Professional Documents
Culture Documents
Principles in The Management of Traumatic Injuries: Metabolic Response To Trauma
Uploaded by
Neiana CarolinaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Principles in The Management of Traumatic Injuries: Metabolic Response To Trauma
Uploaded by
Neiana CarolinaCopyright:
Available Formats
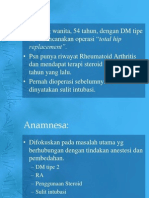
PART
ONE
Principles in the Management of
Traumatic Injuries
CHAPTER
Metabolic Response to Trauma
Thomas A. Stark
Harry L. Anderson, III
OUTLINE
Physiologic Response
Mediators of the Response
Neuroendocrine Response
Lipid-Derived Mediators
Cytokines
Polymorphonuclear Neutrophils
njury produces profound systemic effects. Hormones,
the autonomic nervous system, and cytokines all
produce a series of responses that are teleologically
designed to help defend the body against the insult of
trauma and promote healing. Classically, these responses
have been described as the stress response, a term coined
by the Scottish chemist Cuthbertson in 1932.1 However,
some of these responses may be counterproductive. The
cascade of interactions is orchestrated in the severely
traumatized patient to produce a host of responses that
follow a recognizable pattern, but the depth and duration of these changes are variable, usually proportional
to the extent of the injury and the presence of ongoing
stimulation. Stresses other than major trauma produce
alterations in the metabolic responses; examples are
burns, sepsis, and starvation. Each results in marked
variations in the metabolic response, and this variability
persists during the later chronic and recovery phases of
the original injury (Fig. 1-1).
The bodys initial response to insult (the acute phase)
is directed at maintaining adequate substrate delivery to
the vital organs, in particular oxygen and energy. Cuthbertsons pioneering work recognized the increases in
basal temperature, energy expenditure, and oxygen consumption, and also the loss of potassium and nitrogen.2,3
The term systemic inflammatory response syndrome (SIRS) is
used to describe the bodys response to infectious and
noninfectious causes and consists of two or more of the
followinghyperthermia or hypothermia, leukocytosis
Clinical Implications
Modulation of the Response
Adult Respiratory Distress Syndrome
Nutrition As Therapy
Deep Vein Thrombosis Prophylaxis
Stress Gastritis
or leukopenia, tachycardia, and tachypnea. When the
inflammatory response impairs function of organs or
organ systems, the term multiple organ dysfunction syndrome
(MODS) is used. As greater sophistication in the care of
the multiply injured patient has permitted careful observation and analysis of the metabolic changes that accompany trauma; similar advances in the field of molecular
biology have allowed the identification and measurement of the precise hormones and inflammatory mediators involved in the bodys response to trauma. This
chapter reviews the mechanisms and consequences of
the metabolic response to traumatic injury and some
common approaches to the problems produced by these
metabolic derangements.
PHYSIOLOGIC RESPONSE
Tissue damage produces an inflammatory reaction that
causes local effects, such as tissue edema, vasoconstriction, and thrombosis. Other mediators released into the
systemic circulation act at sites removed from the injury.
For example, they stimulate the autonomic nervous
system, with concomitant production of hormones, cytokines, and arachidonic acid metabolites. The orchestrated response seen with severe injury has been
described as having two phases that overlap, the ebb
phase, which occurs immediately and may last as long as
24 hours after injury, and the flow phase, which may last
for weeks.
Change from baseline
PART I Principles in the Management of Traumatic Injuries
Time
Death
Acute phase
Chronic phase
Recovery
FIGURE 1-1 Phases of metabolism after critical illness and injury.
(Adapted from Mongardon N, Singer M: The evolutionary role of
nutrition and metabolic support in critical illness. Crit Care Clin
26:443450, 2010.)
The first, or ebb, phase is characterized by the release
of catecholamines and vasoactive hormones. Cardiac
output is elevated by increases in heart rate and cardiac
contractility. Peripheral and splanchnic vasoconstriction
occurs and extravascular fluids are mobilized to maintain
blood volume. These hemodynamic consequences act to
preserve blood volume. The respiratory rate is also
increased and this increase, in concert with the hemodynamic changes, drives maximal oxygen delivery.
