Professional Documents
Culture Documents
Gender Differences in Self-Assessed Health-Related Quality of Life in Children With Atopic Dermatitis
Uploaded by
nurulOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gender Differences in Self-Assessed Health-Related Quality of Life in Children With Atopic Dermatitis
Uploaded by
nurulCopyright:
Available Formats
[ORIGINAL
RESEARCH]
Gender Differences in Self-assessed
Health-related Quality of Life in
Children with Atopic Dermatitis
PAVEL V. CHERNYSHOV; bROGER C. HO; cFIORELLA MONTI; dANNA JIRAKOVA;
e
SVITLANA S. VELITCHKO; dJANA HERCOGOVA; cERICA NERI
a
Department of Dermatology and Venereology, National Medical University, Kiev, Ukraine; bDepartment of Psychological Medicine,
Yong Loo Lin School of Medicine, National University of Singapore, Singapore; cDepartment of Psychology, University of Bologna, Bologna, Italy;
d
Dermatovenereology Department of the 2nd Medical Faculty of Charles University, Prague, Czech Republic;
e
Pediatric Polyclinic of Svjatoshin District, Kiev, Ukraine
ABSTRACT
Background: Atopic dermatitis has a significant impact on quality of life of children and families. Objective: It is
important to assess gender differences in health-related quality of life in children with atopic dermatitis in order to
effectively use health-related quality of life results. Methods: Children 5- to 16-years of age with atopic dermatitis from
Italy, Singapore, Czech Republic, and Ukraine were divided into two groups (boys and girls). Each child in the group of
boys was matched to a corresponding child in the group of girls from the same country whose age and scoring atopic
dermatitis value were almost identical. Self-assessed health-related quality of life was measured by the Childrens
Dermatology Life Quality Index. Results: The difference in overall Childrens Dermatology Life Quality Index between
boys and girls was not significant (P=0.33). Girls with atopic dermatitis assessed Childrens Dermatology Life Quality
Index item on embarrassment significantly higher (0.780.93 for boys and 1.140.93 for girls, P<0.05). Lowest scored
items were the same and overall Childrens Dermatology Life Quality Index results significantly correlated with scoring
atopic dermatitis values in both groups. Two separate Childrens Dermatology Life Quality Index items in boys and five
items in girls significantly correlated with atopic dermatitis severity. The Childrens Dermatology Life Quality Index item
on affected sleep significantly correlated with the age of boys (r=0.38, P=0.02) and another Childrens Dermatology Life
Quality Index item on school work/holiday with the age of girls (r=0.59, P<0.01). Conclusion: Despite that the authors
did not find differences in overall health-related quality of life results, girls were more embarrassed, self-conscious, upset,
and sad because of atopic dermatitis. The authors results may influence the educational part of consultations of children
with atopic dermatitis. (J Clin Aesthet Dermatol. 2016;9(8):1924.)
topic dermatitis (AD) has a significant impact on the
quality of life (QoL) of affected children and their
families.13 As in adults, childhood health-related
(HR) QoL is commonly assessed by means of generic
and/or specific instruments, including dermatology-specific
and disease-specific measures.4 Measurement of HRQoL in
pediatric dermatology helps to assess the impact of a single
skin disease on a childs life, to register the patients view on
the efficacy of different treatment methods, educational
programs, and consultations. It makes it possible to
compare the impact of skin diseases and results of the
treatment in children from different age groups on local,
regional, national, and international levels.5 The vast
majority of publications concerning HRQoL assessment in
children with skin conditions is dedicated to AD.4 For the
effective use of HRQoL results, it is important to know
about existing gender differences in HRQoL assessment.
