Professional Documents
Culture Documents
9 - Chapter 1. The Components of Quality in Health Care PDF
Uploaded by
Juanna SoehardyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
9 - Chapter 1. The Components of Quality in Health Care PDF
Uploaded by
Juanna SoehardyCopyright:
Available Formats
1
The Components of Quality in
Health Care
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
t is possible to conceive of quality as the product of two factors. One
is the science and technology of health care, and the second is the
application of that science and technology in actual practice. The
quality of care achieved in practice is the product of these two. As is
shown in Figure 1.1, that product can be characterized by several attributes that include efficacy, effectiveness, efficiency, optimality, acceptability, legitimacy, and equity. These, taken singly or in a variety of combinations, constitute a definition of quality and, when measured in one
way or another will signify its magnitude.
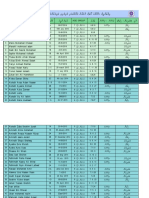
As a prelude to what is to follow, I give in Table 1.1 brief definitions
of each of the attributes of quality that I have just mentioned. A more
detailed, but concise, description follows.
Efficacy
Efficacy is the ability of the science and technology of health care to
bring about improvements in health when used under the most favorable
circumstances. Some further considerations should be noted.
First, it is not always possible to specify what "the most favorable
circumstances" I have postulated are. Therefore, it is possible to substitute
"under specified circumstances" for the vaguer concept of "most favorable."
Second, it follows from what I have just said that efficacy is the
standard against which any improvement in health achieved in actual
practice is to be compared. As suggested in Figure 1.1, efficacy is not
itself subject to monitoring when the quality of practice is being assessed.
Rather, it is given to us, a priori, as a product of research, experience,
and professional consensus.
Third, as I show in Figure 1.1, the science and technology of health
care set the standard not only for efficacy but for the other attributes of
quality as well. This means that actual performance in all its aspects is
compared to what our science and technology, at its best, is expected to
achieve. This formulation has a consequence also alluded to in Figure
1.1. It requires that "science and technology" be defined broadly to in-
The Components of Quality in Health Care
Figure 1.1. Components of quality in health care.
elude not only biological factors but the behavioral sciences as well. It is
true that these sciences may not be, as yet, sufficiently developed to offer
us clear guidelines and precise standards. It is hoped, however, that they
will be able to do so as they mature. And finally, we should remember
that not all standards of performance derive from what we are accustomed
to call "science and technology." Some standards are set by social and
individual preferences, and some others by ethical and moral considerations.
Effectiveness
Effectivenessss isis the degree to which improvements in health now attainable are, in fact, attained. This implies, as I have already said, a compar-
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
Table 1.1. Components of Quality: Definitions
1. EFFICACY
The ability of the science and technology of health care to bring about improvements
in health when used under the most favorable circumstances.
2. EFFECTIVENESS
The degree to which attainable improvements in health are, in fact, attained.
3. EFFICIENCY
The ability to lower the cost of care without diminishing attainable improvements in
health.
4. OPTIMALITY
The balancing of improvements in health against the costs of such improvements.
5. ACCEPTABILITY
Conformity to the wishes, desires, and expectations of patients and their families.
6. LEGITIMACY
Conformity to social preferences as expressed in ethical principles, values, norms, mores,
laws, and regulations.
7. EQUITY
Conformity to a principle that determines what is just and fair in the distribution of
health care and its benefits among members of the population.
ison between actual performance and the performance that the science
and technology of health care, ideally or under specified conditions, could
be expected to achieve. This formulation is presented graphically in Figure 1.2.
To simplify my presentation, I assume in Figure 1.2 that we have in
mind a mostly self-limiting disease; for example, a moderately severe upper respiratory infection, not threatening to life. On the ordinate axis I
have a measure of health status; for example, the ability to perform the
activities of daily living. On the abscissa is plotted the passage of time.
The Components of Quality in Health Care
Figure 1.2. Graphical presentation of effectiveness in a self-limiting disease.
As the figure shows, the person in question (or the average of a group
of persons) begins with a specified level of health close to "wellness."
When illness strikes, as shown by the solid line in the figure, health
deteriorates for a while and then, because the disease has been assumed
to be self-limiting, begins to improve, finally attaining a level similar to
that present at the beginning.
With this formulation, the area A in Figure 1.2 represents the effect
of treatment. Areas A and B combined represent the effect of the best
treatment. Effectiveness can now be represented by the fraction (A) -j- (A
+ B), which is the ratio of the health improvement achieved in actual
practice to the health improvement that could have been achieved had
the best treatment been given. Effectiveness is, therefore a relative concept, which can be defined as follows:
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
Improvements in health expected
from the care to be assessed
Relative httectiveness =
Improvements in health to be expected
from the "best" (or "standard" care)
In this regard, it is important to note a number of considerations.
1. Figure 1.2 is offered as only one example among several that
could be constructed. It could be, for example, easily modified to
represent a progressive disease or one characterized by remissions
and relapses. In each case the comparison would be between what
is actually achieved and what, under better circumstances, could
have been achieved.
2. According to this formulation, effectiveness is only relative to what
the science and technology of health care can accomplish. At any
given time it is limited by that capacity; and as that capacity improves, the standard against which effectiveness is to be judged is
raised accordingly. Clearly, the notion of "continuous improvement" is built into the model, even if some have not seen it.
3. The model, and consequently, the meaning and measure of effectiveness (and of quality as a whole) depend on how one defines
and measures health. Given only partial concepts and measures
of health, one obtains correspondingly partial measures of effectiveness; with inclusive concepts and measures of health, one obtains similarly inclusive measures of effectiveness.
