Professional Documents
Culture Documents
Tuberculosis
Uploaded by
JayricDepalobosCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tuberculosis
Uploaded by
JayricDepalobosCopyright:
Available Formats
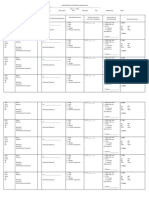
[PHYSIOLOGY LECTURE DR.
REVILLA]
TUBERCULOSIS: Physiologic consideration
Non-immunologic defenses
Cell Mediated Immunity
2 Major types:
1. Primary TB (Primary complex)- due to
underdeveloped immune system; usually
not infectious in nature (children)
2. Post-primary/Secondary TB/ Adult TB
INTRODUCTION:
Problem with management of TBdiscovery to
development (notorious for causing death)past (drug for 12
mos but poor compliance); present (6 mos for TB/made
available to people for FREE)yet people still develop TB due
to culture (when signs and symptoms are reduced, they stop
taking the medication)development of DOTS (Directly
observed treatment shortcourse) where in the patient will take
the drug in front of the health care giver and monitored
weekly.
INFECTION AND MACROPHAGE INVASION:
Once it is not cleared by the mucociliary
system, Mtb reaches the alveoli
Alveolar macrophages phagocytize the bacilli
called PHAGOSOMES (alveolar
macrophage with Mtb inside)
Lipoarabinomannan prevents the killing
*some are killed, some are not
Not killed Replication begins and
macrophage eventually rupturesgoes to
other area of lungs
Since they are AEROBICwant more oxygen
live in area with high oxygen tension (APEX of
the lungs because alveoli in this area is always
distended)
TUBERCULOSIS:
Scourge of mankind for thousand of years
Remains one of the largest problem in the world
Estimated 9 million cases a year
At least 2 million deaths a year
Philippines: 9th among 22 high burden countries
#6th among causes of morbidity and mortality
75 Filipinos die daily
Estimated 240,000 new cases annually
Approximately 15M Filipinos have TB
60% of Filipinos are exposed to TB
HOST RESPONSE & GRANULOMA FORMATION:
Mycobacterial CHONMMP9 (matrix
metalloproteinases 9)stimulate nave macrophage
granuloma formation/TB granuloma
2-4 weeks after infection, 2 host responses to Mtb
development:
1. CMI (Cell Mediated Immunity) response
-activated macrophage neutralizes tubercle
bacilli
-2 things happen:
a) early solid necrosis in the center of tubercle
CASEATION NECROSIS (cheese-like)
b) other viable bacilli may remain DORMANT
**if exposed = only 10-15% develop into disease
(unless: smokers,drinking ROH, sleeping less,
DM, HIV due to less CMI and t-cells CD4, CD8)
**if IMMUNOCOMPROMISEdormant to active
Mtb RELAPSE
2. Delayed-type Hypersensitivity (DTH)
-tissue damaging effect lesion enlarges and
tissue is progressively damage
-caseous material liquefiescavity ( bacilli in
center)
-cavitary Tb: most deadly
-single cavity lesion= 3,000 bacilli
-serves as the basis for TST (Tubercle skin test)
positive due to T cell present in that area of the
skin)
GLOBAL EMERGENCY :needs other people to combat TB
Mycobacterium TB
Rod-shaped, non-spore forming
Importantt:
a. Thin; aerobic loves lung tissue
b. measuring 0.5microns by 3 microns (able to deposit
to alveoli)
acid-fast bacilli- due to failure to decolorized with acid
ROH; cell wall contains mycolic acid
cell wall contains:
a. arabinogalactan and peptidoglycan- makes cell wall
impermeable difficult to treat need more drugs
to destroy bacilli
*** Drugs
Rifampicin, Isoniazid, Pyrazinamide,
Ethambutol
b. Lipoarabinomannan- prevents destruction of bacilli
once engulfed by alveolar macrophages
bacillialveolimacrophage will phagocytize but
due to lipoarabinomannannot immediately killed
and can remain DORMANT/develop own mutation)
An INFECTIOUS DISEASE
Droplet Nuclei
In saliva
Coughing /Speaking
<5 10 microns
If it breaks <5
microns
*bacilli can enter
MODERATELY INFECTIOUS DSE
(+) smear may infect 10-15 persons a year = exponential
TB
***Extensively drug-resistant TB: 95% mortality rate (South
Africa) in 56 pts55 died
**PATIENT should be the one wearing the mask degree of
decrease in infectiousness is greater
***TB great mimicker of all diseases can be found in all
body parts; mimics cancer
CLINICAL MANIFESTATIONS :
I.
