Professional Documents
Culture Documents
Spirometra, Hymenolepis Nana
Uploaded by
JayricDepalobosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Spirometra, Hymenolepis Nana
Uploaded by
JayricDepalobosCopyright:
Available Formats
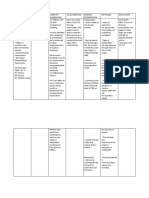
SPIROMETRA, H. NANA- DR.
ASUNCION November 19, 2014
SPIROMETRA
CASE:
A 61 year old man complained of on and off, dry,
non-productive cough for 2 months with
occasional dyspnea, intermittent low-grade fever,
anorexia, and weight loss. He was a smoker with
40 pack years. There is no history of CA or PTB in
the family. A chest x-ray revealed an abnormal
pulmonary shadow.
A CT scan of the lungs was further requested.
- Right upper lobe: 1-3 cm nodule
- Lower lobe of right lung: smaller nodule,
hyperechoic
- TB lesion on upper lung
Intraoperative findings showed minute nodules
with exudates on the surface of the parietal
pleura.
- wiry material larva embedded in the
parietal pleura of the lung
VATS biopsy (Video assisted thoracoscopy) in the
pleura and right upper and lower lobes was
performed
- Eosinophilic body (cut section of larval
parasite) embedded in pleura
Mononuclear cells
- Intense inflammatory reaction response
to parasite
Laboratory data revealed a 9000/cu. mm. WBC
count (normal) with slightly increased eosinophil
count (80%) and increased C-reactive protein
(ongoing inflammatory reaction).
Serum ELISA was taken several days after the
procedure and was tested positive for antiSparganum Antibody.
Disease: SPARGANOSIS
- similar to Diphyllobothria
- disease is associated with plerocercoid larva
(Spargana) in man
- Spirometra species
- Intermediate host: man
- Definitive host: dogs and cats, wild
carnivorous animals
Intermediate hosts:
1st: Cyclops (crustacean)
2nd: small rodents, snakes, frogs, fish, humans*
*Humans: 2nd intermediate host or paratenic (not
obligatory to life cycle) host
A. Branching Spargana
- Spirometra proliferum
- reported cases in Japan and US
- unknown morphology of adult worm and life
cycle
- larva: irregular, lateral, supernumerary
processes that bud off as new spargana in tissues
Diagnosis: larva in chylous, nodular lesions on
affected tissues (skin, subcutaneous tissues,
lungs)
B. Non-branching Spargana
- Spirometra mansoides
- Epidemiology:
- East and Southeast Asia, Japan, Indochina
- less encountered in Africa, Europe, North and
South America, and Africa
- humans acquire Sparganosis by:
- ingestion of infected Cyclops containing
procercoid in drinking water
- consuming fish, frogs, snakes, or rodents
harboring the plerocercoid
- penetration of cutaneous tissues
Adult Sperometra
- resembles Dyphillobothrium latum but smaller
in size
- ribbon-like flat body
Plerocerdoid (also known as Sparganum)
- often white
- varying size cm or mm in length
- ability to have very strong muscular activity
- ability to elongate or shorten
Egg
- similar to D. latum
- operculated
- longer, narrower
- more flattened on one side
SPIROMETRA, H. NANA- DR. ASUNCION November 19, 2014
Symptomatology
- local indurations, periodic giant urticaria,
edema, and erythema
- chills and fever
- high eosinophilia only larval form elicits
immune response
*outcome is always dependent on location of
parasite
Definitve Hosts: dogs and cats
LIFE CYCLE
unembryonated eggs discharged into moist
environment
eggs embryonate