4. The model represents probabilities, not certainties. We measure
the effectiveness of care not by what has occurred in any given
case, or a small number of cases, but by what we can expect to
occur if an adequate sample of cases were to receive a specified
kind of care. If in any given case a practitioner gives care that is
known to give the best results on the average in that kind of case,
the care is judged to have been good even if that particular patient
experiences little improvement, suffers complications, or even
dies.
5. The model requires, if it is to be fully implemented, a great deal
of information that, alas, is often not available. Very often there
The Components of Quality in Health Care
are no good measures (or even agreed-upon definitions) of health
status; the course of untreated illness is often unknown; what "the
best treatment" means or can achieve is equally obscure; and even
what happens under actual treatment in groups of patients is imperfectly documented. These deficiencies, when the model reveals them, should stimulate clinical trials and epidemiological
studies to rectify them.
While we wait for more complete information, we can use
less-rigorous but still useful measures of effectiveness. Instead of
an inclusive measure of health, we could use a specific symptom
or sign such as cough or dyspnea in asthmatics, or a set of blood
pressure readings in hypertensives. We could compare the improvement in health during corresponding illnesses receiving different kinds of treatment.
6. When resources are limited we may have to set two (or more than
two) standards of comparison. One would be what is achievable
with the best use of the resources actually at hand. Another could
be what would be achieved with the best use of resources we
need, and would like to have. The object is to set immediate goals
while we aim for what is better in the future.
Efficiency
"Efficiency" is the ability to lower the cost of care without diminishing
attainable improvements in health. Expressed as an equation:
Improvements in health expected
from the care to be assessed
Efficiency =
1 he cost ot that care
This means that efficiency is increased if, for a given cost, health improvement is increased or if the same degree of health improvement is
attained at a lower cost. It follows that the mere reduction in cost does
not denote efficiency unless health benefits are either unaffected or are
improved.
10
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
There are three ways of improving efficiency in health care.
1. One way is for health-care practitioners to prescribe and implement care that does not include harmful, useless, or less effective
remedies or methods. This kind of efficiency I have called clinical
efficiency because it depends on clinical knowledge, judgment
and skill.
2. Another way of improving efficiency is to produce more efficiently
the goods and services that are used in providing care. For example, costs are lowered if a hospital is run at a higher occupancy
rate, or if a nurse is not asked to do things that an aide or secretary
could do just as well. Perhaps one could also include in this
category changes in procedure (for example for the preparation
and administration of drugs) that reduce the frequency of errors
that might cause injury to health and, consequently, higher costs.
This kind of efficiency I have called production efficiency.y It has
also been called managerial efficiency y because it depends on organizational and managerial decisions in which clinicians do not
play the decisive role. It should be recognized, nevertheless, that
without the participation and consent of clinicians, some of these
changes would be difficult to introduce.
3. Still another way of making care more efficient is to distribute it
among different classes of patients (characterized by age, sex, ethnicity, economic status, place of residence, kind of illness, etc.)
in a way proportionate to expected improvements in health. In
other words, resources are allocated to population subgroups who
are perhaps sicker or are more likely to benefit from care, and do
so for longer periods of time, and at proportionately lower cost.
By doing so one aims for what is called "distributional efficiency."
This is, as we shall see, an aspect of quality at the societal level.
To cite specific, documented examples of these three kinds of efficiency would take us too far afield in a brief review such as this book is
meant to be. But because clinical efficiency is so closely allied to patient
care, I shall mention a few illustrative examples.
The Components of Quality in Health Care
11
The literature contains many examples of the effort to devise new
strategies of care that lower cost while outcomes remain unchanged or
even improve. A recent report demonstrates that, by codifying rules that
guide the physical examination of patients who have suffered injuries of
the ankle or foot, it is possible to reduce the number of X-ray examinations
of these parts by 30% without causing harm. The resulting savings, assuming this procedure were universally adopted, is estimated at $150 million for the United States.'
Still another study has demonstrated the consequences of implementing a procedure (which the investigators call a critical pathway) for
managing patients who seek care for "community acquired pneumonia."
The procedure or protocol in question specifies how the severity of the
pneumonia is to be judged, which patients are to be admitted to the
hospital and which treated at home, the treatment to be given in each of
these two places, and, for hospitalized patients, when the patient is judged
ready to be discharged. It is estimated that, without injury to patients, the
cost to the hospital is reduced by $1,700 per patient, an amount thought
to be much greater than the added cost of treatment at home.4
Optimality
Optimality is the balancing of improvements in health against the cost of
such improvements. This definition implies that there is a "best" or "optimum" relationship between costs and benefits of health care, a point
below which more benefits could be obtained at costs that are low relative
to benefits, and above which additional benefits are obtained at costs too
large relative to corresponding benefits.
Figure 1.3 will help illustrate this somewhat abstract concept. To
generate the figure it is necessary to engage in a "mental experiment": an
experiment rather difficult to duplicate in actual practice, but nonetheless
one from which emerges a fundamental principle very relevant to medical
practice and social policy.
To begin with, we assume that we have an ideal physician, one who
has perfect knowledge of both health-care improvements and cost. This
Figure 1.3. Hypothetical relations between health benefits and costs of progressively more elaborate care, when care is clinically most efficient.
12
The Components of Quality in Health Care
13
physician is, furthermore, a person who will never prescribe unnecessary
care. This physician is given successively larger sets of resources to use in
health care. The upper panel in Figure 1.3 shows that if the physician
has nothing to work with, there is no improvement in health (referred to
as "benefits" in the figure) that could be attributed to care. But as the
physician receives more resources (obviously costing more) progressively
more improvements can be achieved. Accordingly, the curve of improvements attributable to care rises, as does cost, except that improvements
rise faster than costs do. Subsequently, however, as more and more resources are available to the physician, the improvements, though they
continue to occur, become relatively smaller and smaller. Eventually,
there comes a point when no further improvements can be obtained no
matter what resources are available to the physician. At this point, the
"ideal physician" recognizes that no further improvement can be accomplished and will not call for additional resources. "Maximally effective"
care has been achieved.