Pulmonary TB
Primary Disease
a. Middle and lower lung zones
b. Ghon complex
Post-primary (adult type)
a. Apex and post segment of upper lobes
b. Rasmussens aneurysm
II.
Extra-pulmonary TB
a. Lymph nodes TB
b. Pleural TB
c. TB of the upper airways
d. GU TB
From exposure to infectionnot all infected with
TBEXOGENOUS FACTORS
a. Exposure to a TB patient
b. Virulence of case
c. Closeness to patient
d. If living/sleeping together in the same room
From infection to disease ENGENOUS FACTORS: Immunity
a. Good immune system
b. Low immune system
**the risk of developing depend on:
Innate immunologic defenses
[PHYSIOLOGY LECTURE DR. REVILLA]
e.
f.
g.
h.
i.
Skeletal TB
Tuberculous meningitis
Peritoneal TB
Pericardial TB
Miliary TB
Early 2005 = Bill Gates GFATM (Global Funding against AIDS,
TB and Malaria)
*provide funds only for 5 years
*should be self sustainable after
Private initiated PPMD Unit: SLU PPMD (Public Private Mixed
DOTS) Unit
DIAGNOSIS:
AFB SMEAR: most important due to accessibility
Chest X-ray
TB culture
Follow up meeting:
Other problems: educational lapses: pharmacy and
medical school
*Mandated lecture on TB from 1st to 4th year
National CDR 2005: target of 70% case detection rate (met by
Region 3,4,5,6,8,10,12,ARMM)
CAR: lowest rate - only37%
Baguio: lowest - 12% in 2005; 17% in 2006
Together with Mt. Province, Benguet
Note taker: DONATO, MK//DION, Carol//CENIL, Ella
You might also like
- Computer ModuleDocument8 pagesComputer ModuleJayricDepalobosNo ratings yet
- The LightDocument2 pagesThe LightJayricDepalobosNo ratings yet
- Music Order for Northern Luzon Adventist CollegeDocument1 pageMusic Order for Northern Luzon Adventist CollegeJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- Shipping Confirmation 1264941Document1 pageShipping Confirmation 1264941JayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- WWW SlidDocument1 pageWWW SlidJayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- The Church Must Stand TogetherDocument7 pagesThe Church Must Stand TogetherJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Acquaintance Party ParticipantsDocument1 pageAcquaintance Party ParticipantsJayricDepalobosNo ratings yet
- Sample Child Dedication ProgramDocument1 pageSample Child Dedication ProgramJayricDepalobos100% (2)
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Peer Evaluation For Group 5Document1 pagePeer Evaluation For Group 5JayricDepalobosNo ratings yet
- Chapter 01 ChoicesDocument9 pagesChapter 01 ChoicesJayricDepalobosNo ratings yet
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Document3 pages"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNo ratings yet
- Census TemplateDocument3 pagesCensus TemplateJayricDepalobosNo ratings yet
- YHH Strategic Plan 2016-2017Document5 pagesYHH Strategic Plan 2016-2017JayricDepalobosNo ratings yet
- CAA Concert ProgramDocument2 pagesCAA Concert ProgramJayricDepalobosNo ratings yet
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocument2 pagesWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNo ratings yet
- Psalm 23 SermonDocument5 pagesPsalm 23 SermonJayricDepalobosNo ratings yet
- Understanding Thalassemia: Causes, Symptoms and TreatmentDocument19 pagesUnderstanding Thalassemia: Causes, Symptoms and TreatmentJayricDepalobosNo ratings yet
