Professional Documents
Culture Documents
Neuroprotection of Medical IOP-Lowering Therapy
Uploaded by
Irvin MarcelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuroprotection of Medical IOP-Lowering Therapy
Uploaded by
Irvin MarcelCopyright:
Available Formats
Cell Tissue Res (2013) 353:245251
DOI 10.1007/s00441-013-1671-1
REVIEW
Neuroprotection of medical IOP-lowering therapy
Norbert Pfeiffer & Julia Lamparter & Adrian Gericke &
Franz H. Grus & Esther M. Hoffmann & Jochen Wahl
Received: 7 May 2013 / Accepted: 27 May 2013 / Published online: 9 July 2013
# Springer-Verlag Berlin Heidelberg 2013
Abstract Intraocular pressure (IOP)-lowering therapy has
been shown to arrest or retard the progression of optic
neuropathy typical for glaucoma and can, thus, be described
as neuroprotective. At present, six classes of medical therapy
are employed, namely parasympathomimetics, alpha/betasympathomimetics, -blockers, carbonic anhydrase inhibitors, 2-adrenergic receptor agonists and prostaglandin analogues. For several of these substances, some experimental
evidence exists of a possible neuroprotective mechanism,
beyond their IOP-lowering activity. -Blockers are involved
in the up-regulation of brain-derived neurotrophic factor
(BDNF) and can decrease glutamate-mediated NMDA receptor activation. Not only systemic but also topical carbonic
anhydrase inhibitors are able to increase retinal blood flow.
2-Adrenergic receptor agonists can up-regulate the formation of BDNF and anti-apoptotic factors. Prostaglandin analogues increase blood flow to the eye, possibly including the
retina. To date, evidence for a neuroprotective effect independent of IOP regulation in human glaucoma is scarce and
has only been shown to be likely for the 2-adrenergic
receptor agonist, brimonidine.
Keywords Neuroprotection . Intraocular pressure (IOP) .
IOP-lowering medication . Glaucoma
Introduction
Glaucoma is best described as a progressive optic neuropathy
of various origins. A loss of retinal ganglion cells and their
axons is accompanied by loss of visual function ultimately
leading to severe visual impairment and even blindness. At
N. Pfeiffer (*) : J. Lamparter : A. Gericke : F. H. Grus :
E. M. Hoffmann : J. Wahl
Department of Ophthalmology, Johannes Gutenberg-University,
Langenbeckstrasse 1, 55131 Mainz, Germany
e-mail: Norbert.Pfeiffer@unimedizin-mainz.de
present, glaucoma is thought to be the most common cause of
irreversible blindness worldwide. No uniformly accepted definition of glaucoma exists but most definitions involve optic
nerve damage being described as the cupping of the optic
nerve head with a typical appearance distinctly different from
other forms of optic neurodegeneration. This degeneration
also corresponds to a typical centripetal loss of the visual field.
Although by no means mandatory, an increased intraocular pressure (IOP) plays a critical role in the majority of
cases. Normal IOP is described statistically by the mean of
a normal population, which in most populations corresponds
to about 1315 mmHg plus/minus twice the standard deviation (roughly 45 mmHg). However, a large variety of vulnerability to increased IOP is now understood to occur and
glaucomatous damage might appear not only at high IOPs
but also at IOPs in the normal range or even at statistically
low pressures indicating a role of other pathomechanisms
and not IOP alone. To date, glaucoma therapy has been limited
to the lowering of IOP. Thus, for a long time, the success of
therapy has usually been measured as a decrease in IOP. Only
lately have clinical studies focused on the retardation or arrest
of the progressive loss of optic nerve structures as measured
by morphometric methods or image analysis and/or visual
function as measured by white on white perimetry. Interest
has also increased in exploring medical glaucoma therapies
with respect to their neuroprotective potential beyond their
IOP-lowering capacity. This paper reviews the potential of
medical therapy to act as neuroprotective therapy by the
lowering of IOP or by other mechanisms or by both.
Understanding glaucoma and IOP-lowering treatment
A multitude of diseases are called glaucoma. Glaucoma
might be primary or secondary, in the latter case as a result of
other ocular or systemic diseases. The most prevalent form
of glaucoma is primary open angle glaucoma (POAG),
246
which, in Europe, accounts for more than 90 % of glaucoma
cases. The over-all prevalence of glaucoma is about 1 %.
However, its incidence increases sharply starting at the age
of 40 years and doubles every decade. In some populations,
the prevalence in the old age group of >85 years has been
found to be well over 15 %. Worldwide, over 60 million
individuals are estimated to be affected by glaucoma. This
figure will possibly rise to 80 million by 2020. For 2010,
about 6.7 million individuals were estimated to be totally
blind from the disease (Quigley and Broman 2006).
As about one third of glaucoma patients do not show IOPs
beyond the defined normal limits, most definitions suggest
increased IOP as being a major risk factor for developing
POAG but not as the sole cause of it. Patients that have never
had elevated IOPs but develop typical signs and symptoms
of glaucoma are usually termed as having normal tension
glaucoma (NTG).
A number of other risk factors such as race, myopia,
intake of corticosteroids, thin central corneal thickness and
a first-degree relative with glaucoma have been identified as
being associated with a higher risk of glaucoma development. However, to date, of all risk factors, IOP remains the
only modifiable and treatable risk factor for the development
and progression of glaucoma. The association of glaucoma
and increase of IOP had been noted for centuries but was
rediscovered about 150 years ago, amongst others, by
Albrecht von Graefe. Since then, the lowering of IOP was
assumed to be sufficient to stop disease progression. Hence,
various types of medical therapy and surgeries were invented
and applied to glaucoma patients. However, the usefulness of
IOP-lowering therapy was challenged as a vast proportion of
glaucoma patients were observed to have a progression of
glaucoma damage in spite of lowered IOPs. Explanations for
this paradox include the observation that some glaucoma
patients do not comply with their therapies but also that other
local or systemic factors trigger and promote the onset and
progression of glaucoma.