In the lower part of Figure 1.3 there is an attempt to compare improvements in health against the cost of these improvements. To make
such a comparison, we must express costs and improvements in corresponding units of measurement, perhaps dollars.
When health improvements are translated to their corresponding
equivalents they are called benefits, as the figure shows. How this conversion can be made, and precisely how benefits and costs are compared,
is a subject to be taken up in health economics. Here I only assume that
it can be done in a socially acceptable manner. And to simplify the matter
further, I only subtract costs from benefits. When this is done, there is a
point in the lower graph that corresponds to the matching two points in
the graph in the upper pane of the figure. The curve thus generated goes
upward to a point and then begins to decline. It goes upward as long as
additional benefits exceed additional costs. It goes downward when additional benefits are smaller than additional costs. The point of inflection
represents "optimally effective" care.
I provide Table 1.2 as a partial illustration of the notion of optimality.
The table shows some findings of a study of the costs and effects of pneumococcal vaccination. 5 On the left-hand side of the top panel are the net
Table 1.2. Cost-Effect Estimates for Pneumococcal Vaccination
Cost (Dollars)
Losses
Added cost of vaccination
Effects (Quality-adjusted Years)
Gains
Gains
Losses
Reduced cost of
caring for pneumonia
Increased quality of
life as a result of
prevention of
pneumonia
Added cost of caring for complications of vaccination
Reduced quality of
life as a result of
complications of
vaccination
Cost of treatment
of illnesses other
than pneumonia
as a result of
extended life
Increased life
expectancy as a
result of avoiding
death from pneumonia
Discounted at 5% annually
Vaccination Age
2-4
5-24
25-44
45-64
65 plus
Reduced quality of
life as a result of
extended life
Measured as quality-adjusted years of life
(as follows) and discounted at 5%
annually
Death
= 0.0
Bed disability = 0.4
Other disability = 0.6
Full function = 1 . 0
Net Effect: Quality-adjusted
Days per Person Vaccinated
Cost per Quality-adjusted
Year of Life
0.05
0.07
0.15
0.43
1.59
$77,200
35,300
22,900
5,700
1,000
From Willems et al., "Cost effectiveness of vaccination against pneumococcal pneumonia," New England
}. ofMed. 303: 553-559, September 4, 1980.
14
The Components of Quality in Health Care
15
costs of vaccination. These are the losses caused by vaccination minus
the financial gains from the procedure. Note, in particular, that if persons
do not die of pneumonia and as a result live longer and consequently
incur other costs due to illness, this is counted as loss attributed to vaccination. This attribution illustrates an important principle: namely, that
improvement in quality can result in added costs because of resulting
longevity.
The 5% discount rate applied to the monetary gains and losses of
vaccination embodies still another principle or presumption advanced by
economists: namely, that losses and gains further and further in the future
have a progressively lower value to persons living in the present. It is not
clear how much lower that value is. The figure of 5% is a conventional
estimate, the rationale for which I shall not attempt to describe.
In the right-hand portion of Table 1.2 the effects of vaccination are
shown. These appear as both gains and losses. Once again we find that
some improvements in quality, while they enhance the quality of life, can
also have the opposite effect. In order to add up these various effects into
a single sum, a method of measurement is needed that can be compared
to the single measure of monetary cost whether that cost is expressed
in dollars or some other unit.
The single measure of effects used in Table 1.2 is the "qualityadjusted year of life." This measure is derived by attributing different
weights to different states of health so that a total can be computed. The
weights in the table are subjective estimates. This, in addition to the
roughness in the categorization of health states and the relative arbitrariness of the discount rate, introduces yet another element of uncertainty
to the analysis. To this uncertainty must be added the error that generally
pervades all estimates of loss and gain because information about them,
as they occur over a lifetime, is usually incomplete. But these defects,
important as they are factually, need not concern us too much, because
what we are after now is to demonstrate a way of thinking about costs
and effects rather than an effort in actual measurement.
Assuming that these estimates of the costs and effects of vaccination
are reasonable, we can compare them as shown in the lower panel of
Table 1.2. This is a comparison of the costs and effects of vaccination at
16
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
different ages. In the young, health gains are relatively small and costs
high. In the aged, costs are lower and gains higher. Such a comparison
can help in deciding to which age groups it would be socially appropriate
to offer vaccination based on how much society is willing to pay for a
given gain in a year of quality-adjusted life. The comparison does not,
however, fix the optimal point below which gains exceed losses and above
which losses exceed gains. To do that, it would be necessary to set a
monetary value for each year of life gained at each age. So that benefits
(or "gains") expressed in dollars can be compared to losses, also expressed
in dollars. I am not prepared to describe the methods by which economists have proceeded to convert years of life into their equivalent in dollars. I must, however, warn the reader that these methods invariably rest
on assumptions that have serious ethical implications.
Now that the reader has a better understanding of the concept of
optimality, it is time to move on to some further implications of the model
shown in Figure 1.3. One consequence of this model is the presence of
two standards of quality: "maximally effective care" and "optimally effective care." Which of these two standards is the one to be used in defining
and "assuring" the quality of care? As I shall show a little further on, when
I discuss the attribute of "social legitimacy," the answer depends on
whether individual or social interests are to be safeguarded.
Still other implications of the model presented graphically in Figure
1.3 have a bearing on important aspects of the relationship between cost
and quality. First, as I have already shown, if optimality is chosen as the
standard of quality, any expenditures beyond those required to achieve
the optimum can be regarded as wasteful. In other words, beyond the
optimum, quality can be considered to be lower rather than higher.