Contradictory results concerning gender differences in
HRQoL of children with AD under four years measured by
the Infants Dermatitis Quality of Life Index (IDQoL)
questionnaire were previously reported. Park et al6 found
more severe impact of AD on boys in 48 non-matched boys
and 53 girls. Meanwhile, Alzolibani7 did not find gender
differences in non-matched AD children. Chernyshov8 also
had not found a significant gender difference of the overall
IDQoL scores in 102 non-matched AD children, but found
DISCLOSURE: The authors report no relevant conflicts of interest
ADDRESS CORRESPONDENCE TO: Pavel V. Chernyshov, MD, PhD, Department of Dermatology and Venereology, National Medical University, 13,
Bulvar Shevchenko, 01601, Kiev, Ukraine; E-mail: chernyshovpavel@ukr.net
[August 2016 Volume 9 Number 8]
19
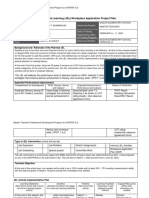
Figure 1. CDLQI results in boys and girls with atopic dermatitis
TABLE 1. Mean age, SCORAD and overall CDLQI scores of boys
and girls with atopic dermatitis
Age in years
SCORAD
CDLQI
BOYS (n=36)
GIRLS (n=36)
9.693.21
9.833.27
28.1419.55
28.1920.70
8.316.33
9.256.73
significant gender differences when each child in the group
of boys was matched to a corresponding child in the group
of girls whose age in months and scoring atopic dermatitis
(SCORAD) value were almost identical.8
Kiebert et al9 found a significant gender difference in
self-assessed HRQoL of older children with AD. The
Childrens Dermatology Life Quality Index (CDLQI) scores
were significantly higher in girls in that study. Hon et al10
and Ang et al11 reported that girls had more problems with
issues of clothes and shoes than did boys10 and had higher
scores on the swimming and other sports item.11 Recently,
the authors did not find significant gender differences in
self-assessed HRQoL of non-matched children from
Ukraine, Italy, Czech Republic, and Singapore.12
In this study, the authors decided to analyze gender
differences in self-assessed HRQoL of children with AD
matched by country, age, and disease severity.
MATERIALS AND METHODS
For the study, data on children with AD from 5 to 16
years of age who had no other manifest diseases from four
countries (Ukraine, Czech Republic, Singapore, and Italy)
were used .
One hundred sixty-seven children with AD from Ukraine,
Singapore, Italy, and Czech Republic were divided into two
20
groups based on their sex and matched according to age
and SCORAD13 values. Each child in the group of boys was
matched to a corresponding child in the group of girls from
the same country whose age and SCORAD value were
almost identical. Age difference in pairs did not exceed one
year. Difference in SCORAD in pairs did not exceed 3.0 (but
both children in pairs were with the same severity grade:
severe, moderate, or mild). AD with a SCORAD higher than
40 was regarded as severe, whereas AD with a SCORAD
below 20 was regarded as mild.14
Thus, 36 girls and 36 boys (16 from Italy, 10 from
Singapore, 20 from Czech Republic, and 26 from Ukraine)
with AD were selected for further investigation. Diagnosis
of AD was made using Hanifin and Rajka or Williams
criteria.15,16 Disease severity was estimated using the
SCORADa clinical disease severity instrument that
combines information on the involved area of skin, as well
as objective and subjective symptoms in patients with AD.13
Self-assessed HRQoL was assessed by means of the
CDLQI.17 The CDLQI HRQoL questionnaire is designed for
use in children with skin conditions who are 5 to 16 years of
age. The CDLQI questionnaire is self-explanatory and can
be simply handed to the patient who is asked to fill it in with
the help of the childs parent or guardian. The 10 questions
of the CDLQI cover six areas of daily activities including
symptoms and feelings, leisure, school or holidays, personal
relationships, sleep, and treatment. Each question is
answered on a 4-point Likert scale scored from 0 to 3. These
are added to give a minimum score of 0 and maximum score
of 30. Higher scores indicate a poorer quality of life. In order
to help the clinical interpretation of the CDLQI scores, a
banding system (consisting of 5 bands) has been
proposed.18 According to this system, a CDLQI score of 01
= no effect on childs life, 26 = small effect on childs life,
712 = moderate effect on childs life, 1318 = very large
effect on childs life, and 1930 = extremely large effect on
childs life. Original (English), Ukrainian, Czech, and Italian
versions of the CDLQI questionnaire were used. Data on
validation of original (English) and Ukrainian versions of
the CDLQI were previously published.17,19 Permission to use
the CDLQI questionnaire was granted by its authors and
copyright owners Professor Andrew Y. Finlay and Dr. M.S.
Lewis-Jones. Ethical permission for the study was granted
by the local ethic research committees.
Data was presented as mean standard deviation of the
mean. Paired t-test (two-sided), Fishers exact test (twosided) and non-parametric correlation (Spearmans r) were
used. The results were considered significant if P<0.05.
RESULTS
Mean age, SCORAD, and overall CDLQI scores of
selected boys and girls with AD are presented in Table 1.
The difference in overall CDLQI between boys and girls was
not statistically significant (P=0.33). No differences were
found in distribution of the overall CDLQI scores of boys
and girls with AD according to the CDLQI banding (Table
2).
Subscale on symptoms and feelings was assessed
[August 2016 Volume 9 Number 8]
20
significantly higher by girls with AD (P<0.05). However,
there was no gender difference in assessment of the CDLQI
item on symptoms (1.530.77 for boys and 1.560.77 for
girls, P=0.42). A gender difference was found for the item
on feelings. Girls with AD assessed the CDLQI item on,
How embarrassed or self conscious, upset or sad have you
been because of your skin? significantly higher than boys
(0.780.93 for boys and 1.140.93 for girls, P<0.05).
