Professional Documents
Culture Documents
Transesophageal Imaging of A Left Common Pulmonary.8
Uploaded by
SindhuNugrohoMuktiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transesophageal Imaging of A Left Common Pulmonary.8
Uploaded by
SindhuNugrohoMuktiCopyright:
Available Formats
ECHO ROUNDS
Transesophageal Imaging of a Left Common
Pulmonary Vein During a Minimaze Procedure
Robert J. Suriani, MD,* Albert C. DiMeo, MD, and Raphael P. Squitieri, MD
57-year-old woman with paroxysmal atrial fibrillation, hypertension, noninsulin-dependent diabetes, obesity, and asthma presented for bilateral
thorocoscopic pulmonary vein (PV) isolation and left atrial
(LA) appendage (LAA) exclusion (Minimaze procedure).
Consent for publication of this case has been obtained from
the patient.
Her preoperative computed tomography thoracic angiogram revealed the absence of filling defects within the LA,
the absence of thrombus in the LAA, and a conjoined upper
and lower PV to form a single common PV on the left,
which entered the LA posteriorly (Fig. 1A). The upper and
lower PVs on the right appeared unremarkable in anatomic
size and orientation.
An initial intraoperative transesophageal echocardiography (TEE) was performed under general endotracheal
anesthesia on 2-lung ventilation. The left common PV was
observed just lateral to the LAA in the midesophageal
4-chamber view with retroflexion and leftward rotation of
the TEE probe, and the multiplane array increased to 47
(Fig. 1B) (Video 1, see Supplemental Digital Content 1,
http://links.lww.com/AA/A385). It entered the posterior
aspect of the LA, had a diameter of 1.4 cm at a point
approximately 2 cm from its origin, and expanded to an
ostial diameter of 2.3 cm using the system calipers. The
bifurcation was not observed along the 4 cm of its length
that could be visualized. Color-flow and pulsed-wave
Doppler imaging demonstrated normal antegrade bloodflow patterns into the LA. The right upper and lower PVs
appeared echocardiographically normal, with ostial diameters measuring 1.5 cm and 1.4 cm, respectively.
During the second phase of a bilateral Minimaze
procedure with right-sided 1-lung ventilation, left-sided
hemithorax insufflation, and anterior surgical retraction
of the pericardium, the surgeon positioned the bipolar
radiofrequency clamp around the common PV and onto
its atrial cuff. He expressed concern that due to the
abnormal proximity of the common PV ostia to the right
PVs, an ablation burn encroaching upon or encompassing the right PVs could result in stenosis. TEE examination was thus requested with the clamp applied and
From the Departments of *Anesthesiology and Cardiothoracic Surgery, St.
Vincents Medical Center, Bridgeport, CT.
Accepted for publication November 4, 2011.
Funding: None.
The authors declare no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations
appear in the printed text and are provided in the HTML and PDF versions
of this article on the journals Website (www.anesthesia-analgesia.org).
Reprints will not be available from the authors.
Address correspondence to Robert J. Suriani, MD, Department of Anesthesiology, St. Vincents Medical Center, 2800 Main Street, Bridgeport, CT
06606. Address e-mail to rsuriani@stvincents.org.
Copyright 2012 International Anesthesia Research Society
DOI: 10.1213/ANE.0b013e318251dac0
July 2012 Volume 115 Number 1
Video 1. A midesophageal 4-chamber view with the multiplane array
increased to 47 degrees and color-flow Doppler displays the left
common pulmonary vein (PV) entering the posterior aspect of the left
atrium via an enlarged ostium. Pulsed-wave Doppler imaging reveals
normal blood flow pattern for a patient in sinus rhythm with elevated
left atrial pressure, notably a decreased PVsystolic (S-wave) in relation
to the PVdiastolic (D-wave).
Video 2. A modified midesophageal view with color-flow Doppler
demonstrating unobstructed, nonturbulent, antegrade flow in the
right upper and lower pulmonary veins when the ablation clamp was
applied to the left common pulmonary vein.
before this ablation. Two-dimensional assessment demonstrated that the clamp did not impinge upon either the
right upper or lower PVs. Color-flow and pulsed-wave
Doppler imaging demonstrated unobstructed and nonturbulent bloodflow (Fig. 2) (Video 2, see Supplemental
Digital Content 2, http://links.lww.com/AA/A387). The
ablation was then uneventfully completed. TEE re-evaluation
at the end of the procedure demonstrated unobstructed and
unchanged pulmonary venous bloodflow in the right upper
and lower PVs as well as the left common PV. The patient had
an unremarkable postoperative course.