Large randomised studies have only recently been
conducted in order to establish whether the lowering of
IOP by either surgical or medical therapy does indeed stop
or at least retard the progression of POAG and its variants.
Such therapy that prevents the deterioration of retinal ganglion cells might be regarded as neuroprotective.
Effect of IOP-lowering therapy: landmark studies
Heijl and collaborators (2002) established in the Early
Manifest Glaucoma Trial (EMGT) that the treatment of individuals with early signs of glaucoma led to a slower progression of glaucoma than if individuals were left untreated.
The authors concluded that a reduction of IOP by 1 mmHg
would reduce the risk of progression by about 10 %.
Cell Tissue Res (2013) 353:245251
Two groups investigated whether the treatment of individuals with increased IOP but without signs of glaucoma, usually termed ocular hypertension (OHT), would prevent the
onset of POAG. The results were contradictory: Kass and
colleagues (2002) showed that, over an observation period
of 5 years, the rate of individuals progressing from OHT to
glaucoma without treatment was 9.5 %, whereas medical
treatment reduced this to 4.4 % (Ocular Hypertension
Treatment Study, OHTS). On the other hand, the European
Glaucoma Prevention Study (EGPS) failed to show such an
effect in a statistically significant proportion of participants
(Miglior et al. 2007). However, the two studies were substantially different: the EGPS had a randomised and, in addition, a
double-masked design, whereas in contrast, the OHT treatment trial was unmasked. The EGPS involved treatment with
one agent only, namely dorzolamide, whereas the OHTS
allowed multiple treatments. The double-masked EGPS
abolished observer bias. However, such a masked design did
not allow for adaptive treatment to reach a certain IOP target.
This, however, was the case with the OHTS in which medications were added until a certain IOP target had been reached.
Thus, the IOP-lowering effect in the OHTS was much greater
than that in the EGPS. Indeed, the neuroprotective effect of
IOP-lowering therapy seems to be dose-dependent considering the results from the EMGT, EGPS and OHTS thereby
emphasising the role of the lowering of IOP.
In general, surgical therapy leads to greater IOP reductions than medical therapy. Both the Advanced Glaucoma
Intervention Study and the Collaborative Glaucoma
Treatment Study (AGIS and CIGTS) have demonstrated a
larger protective effect for greater IOP reductions and lower
IOPs. Data from the AGIS have also suggested that visual
fields of glaucoma patients tend to remain highly stable if
their IOPs always range under 18 mmHg.
Most interesting are the results from the Low-pressure
Glaucoma Study Group (Krupin et al. 2011). This group
showed, in a series of observations, that the lowering of
IOP did indeed retard the progression of glaucoma, even if
previous untreated IOPs had never been elevated beyond the
range of IOP considered to be the normal. However, NTG is
thought to be a disease entity of its own, as numerous distinct
differences exist between NTG and POAG, including the
more frequent occurrence of optic disc haemorrhages, a high
prevalence of migraine, Raynauds syndrome or systemic
hypotension in NTG.
In summary, the lowering of IOP has been shown either to
prevent or at least to retard the onset of POAG. Moreover,
the lowering of IOP slows the progression of established
open angle glaucoma with either high IOP or even normal
IOP. Furthermore, the effects seem to be dose-dependent
with the lower IOPs offering better protection from the
progression of glaucoma than higher IOPs. Thus, the lowering of IOP may be regarded as neuroprotective in glaucoma.
Cell Tissue Res (2013) 353:245251
Neuroprotective mechanisms different from lowering
IOP
While IOP-lowering has now been established as neuroprotective
in glaucoma, other mechanisms have also been discussed.
Improvement of ocular perfusion could play an important
role in glaucoma treatment. Since the description of POAG,
a constant debate has raged about the pathophysiological mechanisms and also the appropriate therapy. Amongst others, the
mechanical hypothesis stressing the role of elevated IOP
and the perfusion hypothesis favouring a role of impaired
perfusion of the eyeball have been advocated. The typical
cupping of the optic nerve in glaucoma has been attributed
to mechanical stress at the lamina cribrosa giving way to
increased pressure inside the eye ball. On the other
hand, failure to stop the disease by the lowering of
IOP has lead to the hypothesis that the loss of retinal
nerve fibres could be attributable to, for example, the
reduced perfusion of critical tissues including the optic
nerve head. This controversy is by no means new.
Priestley Smith wrote in 1879: The truth of the matter
appears to be, that the glaucomatous cup is not a purely
mechanical result of exalted pressure, but is in part at
least, an atrophic condition which, though primarily due
to pressure, includes vascular changes and impaired nutrition
in the area of the disc and around its margin which require a
considerable time for their full development.
Since then and more recently, other mechanisms have
been considered to explain glaucomatous damage on a cellular or even subcellular level. A critical role has been
attributed to functional axonal transport (Anderson and
Hendrickson 1974; Minckler et al. 1976, 1977; Quigley
et al. 1981; Hollander et al. 1995; Burgoyne et al. 2005).
Increased IOP would possibly reduce normal axoplasmic
flow and, hence, transport and retrograde transport, for example, of brain-derived neurotrophic factor (BDNF) from
the synapse of the retinal ganglion cells to the cell body itself
in the retina. Thus, apart from modifying IOP and ocular
perfusion, drugs might directly affect the retinal ganglion
cell or other cell types such as glial cells (Son et al. 2010).