The blood glucose level is also elevated through a
complex and tissue-specific insulin resistance pathway.4
The maintenance of blood glucose levels supports the
obligate glucose-metabolizing tissuesbrain, bone
marrow, erythrocytes, granulation tissue, and the immune
system. Free fatty acids are mobilized by the catabolic
hormones and become the main source of energy for
peripheral tissue. Stored hepatic glycogen is limited and
may be depleted within 1 day.
As the catabolic or flow phase is established, the metabolic emphasis is on the provision of substrate for healing.
The basal metabolic rate is elevated, and thereafter the
patient catabolizes muscle to make glucose. Birkhahn
and colleagues found an almost 80% rise in catabolism
after skeletal trauma, and Kien and associates have
reported elevations as high as 103% in burn patients.5,6
The total body nitrogen balance becomes negative. Some
of the earlier changes of the ebb phase may be reversed;
for example, a diuresis may occur, or the heart rate may
slow.
It may be difficult to separate the effects of the metabolic response to trauma from the effects of shock or
incomplete resuscitation, but clearly such a distinction is
necessary. The initial phase of the trauma response is
complicated by an ongoing deficiency in tissue perfusion. The clinician must respond to dynamic changes in
physiology to make time-sensitive interventions. The pulmonary artery or Swan-Ganz catheter offers a continuous
window into the minute to minute mechanics of the
severely injured patient. More recently, the safety and
usefulness of Swan-Ganz catheters in trauma resuscitation has been scrutinized and their routine use has
declined.7 Less invasive modalities such as the central
venous catheter, near-infrared spectroscopy (NIRS), and
continuous cardiac output monitoring by arterial waveform analysis are as effective at guiding therapy.8-10
The measured serum lactate level may help guide
therapy and additional resuscitation. During shock states,
tissue perfusion is decreased and increasing numbers of
cells depend on anaerobic metabolism for energy. Normalization of serum lactate levels can indicate a return
to global aerobic metabolic states and serve as an end
point for resuscitation. Partly because of the reversible
nature of hypoperfusion in the trauma setting, initial
serum lactate levels are not themselves independent predictors of morbidity and mortality.11
Similar injuries to different body regions can produce
dramatic differences in metabolic requirement (Fig.
1-2). Two injuries in particular are worth special mention
because of their notable metabolic consequences. The
first is injury caused by head trauma. When brain injury
is superimposed on multisystem trauma, the risk of death
more than doubles.12 Increased mortality may not be
directly caused by neurologic injury per se, but rather by
the systemic consequences of deranged metabolism.13 In
addition, many methods whereby brain-injured patients
are managed after injury have themselves profound
effects on metabolism. Examples of these interventions
include steroids, systemic dehydration, muscle paralysis,
hyperventilation, hypothermia, hyperbaric oxygen
therapy, and barbiturate coma. The effectiveness of these
treatments has been challenged but they continue to
remain in use.14-16
The second injury is the clinical entity of classic fat
embolism syndrome, seen particularly after long bone
fractures. Fatty acid and triglyceride-rich fat globules
enter venous sinusoids at the fracture site. These fat
droplets migrate to the lung, where they are converted
by pulmonary lipase to free fatty acids, which can damage
the pulmonary microvasculature. In addition, platelets
are activated, aggregate, and attach to the fat droplet, a
process that may lead to a consumptive coagulopathy.
MEDIATORS OF THE RESPONSE
NEUROENDOCRINE RESPONSE
An early response of the neuroendocrine system is the
upregulation of the sympathoadrenal axis, which generates high plasma concentrations of epinephrine, norepinephrine, vasopressin, and dopamine. The peak and
duration of the response parallel the severity of the
trauma.17 These substances directly affect blood glucose
levels and also produce inhibition of glucose uptake by
tissue, which stimulates glucagon secretion. Sympathetic
activity promotes lipolysis within adipose tissue, which
begins to provide an energy source for gluconeogenesis.18 Gluconeogenesis in the liver is stimulated by
glucagon.