Lowest scored items were the same for boys and girls:
How much has your skin affected your friendships?, How
much trouble have you had because of your skin with other
people calling you names, teasing, bullying, asking questions,
or avoiding you? and How much have you avoided
swimming or other sports because of your skin trouble? The
highest scored CDLQI item was How itchy, scratchy, sore,
or painful has your skin been? Meanwhile, the second highly
scored item in boys was: How much have you changed or
worn different or special clothes or shoes because of your
skin? and in girls: How embarrassed or self conscious,
upset, or sad have you been because of your skin?
Overall, CDLQI results significantly correlated with
SCORAD and not significantly with the age of boys and girls
(Table 3). Correlations between SCORAD and age was
extremely poor (r=0.01, P=0.95 for boys and r=0.03, P=0.84
for girls).
Two separate CDLQI items in boys and five items in girls
significantly correlated with AD severity (Table 4).
A single CDLQI item on How much has your sleep been
affected by your skin problem? significantly correlated
with the age of boys (r=0.38, P=0.02) and another single
item How much did your skin problem affect your school
work/interfered with your enjoyment of the holiday?
significantly correlated with the age of girls (r=0.59,
P<0.01).
TABLE 2. Distribution of the overall CDLQI scores of boys and
girls with AD according to the CDLQI banding
CDLQI BANDING
BOYS (n=36)
GIRLS (n=36)
No effect
Small effect
14
12
Moderate effect
13
14
Very large effect
Extremely large effect
TABLE 3. Correlations of the overall CDLQI scores with SCORAD
and age of boys and girls with AD
CDLQI SCORES
BOYS (n=36)
GIRLS (n=36)
SCORAD
r=0.33, P<0.05
r=0.47, P<0.01
Age
r=0.24, P=0.16
r=0.29, P=0.08
DISCUSSION
In contrast with Kiebert et al,9 in the authors study,
overall CDLQI results of girls with AD were not significantly
higher than boys results. Balci et al20 reported no
statistically significant differences in the CDLQI subscales
scores according to the gender they reported significant
difference in symptoms and feeling subscale. However,
symptoms were assessed almost identically by both genders
in the authors study.
Despite the fact that the authors did not find differences
in overall HRQoL results, girls were more embarrassed, selfconscious, upset, and sad because of AD. These problems
together with subjective complaints on itching, scratching
and pain correlated with disease severity in both sexes.
Meanwhile, effect on friendship, going out, playing, or doing
hobbies and avoidance of swimming or other sports
correlated with SCORAD exclusively in girls and were
scored lowest by both sexes.
The fact that the item on name calling, teasing, bullying,
asking questions, or avoiding was one of the lowest scored
items and had extremely poor correlation with AD severity
in girls indicates that AD impact on friendship, going out,
playing, or doing hobbies and avoiding swimming or other
sports correlates with AD severity not because of other
peoples reactions, but mostly because girls are more
embarrassed, self-conscious, upset, and sad. It may also be
related to having problems at school and age. We can
speculate that older school girls are more concentrated on
social aspects of school life including romantic relations and
it is more difficult for them to appear in class with
manifestations of AD. Meanwhile, in a recent study by
Halvorsen et al,21 18- to 19-year-old men with current
eczema were less likely to have had romantic relationships.
It was previously reported that avoidance strategies are
typical for AD patients, resulting in marked behavioral
avoidance of intimate situations.22 Problems in AD patients
in that study were mediated more by appearance and
texture of non-genital skin than by involvement of genital
skin. However, in asthma, another atopic disease, female
subjects reported significantly greater missed days of
school compared to males despite no difference in asthma
severity.23 Thus, this gender difference may be present even
without skin involvement. Jirakova et al24 previously
reported that 14- to 18-year-old children with AD had more
problems during school or holidays than 7- to 13-year-old
[August 2016 Volume 9 Number 8]
21
TABLE 4. Correlations of separate CDLQI items scores with SCORAD in boys and girls with AD
SCORAD
CDLQI ITEMS
BOYS (n=36)
GIRLS (n=36)
How itchy, scratchy, sore, or painful has your skin been?
r=0.60, P<0.01
r=0.59, P<0.01
How embarrassed or self-conscious, upset or sad have you been because of your skin?
r=0.41, P=0.01
r=0.39, P=0.02
How much has your skin affected your friendships?