Again, ocular perfusion might also play a crucial role and
impaired ocular blood flow might have a critical part in the
pathogenesis of POAG (Yoshida et al. 2010; Harris et al.
1999; Bathija 2000; Zhao and Cioffi 2000). Finally, rather
than a direct effect of ischaemia, an ischaemic insult might
trigger a glutamate induced N-methyl-D-aspartate (NMDA)mediated exitotoxicity (Hiraoka et al. 2003; Kuehn et al.
2005; Rokicki et al. 2007; Osborne et al. 1999).
Some debate can be followed in the literature over whether
IOP-lowering medical therapy can address one or several of
these effects in the treatment of glaucoma. Whereas the effect
on IOP can be easily measured, a potential neuroprotective
effect is much more difficult to establish.
247
Drugs that lower IOP
Drugs that lower IOP in the order in which they became
available for glaucoma treatment are the parasympathomimetics, sympathomimetics, carbonic anhydrase inhibitors,
-adrenergic receptor antagonists, 2-adrenergic receptor
agonists and prostaglandin analogues (Table 1).
Parasympathomimetics
Parasympathomimetics such as pilocarpine were the mainstay of glaucoma treatment for about a century. They lower
IOP by increasing aqueous humor outflow. This is mediated
by the constriction of the smooth muscle tissue of the ciliary
body leading to the opening of the trabecular meshwork
and Schlemms canal. Their IOP-lowering capacity is about
20 % of initial IOP. Because of their side effects of
constricting the pupil and of inducing myopia in younger
individuals, their use is limited. Evidence is lacking for a
neuroprotectie mechanism beyond their IOP-lowering
potential.
Sympathomimetics
Sympathomimetics are now used very rarely. They produce
not only a vasoconstriction of conjunctival vessels
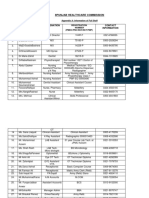
Table 1 Classes of IOP-lowering drugs and typical examples of these
drugs
Class
Examples
Parasympathomimetics
Pilocarpine
Carbachol
Adrenaline
Dipivalyl-epinephrine
Carteolol
Timolol
Betaxolol
Metipranolol
Levobetaxolol
Acetazolamide
Sympathomimetics
-Adrenergic receptor antagonists
Carbonic anhydrase inhibitors
Doclophenamide
Dorzolamide
Brinzolamide
2-Adrenergic receptor agonists
Prostaglandin analogues
Clonidine
Apraclonidine
Brimonidine
Unoprostone
Latanoprost
Travoprost
Bimatoprost
Tafluprost
248
immediately after topical application to the ocular surface
but also a reactive vasodilation. Moreover, their IOPlowering capacity is limited to only about 15 %20 % of
initial IOP. Worldwide, they are now almost out of use. At
present, they are not available in Europe and North America.
However, they show an interesting mechanism of action. In
part, they lower IOP by reducing the content of the glycosaminoglycans that are found in abundance in the trabecular
meshwork of the human aqueous outflow system.
Glycosaminoglycans seem to be increased in steroidinduced glaucoma (Johnson et al. 1990). Thus, sympathomimetics might be an interesting treatment alternative for this
secondary form of glaucoma. Intrinsic activity at both - and
-adrenergic receptors would offer potential effects on the
regulation of vasodilation. However, this has not been investigated in human glaucoma.
Carbonic anhydrase inhibitors
Carbonic anhydrase inhibitors lower IOP by blocking the
enzyme carbonic anhydrase, which is one of the three key
enzymes that are essential for the production of the aqueous
humour. Apart from their ophthalmic use carbonic anhydrase
inhibitors are weak diuretics and are only used in some
neurological disorders including mountain sickness at high
altitudes and pseudotumor cerebri. Both systemic and topical
carbonic anhydrase inhibitors inhibit carbonic anhydrase II,
which is the isoenzyme that has a major role in aqueous
humour production, which takes place in the ciliary body
epithelium in the posterior chamber. Via this mechanism,
IOP is reduced (Sugrue 2000). In addition, carbonic
anhydrase inhibitors have an influence on the buffer system
of the body. They reduce pH and hence appear to induce
vasodilation (Okazawa et al. 2001; Reitsamer et al. 2009;
Torring et al. 2009; Martinez and Sanchez-Salorio 2009).
Vasodilation in turn increases retinal perfusion (Pedersen
et al. 2005). These mechanisms might lead to an additive
neuroprotective effect beyond IOP control (for a review, see
Shih and Calkins 2012). However, the effect of carbonic
anhydrase inhibitors has not yet been shown to be superior
to other similar IOP-lowering drugs in humans. The IOPlowering effect of oral carbonic anhydrase inhibitors can be
large. Unfortunately, chronic use of the stronger systemic
carbonic anhydrase inhibitors, such as acetazolamide, is
often limited by a large spectrum of side effects including
hypokalaemia, formation of stones in the urinary tract, diuresis, pronounced sickness and aplastic anaemia. Topical
carbonic anhydrase inhibitors (dorzolamide, brinzolamide)
exhibit a much lighter spectrum of side effects. However,
because of the necessity to block >99 % of carbonic
anhydrase to lower IOP, both the duration of action and
maximal effect are limited.