Normal pulmonary venous anatomy occurs in only
70% 80% of individuals, consisting of 4 PVs with individual ostia emptying into the LA.1 Mean PV diameter at
the ostia has been reported as left superior 16.6 mm, left
www.anesthesia-analgesia.org
27
ECHO ROUNDS
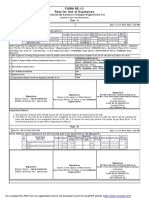
Figure 1. A, Coronal view of the computed tomography thoracic
angiogram demonstrating the left common pulmonary vein (PV)
entering the posterior aspect of the left atrium (LA). B, Midesophageal 4-chamber view with color-flow Doppler demonstrating the left
common PV entering the posterior aspect of the LA through an
enlarged ostium (dotted line). Note that the angiogram is oriented
90 to the transesophageal echocardiography view.
Figure 2. A modified midesophageal view with color-flow Doppler
reveals unobstructed antegrade flow in the right upper and lower
pulmonary veins (PVs) when the ablation clamp was applied to the
left common pulmonary vein. LA left atrium.
inferior 14.8 mm, right superior 17.6 mm, and right inferior
17.1 mm.2 The remaining 20%30% will demonstrate variations in pulmonary venous anatomy consisting of common
28
www.anesthesia-analgesia.org
PV, accessory PV, and anomalous pulmonary venous
drainage.1
A common PV results from ipsilateral superior and
inferior PVs uniting proximal to the LA to form a single
vessel. This occurs more frequently on the left side and
typically results in a single, broad, atriopulmonary junction. Accessory PVs are supernumerary veins with independent LA ostia distinct from the superior and inferior
PVs and more frequently involve the right-sided pulmonary drainage. These veins are named for the segment or
lobe from which they originate, with drainage from the
right lower lobe superior segment or the right middle lobe
the more common variant.3 They can traverse pulmonary
lobar fissures before emptying into the LA and, in contrast
to the superior or inferior PVs, typically have narrow ostia.
They almost always have no clinical impact.
Anomalous pulmonary venous drainage is characterized by the abnormal return of one or more PVs into a
structure other than the LA. In total anomalous pulmonary
venous return, none of the PVs connect to the LA, but
instead form a confluence behind the heart, which drains
into the right atrium by way of a vertical vein. It is the route
by which blood returns to the right atrium via this vertical
vein that leads to its classification as supracardiac, cardiac,
subdiaphragmatic, or mixed.4 Partial anomalous pulmonary venous return occurs when 1 or more, but not all, of
the PVs drain into the right atrium. Commonly, the left
upper PV connects to the innominate vein, or the right
upper PV connects directly to the superior vena cava.
Because of its retrocardiac positioning, TEE is ideally
suited to evaluate the PVs. They are best visualized in the
midesophageal 4-chamber view by initially centering on
the LA and then focusing on each one individually. The left
PVs may be simultaneously imaged by turning the probe
counterclockwise with the omniplane array set at 100 to
110, whereby they appear as an inverted V entering the
LA. Similarly, the right PVs may be simultaneously imaged
by turning the probe clockwise with the omniplane array
set at 45 to 60.5 The right upper PV is also visualized in
the bicaval view with slight clockwise rotation of the probe,
appearing on the far right of the screen as the superior vena
cava disappears from view. It is essential to visualize a
separate venous orifice entering the LA for each PV. The
inability to visualize individual PVs should prompt the
echocardiographer to search for any anomalous PV drainage and to consider the existence of a common PV as in this
report.
During the Minimaze procedure, a bipolar radiofrequency clamp is placed around the atrial cuff of both
ipsilateral PVs. This creates a transmural ablation lesion or
burn to electrically isolate them from the LA. The clamp
is intentionally applied to the atrial cuff to avoid the burn
occurring on the delicate tissue of the PV and potentially
causing PV stenosis. PV stenosis resulting from this burn,
fortunately, has not been reported, but is a recognized
complication of intracardiac radiofrequency catheter ablation of arrhythmias originating from the PVs. Significant
stenosis has been defined as a peak velocity more than or
equal to 110 cm/s, along with turbulence and reduced flow
variations indicative of stenotic flow, and a 50% reduction in lumen diameter.6 The echocardiographer should not
ANESTHESIA & ANALGESIA
TEE Imaging of a Common Pulmonary Vein
assume that high-velocity PV flow is solely due to PV
stenosis, because marked left-to-right shunting, as through
an atrial septal defect, may be an alternative explanation.5
Ideally, a comprehensive baseline examination is performed for later comparison.
