Professional Documents
Culture Documents
Management of Impacted Urethral Stones in Children
Uploaded by
aesculapiusCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Impacted Urethral Stones in Children
Uploaded by
aesculapiusCopyright:
Available Formats
ORIGINAL ARTICLE
Management of Impacted Urethral Stones in Children
Jamshed Akhtar, Soofia Ahmed and Naima Zamir
ABSTRACT
Objective: To find out the clinical presentation, site of impaction, management and outcome of children presenting with
urinary retention due to urethral stone.
Study Design: Case series.
Place and Duration of Study: Surgical Unit B of National Institute of Child Health (NICH), Karachi, from April 2009 to
January 2010.
Methodology: All the patients under the age of 12 years, who presented with urinary retention due to impacted urethral
stones were included. Urinary retention due to other causes like trauma, stricture, pelvic masses etc. were excluded.
Diagnosis was made on clinical examination (palpable stone in penile urethra) and with the help of radiology. Surgical
procedure was tailored according to the site of impaction in urethra. All stones were sent for chemical analysis and patients
were followed in Nephrology OPD (stone clinic) for further work-up.
Results: There were a total of 19 patients with mean age of 3.94 2.27 years. All were males. Twelve patients (63.1%)
had stones impacted in anterior urethra while 7 (36.9%) were found in posterior urethra. Stones in penile urethra were
removed in emergency either by meatotomy (when impacted at urethral meatus, n = 3) or following initial supra-pubic
decompression of urinary bladder (using wide bore cannula) by urethrolithotomy (n = 6). Stones in bulbous (n = 3) and
posterior urethral (n = 7) locations were pushed back into bladder and later removed on elective list by supra-pubic
vesicolithotomy. No patient had proximal urinary tract calculi on further work-up. All patients remained well except one who
developed retention of urine after a week of discharge. He had urinary tract infection and was treated with antibiotics. All
the stones were of calcium oxalate type.
Conclusion: Urethral stones must be kept in differential diagnosis in a child who presents with acute urinary retention.
Clinical examination can identify causes in significant number of cases. Simple procedures like meatotomy, supra-pubic
bladder decompression and urethrolithotomy can relieve the misery in these children.
Key words:
Urethral stones. Acute urinary retention. Child. Urethrolithotomy.
INTRODUCTION
Paediatric urolithiasis is prevalent in some geographical
regions popularly known as the stone belt. This belt
runs from Philippines, Thailand, Myanmar in the Far
East through Pakistan into Iran, Middle East and
extends up-to Turkey.1 Many factors are responsible for
this endemic nature, namely nutritional deficiencies in
vitamin A, magnesium, phosphates and vitamin B6, lowprotein and high-carbohydrate diet, dehydration, urinary
tract infection etc.2 The pattern of urinary tract
involvement is quite distinct. In developed countries, it
is mostly the upper urinary tract where calculi are
found while reverse is noted in children from developing
countries where poverty prevails. A century ago, lower
urinary tracts were also reported frequently from
developed countries but as the socioeconomic
conditions improved, change occurred in the pattern of
stone disease.3,4
Department of Paediatric Surgery, National Institute of Child
Health, Karachi.
Correspondence: Dr. Jamshed Akhtar, Department of
Paediatric Surgery, National Institute of Child Health, Rafiquee
Shaheed Road, Karachi-75510, Pakistan.
E-mail: jamjim88@yahoo.com
Received November 14, 2011; accepted May 16, 2012.
510
Research in the field of stone disease identified many
preventive measures so as to reduce burden of the
disease. This is done to prevent renal loss due to
obstruction and infection. There is also a parallel
development of minimally invasive surgical techniques
to deal with urinary tract calculi. The paediatric population
is usually less fortunate as advancement in technology
aims more at adults and as a trickle down effect children
also receive benefit out of it. Though equipments are
present at many centres for minimally invasive surgical
approach for adults urolithiasis, but not for paediatric
population.5
Acute urinary retention due to impacted urethral calculus
is not an uncommon condition.6 This is extremely painful
situation and demands urgent relief. If remain unattended,
can lead to disastrous consequences of urinary extravasation and infection.7 The diagnosis is usually clinical
and simple measures can help in relieving emergency
situation. There is paucity of data on urethral stones in
paediatric age group.8
This study aimed at determining the management of this
condition so as to provide an algorithm to facilitate the
children with acute retention of urine, due to impacted
urethral stone.