Cell Tissue Res (2013) 353:245251
-Adrenergic receptor antagonists
After their introduction into ophthalmology, topical blockers quickly gained pole position in the topical treatment of glaucoma, because of their relatively mild topical
side effects. The pressure-lowering effect is roughly 25 % of
the initial IOP value and is achieved by reducing aqueous
humour production by blocking adenylate-cyclase, one of
the key enzymes of aqueous humour production. Even when
applied topically, -blockers have a considerable spectrum
of systemic side effects including systemic hypotension,
reduction of heart rate and limitation of maximal heart rate
and, potentially most dangerous, induction of bronchial constriction and asthma. Apart from the IOP-lowering effect,
several studies have suggested an indirect neuroprotective
effect of this class of substance. Betaxolol is a selective 1adrenoceptor antagonist (Cheon et al. 2003). Following
ischaemic reperfusion injury, its application exhibits a protective effect against the loss of cells from the inner plexiform layer. Timolol is a rather non-selective 1- and 2adrenoceptor antagonist. In an experimental glaucoma model in the rat, timolol had a neuroprotective effect for retinal
ganglion cells (Seki et al. 2005). The mechanism by which
-blockers are neuroprotective is uncertain. However, it
might be linked to the regulation of both calcium and sodium
channels, which play a role in the release of glutamate and,
further along the pathway, of NMDA receptors (Osborne
et al. 1997, 2004; Wood et al. 2003). Levobetaxolol appears
to be even more active, possibly by an additional upregulation of BDNF in the retina (Wood et al. 2001).
Debate continues as to whether the influence of blockers on vascular tone is neuroprotective or counterproductive. Betaxolol has been shown to increase the speed
of blood flow in the human optic nerve head. Unfortunately,
this has not been demonstrated to alter the course of
glaucoma.
2-Adrenergic receptor agonists
This group comprises mainly three substances, namely clonidine, apraclonidine (only marketed in some countries) and,
as the latest addition, brimonidine. All lower IOP by reducing aqueous humour production via the inhibition of
adenylate-cyclase, which leads to decreased cAMP levels.
In addition, they have also been shown to increase
uveoscleral outflow (Ogidigben et al. 1994; Toris et al.
1999). 2-Adrenergic receptor agonists have been used as
IOP-lowering drugs but, for a long time, interest has been
shown in a possible additional neuroprotective mechanism.
2A-Adrenergic receptors are present in the non-pigmented
ciliary epithelium and probably, thus, contribute to the regulation of aqueous humour dynamics. 2B-Adrenergic receptors are localised in axons, dendrites and glia. Finally,
Cell Tissue Res (2013) 353:245251
2C-Adrenergic receptors are found in photoreceptors
(Woldemussie et al. 2007).
Brimonidine and other 2-adrenergic receptor agonists
have shown promise as being neuroprotective, as has been
demonstrated by a variety of models, especially in the optic
nerve crush model (Wheeler et al. 1999; Yoles et al. 1999;
Pinar-Sueiro et al. 2011). Thus, brimonidine has been suggested also to be neuroprotective in glaucoma (Saylor et al.
2009). At this time, brimonidine is the only agent for which a
positive neuroprotective effect has been shown to occur in
human glaucoma.
Further evidence has been produced from the Lowpressure Glaucoma Study Group (Krupin et al. 2011). The
investigators randomised their patients into two groups. The
first group was treated with topical brimonidine, whereas the
second group was treated with topical timolol, a nonselective IOP-lowering -blocker. IOP lowering was similar
in both treatment groups. However, the preservation of visual function as measured by white on white perimetry was
better in the brimonidine group. The authors concluded that
brimonidine might preserve visual function by a mechanism
that is not described by IOP lowering alone but, at least in
part, by another mechanism beyond this, i.e., it has a
neuroprotective effect in its own right.
The possible underlying mechanism for such a
neuroprotective effect is not known. Brimonidine has been
shown to up-regulate BDNF in retinal ganglion cells (Gao
et al. 2002). However, brimonidine has various other effects
and side effects that might be involved in such mechanisms.
Nevertheless, for the time being, it remains the only topical
glaucoma therapy for which a possible neuroprotective effect
other than the lowering of IOP alone has been demonstrated
in human glaucoma.
Prostaglandin analogues
Prostaglandin analogues were introduced into ophthalmology about 12 years ago. They quickly gained widespread
acceptance for various reasons. They are very powerful
IOP-lowering agents. In contrast to topical -blockers and
-adrenergic medications, they have next to no systemic side
effects. Moreover, they need to be applied only once daily,
which appears to enhance patient compliance considerably.
Pressure-lowering effects of most of the agents is about
25 %30 % of initial IOP with the exception of unoprostone,
which is much less powerful. This drug is now mainly
marketed in Japan. Prostaglandin analogues are also considered to be the most powerful of all IOP-lowering drugs.
Local side effects include ocular hyperaemia, inflammation,
ocular intolerance and possibly ocular surface disease.
Lengthening of eye lashes and irreversible darkening of the
iris at the moment are considered as rather intriguing but
otherwise probably harmless side effects.
249
Prostaglandin analogues lower IOP by increasing
uveoscleral outflow. However, recent evidence also suggests
that they increase conventional outflow via the trabecular
meshwork and Schlemms canal. In addition, a direct
neuroprotective effect has been shown by Kanamori et al.
(2009) who demonstrated that retinal ganglion cells are
protected from apoptosis both in vitro and in vivo by this
drug. Moreover, glutamate toxicity seems to be antagonised
by latanoprost (Zheng et al. 2011; Nakanishi et al. 2006).
Another suggestion is that a direct neuroprotective (antiapoptotic) effect might be induced by the protein kinase
pathway triggering neurite outgrowth and caspase-3 inhibition. Additionally, prostaglandin analogues can induce vasodilation possibly leading to increased ocular perfusion. In
spite of the worldwide use of prostaglandin analogues and
the plethora of literature, no evidence has been presented to
date for a neuroprotective effect of prostaglandin analogues
in humans, apart from their IOP-lowering capacity.