r=0.25, P=0.14
r=0.45, P<0.01
How much have you changed or worn different or special clothes or shoes because of your
skin?
r=0.24, P=0.16
r=0.20, P=0.24
How much has your skin trouble affected going out, playing, or doing hobbies?
r=0.25, P=0.14
r=0.45, P<0.01
How much have you avoided swimming or other sports because of your skin trouble?
r=0.27, P=0.12
r=0.43, P<0.01
How much did your skin problem affect your school work/interfered with your enjoyment of the
holiday?
r=0.25, P=0.15
r=0.31, P=0.06
How much trouble have you had because of your skin with other people calling you names,
teasing, bullying, asking questions, or avoiding you?
r=0.18, P=0.30
r=-0.01, P=0.99
How much has your sleep been affected by your skin problem?
r=0.10, P=0.54
r=0.31, P=0.06
How much of a problem has the treatment for your skin been?
r=0.10, P=0.56
r=0.14, P=0.42
children. We can speculate that the girls answers caused
this difference.
Meanwhile, correlation of the CDLQI item How much
has your sleep been affected by your skin problem?
exclusively with the age of boys may be explained by the
results of other published studies. Thus, the findings of
Sadeh et al25 reflected significant age differences, indicating
that older children have more delayed sleep onset times and
increased reported daytime sleepiness. Girls were found to
spend more time in sleep and to have an increased
percentage of motionless sleep. Gaina et al26 also found that
boys sleep was less efficient and more fragmented during
the entire week in comparison to that of the girls. Finally,
Krishnan and Collop27 found that gender differences in sleep
become apparent after the onset of puberty. In the authors
study, sleep problems in boys correlated with age and did
not correlate with disease severity. Thus, these problems
may be more related to physiologic peculiarities of puberty.
Despite the authors expectations, they did not find
gender difference in problems with issues of clothes and
22
shoes, as reported by Hon et al.10
In the study by Ang et al,11 the CDLQI item on problems
with swimming and other sports was the second highly
scored item in girls and had a significantly higher impact on
HRQoL of girls. In the authors study, this CDLQI item was
assessed as one of the lowest scored items by both sexes.
This may be explained by poorer involvement of the
authors study population in sport activities and swimming.
Gender differences in self-assessed HRQoL of 5- to 16year-old children with AD in the authors study appeared to
be less prominent than in younger AD children assessed by
disease-specific proxy questionnaire.8 The same principals
of matching of AD patients were used in both studies. Use
of questionnaire in a single center with a particular
language version could be thought to restrict the
generalizability of the findings of the study. However,
recent international studies reported that parents of AD
children from different countries assess their childrens
HRQoL in a quite similar manner.28,29
The authors present international study confirmed the
[August 2016 Volume 9 Number 8]
22
tendency for AD to have more of a severe impact on girls
lives. These results may influence the educational part of
consultations with children who have AD. Meanwhile,
psychological problems increase with AD disease severity in
both sexes, and girls in general need more attention to their
AD-related psychological problems. In particular,
specialists advice should focus on the prevention of
avoidance behavior formation in girls who have more severe
AD and older adolescent girls in cases of absence of teasing
and bullying. Otherwise, progression of such avoidance
behavior may affect friendships, hobbies, sports, and even
school studies in older girls and may lead to more serious
consequences in their future life.
Older boys with AD should receive general
recommendations on improving their sleep. According to
the United States National Sleep Foundation
recommendations, children of all ages should fall asleep
independently, go to bed before 9:00 pm, have an
established bedtime routine, include reading as part of their
bedtime routine, refrain from caffeine, and sleep in
bedrooms without televisions.30 Those who exercize
vigorously in the morning also have favorable sleep
outcomes, including greater likelihood of reporting good
sleep quality and lower likelihood of waking unrefreshed.
Evening exercise is not associated with worse sleep31 and
may increase objectively assessed sleep efficiency.32
The main limitation of this study is the different number
of patients per country, which may cause speculation on
cross-cultural inequivalence. However, a recent study
revealed that highest and lowest scored CDLQI items in
these countries are quite common.12 The relatively low
number of patients in this study is the result of the
scrupulous matching process.
To the best of the authors knowledge, this is the first
study on gender differences of self-assessed HRQoL in
children with AD when patients were well-matched. The
results of this study may influence the educational portion
of consultations with children who have AD.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
ACKNOWLEDGMENT
The authors thank Professor A.Y. Finlay and Dr. M.S.
Lewis-Jones for permission to use the CDLQI and the DFI
questionnaires.
17.
REFERENCES
18.
1.
2.
3.