Journal of the College of Physicians and Surgeons Pakistan 2012, Vol. 22 (8): 510-513
Management of impacted urethral stones in children
METHODOLOGY
RESULTS
This case series was conducted from March 2009 to
January 2010 at one of the two Surgical Units of
Department of Paediatric Surgery, NICH, Karachi. The
data of all the patients admitted with the diagnosis of
acute retention of urine due to impacted urethral stone
were analyzed. Patients aged less than 12 years were
included. All those with retention of urine due to other
causes like urethral injury, stricture, pelvic mass etc.
were excluded.
Patients were admitted and detailed history and diligent
clinical examination were done specially palpating penile
urethra and also feeling for presence of any firm
structure in the line of urethra through scrotum and at
perineal region. All patients had complete blood count,
blood urea, serum creatinine and electrolytes done.
Urine analysis and culture of sample of urine obtained,
were also performed. All patients had X-ray KUB and
ultrasound for evaluation of urinary tract.
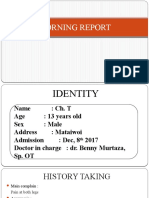
In a duration of 10 months, 19 patients presented with
acute retention of urine due to impacted urethral stone
(Figure 1). All were males. Age ranged from one year to
10 years with the mean age of 3.94 years 2.27 years.
None of (63.1%) the patients had any anatomical lesion.
In 12 patients (63.1%) stones were impacted in anterior
urethra while 7 patients (36.9%) were located at posterior
part. Stones impacted at external urethral meatus were
removed in emergency in 3 patients (15.7%) by meatotomy. In 6 patients (31.5%) with stone impacted in penile
shaft, initially supra-pubic catheterization was done to
relieve the acute symptom of urinary retention. Urethrolithotomy was then performed under general anaesthesia. During surgery an attempt was made to milk the
stone distally by instilling lubricant jelly. When procedure
remained unsuccessful, urethrolithotomy was done.
In cases where stone was clinically palpable, an urgent
examination under anaesthesia was planned. Where
urinary bladder was grossly palpable, size 16 cannula
was passed supra-pubically for decompression of urine
to relieve pain. The choice of further procedure was
dictated by location of stone and its gentle maneuvering
(milking) through urethra distally, after instilling xylocaine
jelly through urinary meatus facilitated by meatotomy. If
the procedure was unsuccessful, surgical exploration
(urethrolithotomy) was performed. In this procedure,
after taking proximal control of stone by fixing it between
index finger and thumb, an incision was made over the
calculus and stone was retrieved. Closure of periurethral
tissues was done over size 8 urethral tube with
polyglycolic 5/0 sutures applied in interrupted fashion,
taking care not to penetrate urethral mucosa. Urethral
tube remained in place for 7 days. After passage of urine
following removal of urethral tube, patients were discharged home, to be followed in outpatient department.
Calculi in bulbous (n = 3) and posterior urethral locations
(n = 7) were pushed back into the bladder. All patients
Figure 1: Stone impacted at external urinary meatus.
For stones located in bulbous and posterior urethra as
revealed by X-ray, gentle push back was done using size
8 Fr. urethral tube and stone was removed suprapubically by transvesical approach on elective list,
usually within 48 hours. Minimally invasive surgery was
not available in NICH. In cases where push back was
not successful a supra-pubic size 16 French cannula
was placed in palpable urinary bladder to drain urine and
vesicolithotomy was then scheduled at the earliest.
Bladder was drained for 48 hours after open procedure.
All stones were sent for chemical analysis.
Data were entered on a proforma and analyzed with
Statistical Package for Social Sciences (SPSS)
version 16. Descriptive analysis was performed. Mean
and standard deviation were calculated for variable like
age. Frequency and percentages were calculated for
parameters like gender, anatomical site, type of
procedure and complications.
Figure 2: Algorithm for management of impacted urethral stones.
Journal of the College of Physicians and Surgeons Pakistan 2012, Vol. 22 (8): 510-513
511
Jamshed Akhtar, Soofia Ahmed and Naima Zamir
did well except for one who developed retention of urine
after a week. This patient had urinary tract infection and
antibiotics were given. None of the patients had difficulty
in urination, urethrocutaneous fistula or development of
urethral stricture at follow-up. The chemical analysis of
stone showed all to be of calcium oxalate type. An
algorithm for the management of impacted urethral
stones based upon the results is shown in Figure 2.