Although PV morphology had been determined preoperatively on computed tomography thoracic angiogram,
real-time assessment of the anatomic relationship of the left
common PV to the right PVs was required during surgical
instrumentation. This case highlights the importance of
TEE during the Minimaze procedure in patients with
congenitally abnormal pulmonary venous anatomy. TEE
imaging allowed for assessment of common PV morphology proximate to the LA, evaluation of pulmonary venous
bloodflow during surgical instrumentation, and then reevaluation after surgical intervention.
DISCLOSURES
Name: Robert J. Suriani, MD.
Contribution: This author helped design the study, conduct
the study, analyze the data, and write the manuscript.
Attestation: Robert J. Suriani approved the final manuscript.
Name: Albert C. DiMeo, MD.
Contribution: This author helped conduct the study and write
the manuscript.
Attestation: Albert C. DiMeo approved the final manuscript.
Clinicians Key Teaching Points
Name: Raphael P. Squitieri, MD.
Contribution: This author helped analyze the data and write
the manuscript.
Attestation: Raphael P. Squitieri approved the final manuscript.
This manuscript was handled by: Martin J. London, MD.
REFERENCES
1. Stanford W, Breen JF. CT evaluation of left atrial pulmonary
venous anatomy. Int J Cardiovasc Imaging 2005;21:1339
2. Cronin P, Kelly AM, Desjardins B, Patel S, Gross B, Kazerooni E,
Morady F, Oral H, Carlos R. Normative analysis of pulmonary
vein drainage patterns on multicenter CT with measurements of
pulmonary vein ostial diameter and distance to first bifurcation.
Acad Radiol 2007;14:178 88
3. Lacomis JM, Wigginton W, Fuhrman C, Schwartzman D, Armfield DR. Multi-detector row CT of the LA and PVs before
radio-frequency catheter ablation for atrial fibrillation. Radiographics 2003;23:S35 48
4. Herlong JR, Jaggers JJ, Ungerleider RM. Congenital Heart
Surgery Nomenclature and Database Project: pulmonary venous anomalies. Ann Thorac Surg 2000;69:S56 69
5. Myles PS, Marasco S. Misleading turbulent flow through pulmonary venous anastomoses during lung transplantation.
Anesth Analg 2008;107:1504 5
6. Jander N, Minners J, Arentz T, Gornandt L, Furmaier R,
Kalusche D, Neumann FJ. Transesophageal echocardiography
in comparison with magnetic resonance imaging in the diagnosis of pulmonary vein stenosis after radiofrequency ablation
therapy. J Am Soc Echocardiogr 2005;18:654 9
By Martin M. Stechert, MD, Roman M. Sniecinski, MD,
and Martin J. London, MD
Variations of pulmonary venous anatomy include total or partial connection to the systemic venous system (i.e.,
entering into the right atrium or contributory large veins), additional connections with accessory pulmonary veins, and
fused connections (i.e., a common pulmonary vein). The latter refers to distal fusion of 2 ipsilateral pulmonary veins,
resulting in a common pulmonary trunk and single inlet (orifice) into the left atrium.
The left upper (seen superior to the left atrial appendage in the midesophageal 2-chamber view) and right upper
(developed from the bicaval view by turning the probe to the right) pulmonary veins are the easiest to image and are
ideally aligned for Doppler interrogation. High velocities or turbulent flow on color flow Doppler can be seen with
pulmonary vein stenosis. The lower pulmonary veins lie further away from the transducer, but can often be imaged by
first finding the ipsilateral upper pulmonary vein and slightly advancing the probe.
In this case of thorascopic bilateral pulmonary vein isolation and left atrial appendage exclusion, transesophageal
echocardiography was used to monitor pulmonary vein flow which could be compromised by the radiofrequency
ablation. The widened ostium, in the location of what would typically have been the left upper pulmonary vein, was
consistent with a common pulmonary vein.