Beattie PE, Lewis-Jones MS. An audit of the impact of a
consultation with a pediatric dermatology team on quality of
life in infants with atopic eczema and their families: further
validation of the Infants Dermatitis Quality of Life Index and
Dermatitis Family Impact score. Br J Dermatol. 2006;155:
12491255.
Monti F, Agostini F, Gobbi F, et al. Quality of life measures in
Italian children with atopic dermatitis and their families. Ital
J Pediatr. 2011;37:59.
Chernyshov PV, Kaliuzhna LD, Reznikova AA, Basra MK.
Comparison of the impairment of family quality of life
assessed by disease-specific and dermatology-specific
instruments in children with atopic dermatitis. J Eur Acad
19.
20.
21.
Dermatol Venereol. 2014;29(6):12211224.
Chernyshov P, de Korte J, Tomas-Aragones L, Lewis-Jones S.
EADV Taskforces recommendations on measurement of
health-related quality of life in paediatric dermatology. J Eur
Acad Dermatol Venereol. 2015;29:23062316.
Chernyshov P. Dermatological quality of life instruments in
children. G Ital Dermatol Venereol. 2013;148:277285.
Park CK, Park CW, Lee CH. Quality of life and the family
impact of atopic dermatitis in children. Korean J Dermatol.
2007;45:429438.
Alzolibani A. Impact of atopic dermatitis on the quality of life
of Saudi children. Saudi Med J. 2014;35:391396.
Chernyshov PV. Gender differences in health-related and
family quality of life in young children with atopic dermatitis.
Int J Dermatol. 2012;51:290294.
Kiebert G, Sorensen SV, Revicki D, et al. Atopic dermatitis is
associated with a decrement in health-related quality of life.
Int J Dermatol. 2002;41:151158.
Hon KL, Leung TF, Wong KY, et al. Does age or gender
influence quality of life in children with atopic dermatitis?
Clin Exp Dermatol. 2008;33:705709.
Ang SB, Teng CWC, Monika TP, Wee H. Impact of atopic
dermatitis on health-related quality of life among infants and
children in Singapore: a pilot cross-sectional study.
Proceedings of Singapore Healthcare. 2014;23:100107.
Chernyshov PV, Ho RC, Monti F, et al. An international multicenter study on self-assessed and family quality of life in
children with atopic dermatitis. Acta Dermatovenerol Croat.
2015;23:247253.
Severity scoring of atopic dermatitis: the SCORAD index.
Consensus Report of the European Task Force on Atopic
Dermatitis. Dermatology. 1993;186:2331.
Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of
atopic eczema (atopic dermatitis). Part I. J European Acad
Dermatol Venereol. 2012;26:10451060.
Hanifin GM, Rajka G. Diagnostic feature of atopic dermatitis.
Acta Derm Venereol. 1980;92(Suppl.):4447.
Williams HC, Burney PG, Pembroke AC, Hay RJ. The U.K.
Working Partys Diagnostic Criteria for Atopic Dermatitis. III.
Independent hospital validation. Br J Dermatol.
1994;131:406416.
Lewis-Jones MS, Finlay AY. The Childrens Dermatology Life
Quality Index (CDLQI): initial validation and practical use. Br
J Dermatol. 1995;132:942949.
Waters A, Sandhu D, Beattie P, et al. Severity stratification of
Childrens Dermatology Life Quality Index (CDLQI) scores.
Br J Dermatol. 2010;163(Suppl 1):121.
Chernyshov PV. Creation and cross-cultural adaptation of
Ukrainian versions of questionnaires for assessment of quality
of life of children with atopic dermatitis and their families. Lik
Sprava. 2008;12:124128.
Balci D, Sangn , Inandi T. Cross validation of the Turkish
version of Childrens Dermatology Life Quality Index. J Turk
Acad Dermatol. 2007;1:71402a.
Halvorsen JA, Lien L, Dalgard F, et al. Suicidal ideation,
mental health problems, and social function in adolescents
with eczema: a population-based study. J Invest Dermatol.
2014;134:18471854.
[August 2016 Volume 9 Number 8]
23
22.
23.
24.
25.
26.
27.
24
Magin P, Heading G, Adams J, Pond D. Sex and the skin: a
qualitative study of patients with acne, psoriasis and atopic
eczema. Psychol Health Med. 2010;15:454462.
Lee JH, Haselkorn T, Chipps BE, Miller DP, Wenzel SE; Tenor
Study Group. Gender differences in IgE-mediated allergic
asthma in the epidemiology and natural history of asthma:
Outcomes and Treatment Regimens (TENOR) study. J
Asthma. 2006;43:179184.