hatch and release coracidium
coracidium is ingested by crustacean (similar
to D. latum)
crustacean harbors coracidium
coracidium transforms to procercoid
procercoid settles in body cavity of crustacean
crustacean is ingested by frog, fish, reptile,
or amphibian
procercoid transforms to plerocercoid
man accidentally ingests plerocercoid by
eating raw fish,
raw frog, raw snakes, raw rodents (O.o)
dead end infection
Pathogenicity
- found in any part of the body of man
* muscular contractility of sparganum causes
further inflammation and tissue damage
- eyes, subcutaneous and muscular tissue of
thorax, abdomen, thighs, inguinal region, thoracic
viscera
* most common thorax and abdomen
-migrate through tissues: inflammation and
edema of surrounding tissues
*chronicity but absence of fibrous tissue
deposition
continuously moves within affected tissues
unless calcified by chemotherapy
- degenerated larva: intense local inflammation
and necrosis
Cutaneous sparganosis
- pointed nodules = embedded Sparganum larva
encircles
Therapy: remove larva
- pruritic/painful nodule seen in subcutaneous
tissue, noed in extremities, trunk, genitalia,
breast
Ocular sparganosis
- infected eye
- encountered in Southeast Asia
- orbital edema, ptosis in affected eye
- pain, intense lacrimation of eye
- Treatment: remove Sparganum causing
inflammation and edema
Cerebral Sparganosis
CT Scan
-hyperechoic dense, wiry objects within brain
parenchyma
SPIROMETRA, H. NANA- DR. ASUNCION November 19, 2014
pathogenic for cerebral sparganosis
-not associated with ischemia or any organism
causing lesions
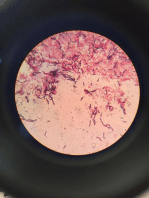
Histologic section:
intense
inflammatory
reaction around
affected area
DIAGNOSIS, TREATMENT, AND PREVENTION
Diagnosis:
- finding larvae in lesions
- not just based on clinical data
- best to look for larva
Treatment:
- surgical removal of larval plerocercoid
Prevention:
- In endemic areas: drinking water should be
boiled
or
filtered,
thorough
cooking
of
intermediate hosts (fish/frogs)
- use of protective equipment when handling
contaminated water
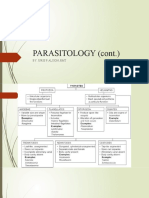
HYMENOLEPIS NANA
CASE:
A 6 year old boy experienced weight loss of about
5 kg and reported a periodic fever predominantly
at night time for 2 to 3 months. He also
complained of abdominal pain. No family history
of cancer.
Clinical examination showed multiple mobile,
non-tender submandibular lympg nodes with
maximum size of 1 x 1 cm. A solid, tender
epigastric mass extending to the umbilical region
was palpated. The abdomen was soft with no
organomegaly.
*epigastric to umbilicus = small intestine
Lab tests requested include: CBC, U/A, and
fecalysis. All were normal.
An abdominal UTZ showed presence of a mass 6
x 3 cm in size, located between the aorta and
superior mesenteric artery.
CT scan of the abdomen showed multiple,
integrated mesenteric lymph nodes with areas of
distended loops of small bowels with areas of
thickened wall.
Head CT scan was normal.
*ongoing
inflammation
distended
and
thickened
associated with chronic persistent infection
deposition of fibrous tissue
*enteritis distention of small bowels
Bone marrow aspiration and biopsy revealed
increased number of PMNs and eosinophils.
A repeat stool exam showed positive for nonoperculated eggs.
A repeat CBC was done and revealed mild
eosinophilia (10%).