Concluding remarks
Glaucoma appears to be an enigma. When first described, it
was thought to be a disease that was precipited by increased
IOP attributable to various origins inducing the cupping of
the optic disc purely by mechanical stress. However, almost
at the same time, the idea was conceived that glaucoma
might be a primary optic nerve disease that makes it only
more prone to respond to risk factors such as increased IOP.
Indeed, good arguments for both views can still be made.
OHT is about eight times more prevalent than glaucoma.
This is a condition in which IOP is increased above normal
limits but optic nerve damage does not occur or has not
occurred as yet. A mechanism leading to glaucoma independent of IOP is supported by the observation that some patients present with typical optic disc cupping and a typical
loss of visual function on perimetry but have apparently
never had elevated IOP.
Only recently, studies have demonstrated convincingly
that the lowering of ocular pressure seems to be helpful in
all conditions: in patients with elevated IOP and
glaucomatous optic nerve cupping, in patients with such
nerve cupping without elevated IOP and finally also in individuals with elevated IOP. Under IOP-lowering treatment,
patients develop glaucoma less frequently. Thus, the lowering of IOP by means of medication and probably also by
surgical therapy appears to be neuroprotective for the optic
nerve in the human eye.
A multitude of pharmacological substances have been
shown to have neuroprotective properties in various models
including those that concern the optic nerve. Some of them
also lower IOP, which, for example, in the case of the optic
nerve crush injury model, probably does not play a major
250
role. Of all topical or systemic pressure-lowering agents that
are nowadays used in the treatment of human glaucoma, only
brimonidine appears to have a mechanism that is independent of IOP lowering and neuroprotective for the optic nerve
in human glaucoma. The evidence is not complete.
Brimonidine treatment is superior over either timolol or
argon-laser-trabeculoplasty treatment, although both timolol
and argon-laser trabeculoplasty treatment exhibit an equal or
greater IOP-lowering effect. However, timolol, for example,
has well-known systemic side effects including bradycardia
and systemic hypotension, which are present in many patients that receive topical timolol therapy. Thus, the IOPlowering neuroprotective effect might be counter-acted by
reduced ocular perfusion caused by systemic hypotension or
bradycardia. Such a systemic effect has not been described
for argon-laser trabeculoplasty. Again, a topical side effect
such as intraocular inflammation caused by laser treatment
might counter-act the IOP-lowering effect of that laser procedure. However, the eventual establishment of a
neuroprotective effect in human glaucoma will need to come
from large randomised studies in patients with wellphenotyped glaucoma and sufficient (>5 years) follow-up
with both morphometric measurements of the optic nerve
and functional test endpoints.
References
Anderson DR, Hendrickson A (1974) Effect of intraocular pressure on
rapid axoplasmic transport in monkey optic nerve. Invest
Ophthalmol 13:771783
Bathija R (2000) Optic nerve blood flow in glaucoma. Clin Exp Optom
83:180184
Burgoyne CF, Downs JC, Bellezza AJ, Suh JK, Hart RT (2005) The
optic nerve head as a biomechanicl structure: a new paradigm for
understanding the role of IOP-related stress and strain in the
pathophysiology of glaucomatous optic nerve head damage.
Prog Retin Eye Res 24:3973
Cheon EW, Park CH, Kang SS, Cho GJ, Yoo JM, Song JK, Choi WS
(2003) Betaxolol attenuates retinal ischemia/reperfusion damage
in the rat. Neuroreport 14:19131917
Gao H, Qiao X, Cantor LB, WuDunn D (2002) Up-regulation of brainderived neurotrophic factor expression by brimonidine in rat retinal ganglion cells. Arch Ophthalmol 120:797803
Harris A, Chung HS, Ciulla TA, Kagemann L (1999) Progress flow and
relevance to our understanding of glaucoma and age-related macular degeneration. Prog Retin Eye Res 18:669687
Heijl A, Leske MC, Bengtsson B, Hymann L, Hussein M (2002)
Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol
120:12681279
Hiraoka M, Inoue K, Ninomiya T, Takada M (2003) Ischaemia in the
Zinn-Haller circle and glaucomatous optic neuropathy in macaque
monkeys. Trans Am Ophthalmol Soc 101:163269
Hollander H, Makarov F, Stefani FH, Stone J (1995) Evidence of
constriction of optic axons at the lamina cribrosa in the normotensive eye in humans and other mammals. Ophthalmic Res 27:296
309
Cell Tissue Res (2013) 353:245251
Johnson DH, Bradley JMB, Acott TS (1990) The effect of dexamethasone on glycosaminoglycans of human trabecular meshwork in
perfusion organ culture. Invest Ophthalmol Vis Sci 31:25682571
Kanamori A, Naka M, Fukuda M, Nakamuta M, Negi A (2009)
Latanoprost protects rat retinal ganglion cells from apoptosis
in vitro and in vivo. Exp Eye Res 88:535541
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL,
Miller JP, Parrish RK 2nd, Wilson MR, Gordon MO (2002) The
Ocular Hypertension Treatment Study: a randomized trial determines that tropical ocular hypotensive medication delays or prevents the onset of privary open-angle glaucoma. Arch Ophthalmol
120:701713
Krupin T, Liebmann JM, Greenfield DS, Ritch R, Gardiner S (2011) A
randomized trial of brimonidine versus timolol in preserving visual function: results from the Low-Pressure Glaucoma Treatment
Study. Am J Ophthalmol 151:671681
Kuehn MH, Fingert JH, Kwon YH (2005) Retinal ganglion cell death in
glaucoma: mechanisms and neuroprotective strategies.