Jirkov A, Vojckov N, Gpfertov D, Hercogov J. A
comparative study of the impairment of quality of life in
Czech children with atopic dermatitis of different age groups
and their families. Int J Dermatol. 2012;51:688692.
Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep
disruptions in school-age children. Developmental
Psychology. 2000;36:291301.
Gaina A, Sekine M, Hamanishi S, et al. Gender and temporal
differences in sleep-wake patterns in Japanese
schoolchildren. Sleep. 2005;28:337342.
Krishnan V, Collop NA. Gender differences in sleep disorders.
Curr Opin Pulm Med. 2006;12:383389.
28.
29.
30.
31.
32.
Chernyshov P, Jirkov A, Hercogov J. Comparative study of
the quality of life of children with atopic dermatitis from
Ukraine and the Czech Republic. J Eur Acad Dermatol
Venereol. 2011;25:14831484.
Chernyshov PV, Jirakova A, Ho RC, et al. An international
multicenter study on quality of life and family quality of life in
children with atopic dermatitis. Indian J Dermatol Venereol
Leprol. 2013;79:5258.
Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD.
Developmental aspects of sleep hygiene: findings from the
2004 National Sleep Foundation Sleep in America Poll. Sleep
Med. 2009;10:771779.
Buman MP, Phillips BA, Youngstedt SD, et al. Does nighttime
exercise really disturb sleep? Results from the 2013 National
Sleep Foundation Sleep in America Poll. Sleep Med.
2014;15:755761.
Brand S, Kalak N, Gerber M, et al. High self-perceived
exercise exertion before bedtime is associated with greater
objectively assessed sleep efficiency. Sleep Med.
2014;15:10311036.
[August 2016 Volume 9 Number 8]
24
You might also like
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hedgehog Interacting Protein Promotes Fibrosis and Apoptosis in Glomerular Endothelial Cells in Murine DiabetesDocument10 pagesHedgehog Interacting Protein Promotes Fibrosis and Apoptosis in Glomerular Endothelial Cells in Murine DiabetesnurulNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Drosophila Species Learn Dialects Through Communal Living.Document32 pagesDrosophila Species Learn Dialects Through Communal Living.nurulNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Carriage Methicillin-Resistant Staphylococcus Aureus in Poultry and Cattle in Northern AlgeriaDocument6 pagesCarriage Methicillin-Resistant Staphylococcus Aureus in Poultry and Cattle in Northern AlgerianurulNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Iodine Deficiency in Women of Childbearing AgeDocument1 pageIodine Deficiency in Women of Childbearing AgenurulNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Latent Profile Analysis Approach To The Relationship Between Patient and Physician Global Assessments of Rheumatoid Arthritis Activity.Document10 pagesLatent Profile Analysis Approach To The Relationship Between Patient and Physician Global Assessments of Rheumatoid Arthritis Activity.nurulNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Differences in Self-Reported Weekend Catch Up Sleep Between Children and Adolescents With and Without Primary HypertensionDocument8 pagesDifferences in Self-Reported Weekend Catch Up Sleep Between Children and Adolescents With and Without Primary HypertensionnurulNo ratings yet
- Wang Et Al-2017-The Journal of Clinical HypertensionDocument10 pagesWang Et Al-2017-The Journal of Clinical HypertensionnurulNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Assessment of Accuracy and Recognition of Three-Dimensional Computerized Forensic Craniofacial ReconstructionDocument13 pagesAssessment of Accuracy and Recognition of Three-Dimensional Computerized Forensic Craniofacial ReconstructionnurulNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Ijhy2018 6959165 PDFDocument7 pagesIjhy2018 6959165 PDFnurulNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Therapeutic Effects of Fermented Flax Seed Oil On NC/Nga Mice With Atopic Dermatitis-Like Skin LesionsDocument11 pagesTherapeutic Effects of Fermented Flax Seed Oil On NC/Nga Mice With Atopic Dermatitis-Like Skin LesionsnurulNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- 2018 Article 356Document9 pages2018 Article 356nurulNo ratings yet