probably parasitic infection
HYMENOLEPIS NANA
Disease: Dwarf tapeworm infection
Common name: dwarf tapeworm
Definitive host: humans, mice, rats
NO INTERMEDIATE HOST
Infective stage: embryonated egg
Epidemiology
- more than 20 million worldwide is infected
*increased number of cases reported in US
- younger age group is more affected
- transmission is dependent on immediate
contact
- hand to mouth
- contaminated food and water
- chief source of infection: humans
Adult: very short worm
- 200 proglottids; very short life span: several
days
Scolex of H. nana
-small globular scolex
- with rostellum (very
small)
- single ring of hooks
- 4 muscular suckers
- short, retractile
SPIROMETRA, H. NANA- DR. ASUNCION November 19, 2014
Proglottids
- broad than long
- 1 genital pore on lateral ends, usually lateral left
side
- 3 round testes
- bilobed ovary
*gravid proglottid: similar to other
Cyclophyllideans
- sacular uterus
- less eggs: <200 eggs within gravid uterus
- very short segment
Ova
- oval to globular
- 2 membranes enclosing embryo
- with 6 hooks (3 pairs)
hexacanth embryo
- thinner filaments (polar filaments/ thickenings)
- seen within embryo
- non-operculated
- embryonated (mature) when laid
LIFE CYCLE
proglottid ruptures in intestine
disseminate through apolysis
detach from main scolex, neck, immature
proglottids
attach to intestinal lumen
lays embryonated eggs
immediatedly infective once released into
environment
ingested by host (insect/rodent)
ingested by humans from contaminated food,
water,
hands
reaches small intestine and releases larva
another infection occurs in human host
*autoinfection is prominent
Infective stage: embryonated egg
Diagnostic stage: embryonated egg and
proglottids
Pathogenicity
- no intestinal mucosal damage
- light infections: asymptomatic or vague
abdominal disturbances
- fairly heavy infections: lack of appetite,
abdominal pain, diarrhea, anorexia, vomiting,
dizziness
due to elaborated byproducts of worm
- heavy infections: enteritis
DIAGNOSIS, TREATMENT, AND PREVENTION
Diagnosis:
Finding eggs, sometimes proglottids, in feces
Treatment:
SPIROMETRA, H. NANA- DR. ASUNCION November 19, 2014
DOC: Praziquantel 25 mg/kg SD
Alternative:
- Niclosamide 2 g (4 tabs) OD for 5 7 days
(adult)
o Children: 1 g OD for 5 days
- Paromomycin 45 mg/kg daily for 4 doses
with an hour interval per dose for 5 days
Prevention:
- Difficult
- Better hygiene practices
- eliminate sources: control rodents
- environmental sanitation prevent spread
You might also like
- Sample Child Dedication ProgramDocument1 pageSample Child Dedication ProgramJayricDepalobos100% (2)
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Document3 pages"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNo ratings yet
- Proceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964From EverandProceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964Augusto CorradettiNo ratings yet
- Clinical Pastoral OrientationDocument3 pagesClinical Pastoral OrientationJayricDepalobos100% (1)
- NCP 3rd YearDocument6 pagesNCP 3rd YearTotoro AblogNo ratings yet
- Ent Bcqs 2Document22 pagesEnt Bcqs 2Ghazi Uddin Ahmed100% (1)
- The Intestinal NematodesDocument107 pagesThe Intestinal Nematodesblue_blooded23100% (1)
- NematodesDocument9 pagesNematodesJessa MayNo ratings yet
- Blood Trematodes: Isna Indrawati Department of ParasitologyDocument30 pagesBlood Trematodes: Isna Indrawati Department of ParasitologyElisa Fata Marokeh TedadEspochachaNo ratings yet
- Untitled Document PDFDocument5 pagesUntitled Document PDFRizzy VillanuevaNo ratings yet