Second, if maximally effective care is taken as the standard of quality,
expenditures below that point are justified. Only expenditures beyond that
point are considered wasteful. And if they result in harm, care is not only
wasteful but also of lower quality.
It will be recalled that in order to generate the curves in Figure 1.3
it was assumed that the care given was that by an "ideal physician" who
consistently avoided all useless care. In actual practice, in any community,
most physicians depart from the ideal, sometimes to a remarkable degree.
The Components of Quality in Health Care
17
Consequently, the improvement in health is not as rapid or as large, and
where resources are plentiful (in a relatively wealthy country, for example)
practitioners are thought to offer care not only beyond the optimal but
beyond the maximal as well. Useless or even harmful care is piled upon
care beyond the point of any reasonable hope for improvement. In such
situations it is believed that restrictions on the cost of care can produce
a significant improvement in quality. But this is only true if the consequent reductions in care are judicious, so that only useless or harmful
care is omitted while everything useful remains a consequence by no
means certain.
By contrast, where resources are limited and, frequently, improvements in health are below the optimal, more care, and costlier care, rather
than less are needed. But even in such situations, what resources are
available could be more effectively used if clinical and production efficiency were improved.
This brings us to still another question. Are considerations of
cost relevant to the definition of quality? Or, on the contrary, should
quality be defined independently of cost considerations? In other words,
is cost an ingredient in quality itself or is it simply the price at which
quality is bought? On this point opinions differ; and it does not matter
much what position one takes as long as cost and quality are assessed
simultaneously.
I have argued that, in some ways, cost is an ingredient in the definition of quality itself. This is obviously true when practitioners give care
more likely to be harmful than useful. It could be argued that this is also
true if the care given is not harmful but merely useless. Besides questioning that there is such a thing as "merely useless," (since almost everything
we do could be harmful) we could argue that such care shows inattention,
ignorance, or carelessness on the part of the practitioner, and for those
reasons, can be considered to be of poor quality. Moreover, because "useless" care for some leaves less for others who could have benefited from
it, such care is socially irresponsible and therefore reprehensible.
Having completed our discussion of efficiency and optimality we are
ready to move on to the fifth component or attribute of quality, as listed
in Figure 1.1.
18
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
Acceptability
Acceptability is defined as conformity to the wishes, desires, and expectations of patients and responsible members of their families. I shall develop this definition in five parts:
1. Accessibility
2. The patient-practitioner relationship.
3. The amenities of care
4. Patient preferences regarding the effects, risks, and cost of care
5. What patients consider to be fair and equitable
I shall briefly comment on each of these.
Accessibility
By accessibility I mean the ease with which persons can obtain care. This
depends on spatial factors such as distance from the sources of care and
on the availability and cost of transportation; on organizational factors
such as the days and hours when sources of care are open to receive
patients; on economic factors such as income and the possession of health
insurance; on social and cultural factors such as the ethnic or religious
preferences of those who seek care or the biases of those who provide it.6
We could debate whether or not accessibility is properly an aspect,
attribute, or component of quality or, on the contrary, whether it is only
an attribute of care separate from quality. Irrespective of such debate, it
is true that people continue to be vitally concerned about their ability to
get care when they want it and with how easily and conveniently it can
be obtained. And, as we shall see soon, accessibility is also a critical
component in the social acceptability of care.
The Patient-Practitioner Relationship
It is not easy to list all the properties that stand for goodness in the
patient-practitioner relationship. As a beginning, mainly to stimulate the
The Components of Quality in Health Care
19
reader's thinking, I offer the attributes listed in Table 1.3. I shall not go
over these in detail. To put it briefly: personal concern, empathy, respectfulness, avoidance of condescension, willingness to take time, effort to
explain, attention to the patient's preferences, honesty, truthfulness, and
plain good manners are essential ingredients in good care.
To begin with, these attributes are desirable in their own right. They
embody cherished values of the health care professions, and include desirable characteristics of every interaction in a civilized society. Moreover,
when such attributes are present, patients are not only pleased, but also
reassured. They regard their presence as evidence (which they understand) that technical care (which they do not understand so well) will
also be good. For these reasons, when patients have a choice, and when
competition among providers of care is allowed, the attractiveness of the
patient-practitioner relationship becomes a key to success among competing organizations. To emphasize this point, some have taken to using
the terms client or customer, rather than patient, to designate those who
Table 1.3. Some Attributes of a Good Patient-Practitioner Relationship
Congruence between therapist and client expectations.
Adaptation and flexibility: the ability of the therapist to accept his or her approach not
only to the expectations of the client but also to the demands of the clinical situation.
Mutuality: gains for both therapist and client.
Stability: a stable relationship between client and therapist.
Maximum client autonomy, freedom of action, and movement
Maintenance of family and community communication and ties.
Maximum egalitarianism.
Active client participation through shared knowledge concerning the health situation,
shared decision making and participation in carrying out therapy.
Empathy and rapport without undue emotional involvement of the therapist.
A supportive relationship without undue dependency.
Confining therapist and client influence and action to the boundaries of their legitimate social functions.
Avoidance of client and therapist exploitation economically, socially, or sexually.
Maintenance of client and therapist dignity and individuality.
Privacy.
Confidentiality.
From Donabedian, A., "Models for Organizing the Delivery of Personal Health Services and Criteria for
Evaluating Them." Milbank Memorial Fund Quarterly 50: 103-153, October 1972, Part 2.
20
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
are likely to need care or actually to seek it. In this way, one recognizes
the health care system as a market rather than a social organism motivated
mainly by its internal commitments and values.