The hypothalamic-pituitary axis is stimulated at the
same time as the sympathetic nervous system after
trauma.19 The pituitary releases adrenocorticotropic
hormone (corticotropin, or ACTH), which stimulates
the adrenal cortex to secrete glucocorticoid hormones
such as cortisol and aldosterone. Epinephrine and
Metabolic Response to Trauma CHAPTER 1
1300
1200
1100
1000
900
800
700
600
5500
5000
4500
5000
4000
4375
3500
3750
3500
3250
3000
2750
2500
3000
2800
2600
2400
2200
2000
2250
1800
2000
1600
1750
1400
1500
1250
1200
1100
1000
1125
900
1000
800
10
875
700
750
600
Normal 0
625
500
Percent change in metabolic activity
1400
6875
6250
5625
Estimated metabolic rate Kcal/day
2800
2700
2600
2500
2400
2300
2200
2100
2000
1900
1800
1700
1600
1500
Estimated caloric intake (MR + 25%) Kcal/day
Daily basal metabolic rate Kcal/day
Burn size
115
110
105
100
95
90
85
90
75
70
65
60
55
50
45
40
500
400
50%
40%
30%
Multiple trauma with
patient on ventilator
20%
Severe infection,
multiple trauma
35
30
25
20
10%
Long bone fracture
15
Peritonitis
Postoperative
-5
-10
500
70%
60%
Mild starvation
-15
FIGURE 1-2 Changes in resting energy expenditure associated with trauma, burns, and other common clinical conditions. (Adapted From
Wilmore DW: The metabolic management of the critically ill, New York, 1977, Plenum Press.)
cortisol promote muscle breakdown, protein catabolism,
and amino acid release.
The effects of the flow phase of the metabolic response
to trauma are partly attributable to hormones such as
glucagon and cortisol, but not entirely, because the catabolic consequences extend beyond measurable elevated
levels of these hormones.20,21 This finding has implicated
other factors such as cytokines or the suppression of
other hormonal axes such as those of somatostatin and
growth hormone.
LIPID-DERIVED MEDIATORS
Cyclooxygenase products of arachidonic acid metabolism are present in increased amounts in human studies
of injury. Thromboxane A2 accentuates neutrophil
aggregation and, with prostacyclin, has potent and opposing vascular effects that may have a role in pulmonary
hypoxic vasoconstriction and systemic vasodilation.
Lipoxygenase products are also released in large quantities and affect the permeability of the pulmonary vascular bed.
Platelet-activating factor (PAF) is a phospholipid
metabolite released by a number of cells, including neutrophils. The response to PAF at the endothelial surface
results in enhanced superoxide production, enhanced
platelet aggregation, altered pulmonary vascular reactivity, and changes in endothelial permeability.
CYTOKINES
Protein mediators, collectively called cytokines, are produced at the site of injury and by diverse circulating
immune cells. Monocytes, lymphocytes, macrophages,
and other cells release cytokines. They can act locally as
paracrines by way of direct cell to cell communication or
systemically when produced in excess by way of endocrine mechanisms. The most important cytokines in
trauma are tumor necrosis factor (TNF), the interleukins
(IL-1, IL-2, IL-6, and IL-8), the interferons, and various
growth factors such as granulocyte-macrophage colonystimulating factor (GM-CSF), and platelet-derived growth
factors (PDGFs). They enhance immune cell function
and are responsible for the systemic effects of inflammation and sepsis, such as fever, leukocytosis, hypotension,
delayed gastric emptying, and malaise.
Thought to be the most proximal mediator of the
inflammatory response, TNF was originally described as
the catabolic factor cachectin.22 At least two forms of TNF
exist.23,24 TNF influences cellular attraction as part of the
local inflammatory response, leukocyte migration, and
systemic hypotension.25,26 It also promotes muscle
PART I Principles in the Management of Traumatic Injuries
catabolism, free fatty acid release, and hepatic synthesis
of acute-phase reactants. TNF free receptor is a glycosylated protein found in membrane-bound and free-floating
forms. In contrast to IL-1, TNF appears to act peripherally and has no direct effect on lymphocyte activation.27
The interleukins are polypeptides released from lymphocytes; each is numbered according to the amino acid
sequence that elicits its action.28 Circulating free receptors are known for IL-1 and IL-6. Free receptors may exist
for all cytokines. They appear to function in the regulation of cytokine activity. IL-1, which can be detected in
the circulation within a few hours after injury, has multiple biologic effects, including the activation of resting
T lymphocytes and macrophages, induction of hematopoietic growth factors, stimulation of chemotaxis of neutrophils, and synthesis of collagen and collagenases.