- Research ArticleDocument11 pagesResearch ArticlenurulNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Oncotarget 08 115326Document19 pagesOncotarget 08 115326nurulNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Ijbsv 14 P 0087Document13 pagesIjbsv 14 P 0087nurulNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Establishing Reference Ranges of Hematological Parameters From Malian Healthy AdultsDocument11 pagesEstablishing Reference Ranges of Hematological Parameters From Malian Healthy AdultsnurulNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Maltreated Children Use More Grammatical NegationsDocument12 pagesMaltreated Children Use More Grammatical Negationsnurul100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Malaria Severity: Possible Influence of The E670G PCSK9 Polymorphism: A Preliminary Case-Control Study in Malian ChildrenDocument1 pageMalaria Severity: Possible Influence of The E670G PCSK9 Polymorphism: A Preliminary Case-Control Study in Malian ChildrennurulNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Mesenchymal Stem Cell Therapy For in Ammatory Skin Diseases: Clinical Potential and Mode of ActionDocument25 pagesMesenchymal Stem Cell Therapy For in Ammatory Skin Diseases: Clinical Potential and Mode of ActionnurulNo ratings yet
- 2016 Article 1945 PDFDocument24 pages2016 Article 1945 PDFnurulNo ratings yet
- Research | Dermatol Pract Concept 2016;6(3):4 11 DERMATOLOGY PRACTICAL & CONCEPTUAL www.derm101.com Introduction Seborrheic dermatitis (SD), a common skin disorder that typically presents as erythematous plaques or patches and can vary from mild dandruff to dense, diffuse, adherent scale affecting the areas where sebaceous glands are prominent, including the scalp, face and chest. Its precise etiology remains unknown, though it is associated with genetic, environmen - tal, and general health factors. Other important pathogenic factor seems to be Malassezia colonization. Its role could be Effect of itraconazole on the quality of life in patients with moderate to severe seborrheic dermatitis: a randomized, placebo-controlled trialDocument6 pagesResearch | Dermatol Pract Concept 2016;6(3):4 11 DERMATOLOGY PRACTICAL & CONCEPTUAL www.derm101.com Introduction Seborrheic dermatitis (SD), a common skin disorder that typically presents as erythematous plaques or patches and can vary from mild dandruff to dense, diffuse, adherent scale affecting the areas where sebaceous glands are prominent, including the scalp, face and chest. Its precise etiology remains unknown, though it is associated with genetic, environmen - tal, and general health factors. Other important pathogenic factor seems to be Malassezia colonization. Its role could be Effect of itraconazole on the quality of life in patients with moderate to severe seborrheic dermatitis: a randomized, placebo-controlled trialnurulNo ratings yet
- Extract of Polygala Tenuifolia Alleviates Stress-Exacerbated Atopy-Like Skin Dermatitis Through The Modulation of Protein Kinase A and p38 Mitogen-Activated Protein Kinase Signaling PathwayDocument16 pagesExtract of Polygala Tenuifolia Alleviates Stress-Exacerbated Atopy-Like Skin Dermatitis Through The Modulation of Protein Kinase A and p38 Mitogen-Activated Protein Kinase Signaling PathwaynurulNo ratings yet
- Pityriasis Amiantacea: A Study of Seven CasesDocument3 pagesPityriasis Amiantacea: A Study of Seven CasesnurulNo ratings yet
- The mPEG-PCL Copolymer For Selective Fermentation of Staphylococcus Lugdunensis Against Candida Parapsilosis in The Human MicrobiomDocument19 pagesThe mPEG-PCL Copolymer For Selective Fermentation of Staphylococcus Lugdunensis Against Candida Parapsilosis in The Human MicrobiomnurulNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Efficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudyDocument7 pagesEfficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudynurulNo ratings yet
- Efficacy of A Film-Forming Medical Device Containing Piroxicam and Sun Filters in The Treatment of Multiple Actinic Keratosis Lesions in A Subject With A History of Kaposi SarcomaDocument8 pagesEfficacy of A Film-Forming Medical Device Containing Piroxicam and Sun Filters in The Treatment of Multiple Actinic Keratosis Lesions in A Subject With A History of Kaposi SarcomanurulNo ratings yet
- Capacity For Management of Type 2 Diabetes Mellitus (T2 DM) in Primary Health Centers in IndonesiaDocument5 pagesCapacity For Management of Type 2 Diabetes Mellitus (T2 DM) in Primary Health Centers in IndonesiaMapsNo ratings yet
- Efficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudyDocument7 pagesEfficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudynurulNo ratings yet