Whether those who seek care are called clients, customers, or patients, it is reasonable to expect a link between the goodness of care and
the goodness of the patient-practitioner relationship. This is because this
relationship is the vehicle by which technical care is implemented. A
good relationship motivates the practitioner to do well. It also motivates
the patient to cooperate, so that the effectiveness of care is enhanced. In
fact, in many cases, the proper management of the patient-practitioner
relationship is in itself the most important technique of care.
Finally, the patient-practitioner relationship is perhaps the most sensitive indicator of the persistence of differences adverse to the underprivileged in the organization and delivery of care. Such differences are the
last to disappear when the goal is to put all patients on an equal footing
with regard to the care offered to them.
The Amenities of Care
The amenities of care are the desirable aspects of the circumstances under
which care is given. They include properties such as convenience, privacy, comfort, restfulness, cleanliness, the availability of adequate parking
(in a motorized society), the availability of refreshments, good food, and
so on. These features are adjuncts to the desirable aspects of the patientpractitioner relationship and, like the latter, help make the experience of
receiving health care either pleasant and rewarding or unpleasant and
humiliating.
Because I have put so much emphasis on the patient-practitioner
relationship and the amenities of care, I should also mention some dangers of an over-reliance on these in judging the quality of care. One
should be alert to the possibility that attractive surroundings and a pleasant
"bedside manner" might cover up, or substitute for, deficiencies in technical care because it is expected that patients will readily appreciate and
be gratified by the former but will be less likely to understand and ap-
The Components of Quality in Health Care
21
preciate the latter, especially when the consequences or success or failure
in technical care are delayed and responsibility for them obscured.
It is, moreover, difficult to set up preconceived specifications of the
patient-practitioner relationship as attributes of its goodness. This is because patients differ so widely in their expectations and preferences. Some
would prefer a cool, distant, authoritarian practitioner, whereas others
would wish to have one who is warm, empathetic and friendly. Some
patients prefer to be told; others wish to be consulted. This means that
the criterion of quality in the patient-practitioner relationship could be
its congruence with the patient's expectations and preferences, rather than
with a list of preconceived attributes. But one cannot completely relinquish the latter. The expectations and preferences of patients are heavily
conditioned by personal experiences in privileged or underprivileged circumstances. Therefore, norms of what the patient-practitioner relationship, and of the amenities of care as well, should be, continue to be
necessary.
There is still another difficulty in being guided only by what patients
like or desire. In some cases, patients wish to have treatments or procedures that are not good for them, or are unnecessary, or are socially undesirable. The conscientious practitioner cannot relinquish the standards
of what is right and moral.
The cost of care, and the priorities imposed by it, is still another
consideration. Some amenities can be costly to institute and maintain.
The patient-practitioner relationship, if it is to be satisfactory, cannot be
hurried; it requires time and is therefore costly. The benefits derived from
incurring these added costs will have to be compared with those of the
alternative uses resources could be put to.
Patient Preferences Regarding the Effects, Risks, and Cost of Care
Patients agree with their practitioners in recognizing the effects on health
as the primary attribute of quality in health care. And, as their practitioners also do, patients compare the expected improvements in health to the
risks associated with care. But, it is also important to recognize that patients may value each of these consequences of care (effects, risks, and
22
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
cost) in a way that differs from the valuations of their practitioners. Moreover, patients differ greatly from one another in their valuations.
When these differences arise out of ignorance of the consequences
of the care contemplated or received, education is the remedy. When
they arise out of economic considerations, the social financing of care
can help reduce the differences. But even then, differences among patients persist. For example, some are anxious to avoid an immediate risk
(let us say, from a surgical operation) whereas others are willing to accept
that risk if the prospect of subsequent longevity is improved.7 Similarly,
some patients would prefer a shorter life of higher quality, whereas others
would prefer longer survival even if the quality of life is relatively low.8
The consequence of the preceding considerations is that practitioners
should take time to explain to patients (or their relatives when patients
are unable to fully understand the situation) the expected cost, risk, and
effects of alternative methods of care, and be guided by the informed
opinion of these parties.9
What Patients Consider to Be Fair or Equitable
Patients have decided opinions about how fairly or equitably they are
treated when it comes to such things as access to care, the patientpractitioner relationship, the amenities, and the expected benefits from
care. Because the concepts of fairness or equity, even when individually
assessed, are matters of social concern, I shall deal with the subject when
I consider the social aspects of quality.
Legitimacy
Legitimacy is defined as conformity to social preferences, as expressed in
ethical principles, values, norms, laws, and regulations. Briefly, it can be
regarded as social acceptability, the property that corresponds to "acceptability to individuals." In a democratic society, where patients and potential patients can express their wishes through a representative political
process, individual and social concerns can be expected to correspond,
The Components of Quality in Health Care
23
and, in general, this is the case. Nevertheless the specification of quality
can differ depending on whether it is viewed by individuals making decisions for themselves or by society when it seeks to advance the welfare
of an entire community. Consequently, society can arrive at different conclusions in determining which kinds of care are most effective, efficient,
optimal, or equitable. How does that happen?
The disparity between individuals and collectivities in their views of
efficiency and optimality arise because society has different estimates of
costs and effects. As regards costs, individuals are concerned with what
they themselves pay, whereas society takes into account as well the costs
it assumes in the shape of government programs, health insurance, and
the like.
As regards effects, individuals are concerned with what pertains to
themselves. They are less mindful of harm or benefit to others (beyond
their own families) when they themselves either receive care or do not
receive it. Society takes the broader view. For example, it may be important to society that individuals be immunized in sufficient numbers to
prevent the spread of disease even when some individuals do not wish it.