- Cestode SDocument49 pagesCestode SDiana CaceresNo ratings yet
- PG Notes 3Document29 pagesPG Notes 3Eliza SparkNo ratings yet
- Pott's SpineDocument47 pagesPott's Spinesigarun67% (3)
- Tables - CestodesDocument8 pagesTables - CestodesSid Loverholic50% (4)
- Classification of Medically Significant NematodesDocument134 pagesClassification of Medically Significant Nematodesblue_blooded23100% (1)
- Kuliah 17 - Nematoda Dan ProtozoaDocument72 pagesKuliah 17 - Nematoda Dan ProtozoaivaNo ratings yet
- Parasite Project BIOLOGY EditedDocument21 pagesParasite Project BIOLOGY EditedPadma CharanNo ratings yet
- Medical Parasitology - FullDocument30 pagesMedical Parasitology - FullJesse Osborn100% (2)
- Nematodes LabDocument57 pagesNematodes LabAlaa ZiyadNo ratings yet
- Female Reproductive System-AnatomyDocument57 pagesFemale Reproductive System-AnatomyEstellaNo ratings yet
- Q Bladder L1 +2Document14 pagesQ Bladder L1 +2youssef.aziz2020No ratings yet
- Lecture 3 para Summer 2023-1Document47 pagesLecture 3 para Summer 2023-1محمود سليمانNo ratings yet
- Intestinal NematodesDocument88 pagesIntestinal NematodesVincent Manganaan100% (1)
- TrematodesDocument10 pagesTrematodesUhjafwnuijhnfa Kmerkgoe100% (1)
- Phylum NematodaDocument285 pagesPhylum NematodaBrielleNo ratings yet
- Hymenolepis Nana Group 5 Write UpDocument7 pagesHymenolepis Nana Group 5 Write UpSusan GachukiaNo ratings yet
- Other AphasmidsDocument4 pagesOther AphasmidsJayricDepalobosNo ratings yet
- Pediatric Radiology ShortDocument95 pagesPediatric Radiology ShortNelly ChinelliNo ratings yet
- Trematodes 2Document37 pagesTrematodes 2Akanksha BaireddyNo ratings yet
- ParasitologyDocument4 pagesParasitologyJovanni andesNo ratings yet
- Helminths: NematodesDocument17 pagesHelminths: NematodesNicolle PanchoNo ratings yet
- Lecture 6 2023Document16 pagesLecture 6 2023ayaessam392002No ratings yet
- Kuliah Paragonimus WestermaniDocument17 pagesKuliah Paragonimus WestermaniIda Bagus Putu SwabawaNo ratings yet
- Tissue and Blood NematodesDocument53 pagesTissue and Blood NematodesVincent ManganaanNo ratings yet
- Platyhelminthes: Hazel Anne L. Tabo Olgga A. HaraDocument79 pagesPlatyhelminthes: Hazel Anne L. Tabo Olgga A. HaraHara OgheeNo ratings yet
- Inguinal Hernia: Dr. Amar Rathod M.S. (Ayurved)Document18 pagesInguinal Hernia: Dr. Amar Rathod M.S. (Ayurved)GAURAV0% (1)
- Scrotal Conditions: Done By: Enas Almazraway Sarah Al-HawamdehDocument65 pagesScrotal Conditions: Done By: Enas Almazraway Sarah Al-HawamdehMohammad GharaibehNo ratings yet
- Communicable DiseasesDocument162 pagesCommunicable DiseasesCarlo VigoNo ratings yet
- Parasitology Lec 3.01a Intestinal NematodesDocument16 pagesParasitology Lec 3.01a Intestinal NematodesEnaWahahaNo ratings yet
- Exercise 7 ParasitDocument6 pagesExercise 7 ParasitIvanNo ratings yet
- Phylum Nematoda PDFDocument257 pagesPhylum Nematoda PDFsummer dj100% (1)
- Branchial Cyst: DR Sowmya (PG in Ent)Document21 pagesBranchial Cyst: DR Sowmya (PG in Ent)drchinnaNo ratings yet
- TaeniasisDocument24 pagesTaeniasisDafne Maribel Hernandez HerreraNo ratings yet
- Trematodes (Flukes)Document35 pagesTrematodes (Flukes)api-3856362No ratings yet
- Trichinella and TrichurisDocument36 pagesTrichinella and TrichurisCristine BarrozaNo ratings yet
- Pneumocystis Carinii: Disease: PneumocystosisDocument20 pagesPneumocystis Carinii: Disease: PneumocystosisTharsini SalyamNo ratings yet
- Intussusception 161007042729 PDFDocument44 pagesIntussusception 161007042729 PDFDina MarselinaNo ratings yet