- Intraoperative High-Resolution Ultrasound and Contrast-Enhanced Ultrasound of Peripheral Nerve Tumors and Tumorlike LesionsDocument8 pagesIntraoperative High-Resolution Ultrasound and Contrast-Enhanced Ultrasound of Peripheral Nerve Tumors and Tumorlike LesionsnurulNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Jurnal 3 PDFDocument6 pagesJurnal 3 PDFnurulNo ratings yet
- Whole-Body PET/CT-mammography For Staging Breast Cancer: Initial ResultsDocument6 pagesWhole-Body PET/CT-mammography For Staging Breast Cancer: Initial ResultsnurulNo ratings yet
- Umair Mazher ThesisDocument44 pagesUmair Mazher Thesisumair_mazherNo ratings yet
- PIC16 F 1619Document594 pagesPIC16 F 1619Francisco Martinez AlemanNo ratings yet
- (Cambridge Series in Statistical and Probabilistic Mathematics) Gerhard Tutz, Ludwig-Maximilians-Universität Munchen - Regression For Categorical Data-Cambridge University Press (2012)Document574 pages(Cambridge Series in Statistical and Probabilistic Mathematics) Gerhard Tutz, Ludwig-Maximilians-Universität Munchen - Regression For Categorical Data-Cambridge University Press (2012)shu100% (2)
- Formula Sheet For Astronomy 1 - Paper 1 and Stars & PlanetsDocument2 pagesFormula Sheet For Astronomy 1 - Paper 1 and Stars & PlanetsprashinNo ratings yet
- P7 Summary of ISADocument76 pagesP7 Summary of ISAAlina Tariq100% (1)
- Japanese Tea Cups LessonDocument3 pagesJapanese Tea Cups Lessonapi-525048974No ratings yet
- Neoclassicism: Romanticism Realism ImpressionismDocument16 pagesNeoclassicism: Romanticism Realism ImpressionismErika EludoNo ratings yet
- EY The Cfo Perspective at A Glance Profit or LoseDocument2 pagesEY The Cfo Perspective at A Glance Profit or LoseAayushi AroraNo ratings yet
- Report-Picic & NibDocument18 pagesReport-Picic & NibPrincely TravelNo ratings yet
- 5 - Econ - Advanced Economic Theory (Eng)Document1 page5 - Econ - Advanced Economic Theory (Eng)David JackNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Reconsidering Puerto Rico's Status After 116 Years of Colonial RuleDocument3 pagesReconsidering Puerto Rico's Status After 116 Years of Colonial RuleHéctor Iván Arroyo-SierraNo ratings yet
- Fuzzys CodesDocument39 pagesFuzzys CodesJak JakNo ratings yet
- Marwar Steel Tubes Pipes StudyDocument39 pagesMarwar Steel Tubes Pipes Studydeepak kumarNo ratings yet
- Levenbach Causal2017Document15 pagesLevenbach Causal2017Jenna GrantNo ratings yet
- Book Review Reclaim Your HeartDocument7 pagesBook Review Reclaim Your HeartShaheer KhanNo ratings yet
- Chapter 10 HandoutDocument18 pagesChapter 10 HandoutChad FerninNo ratings yet
- Philosophical Perspectives Through the AgesDocument13 pagesPhilosophical Perspectives Through the Agesshashankmay18No ratings yet
- Mr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedDocument538 pagesMr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedGutenberg.orgNo ratings yet
- Nitrate Reduction in Sulfate Reducing BacteriaDocument10 pagesNitrate Reduction in Sulfate Reducing BacteriaCatalinaManjarresNo ratings yet
- The Road To Privatization: TQM and Business Planning: Bennington, Lynne Cummane, JamesDocument11 pagesThe Road To Privatization: TQM and Business Planning: Bennington, Lynne Cummane, JamesBojan KovacevicNo ratings yet
- Testing Your Understanding: The Dash, Slash, Ellipses & BracketsDocument2 pagesTesting Your Understanding: The Dash, Slash, Ellipses & BracketsBatsaikhan DashdondogNo ratings yet
- 6 Strategies For Effective Financial Management Trends in K12 SchoolsDocument16 pages6 Strategies For Effective Financial Management Trends in K12 SchoolsRainiel Victor M. CrisologoNo ratings yet
- Speakout Vocabulary Extra Advanced Unit 03Document3 pagesSpeakout Vocabulary Extra Advanced Unit 03shasha1982100% (2)
- Paul Daugerdas IndictmentDocument79 pagesPaul Daugerdas IndictmentBrian Willingham100% (2)
- BUMANGLAG - CLASS D - JEL PlanDocument3 pagesBUMANGLAG - CLASS D - JEL PlanMAUREEN BUMANGLAGNo ratings yet
- FunambolDocument48 pagesFunambolAmeliaNo ratings yet
- 4th Singapore Open Pencak Silat Championship 2018-1Document20 pages4th Singapore Open Pencak Silat Championship 2018-1kandi ari zonaNo ratings yet
- MF 04Document21 pagesMF 04Carlos De la CruzNo ratings yet
- Vadiyanatha AstakamDocument4 pagesVadiyanatha AstakamRaga MalikaNo ratings yet
- 3B Adverbial PhrasesDocument1 page3B Adverbial PhrasesSarah INo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)