Because deviation from the typical 4 pulmonary vein anatomy is present in up to 30% of the population,
echocardiographers should be aware of the common normal variants. Fortunately, most of these have not been
reported to be clinically significant.
July 2012 Volume 115 Number 1
www.anesthesia-analgesia.org
29
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Entity Level ControlsDocument45 pagesEntity Level ControlsNiraj AlltimeNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Mazda Fn4A-El 4 Speed Ford 4F27E 4 Speed Fnr5 5 SpeedDocument5 pagesMazda Fn4A-El 4 Speed Ford 4F27E 4 Speed Fnr5 5 SpeedAnderson LodiNo ratings yet
- Instrumentation Positioner PresentationDocument43 pagesInstrumentation Positioner PresentationSangram Patnaik100% (1)
- Origins and Rise of the Elite Janissary CorpsDocument11 pagesOrigins and Rise of the Elite Janissary CorpsScottie GreenNo ratings yet
- Postgraduate Notes in OrthodonticsDocument257 pagesPostgraduate Notes in OrthodonticsSabrina Nitulescu100% (4)
- Intraoperative Transesophageal Echocardiography.10Document4 pagesIntraoperative Transesophageal Echocardiography.10SindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiography Findings.6Document4 pagesTransesophageal Echocardiography Findings.6SindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiographic Evaluation.13Document12 pagesTransesophageal Echocardiographic Evaluation.13SindhuNugrohoMuktiNo ratings yet
- Three Dimensional Transesophageal Echocardiography.18Document3 pagesThree Dimensional Transesophageal Echocardiography.18SindhuNugrohoMuktiNo ratings yet
- 45 Transesophageal Echocardiography For.45Document1 page45 Transesophageal Echocardiography For.45SindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiography For The Noncardiac Surgical PatientDocument13 pagesTransesophageal Echocardiography For The Noncardiac Surgical PatientSindhuNugrohoMuktiNo ratings yet
- 516Document115 pages516Anonymous OlS0WZwNo ratings yet
- Transesophageal Echocardiography Images of Dynamic.14Document3 pagesTransesophageal Echocardiography Images of Dynamic.14SindhuNugrohoMuktiNo ratings yet
- ECG InterpretationDocument3 pagesECG InterpretationDiana MeceaNo ratings yet
- Seminars TOE in Non CardiacDocument25 pagesSeminars TOE in Non CardiacSindhuNugrohoMuktiNo ratings yet
- Utility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgeryDocument8 pagesUtility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgerySindhuNugrohoMuktiNo ratings yet
- Contemporary Reviews in Cardiovascular Medicine: Cardiogenic ShockDocument32 pagesContemporary Reviews in Cardiovascular Medicine: Cardiogenic ShockSindhuNugrohoMuktiNo ratings yet
- Utility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgeryDocument8 pagesUtility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgerySindhuNugrohoMuktiNo ratings yet
- Seminars TOE in Non CardiacDocument25 pagesSeminars TOE in Non CardiacSindhuNugrohoMuktiNo ratings yet
- Complete Intraoperative Transesophageal.9Document3 pagesComplete Intraoperative Transesophageal.9SindhuNugrohoMuktiNo ratings yet
- 8 Transesophageal Echocardiography For.8Document4 pages8 Transesophageal Echocardiography For.8SindhuNugrohoMuktiNo ratings yet
- Practice Guidelines For Perioperative Transesophageal EchocardiographyDocument24 pagesPractice Guidelines For Perioperative Transesophageal EchocardiographySindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiography Images of Dynamic.14Document3 pagesTransesophageal Echocardiography Images of Dynamic.14SindhuNugrohoMuktiNo ratings yet
- Complete Intraoperative Transesophageal.9Document3 pagesComplete Intraoperative Transesophageal.9SindhuNugrohoMuktiNo ratings yet
- Clinical Manual and Review of Transesophageal.45Document2 pagesClinical Manual and Review of Transesophageal.45SindhuNugrohoMuktiNo ratings yet