- Ancy Lost OmaDocument41 pagesAncy Lost OmaMuhmmad TahaNo ratings yet
- Introduction To Tromatodes: Phylum Platyhelminthes Class Trematoda Order DigeneaDocument104 pagesIntroduction To Tromatodes: Phylum Platyhelminthes Class Trematoda Order DigeneaFabian QuinteroNo ratings yet
- African Trypanosomiasis African Trypanosomiasis: Sleeping SicknessDocument65 pagesAfrican Trypanosomiasis African Trypanosomiasis: Sleeping SicknessdrgunavetNo ratings yet
- Pneumocystis Cariinii 1Document13 pagesPneumocystis Cariinii 1Tharsini SalyamNo ratings yet
- Trichinella SpiralisDocument2 pagesTrichinella SpiralisJayricDepalobosNo ratings yet
- The Fourier GangreneDocument39 pagesThe Fourier Gangreneomkar.rakomNo ratings yet
- Intestinal Parasitism: ProtozoansDocument10 pagesIntestinal Parasitism: ProtozoansdtimtimanNo ratings yet
- Testis and ScrotumDocument7 pagesTestis and Scrotumyoussef.aziz2020No ratings yet
- Paracytology Chart SummeryDocument15 pagesParacytology Chart SummeryOnSolomonNo ratings yet
- Anorectal Malformations: Presented by Khushveer KaurDocument91 pagesAnorectal Malformations: Presented by Khushveer KaurKataria DavinNo ratings yet
- Granulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)Document7 pagesGranulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)moosNo ratings yet
- Chapter 56 Liver & Lung TrematodesDocument24 pagesChapter 56 Liver & Lung TrematodesbartsnewNo ratings yet
- 8 Intestenal TrematodesDocument6 pages8 Intestenal Trematodesبلسم محمود شاكرNo ratings yet
- A Compilation of Cellular and Tissue Xenotransplantation Studies (1838-2022): A Promising Approach for the Treatment of DiseasesFrom EverandA Compilation of Cellular and Tissue Xenotransplantation Studies (1838-2022): A Promising Approach for the Treatment of DiseasesNo ratings yet
- Bill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341Document1 pageBill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341JayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- Shipping Confirmation 1264941Document1 pageShipping Confirmation 1264941JayricDepalobosNo ratings yet
- The LightDocument2 pagesThe LightJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Chapter 01 ChoicesDocument9 pagesChapter 01 ChoicesJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocument2 pagesWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNo ratings yet
- YHH Strategic Plan 2016-2017Document5 pagesYHH Strategic Plan 2016-2017JayricDepalobosNo ratings yet
- Acquaintance Party ParticipantsDocument1 pageAcquaintance Party ParticipantsJayricDepalobosNo ratings yet
- CAA Concert ProgramDocument2 pagesCAA Concert ProgramJayricDepalobosNo ratings yet
- Thalassemia: Presentor: Don Jayric DepalobosDocument19 pagesThalassemia: Presentor: Don Jayric DepalobosJayricDepalobosNo ratings yet
- Teen Parenting Brochure AssignmentDocument1 pageTeen Parenting Brochure AssignmentJayricDepalobosNo ratings yet
- Peer Evaluation For Group 5Document1 pagePeer Evaluation For Group 5JayricDepalobosNo ratings yet
- Acute Gastroenteritis: By: Madhavi Pandya Priyanka NandiDocument16 pagesAcute Gastroenteritis: By: Madhavi Pandya Priyanka NandiJayricDepalobosNo ratings yet
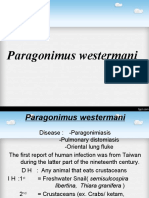
- Parasitology 18 Lung FlukesDocument25 pagesParasitology 18 Lung FlukesJayricDepalobosNo ratings yet
- Female BW - 3800 BL - 55 AS - 8,9 PA - 40Document3 pagesFemale BW - 3800 BL - 55 AS - 8,9 PA - 40JayricDepalobosNo ratings yet
- Microbiology Lecture Series Luz Gregoria Lazo-Velasco, MDDocument105 pagesMicrobiology Lecture Series Luz Gregoria Lazo-Velasco, MDJayricDepalobos100% (1)