Ophthalmol Clin North Am 18:383395
Martinez A, Sanchez-Salorio M (2009) A comparison of the long-term
effects of dorzolamide 2% and brinzolamide 1%, each added to
timolol 0.5%, on retrobulbar hemodynamics and intraocular pressure in open-angle glaucoma patients. J Ocul Pharmacol Ther
25:239248
Miglior S, Pfeiffer N, Torri V, Zeyen T, Cunha-Vaz J, Adamsons I
(2007) Predictive factors for open-angle-glaucoma among patients
with ocular hypertension in the European Glaucoma Prevention
Study. Ophthalmology 114:39
Minckler DS, Tso MO, Zimmerman LE (1976) A light microscopic,
autoradiographic study of axoplasmic transport in the optic nerve
head during ocular hypotonie, increased intraocular pressure, and
papilledema. Am J Ophthalmol 82:741757
Minckler DS, Bunt AH, Johanson GW (1977) Orthograde and retrograde axoplasmic transport during acute ocular hypertension in the
monkey. Invest Ophthalmol Vis Sci 16:426441
Nakanishi Y, Nakamura M, Mukuno H, Kanamori A, Seigel GM, Negi
A (2006) Latanoprost rescues retinal neuro-glial cells from apoptosis by inhibiting caspase-3 which is mediated by p44/p42
migenactivated protein kinase. Exp Eye Res 83:11081117
Ogidigben M, Chu TC, Potter DE (1994) Alpha-2-adrenoceptor mediated changes in aqueous dynamics: effect of perussis toxin. Exp
Eye Res 58:729736
Okazawa H, Yamauchi H, Sugimoto K, Toyoda H, Kishibe Y,
Takahashi M (2001) Effects of acetazolamide on cerebral blood
flow, blood volume, and oxygen metabolism: a positron emission
tomography study with healthy volunteers. J Cereb Blood Flow
Metab 21:14721479
Osborne NN, Cazervieille C, Carvalho AL, Larsen AK, DeSantis L
(1997) In vivo and in vitro experiments show that betaxolol is
retinal neuroprotective agent. Brain Res 751:113123
Osborne NN, Ugarte M, Chao M, Chidlow G, Bae JH, Wood JP, Nash
MS (1999) Neuroprotection in relation to retinal ischemia and
relevance to glaucoma. Surv Ophthalmol 43(Suppl 1):S102S128
Osborne NN, Wood JP, Chidlow G, Casson R, DeSantis L, Schmidt KG
(2004) Effectiveness of levobetaxolol and timolol at blunting
retinal ischaemia is related to their calcium and sodium blocking
activities: relevance to glaucoma. Brain Res Bull 62:525428
Pedersen DB, Koch Jensen P, Cour M la, Kiilgaard JF, Eysteinsson T,
Bang K, Wiencke AK, Stefnsson E (2005) Carbonic anhydrase
inhibition increases retinal oxygen tension and dilates retinal vessels. Graefe Arch Clin Exp Ophthalmol 243:163168
Pinar-Sueiro S, Urcola H, Rivas MA, Vecino E (2011) Prevention of
retinal ganglion cell swelling by systemic brimonidine in a rat
experimental glaucoma model. Clin Exp Ophthalomol 39:799807
Priestley Smith J (1879) Glaucoma:its causes, symptoms, pathology,
and treatment. Churchill, London
Cell Tissue Res (2013) 353:245251
Quigley HA, Broman AT (2006) The number of people with glaucoma
worldwide in 2010 and 2020. Br J Ophthalmol 90:262267
Quigley HA, Addicks EM, Greenn WR, Maumence AE (1981) Optic
nerve damage in human glaucoma. II. The site of injury and
susceptibility to damage. Arch Ophthalmol 99:635649
Reitsamer HA, Bogner B, Tockner B, Kiel JW (2009) Effects of
dorzolamide on chorioidal blood flow, ciliary blood flow, and aqueous production in rabbits. Invest Ophthalmol Vis Sci 50:23012307
Rokicki W, Dorecka M, Romaniuk W (2007) Retinal ganglion cells
death in glaucomamechanism and potential treatment. Part II.