- General Anesthesia in Caesarean SectionDocument7 pagesGeneral Anesthesia in Caesarean SectionJayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- Clinical Pastoral OrientationDocument3 pagesClinical Pastoral OrientationJayricDepalobos100% (1)
- Pneumonia Antibiotics PDFDocument1 pagePneumonia Antibiotics PDFRudy KurniawanNo ratings yet
- Teen Parenting Brochure AssignmentDocument1 pageTeen Parenting Brochure AssignmentJayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 12 - Blood Groups and Blood Transfusion 2018Document27 pages12 - Blood Groups and Blood Transfusion 2018gimspath cme2022No ratings yet
- IntroductionDocument5 pagesIntroductionDivyansh GolyanNo ratings yet
- Diseases of The EarDocument48 pagesDiseases of The Earabela_amulu100% (1)
- Cardiovascular Assessment ChecklistDocument2 pagesCardiovascular Assessment Checklistvishnu100% (3)
- Salbutamol + IpratropiumDocument3 pagesSalbutamol + IpratropiumShiva TorinsNo ratings yet
- Fluid and Electrolyte ImbalanceDocument65 pagesFluid and Electrolyte Imbalancesreenu100% (4)
- Abnormal Psychology V2Document343 pagesAbnormal Psychology V2Bianca Dennise Villar Guingab100% (2)
- The Many Benefits of Hydrogen PeroxideDocument9 pagesThe Many Benefits of Hydrogen PeroxideRedza100% (7)
- Levels PreventionDocument10 pagesLevels PreventionSoumya KrishnaNo ratings yet
- Cristal TrialDocument9 pagesCristal TrialJorge Barrios FloresNo ratings yet
- Principles of Blood Transfusion 2Document21 pagesPrinciples of Blood Transfusion 2dhivya singhNo ratings yet
- Rinderpest: ImportanceDocument5 pagesRinderpest: Importancekadek ayu ichaNo ratings yet
- MIDTERMS MS SL NGT TPN FeedingDocument7 pagesMIDTERMS MS SL NGT TPN FeedingMarie Cris SorianoNo ratings yet
- FREE RANGE CHICKEN AND GOAT PRODUCTION GUIDEDocument78 pagesFREE RANGE CHICKEN AND GOAT PRODUCTION GUIDEMA DapNo ratings yet
- Growth Hormone DeficiencyDocument11 pagesGrowth Hormone DeficiencyIgor VasićNo ratings yet
- Prevention of Substance Use and AbuseDocument14 pagesPrevention of Substance Use and AbuseDianne SagunNo ratings yet
- Medical Terminology Word Parts, Prefixes, and SuffixesDocument24 pagesMedical Terminology Word Parts, Prefixes, and SuffixesMuhammad Bilal Bin Amir100% (2)
- Join Radiotherapy Physics TeamDocument2 pagesJoin Radiotherapy Physics TeamAlina RogojanuNo ratings yet
- Antianginal Drugs: Claro M. Isidro M.DDocument34 pagesAntianginal Drugs: Claro M. Isidro M.DNikki ChauhanNo ratings yet
- NCP #2Document2 pagesNCP #2Faith CalimlimNo ratings yet
- Cad NCPDocument1 pageCad NCPKrizzia Mae F. MayoresNo ratings yet
- Tutorial 9 PDFDocument6 pagesTutorial 9 PDFPututWisnuNugrohoNo ratings yet
- Lab Units - AbbreviationsDocument2 pagesLab Units - Abbreviationsbilashdon100% (1)
- High-Performance Ultrasound System SonixTouchDocument4 pagesHigh-Performance Ultrasound System SonixTouchdianNo ratings yet
- GRAND PRES - CorrectedDocument22 pagesGRAND PRES - CorrectedDarlen RabanoNo ratings yet
- Piezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegeDocument36 pagesPiezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegePrathusha Umakhanth100% (1)
- 60 Most Common DrugsDocument1 page60 Most Common DrugsNikkaLim100% (1)
- Management of Infected Pancreatic Necrosis 65Document4 pagesManagement of Infected Pancreatic Necrosis 65zahir_jasNo ratings yet
- Therapeutic MassageDocument3 pagesTherapeutic MassageColleen Katherine CloseNo ratings yet
- Nursing Stomach NotesDocument5 pagesNursing Stomach Noteslucas dibenedettoNo ratings yet