- Basic Physical Examination in ENT PDFDocument44 pagesBasic Physical Examination in ENT PDFJayricDepalobosNo ratings yet
- Department of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017Document1 pageDepartment of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017JayricDepalobosNo ratings yet
- Prevalencia de Ulcera Gastrica en Caballos Con Colico EquinoDocument7 pagesPrevalencia de Ulcera Gastrica en Caballos Con Colico EquinoMaria Paula DuqueNo ratings yet
- Tinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanDocument7 pagesTinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanSatriadwykiyprasetya ThiodwkiyNo ratings yet
- Typhoid Fever WorkupDocument13 pagesTyphoid Fever WorkupPlot BUnniesNo ratings yet
- COMER Handoutslides Ch07Document33 pagesCOMER Handoutslides Ch07Ty BakrNo ratings yet
- Test Bank For Acquiring Medical Language 2nd Edition by JonesDocument44 pagesTest Bank For Acquiring Medical Language 2nd Edition by JonesArthur Robinson100% (38)
- Pathological Anatomy IntroductionDocument9 pagesPathological Anatomy IntroductionRashid NawazNo ratings yet
- GOING TO THE DOCTOR (Body and Health) : VocabularyDocument2 pagesGOING TO THE DOCTOR (Body and Health) : VocabularyDiana CuleaNo ratings yet
- Case Ana-Hypothyroidism 2020Document7 pagesCase Ana-Hypothyroidism 2020Nicole cuencosNo ratings yet
- Sleep Apnea PDFDocument257 pagesSleep Apnea PDFdantevermillion100% (6)
- Anesthesia Books 2016 BLS BasicDocument5 pagesAnesthesia Books 2016 BLS BasicVinay KumarNo ratings yet
- Ophthalmology ImpDocument12 pagesOphthalmology Imp074 Jeel PatelNo ratings yet
- 490.082 Microsite PublicDocument16 pages490.082 Microsite PublicA.J. YounesNo ratings yet
- Deficiencies of Water Soluble VitaminsDocument20 pagesDeficiencies of Water Soluble Vitaminsbpt2No ratings yet
- Lasa High Alert PelayananDocument6 pagesLasa High Alert PelayananUlfa ErviliaNo ratings yet
- Endocrinology OSCEDocument17 pagesEndocrinology OSCEswamy rao100% (1)
- How Humor Heals Public Speech SampleDocument1 pageHow Humor Heals Public Speech SampleRene ChuaNo ratings yet
- Medication Information For Parents and Teachers: Atomoxetine-StratteraDocument8 pagesMedication Information For Parents and Teachers: Atomoxetine-StratteraMonique WrightNo ratings yet
- Normal Spontaneous Delivery Case StudyDocument5 pagesNormal Spontaneous Delivery Case StudyJerwin Ogoy50% (10)
- Trauma VascularDocument30 pagesTrauma Vascularblip blip blooop0% (2)
- Pgy Git AssigmentDocument6 pagesPgy Git Assigmentlawrence mulengaNo ratings yet
- Bacteriology by Dhshan Hassan DhshanDocument48 pagesBacteriology by Dhshan Hassan Dhshanعلي الكوافي100% (1)
- Factors Affecting Stability of OrthodontDocument7 pagesFactors Affecting Stability of OrthodontSALAHEDDINE BLIZAKNo ratings yet
- (10920684 - Neurosurgical Focus) Factors Associated With Survival in Patients With MeningiomaDocument17 pages(10920684 - Neurosurgical Focus) Factors Associated With Survival in Patients With MeningiomaDarlene LebasteNo ratings yet
- CHN Lecture - 2Document13 pagesCHN Lecture - 2HANNAH LEAL RENDAJE SHARIFFNo ratings yet
- English For Nursing 2: Vocational English Teacher's BookDocument17 pagesEnglish For Nursing 2: Vocational English Teacher's BookSelina Nguyễn VuNo ratings yet
- 234 240 PDFDocument7 pages234 240 PDFlegivethNo ratings yet
- Pathophysiology of Upper Gastrointestinal BleedingDocument1 pagePathophysiology of Upper Gastrointestinal BleedingkimmybapkiddingNo ratings yet
- Whole Spine MriDocument2 pagesWhole Spine MriImg UsmleNo ratings yet