DISCUSSION
The urinary tract calculi are prevalent in many regions of
the world. Extensive literature is found on both adult and
paediatric population, but surprisingly data on urethral
calculi is sparse. Few studies are available on the
subject from the stone belt region in children.9,10
Occasional case reports were also retrieved from
internet search, but no study can be found with a large
number of patients with any well-defined protocol for the
management of stones impacted in urethra without any
obstructive pathology.11,12 It thus becomes important to
contribute the data related to this infrequently addressed
condition which is extremely painful both for the children
and their families. Pain due to inability to pass urine is
described as one of the worst pain in humans. In this
study, 19 patients were managed in a span of 10
months. This number is quite high when compared with
overall frequency of stone disease in hospital based
studies from western countries.13 Even from the regional
countries like Turkey, Verit et al. reported only 8 patients
with urethral stone in a 6 years period.14 In 8 studies on
a large cohort of urinary tract calculi from pediatric
urological department in Pakistan, not a single case of
urethral calculus has been reported.15,16 The authors of
those studies concluded that upper urinary tract stones
are now increasingly reported in comparison with lower
urinary tract stone in Pakistan. These observations thus
may not be reflective of true picture from Pakistan. It
may be possible that patients with lower urinary tract
stones seek treatment in nearby facilities rather than
tertiary care hospitals.
Urethral calculi are divided into two types namely
primary (when formed within urethra due to some
anatomical defect) or secondary when stones from
upper urinary tract or bladder gets lodged into urethra.
These are called migratory stones. In a study on urethral
calculi from London in year 1930, 37 cases of secondary
urethral calculi were reported in a span of 20 years.17
While reporting on urinary calculi not much stress is
made on urethral calculi thus it is not clear as to the true
incidence and age distribution of this type of calculi. In
one study, it is reported that urethral calculi constitute
0.3% of all the urinary tract calculi.14
In the era of minimally invasive surgery, equipment has
been developed for treating urinary calculi at various
anatomical regions. For urethral calculi, use of Holmium
laser lithotripsy is reported in paediatric age group with
512
success.18 For those stones that can be pushed back
into bladder, minimally invasive surgery is another
option.19 The availability of the advanced equipment and
expertise remains an issue. The children are referred
from far flung areas and a more practical approach thus
would be an open surgical procedure, that can be used
by surgeons even at district level hospital. Simple pushback, meatotomy and urethrolithotomy procedures
suffice in this emergency situation. If surgical facilities
are not available supra-pubic decompression of urinary
bladder with large bore cannula is another option
before referring the child to a nearby facility where
operative procedure can be undertaken. Supra-pubic
decompression can be performed with commercially
available kit though it is difficult to obtain this even in an
urban region. This technique can be used if surgeon has
to buy time while waiting for availability of operation
suite and anaesthesia facility. In this study, bladder
decompression was employed as a bridging step by
using cannula to relieve the child from the agonizing
pain.
Urethrolithotomy needs attention to meticulous details of
closure of urethrotomy. Use of fine suture material,
urethral stent, and obtaining a water tight seal without
compromising blood supply of urethra are mainstay of
surgical approach. With observations of these surgical
principles chances of stricture and urethrocutaneous
fistula are negligible. In this series, no such complication
occurred. Interrupted sutures are equally effective in
achieving goals as noted in this study. In an oedematous
tissue at the site of impaction of stone, continuous
sutures may cut through easily.
The chemical analysis of the calculi revealed calcium
oxalate as a constituent in this series. Calcium oxalate
stones are commonly reported as most common type of
stones in many series though a change in pattern has
been observed, where similarities are reported with
developed countries both in terms of location and
chemical composition of calculi.20-22 Oxalates rich food
like dark green leafy vegetables should be avoided.
Vitamin C is another source of oxalate.23 Increase fluid
intake works in all types of stones. The data on role of
calcium intake is also controversial but it must be
remembered that calcium binds with oxalate in diet and
prevents its absorption from gastrointestinal tract. A
balanced diet is thus recommended with plenty of water
intake for prevention of recurrence of stones.24
CONCLUSION
Urethral stone is an important cause of acute retention
of urine in children. Anterior urethra is more frequent site
of obstruction. Variety of procedures can be employed to
relieve obstruction that does not require costly
equipment and surgery can be undertaken at peripheral
hospitals where operation theatre facility is available.
Journal of the College of Physicians and Surgeons Pakistan 2012, Vol. 22 (8): 510-513
Management of impacted urethral stones in children
REFERENCES
1.