More profound systemic effects include fever and changes
in protein metabolism. Originally described as pyrexin,
IL-1 was shown in subsequent studies to act via the production of prostaglandins in the hypothalamus and to
alter the set point of the thermoregulator in the hypothalamus.29,30 It is in this way that antiprostaglandin
agents, such as aspirin, can block the fever effect of
IL-1.31 A byproduct of IL-1 metabolism can increase proteolysis of human muscle and induce hepatic protein
synthesis.32,33 Identified as a B cell differentiation factor,
IL-6 is now recognized as the final common mediator in
a cascade of cytokine activity that alters hepatocyte
protein synthesis.34,35
The interactions of cytokines with one another and
the stress response hormones have been increasingly
studied. Cytokines are potent stimulators of the release
of other mediators (e.g., IL-1 acting on the hypothalamus). Evidence exists for convoluted positive-feedback
relationships organized within the cytokine cascade.
Release of early mediators, for example TNF, triggers
release of the complete aggregate of cytokines, which
then combine to elicit the host response.
The cytokine receptors and cytokine agonists may
have several roles in trauma patients. Both are released
in a sequential manner, paralleling the release of cytokines, and they modulate the bodys response to trauma.36
Figure 1-3 demonstrates the fluctuating levels of cytokine
receptors over time. Quantitative serum cytokine levels,
particularly IL-6, correlate with injury severity and serve
as a predictor of adverse outcomes and mortality.37,38
Although highly sensitive, lack of specificity has limited
their use in clinical settings.
POLYMORPHONUCLEAR NEUTROPHILS
Catecholamines and glucocorticoids marginalize peripheral polymorphonuclear neutrophils (PMNs) and recruit
them from the bone marrow.39,40 Lipids and cytokines
(e.g., IL-1, TNF, PAF) then prime these cells for enhanced
superoxide anion release and sequestration in endorgans.41 Capillary endothelial integrity is disrupted,
leading to the formation of edema, defects in oxygen
delivery, hypoxic cellular injury, and other adverse consequences for cellular homeostasis. This derangement
leads to the clinical entity of multiple-organ failure.
Human studies have supported this sequence and also
suggested that additional stress results in a rerelease of
sTNFr
IL-1RA
sIL-2r
Control
1
hour
2
hour
4
hour
12
hour
1
day
3
day
7
day
Time post-injury
FIGURE 1-3 The sequential release of cytokine receptors and
receptor agonists after injury. IL-1RA, interleukin-1 receptor
antagonist; sIL-2r, soluble interleukin-2 receptor; sTNFr, soluble
TNF receptor. (Adapted from Cinat M, Waxman K, Vaziri ND,
etal: Soluble cytokine receptors and receptor antagonists are
sequentially released after trauma. J Trauma 39:112118,1995.)
mediators of the stress response that multiplies the effect
of the already enhanced PMNs.42,43
CLINICAL IMPLICATIONS
The successful management of the metabolic changes
that accompany severe trauma influences and may
prevent some of the major complications of trauma
namely impaired immune function, multiple organ
failure, and sepsis.44
MODULATION OF THE RESPONSE
Researchers have tested novel therapeutic strategies and
options aimed at selectively inhibiting the undesirable
actions of cytokines while allowing the appropriate
responses to be expressed. Some effects of cytokines on
target tissue have been successfully blocked by the use of
anticytokine antibodies and specific cytokine receptor
antagonists. Animal studies, in particular, have suggested
significant efficacy of these agents, but the results in
humans have been largely disappointing, particularly
when they have been used in septic patients.45 Most of
the work, however, has focused on multicenter trials of
patients who have sepsis from many causes, rather than
solely the multiply injured. Caution must nonetheless be
exercised because of the risk that these agents may neutralize the beneficial, survival-enhancing effects of the
cytokines and other elements of inflammation. Another
problem with these therapies is that cytokines are rapidly
released after injury, and the administration of antibodies, by necessity, occurs laterafter the initiation of the
cytokine cascade.