- Utility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgeryDocument8 pagesUtility of Perioperative Transesophageal Echocardiography in Non-Cardiac SurgerySindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiography Detection Of.5Document3 pagesTransesophageal Echocardiography Detection Of.5SindhuNugrohoMuktiNo ratings yet
- DafpusDocument2 pagesDafpusSindhuNugrohoMuktiNo ratings yet
- Etiologi CLDDocument4 pagesEtiologi CLDSindhuNugrohoMuktiNo ratings yet
- Meds CapeDocument11 pagesMeds CapeSindhuNugrohoMuktiNo ratings yet
- Sleep and Fatigue in Cancer PatientDocument6 pagesSleep and Fatigue in Cancer PatientSindhuNugrohoMuktiNo ratings yet
- Transesophageal Echocardiography For The Noncardiac Surgical PatientDocument13 pagesTransesophageal Echocardiography For The Noncardiac Surgical PatientSindhuNugrohoMuktiNo ratings yet
- Sleep and Fatigue in Cancer PatientDocument6 pagesSleep and Fatigue in Cancer PatientSindhuNugrohoMuktiNo ratings yet
- FINAL A-ENHANCED MODULES TO IMPROVE LEARNERS - EditedDocument22 pagesFINAL A-ENHANCED MODULES TO IMPROVE LEARNERS - EditedMary Cielo PadilloNo ratings yet
- Mtle - Hema 1Document50 pagesMtle - Hema 1Leogene Earl FranciaNo ratings yet
- Krok2 - Medicine - 2010Document27 pagesKrok2 - Medicine - 2010Badriya YussufNo ratings yet
- Energy AnalysisDocument30 pagesEnergy Analysisca275000No ratings yet
- Pre Job Hazard Analysis (PJHADocument2 pagesPre Job Hazard Analysis (PJHAjumaliNo ratings yet
- C6030 BrochureDocument2 pagesC6030 Brochureibraheem aboyadakNo ratings yet
- PESO Online Explosives-Returns SystemDocument1 pagePESO Online Explosives-Returns Systemgirinandini0% (1)
- How Psychology Has Changed Over TimeDocument2 pagesHow Psychology Has Changed Over TimeMaedot HaddisNo ratings yet
- Iso 9001 CRMDocument6 pagesIso 9001 CRMleovenceNo ratings yet
- GATE ECE 2006 Actual PaperDocument33 pagesGATE ECE 2006 Actual Paperkibrom atsbhaNo ratings yet
- Accomplishment Report 2021-2022Document45 pagesAccomplishment Report 2021-2022Emmanuel Ivan GarganeraNo ratings yet
- Marketing Plan for Monuro Clothing Store Expansion into CroatiaDocument35 pagesMarketing Plan for Monuro Clothing Store Expansion into CroatiaMuamer ĆimićNo ratings yet
- Difference Between Text and Discourse: The Agent FactorDocument4 pagesDifference Between Text and Discourse: The Agent FactorBenjamin Paner100% (1)
- MBO, Management by Objectives, Pooja Godiyal, Assistant ProfessorDocument20 pagesMBO, Management by Objectives, Pooja Godiyal, Assistant ProfessorPooja GodiyalNo ratings yet
- DNA Gel Electrophoresis Lab Solves MysteryDocument8 pagesDNA Gel Electrophoresis Lab Solves MysteryAmit KumarNo ratings yet
- Family Service and Progress Record: Daughter SeptemberDocument29 pagesFamily Service and Progress Record: Daughter SeptemberKathleen Kae Carmona TanNo ratings yet
- Decision Maths 1 AlgorithmsDocument7 pagesDecision Maths 1 AlgorithmsNurul HafiqahNo ratings yet
- Portfolio Artifact Entry Form - Ostp Standard 3Document1 pagePortfolio Artifact Entry Form - Ostp Standard 3api-253007574No ratings yet
- Personalised MedicineDocument25 pagesPersonalised MedicineRevanti MukherjeeNo ratings yet
- Sarvali On DigbalaDocument14 pagesSarvali On DigbalapiyushNo ratings yet
- 3ccc PDFDocument20 pages3ccc PDFKaka KunNo ratings yet
- Surgery Lecture - 01 Asepsis, Antisepsis & OperationDocument60 pagesSurgery Lecture - 01 Asepsis, Antisepsis & OperationChris QueiklinNo ratings yet
- ERP Complete Cycle of ERP From Order To DispatchDocument316 pagesERP Complete Cycle of ERP From Order To DispatchgynxNo ratings yet
- Mission Ac Saad Test - 01 QP FinalDocument12 pagesMission Ac Saad Test - 01 QP FinalarunNo ratings yet
- 2010 - Impact of Open Spaces On Health & WellbeingDocument24 pages2010 - Impact of Open Spaces On Health & WellbeingmonsNo ratings yet