Klin Oczna 109:353355
Saylor M, Mc Loon LK, Harrison AR, Lee MS (2009) Experimental and
clinical evidence for brimonidine as an optic nerve and retinal
neuroprotective agent: an evidence-based review. Arch Ophthalmol
12:402406
Seki M, Tanaka T, Matsuda H, Togano T, Hashimoto K, Ueda J, Fukuchi
T, Abe H (2005) Topically adminstered timolol and dorzolamide
reduce intraocular pressure and protect retinal ganglion cells in a rat
experimental glaucoma model. Br J Ophthalmol 89:504507
Shih GC, Calkins DJ (2012) Secondary neuroprotective effects of
hypotensive drugs and potential mechanisms of action. Expert
Rev Ophthalmol 7:161-175
Son JL, Soto I, Oglesby E, Lopez-Roca T, Pease ME, Quigley HA,
Marsh-Armstrong N (2010) Glaucomatous optic nerve injury involves early astrocyte reactivity and late olig dendrocyte loss. Glia
58:780789
Sugrue MF (2000) Pharmocological and ocular hypotensive properties of
topical carbonic anhydrase inhibitors. Prog Retin Eye Res 19:87112
Toris CB, Camras CB, Yablonski ME (1999) Acute versus chronic
effects of brimonidine on qqueous humor dynamics in ocular
hypertensive patients. Am J Ophthalmol 128:814
251
Torring MS, Holmgaard K, Hessellund A, Aalkjaer C, Bek T (2009)
The vasodilating effect of actazolamide and dorzolamide involves
mechanisms other than carbonic anhydrase inhibition. Invest
Opthalmol Vis Sci 50:345351
Wheeler LA, Lai R, Woldemussie E (1999) From the lab to the clilnic:
activation of an alpha-2 agonist pathway is neuroprotective in
models of retinal and optic nerve injury. Eur J Ophthalmol 9
(Suppl 1):S17S21
Woldemussie E, Wijono M, Pow D (2007) Localization of alpha 2
receptors in ocular tissues. Vis Neurosci 24:745756
Wood JP, DeSantis L, Chao HM, Osborne NN (2001) Topically applied
betaxolol anttenuates ischaemia-induced effects to the rat retina
and stimulates BDNF mRNA. Exp Eye Res 72:7986
Wood JP, Schmidt KG, Melena J, Chidlow G, Allmeier H, Osborne NN
(2003) The beta-adrenoceptor antagonists metipranolol and timolol are retinal neuroprotectants: comparison with betaxolol.Exp
Eye Res 76:505-516
Yoles E, Wheeler LA, Schwartz M (1999) Alpha-2 adrenoreceptor
agonists are neuroprotective in a rat model of optic nerve degeneration. Invest Ophthalmol Vis Sci 40:6573
Yoshida Y, Sugiyama T, Utsunomiya K, Oguta Y, Ikeda T (2010) A
pilot study for the effects of donepezil therapy on cerebral and
optic nerve head flow, visual field defect in normal-tension glaucoma. J Ocul Pharmacol Ther 26:187192
Zhao DY, Cioffi GA (2000) Anterior optic nerve microvascular
changes in human glaucomatous optic neuropathy. Eye
(Lond) 14:445449
Zheng J, Feng X, Hou L, Cui Y, Zhu L, Ma J, Xia Z, Zhou W, Chen H
(2011) Latanoprost promotes neurote outgrowth in differentiated
RGC-5 cells via the PI3K-Akt-mTOR signalling pathway. Cell
Mol Neurobiol 31:597604
You might also like
- Barriers To Identifying Occupational Asthma Among Primary Healthcare Professionals: A Qualitative StudyDocument11 pagesBarriers To Identifying Occupational Asthma Among Primary Healthcare Professionals: A Qualitative StudyIrvin MarcelNo ratings yet
- Astigmatism - Definition, Etiology, Classification, Diagnosis and Non-Surgical TreatmentDocument18 pagesAstigmatism - Definition, Etiology, Classification, Diagnosis and Non-Surgical TreatmentIrvin MarcelNo ratings yet
- Mild Cognitive Impairment in Clinical Practice: A Review ArticleDocument11 pagesMild Cognitive Impairment in Clinical Practice: A Review ArticleIrvin MarcelNo ratings yet
- Pain Definitions and Concepts I ANZCA Blue Book Text P2 CH4 29Document5 pagesPain Definitions and Concepts I ANZCA Blue Book Text P2 CH4 29Irvin MarcelNo ratings yet
- Cognitive Impairment: Classification and Open Issues: Mini ReviewDocument7 pagesCognitive Impairment: Classification and Open Issues: Mini ReviewIrvin MarcelNo ratings yet
- Toxicology Letters: Pesticides, Cognitive Functions and Dementia: A ReviewDocument31 pagesToxicology Letters: Pesticides, Cognitive Functions and Dementia: A ReviewIrvin MarcelNo ratings yet
- Correlation Between Serum 25-Hydroxyvitamin D Levels and Severity of Atopic Dermatitis in ChildrenDocument5 pagesCorrelation Between Serum 25-Hydroxyvitamin D Levels and Severity of Atopic Dermatitis in ChildrenIrvin MarcelNo ratings yet
- Dermatitis Atópica Guideline 2014 Aad PDFDocument29 pagesDermatitis Atópica Guideline 2014 Aad PDFAnghelo Aldair Velásquez CarrilloNo ratings yet
- The Roles of Sex Hormones in The Course of Atopic DermatitisDocument21 pagesThe Roles of Sex Hormones in The Course of Atopic DermatitisIrvin MarcelNo ratings yet
- Wang 2014Document6 pagesWang 2014Irvin MarcelNo ratings yet
- Simonsen 2013Document8 pagesSimonsen 2013Irvin MarcelNo ratings yet
- Intestinal Obstruction2014ReviewDocument8 pagesIntestinal Obstruction2014ReviewCésar Dedios FernándezNo ratings yet
- Atopic Dermatitis Natural History, Diagnosis, and Treatment (2014) PDFDocument8 pagesAtopic Dermatitis Natural History, Diagnosis, and Treatment (2014) PDFBeny Pratama SidabutarNo ratings yet
- Vitamin D Level and Supplementation in Pediatric Atopic Dermatitis: A Randomized Controlled TrialDocument6 pagesVitamin D Level and Supplementation in Pediatric Atopic Dermatitis: A Randomized Controlled TrialIrvin MarcelNo ratings yet