Lpez M, Hoppe B. History, epidemiology and regional
diversities of urolithiasis. Pediatr Nephrol 2010; 25:49-59.
2.
Kit LC, Filler G, Pike J, Leonard MP. Paediatric urolithiasis:
experience at a tertiary care paediatric hospital. Can Urol Assoc J
2008; 2:381-6.
3.
Sharma AP, Filler G. Epidemiology of paediatric urolithiasis.
Indian J Urol 2010; 26:516-22.
4.
Asgari SA, Ghanaie MM, Simforoosh N, Kajbafzadeh A, Zare A.
Acute urinary retention in children. Urol J 2005; 2:23-7.
5.
Rizvi SA, Naqvi SA, Hussain Z, Hashmi A, Hussain M, Zafar MN,
et al. Management of paediatric urolithiasis in Pakistan:
experience with 1,440 children. J Urol 2003; 169:634-7.
6.
7.
8.
13. Nicoletta JA, Lande MB. Medical evaluation and treatment of
urolithiasis. Pediatr Clin North Am 2006; 53:479-91.
14. Verit A, Savas M, Ciftci H, Unal D, Yeni E, Kaya M. Outcomes of
urethral calculi patients in an endemic region and an undiagnosed primary fossa navicularis calculus. Urol Res 2006;
34:37-40. Epub 2006 Jan 24.
15. Rizvi SA, Naqvi SA, Hussain Z, Hashmi A, Hussain M, Zafar MN,
et al. Paediatric urolithiasis: developing nation perspectives.
J Urol 2002; 168:1522-5.
16. Rizvi SA, Sultan S, Ijaz H, Mirza ZN, Ahmed B, Saulat S, et al.
Open surgical management of paediatric urolithiasis: a developing
country perspective. Indian J Urol 2010; 26:573-6.
17. Debenham RK. Urethral calculi. Br J Urol 1930; 2:113-21.
Bedii SA. Urethral calculi in children. J Pediatr Surg 1996; 31:
1379-82.
18. Walker BR, Hamilton BD. Urethral calculi managed with
transurethral Holmium laser ablation. J Pediatr Surg 2001;
36:E16.
Eckstein HB, Kenanoglu A. Perforation of the urethra and
extravasation of urine caused by a calculus; report of two cases.
Lancet 1961; 7:20-2.
19. el-Sherif AE, Prasad K. Treatment of urethral stones by retrograde
manipulation and extracorporeal shock wave lithotripsy. Br J Urol
1995; 76:761-4.
Seltzer LG, Fischer WW, Miller SZ. Paediatric bladder outlet
obstruction due to urethral calculus: case report and review of
the literature. Pediatr Radiol 1993; 23:549-50.
20. Jahan Y, Akhtar J, Aziz A. Chemical analysis of urinary calculi in
children. J Surg Pak 2000; 5:8-9.
Aggour A, Ziada AM, AbdelHamid AZ, AbdelRahman S, Morsi A.
Metabolic stone composition in Egyptian children. J Pediatr Urol
2009; 5:132-5. Epub 2008 Dec 6.
21. Rizvi SA, Sultan S, Zafar MN, Ahmed B, Faiq SM, Hossain KZ,
et al. Evaluation of children with urolithiasis. Indian J Urol 2007;
23:420-7.
10. Prasongwatana V, Sriboonlue P, Suntarapa S. Urinary stone
composition in North-East Thailand. Br J Urol 1983; 55:353-5.
22. Alaya A, Najjar MF, Nouri A. Changes in stone composition
according to age in Tunisian paediatric patients. Int Urol Nephrol
2010; 42:621-8. Epub 2009 Nov 24.
9.
11. Murtaza B, Khan NA, Nadeem A, Saeed S. Combined
urethrolithotomy with vesicolithotomy in an 18-months old boy.
J Ayub Med Coll Abbottabad 2008; 20:138-40.
23. Saxena A, Sharma RK. Nutritional aspect of nephrolithiasis.
Indian J Urol 2010; 26:523-30.
12. Joshi P, Sarda D, Ahmad A, Gursev, Kothari P. Double dumb-bell
calculus in childhood. Afr J Paediatr Surg 2009; 6:122-3.