Pharmacologic manipulation of the end-organ
response to stress is also accomplished with some drug
classes that act on specific mediators of the response. For
example, cyclooxygenase inhibitors such as ibuprofen
Metabolic Response to Trauma CHAPTER 1
Critical illness
Catabolism
Starvation for
medical reasons
Impaired GI motility
Risk of aspiration
Increased energy
requirements
Unsuitable
nutrition protocols
Insufficient coverage of energy target by EN alone
Supplemental
parenteral
nutrition
Negative protein-energy balance
Undernutrition
Increased morbidity
Increased mortality
Longer length of stay
Longer recovery
FIGURE 1-4 Factors whereby enteral nutrition may result in undernutrition of critically ill and injured patientsthe potential role of
supplemental parenteral nutrition. (Adapted from Thibault R, Pichard C: Parenteral nutrition in critical illness: Can it safely improve
outcomes? Crit Care Clin 26:467480, 2010.)
inhibit the production of eicosanoids and may thus blunt
the physiologic response to cytokines, such as fever, associated with TNF, IL-1, and IL-6. In patients with sepsis,
ibuprofen has shown some improvement in clinical
parameters, but has not been proven to decrease the
duration of shock or improve mortality.46
Control of hyperglycemia in critically ill surgical
patients has been shown in a large, prospective, randomized trial to decrease morbidity and mortality. Intensive
insulin therapy (IIT) requires maintenance of blood
glucose levels below 110mg/dL.47 Subsequent analysis
found that increased mortality from hypoglycemic events
negates the benefits of IIT in clinical practice. Trauma
patients, however, were a subset found to having benefited the most from IIT.48 Further investigation is necessary to determine safe and effective mechanisms for
glycemic control in trauma patients.
The role of glucocorticoids in modulating the stress
response remains unclear. In severe cases of injury, sepsis,
and critical illness, the adrenal system is unable to supply
the overwhelming demand for glucocorticoids, and a
relative adrenal insufficiency ensues.49 Pharmacologic
factors such as even a single dose of etomidate have also
proven to increase rates of adrenal insufficiency and
mortality in the critically ill.50 Multiple trials have failed
to identify a definite improvement in mortality, although
low-dose corticosteroid therapy may decrease the duration of shock states and improve short-term survival.51-53
In trauma patients, there is some evidence that
hydrocortisone therapy attenuates the stress response
and decreases the likelihood of hospital-acquired pneumonia.54 Further research is needed to establish practical
therapeutic strategies, particularly in traumatic brain
injury, in which high-dose steroids have been associated
with an increase in mortality.55
Human activated protein C (drotrecogin alfa [activated]) was one of the first approved recombinant agents
targeting the procoagulant and generalized inflammatory response that occurs during sepsis. It had been initially found to reduce death rates in patients with severe
sepsis.56 Ongoing surveillance proved that there was no
survival benefit in patients with severe sepsis when compared with placebo, and the drug has since been withdrawn from the market.57
Pharmacologic manipulation of the response to traumatic injury has been met with limited success. Research
continues to attempt to identify agents that protect the
patient from the deleterious effects of the host response.
Knowing which patient may benefit from a particular
medication may be a function of that individuals unique
DNA. Current studies have identified specific genetic
polymorphisms that are predictors of adverse outcomes
in severe trauma and sepsis.58 Future investigation may
help develop individually tailored treatments.
ADULT RESPIRATORY DISTRESS SYNDROME
The adult respiratory distress syndrome (ARDS) is an
acute illness characterized by noncardiogenic pulmonary
PART I Principles in the Management of Traumatic Injuries
edema. This refractory hypoxemia arises in part as a
consequence of lung inflammation secondary to the
mediators of the acute response to trauma. Damage to
the alveolar-capillary interface results in intrapulmonary
shunting of blood, raised pulmonary vascular pressures,
and surfactant depletion.