In other words, society takes into account the "externalities" (as economists call them) of the actions of individuals. Moreover, society may differ
from individuals in its assessment of effects by placing greater or lesser
valuations on the health and longevity of certain individuals than of others. One example is greater attention to the health and welfare of children
as compared to that of old people because children have an entire lifetime
ahead of them; or more attention to wage earners because they contribute
more to the economy.
The consequence of such disparities as I have described is conflict
between the interests of individuals and the public, at least in the short
term. This conflict can be resolved only by political and social consensus
in a free society. But even if this occurs, a heavy burden may be placed
on health care practitioners if they are expected, individually, to carry out
social policy as they care for individual patients, allowing more care for
some while denying some useful care to others. Such rationing decisions
should be made by regulations that transcend the particular patientpractitioner transaction.
24
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
Equity
Equity is defined as conformity to a principle that determines what is just
and fair in the distribution of health care and of its benefits among the
members of a population. Although equity is an important determinant
of individual and social acceptability, I have thought it worthy of separate
mention as a component of quality.
Obviously, equity depends first, on access to care, and second, on
the effectiveness and acceptability of the care received. As a general rule,
the aim is to erase all differences in these regards between population
groups characterized by age, sex, income, social class, ethnic origin, place
of residence, and so on. But, once again, we must recognize that individual and social preferences can intrude to disrupt the balance of what
could be considered equitable. As I have already said, individuals have
decided views of what equitably should be theirs. But society may determine, in the pursuit of equity, that persons already privileged should have
less care than they want, so that others, heretofore deprived, should receive more.
Attention to what is effective, efficient, or optimal can also intrude
on determinations of social equity. For example, it may be concluded that
certain categories of persons should have more care because the results
in health improvement are significantly greater when compared to cost.
The relative emphasis on prevention as compared to treatment is another
example of this kind of reasoning.
One can ask, therefore, whether or not everyone should receive
equal care relative to "need," whether need is determined by what individuals want or what health professionals estimate. One can also ask
whether, rather than distributing care according to "need," it should be
distributed according to the expected benefits from care. These issues are
to be settled by social consensus in a free society.
Choosing a Definition of Quality
I have already said that agreement on a definition of quality is one of the
foundations of an effort to assure quality. But, having seen how many
The Components of Quality in Health Care
25
different attributes go into the definition of goodness, one must wonder
about the relative priority to be assigned to each of the several attributes
what to include or exclude, where to begin.
In my opinion, there is no general answer to these questions. Much
depends on the context for assessment; on what is most relevant, on what
one is responsible for, on what one can control. Merely as an illustration
of this viewpoint, I offer Figure 1.4, which is meant to suggest what components of quality are most pertinent at successively more inclusive levels
of attention, responsibility, and control. I use as a visual device a set of
concentric semicircles, at the core of which is the patient-practitioner
Figure 1.4. Quality assessment at successively more inclusive levels.
26
AN INTRODUCTION TO QUALITY ASSURANCE IN HEALTH CARE
interaction. Beyond the core, in order, is first, the care implemented by
the patient, and then, the care received by the community. This order is
not invariant. I adopt it because it is congenial to a health care practitioner.
With regard to the care provided by physicians and other practitioners, attention focuses on the effectiveness and efficiency of technical care,
and on the patient-practitioner relationship. Technical care depends on
the knowledge, judgment, and skill of those who offer it.
The amenities of care are at one remove from the health-care transaction itself. They depend on factors generally beyond the direct control
of the practitioners, unless these also own the firm that provides care or,
in some other way, can influence it.
When one is concerned with the domain that surrounds the core
transaction, something is added. That is, attention to the care implemented by patients and their families when these are removed from the
direct influence or control of their practitioners. Clearly, the practitioners
may perform faultlessly but care can be ineffective if patients do not do
their share.
When attention focuses on the care received by a community as a
whole, a new set of concerns is added to those already mentioned. These
include access to care, with due regard to effectiveness and equity. And,
as I have already described, new specifications of optimality are likely to
emerge.
The figure I have offered is, of course, nothing more than a sketchy
illustration. It is far from an exhaustive description of how the attributes
of quality that are most salient vary from situation to situation. The lesson
to be learned is that one must focus on what one is responsible for, what
one can improve, and what is most in need of improvement.
Steps in Monitoring and Improving Clinical Performance
Again, my intent in this little book is to describe briefly how one may
assure the quality of health care by monitoring clinical performance and
The Components of Quality in Health Care
27
improving it when necessary. The steps one might take in carrying out
this intention can be listed as follows:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Determining what to monitor
Determining priorities in monitoring
Selecting an approach (or approaches) to assessing performance
Formulating criteria and standards
Obtaining the necessary information
Choosing when to monitor
Choosing how to monitor
Constructing a monitoring system
Bringing about behavior change
I shall now deal with each of these in turn.