24. Finkielstein VA, Goldfarb DS. Strategies for preventing calcium
oxalate stones. Canadian Med Assoc J 2006; 174:1407-9.
l l l l l
l l l l l
Journal of the College of Physicians and Surgeons Pakistan 2012, Vol. 22 (8): 510-513
513
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Froz Rotator Cuff TendinitisDocument11 pagesFroz Rotator Cuff TendinitisestherNo ratings yet
- MCQ5FULL (Watermarked) PDFDocument164 pagesMCQ5FULL (Watermarked) PDFAbuMajedNo ratings yet
- Model of Heavy Work InvestmentDocument12 pagesModel of Heavy Work InvestmentaNo ratings yet
- Chemical Approval Form - Polintek Lining & ProtectionDocument2 pagesChemical Approval Form - Polintek Lining & ProtectionYosep SasadaNo ratings yet
- Stopbang in AsianDocument6 pagesStopbang in AsianwandapandabebeNo ratings yet
- Reporting MicroparaDocument3 pagesReporting MicroparaSuzzane MijoNo ratings yet
- Essay 3 Draft 2Document4 pagesEssay 3 Draft 2api-643529353No ratings yet
- Hygiene PolicyDocument4 pagesHygiene Policyprettyy chauhanNo ratings yet
- SCHEDULE S Nursing English SMSTR 4Document5 pagesSCHEDULE S Nursing English SMSTR 4RezhaNo ratings yet
- MX and Medico Legal AssignDocument14 pagesMX and Medico Legal AssignyeapgyNo ratings yet
- Stress Relief Reading - 424Document2 pagesStress Relief Reading - 424Laura TrifanNo ratings yet
- Psy 2300 Clinical Case 2 BDocument2 pagesPsy 2300 Clinical Case 2 BFaruse Ali0% (1)
- Vegetarianism: Presented By: Karen Yulieth Rojas Valencia Leidy Johana Tellez VelascoDocument17 pagesVegetarianism: Presented By: Karen Yulieth Rojas Valencia Leidy Johana Tellez VelascoJulietth RojasNo ratings yet
- A Review of Ethics For The Radiologic TechnologistDocument18 pagesA Review of Ethics For The Radiologic TechnologistEka Juliantara50% (2)
- Physical Education - Activity 2Document7 pagesPhysical Education - Activity 2Neil LayagueNo ratings yet
- Bea Case StudyDocument19 pagesBea Case StudyBea Flor Rapisura-PegadNo ratings yet
- Sample of Argumentative ArticleDocument4 pagesSample of Argumentative Articlelastnotes84No ratings yet
- PPI Durante Opeasi Okt'21Document36 pagesPPI Durante Opeasi Okt'21banyai90No ratings yet
- Case StudiesDocument2 pagesCase StudiesLLLJJJNo ratings yet
- STEAM INHALATION and NEBULIZATIONDocument4 pagesSTEAM INHALATION and NEBULIZATIONRenzo GabrielNo ratings yet
- Evaluation of California Non-Comprehensive Death File Against National Death IndexDocument14 pagesEvaluation of California Non-Comprehensive Death File Against National Death IndexCONSTANZA TERESA BERNA ARAYANo ratings yet
- Stroke Related Thesis TopicsDocument6 pagesStroke Related Thesis Topicskatrekahowardatlanta100% (2)
- Letter From Ottawa Public Health To Ottawa BusinessesDocument5 pagesLetter From Ottawa Public Health To Ottawa BusinessesCTV OttawaNo ratings yet
- Multipel Vulnus IncisivumDocument11 pagesMultipel Vulnus IncisivumDeaz CressendoNo ratings yet
- Note Ebshe - Osh Management System (2747)Document56 pagesNote Ebshe - Osh Management System (2747)Helo DixonNo ratings yet
- CSS IIApply Quality StandardsDocument17 pagesCSS IIApply Quality StandardsNordyl BianzonNo ratings yet
- Social Media Addiction and Its Impact On Pakistani 1Document12 pagesSocial Media Addiction and Its Impact On Pakistani 1arsalad.hameedNo ratings yet
- Panduka Jayakuru: Medical Writer Providence Business ServicesDocument14 pagesPanduka Jayakuru: Medical Writer Providence Business ServicesRajith PereraNo ratings yet
- Halcyon Brochure RAD10443B 092417Document14 pagesHalcyon Brochure RAD10443B 092417Anonymous 0TOLgQWuHvNo ratings yet
- Essay Outline (10133979)Document6 pagesEssay Outline (10133979)Shivu VermaNo ratings yet