Examination Form: Return by July 15Th:: ThisLinh HoangNo ratings yet
- Medical ReportDocument1 pageMedical Reportwhit.ehouseboyquantiumNo ratings yet
- Comprehensive H&PDocument2 pagesComprehensive H&PjwwisnerNo ratings yet
- Nursing Nursing Care PlanDocument15 pagesNursing Nursing Care Planyourmom111No ratings yet
- Medical Examintation Report: Document No MTIPL/HR/F0006 1Document1 pageMedical Examintation Report: Document No MTIPL/HR/F0006 1Kabir ShelkeNo ratings yet
- Forms For DuanJunhongDocument1 pageForms For DuanJunhongSean YanNo ratings yet
- NB AssessmentDocument6 pagesNB AssessmentstephanyNo ratings yet
- Obstetrics History General DataDocument7 pagesObstetrics History General DataColeen NeyraNo ratings yet
- 7.8 Collect Data & Come Up With Plan For Day & Nursing Diagnosis Pre-Conference 8-9 Vitals Then Chart, AM Care, StartDocument2 pages7.8 Collect Data & Come Up With Plan For Day & Nursing Diagnosis Pre-Conference 8-9 Vitals Then Chart, AM Care, StartSade' CovingtonNo ratings yet
- Medical History FormDocument5 pagesMedical History FormgaloperiscolNo ratings yet
- Pediatric Assessment (1 - 12)Document11 pagesPediatric Assessment (1 - 12)Rose Ann Salanap80% (5)
- GORDON and PADocument3 pagesGORDON and PAAirglow GNo ratings yet
- Assessment ToolDocument5 pagesAssessment ToolNaneth CadisalNo ratings yet
- Patient Assessment SheetsDocument4 pagesPatient Assessment Sheetsblaktrac0% (1)
- History Taking FormDocument2 pagesHistory Taking FormMaria Santiago100% (1)
- Sbar 2Document2 pagesSbar 2Nurse Betty100% (3)
- Student Athlete ParticipationDocument4 pagesStudent Athlete Participationlhmiles2No ratings yet
- Pre-Employment Medical Examination Cum Fitness CertificateDocument7 pagesPre-Employment Medical Examination Cum Fitness CertificateAshutosh PathakNo ratings yet
- Weekly Clinical Prep Packet 12 REVISEDDocument12 pagesWeekly Clinical Prep Packet 12 REVISEDMei SarteNo ratings yet
- MedSurg SBARDocument2 pagesMedSurg SBARduaalipa18No ratings yet
- Tex Cuestionario SaludDocument2 pagesTex Cuestionario SaludRaul ParsivalNo ratings yet
- Central Mindanao University College of Nursing Preschool Assessment FormDocument6 pagesCentral Mindanao University College of Nursing Preschool Assessment FormKyleRepolidon MoralesNo ratings yet
- Nurse 360 CapstoneDocument21 pagesNurse 360 Capstoneapi-302588274No ratings yet
- Document Developed by Developmental-Behavioral Pediatrics Lucile Packard Children's Hospital at Stanford Last Update 10/08/13Document6 pagesDocument Developed by Developmental-Behavioral Pediatrics Lucile Packard Children's Hospital at Stanford Last Update 10/08/13TanFransisca DianNo ratings yet
- Medicare Patient Health Risk AssessmentDocument2 pagesMedicare Patient Health Risk AssessmentShobhitNo ratings yet
- Medical Cer Ficate of Fitness: To Be Filled by CandidateDocument2 pagesMedical Cer Ficate of Fitness: To Be Filled by CandidateDINESH CHANDRA GANNAVARAPUNo ratings yet
- Frailty Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandFrailty Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Exercise Physiology for the Pediatric and Congenital CardiologistFrom EverandExercise Physiology for the Pediatric and Congenital CardiologistNo ratings yet
- Past Medical History: Wak SOS Version 5:091102bDocument4 pagesPast Medical History: Wak SOS Version 5:091102bNahjarNo ratings yet
- Medical Reconciliation Form: Name: Source of InformationDocument1 pageMedical Reconciliation Form: Name: Source of InformationmutiaNo ratings yet
- WHO Guidelines Hand Hygiene in Health CareDocument270 pagesWHO Guidelines Hand Hygiene in Health CareÐr Salma100% (1)
- WHO Guidelines Hand Hygiene in Health CareDocument270 pagesWHO Guidelines Hand Hygiene in Health CareÐr Salma100% (1)
- Automatic Stop Order Univ Kentucky hospitalPH04-04 PDFDocument1 pageAutomatic Stop Order Univ Kentucky hospitalPH04-04 PDFNahjarNo ratings yet
- Automatic Stop Order Univ Kentucky hospitalPH04-04 PDFDocument1 pageAutomatic Stop Order Univ Kentucky hospitalPH04-04 PDFNahjarNo ratings yet
- Helping Babies Breathe Guide 2011Document74 pagesHelping Babies Breathe Guide 2011Prio Sapto UtomoNo ratings yet
- Infant and Young Child FeedingDocument173 pagesInfant and Young Child FeedingNahjarNo ratings yet