You might also like
- Quality Manual Mental HospitalDocument54 pagesQuality Manual Mental Hospitalsurigao doctors'No ratings yet
- Philippine Politics and Governance: Lesson 6: Executive DepartmentDocument24 pagesPhilippine Politics and Governance: Lesson 6: Executive DepartmentAndrea IbañezNo ratings yet
- The COAT & Review Approach: How to recognise and manage unwell patientsFrom EverandThe COAT & Review Approach: How to recognise and manage unwell patientsRating: 5 out of 5 stars5/5 (1)
- Medication Error PaperDocument6 pagesMedication Error Paperapi-272761526No ratings yet
- 2.quality Assurance in NursingDocument7 pages2.quality Assurance in NursingNancy SamuelNo ratings yet
- Chapter 7: Ambulatory Health CareDocument8 pagesChapter 7: Ambulatory Health CareTrixie AlvarezNo ratings yet
- GDPR Whitepaper FormsDocument13 pagesGDPR Whitepaper FormsRui Cruz100% (6)
- Patient SafetyDocument22 pagesPatient SafetyRensy Sabi100% (1)
- Nursing AdministrationDocument64 pagesNursing Administrationjosephsantuyo0% (1)
- PfeDocument2 pagesPfeCaryl Lou Casamayor100% (3)
- 13 Patient Saefty and Quality ImprovementDocument36 pages13 Patient Saefty and Quality ImprovementShafiq Ur RahmanNo ratings yet
- Sample RN Staff School Nurse Evaluation Form Final 10 6 2011Document4 pagesSample RN Staff School Nurse Evaluation Form Final 10 6 2011Archie PunzalanNo ratings yet
- You Are The Light of The WorldDocument2 pagesYou Are The Light of The WorldKathleen Lantry100% (1)
- International Patient Safety Goals PDFDocument36 pagesInternational Patient Safety Goals PDFHarsya Parma PhastikaNo ratings yet
- Patient Safety PlanDocument4 pagesPatient Safety PlanDhananjay SainiNo ratings yet
- LeadershipDocument17 pagesLeadershipHadi Mohammed HamedNo ratings yet
- Health Care Quality ConceptsDocument11 pagesHealth Care Quality Conceptsmike700usNo ratings yet
- CHAPTER 1 - 3 Q Flashcards - QuizletDocument17 pagesCHAPTER 1 - 3 Q Flashcards - Quizletrochacold100% (1)
- CBAHI and JCI Common Asked Questions. 2023Document5 pagesCBAHI and JCI Common Asked Questions. 2023Rini NoviantiNo ratings yet
- 12-Patient and Family EducationDocument5 pages12-Patient and Family Educationakositabon100% (2)
- Ethics and NursingDocument4 pagesEthics and NursingMarcus, RN100% (8)
- 11 Core Competencies Part 1 To Part 2Document4 pages11 Core Competencies Part 1 To Part 2marie100% (2)
- Home Care CompetencyDocument54 pagesHome Care Competencyapi-3002188600% (1)
- Quality in Healthcare and AccreditationDocument25 pagesQuality in Healthcare and AccreditationSooraj ThomasNo ratings yet
- Principles of DelegationDocument16 pagesPrinciples of DelegationStephanie Talbot100% (1)
- Legal and Ethical Issues in NursingDocument6 pagesLegal and Ethical Issues in NursingCharm TanyaNo ratings yet
- Resume: Mobile KSA: 00966536979152 Mobile Jordan: 00962795661774 EmailDocument8 pagesResume: Mobile KSA: 00966536979152 Mobile Jordan: 00962795661774 EmailAhmad Khalil Ahmad Al-SadiNo ratings yet
- Shipping - Documents - Lpg01Document30 pagesShipping - Documents - Lpg01Romandon RomandonNo ratings yet
- Leadership Practice QDocument19 pagesLeadership Practice QRandyNo ratings yet
- JciDocument5 pagesJcialfredsamuelNo ratings yet
- Introduction to Clinical Effectiveness and Audit in HealthcareFrom EverandIntroduction to Clinical Effectiveness and Audit in HealthcareNo ratings yet
- Joint Commission International: Nepomuceno, Rose Ann TDocument42 pagesJoint Commission International: Nepomuceno, Rose Ann TRoan Nepomuceno - Joaquin100% (1)
- TPH TherapheuticsDocument10 pagesTPH TherapheuticsAl Sah Him100% (2)
- Patient SafetyDocument27 pagesPatient Safetyarahman168No ratings yet
- History of The Nursing ProcessDocument13 pagesHistory of The Nursing ProcessDxc Corrales75% (4)
- Code Blue Training and WorkshopDocument15 pagesCode Blue Training and WorkshopeychceeNo ratings yet
- Chapter 1defining Patient Safety and Quality CareDocument6 pagesChapter 1defining Patient Safety and Quality CareErinNo ratings yet
- Health Care DeliveryDocument27 pagesHealth Care DeliveryAriane joy Cantilero100% (2)
- CBAHI PresentationDocument12 pagesCBAHI PresentationPrince Jhessie L. AbellaNo ratings yet
- Chapter 23 Managing Quality and RiskDocument7 pagesChapter 23 Managing Quality and RiskLorene Reynolds100% (1)
- Nursing Leadership and Management Practice TestDocument1 pageNursing Leadership and Management Practice TestMikhaela GonzalesNo ratings yet
- Patient SafetyDocument11 pagesPatient SafetyMardiyanti FirmanNo ratings yet
- Quality Assurance ProgramDocument16 pagesQuality Assurance ProgramMyca Omega Lacsamana100% (1)
- Infection Control Program in The HospitalDocument14 pagesInfection Control Program in The HospitalLorelie Asis100% (1)
- Post Test NP1Document42 pagesPost Test NP1Bobet ReñaNo ratings yet
- Task 1 Nursing Quality IndicatorsDocument9 pagesTask 1 Nursing Quality IndicatorsHogan ObiNo ratings yet
- Laws in NursingDocument16 pagesLaws in NursingAnusha Verghese100% (1)