- Accepted Manuscript: 10.1016/j.neuint.2017.01.005Document42 pagesAccepted Manuscript: 10.1016/j.neuint.2017.01.005Irvin MarcelNo ratings yet
- 7 Surgical - Menopause After Effect SymptomsDocument5 pages7 Surgical - Menopause After Effect SymptomsIrvin MarcelNo ratings yet
- Journal Atopic Dermatitis PDFDocument8 pagesJournal Atopic Dermatitis PDFJundi Agung SamjayaNo ratings yet
- Forensic Photography: Prospect Through The Lens: Eview RticleDocument3 pagesForensic Photography: Prospect Through The Lens: Eview RticleIrvin MarcelNo ratings yet
- Accepted ManuscriptDocument12 pagesAccepted ManuscriptIrvin MarcelNo ratings yet
- Ross 2014Document8 pagesRoss 2014Irvin MarcelNo ratings yet
- Acute Phase Reactants: Inflammation and Risk of StrokeDocument22 pagesAcute Phase Reactants: Inflammation and Risk of StrokeIrvin MarcelNo ratings yet
- Standard Management Options For Rosacea: The 2019 Update by The National Rosacea Society Expert CommitteeDocument10 pagesStandard Management Options For Rosacea: The 2019 Update by The National Rosacea Society Expert CommitteeIrvin MarcelNo ratings yet
- Effect of Symptoms of DJDJDDocument6 pagesEffect of Symptoms of DJDJDIrvin MarcelNo ratings yet
- Barington 2017Document10 pagesBarington 2017Irvin MarcelNo ratings yet
- Body Plethysmography e Its Principles and Clinical Use: ReviewDocument16 pagesBody Plethysmography e Its Principles and Clinical Use: ReviewIrvin MarcelNo ratings yet
- Doshi 2018Document7 pagesDoshi 2018Irvin MarcelNo ratings yet
- Ileus in Adults: MedicineDocument11 pagesIleus in Adults: MedicineAmanda PutriNo ratings yet
- Ileus in Adults: MedicineDocument11 pagesIleus in Adults: MedicineAmanda PutriNo ratings yet
- BJS5 1 30Document9 pagesBJS5 1 30Irvin MarcelNo ratings yet
- Bet 3 022Document5 pagesBet 3 022Irvin MarcelNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Mucocele 5Document4 pagesMucocele 5Devi Alfiani100% (1)
- Theories of Counseling and Psychotherapy A CaseDocument25 pagesTheories of Counseling and Psychotherapy A Casedaffdg dsfNo ratings yet
- Occipital NeuralgiaDocument12 pagesOccipital NeuralgiaStudentNo ratings yet
- 10 Surprising Health Benefits of HoneyDocument5 pages10 Surprising Health Benefits of Honeykarina chaswinNo ratings yet
- CBT WorkshopDocument52 pagesCBT WorkshopKhoa Le Nguyen100% (13)
- Generalized Anxiety Disorder: Timothy A. Brown Tracy A. O'Leary David H. BarlowDocument55 pagesGeneralized Anxiety Disorder: Timothy A. Brown Tracy A. O'Leary David H. BarlowCamila JoaoNo ratings yet
- Comprehensive Cognitive-Behavior TherapyDocument106 pagesComprehensive Cognitive-Behavior Therapypsihologice100% (4)
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-447388856No ratings yet
- JCI Reference Guide WRDocument55 pagesJCI Reference Guide WRSanjeev Chougule100% (1)
- Psych Midterm ExamDocument6 pagesPsych Midterm Examteabagman100% (3)
- No Nama Obat Sediaan Dosis Indikasi Dewasa Anak: 2 Yr: 12 mg/kg/24Document6 pagesNo Nama Obat Sediaan Dosis Indikasi Dewasa Anak: 2 Yr: 12 mg/kg/24JovitaNo ratings yet
- The Coping Cat Program For Anxious YouthDocument10 pagesThe Coping Cat Program For Anxious YouthDeepika BhandariNo ratings yet
- A Brief Introduction To HypnotherapyDocument10 pagesA Brief Introduction To HypnotherapyEndy MulioNo ratings yet
- 2015E Updated GuidelinesDocument1,269 pages2015E Updated GuidelinesYipno Wanhar El MawardiNo ratings yet
- 00 Statistical Report 2016Document248 pages00 Statistical Report 2016wudthipanNo ratings yet
- Oleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Document40 pagesOleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Mbenk NjoeNo ratings yet
- Galvanic Current: by Anisa Altaf 18205 Presented To DR Daniyal Baig ElectrotherapyDocument27 pagesGalvanic Current: by Anisa Altaf 18205 Presented To DR Daniyal Baig ElectrotherapyArsal MushtaqNo ratings yet
- Fractures of Radius and Ulnar Shaft: Dima HabanjarDocument56 pagesFractures of Radius and Ulnar Shaft: Dima HabanjarDima HabanjarNo ratings yet
- 4 Powerful Eye Exercises For Rapidly Improving Your VisionDocument8 pages4 Powerful Eye Exercises For Rapidly Improving Your VisionDoraemon Noby100% (1)
- 1026 FullDocument5 pages1026 FullMuhammad Yufimar Rizza FadilahNo ratings yet
- Vergo 16: Betahistine Dihydrochloride Tablet 16 MGDocument4 pagesVergo 16: Betahistine Dihydrochloride Tablet 16 MGmegha_okztNo ratings yet
- Violet Oaklander MOdelDocument212 pagesViolet Oaklander MOdelNerea F GNo ratings yet
- Nominal RollDocument11 pagesNominal RollMuhammad FarooqNo ratings yet
- Autocoid PharmacologyDocument29 pagesAutocoid PharmacologyLyadelou Fortu100% (1)
- Preventative StrategiesDocument23 pagesPreventative Strategiesnegel shanNo ratings yet
- Active Movement and Passive Movement (Compatibility Mode)Document3 pagesActive Movement and Passive Movement (Compatibility Mode)drhemangNo ratings yet
- Abnormal Illness BehaviorDocument7 pagesAbnormal Illness Behavioransha2011p0% (1)
- Julia H Bartlett ResumeDocument3 pagesJulia H Bartlett Resumeapi-484975401No ratings yet
- Pharmacology RepeaterDocument5 pagesPharmacology RepeaterMarium JavedNo ratings yet
- Peptic Ulcer DiseaseDocument3 pagesPeptic Ulcer DiseasePhilip SimanganNo ratings yet