- MAN-EMPOWERMENT - Strategies For Enhancing Autonomy and Control Over Nursing Practice PDFDocument10 pagesMAN-EMPOWERMENT - Strategies For Enhancing Autonomy and Control Over Nursing Practice PDFfriolan_cacliniNo ratings yet
- IPC Policy 4 PDFDocument128 pagesIPC Policy 4 PDFgary ann jimenez100% (1)
- Accreditation PrinciplesDocument44 pagesAccreditation Principleshanan abbasNo ratings yet
- Relevance of Nursing Documentation and Its Legal ImplicationsDocument8 pagesRelevance of Nursing Documentation and Its Legal ImplicationsGeorge AyiteyNo ratings yet
- Dimensions of Quality in HealthcareDocument21 pagesDimensions of Quality in HealthcareKaranNo ratings yet
- Clinical AuditDocument5 pagesClinical AuditdrskumarNo ratings yet
- The - Logistics - Handbook (1) - Assessing Stock StatusDocument11 pagesThe - Logistics - Handbook (1) - Assessing Stock StatusDanielNo ratings yet
- Republic Act DOHDocument45 pagesRepublic Act DOHMARIA AURORA COMMUNITY HOSPITALNo ratings yet
- Question Bank QP 1774 Management of Nursing Services and EducationDocument14 pagesQuestion Bank QP 1774 Management of Nursing Services and Educationmelby2604No ratings yet
- Chapter 3: Delivering Nursing CareDocument3 pagesChapter 3: Delivering Nursing CareLynette Olavides Calago100% (1)
- SW 151 Study GuideDocument20 pagesSW 151 Study GuidegcodouganNo ratings yet
- Faculty of Nursing Zagazig University Nursing Administration 4 Year ExamDocument16 pagesFaculty of Nursing Zagazig University Nursing Administration 4 Year ExamserviceNo ratings yet
- The Value of Healthcare AdministrationDocument3 pagesThe Value of Healthcare AdministrationKrizzella ShainaNo ratings yet
- Sullivan ch03 LectureDocument36 pagesSullivan ch03 LectureNyein Nu Winn100% (1)
- All Final Exam QuestionsDocument16 pagesAll Final Exam QuestionsasieNo ratings yet
- Lesson 5 - Electronic Health Record and Clinical Informatics - PPT StudentDocument42 pagesLesson 5 - Electronic Health Record and Clinical Informatics - PPT Studentbeer_ettaaNo ratings yet
- Evidence Based PracticeDocument6 pagesEvidence Based PracticeDianaManifoldBryant100% (1)
- Patient Record MaintenanceDocument2 pagesPatient Record MaintenanceSai SridharNo ratings yet
- RwservletDocument2 pagesRwservletsallyNo ratings yet
- Testamentary Succession CasesDocument69 pagesTestamentary Succession CasesGjenerrick Carlo MateoNo ratings yet
- Pulse of The Profession 2013Document14 pagesPulse of The Profession 2013Andy UgohNo ratings yet
- Is 2750 Specifiction For Steel Scaffoldings R0.183134252Document29 pagesIs 2750 Specifiction For Steel Scaffoldings R0.183134252Suhas Karar0% (1)
- Power of Attorney UpdatedDocument1 pagePower of Attorney UpdatedHitalo MariottoNo ratings yet
- NF79178240335624 ETicketDocument2 pagesNF79178240335624 ETicketridam aroraNo ratings yet
- Test Bank For We The People 10th Essentials Edition Benjamin Ginsberg Theodore J Lowi Margaret Weir Caroline J Tolbert Robert J SpitzerDocument15 pagesTest Bank For We The People 10th Essentials Edition Benjamin Ginsberg Theodore J Lowi Margaret Weir Caroline J Tolbert Robert J Spitzeramberleemakegnwjbd100% (14)
- C1 Level ExamDocument2 pagesC1 Level ExamEZ English WorkshopNo ratings yet
- TRB - HSK NC IiiDocument7 pagesTRB - HSK NC IiiBlessy AlinaNo ratings yet
- QuickRecharge - Ae Is Launched by Paynet - OneDocument2 pagesQuickRecharge - Ae Is Launched by Paynet - OnePR.comNo ratings yet
- (MX) Public Figures, Private LivesDocument3 pages(MX) Public Figures, Private LivesbestatemanNo ratings yet
- Coorg Chicken CurryDocument1 pageCoorg Chicken CurryAnitha VinukumarNo ratings yet
- 5 15 19 Figaro V Our Revolution ComplaintDocument12 pages5 15 19 Figaro V Our Revolution ComplaintBeth BaumannNo ratings yet
- NPS Completed ProjectDocument53 pagesNPS Completed ProjectAkshitha KulalNo ratings yet
- ADPO Syllabus - 10Document2 pagesADPO Syllabus - 10pranjal.singhNo ratings yet
- 7wonders ZeusDocument18 pages7wonders ZeusIliana ParraNo ratings yet
- API1 2019 Broken Object Level AuthorizationDocument7 pagesAPI1 2019 Broken Object Level AuthorizationShamsher KhanNo ratings yet
- International PositioningDocument37 pagesInternational PositioningMansi A Kathuria100% (1)
- MC Script For StorytellingDocument1 pageMC Script For StorytellingPPD LUBOK ANTU-CM15 KPMNo ratings yet
- Singles Inferno SpreekexamensDocument10 pagesSingles Inferno SpreekexamensIlhamNo ratings yet
- Business Enterprise Simulation Quarter 3 - Module 2 - Lesson 1: Analyzing The MarketDocument13 pagesBusiness Enterprise Simulation Quarter 3 - Module 2 - Lesson 1: Analyzing The MarketJtm GarciaNo ratings yet
- Open Quruan 2023 ListDocument6 pagesOpen Quruan 2023 ListMohamed LaamirNo ratings yet
- Philippine National Development Goals Vis-A-Vis The Theories and Concepts of Public Administration and Their Applications.Document2 pagesPhilippine National Development Goals Vis-A-Vis The Theories and Concepts of Public Administration and Their Applications.Christian LeijNo ratings yet
- Jurnal AJISDocument16 pagesJurnal AJISElsa AugusttenNo ratings yet
- Fatawa Aleemia Part 1Document222 pagesFatawa Aleemia Part 1Tariq Mehmood TariqNo ratings yet