The syndrome is primarily treated by mechanical ventilation, and the National Institutes of Health Acute
Respiratory Distress Syndrome Network has identified
that low tidal volume ventilation (6mL/kg predicted
body weight) was superior to using traditional tidal
volumes (12mL/kg of predicted body weight) in treating hypoxemia.59 When therapy fails to keep pace with
progressive lung dysfunction, alternative therapies
such as high-frequency oscillatory ventilation, prone
positioning, and extracorporeal life support (ECLS) or
extracorporeal membrane oxygenation (ECMO)may
be indicated.60-63
NUTRITION AS THERAPY
The advantages of enteral nutrition over parenteral
nutrition have been clearly demonstrated, and the gastrointestinal tract should be used whenever possible.
Recently, a role for supplemental parenteral nutrition
has been advocated (Fig. 1-4). The traditional preference is to feed patients by the enteral route for reasons
that include a reduction of the number of enteric organisms that may be responsible for bacterial translocation.
Stimulation of the enterocyte brush border and gutassociated lymphoid tissue is an important protective
mechanism against the proliferation of the offending
organisms.64 The route of feeding may also have an
impact on the production of cytokines after injury;
thus, use of the enteral route may confer an additional
advantage.65
Considerable attention has focused on nutrients that
attenuate the metabolic response to injury. Nutrients
that appear to enhance the immune system include arginine, glutamine, and nucleic acids. The immune system
may be enhanced by altering the relative amounts of
omega-6 versus omega-3 unsaturated fatty acids.66,67
Other nutrients may act as oxidants, preventing damage
by free radicals, such as the common antioxidants vitamins A, C, E, and the trace element selenium.
There has been lukewarm interest in the concept of
immunonutritionto ameliorate the end-organ damage
from critical illness and sepsis, which may later result in
acute renal failure and ARDS. A study of supplementation with an enteral diet of omega-3 fatty acid, gammalinolenic acid, and antioxidants versus an isocaloric
enteral formulation was reported in 2011. These nutrients are typically thought to modulate the systemic
inflammatory response.68 The study randomized 272
adults who had developed acute lung injury and required
mechanical ventilation. Enteral nutrition was provided to
both patient groups using a standard protocol, and the
study supplement was provided twice daily to the study
cohort of patients. The study was halted early because of
futility. The ventilator-free and intensive care unit-free
days were lower in the omega-3 group and, although not
significant, hospital and 60-day mortality were higher in
the omega-3 group.
A recent study comparing a special enteral formulation of eicosapentaenoic acid, gamma-linolenic acid, and
antioxidants versus a standard formulation to patients
during the early stages of sepsis (without organ failure)
yielded different results.69 The study, funded in part by
the product manufacturer, revealed no significant difference in mortality between the two groups. A significant
reduction in the appearance of cardiac and respiratory
failure occurred in the study population given the special
enteral formulation versus those given the standard
formula control. Subjects in the test arm also experienced
a benefit of fewer days on mechanical ventilation, fewer
days in the intensive care unit, and shorter length of hospital stay. The concept of immunonutrition continues to
evolve and, particularly within the last 5 years, the approach
to the modulation of nutrition by timing to feed, amounts,
route of administration,and composition of the nutritional product have yielded new information regarding
how to optimally feed injured and critically ill patients.
DEEP VEIN THROMBOSIS PROPHYLAXIS
The hypercoagulable state exists immediately following
severe traumatic injury, and an even more severe injury
may be followed by increases in the hypercoagulable
state.70 When this condition exists in combination with
patient immobility and direct venous injury, Virchows
triad for venous thrombosis is complete. Tissue injury
may be responsible for the release of tissue thromboplastin, which initiates the conversion of factor VII to enzyme
factor VIIa. Therefore, it is important to provide deep
venous thrombosis (DVT) prophylaxis with subcutaneous mixed or low-molecular-weight heparins when possible, except in cases in which specific contraindications
exist, such as intracranial hemorrhage, known peptic
ulcer, solid organ laceration, and hematoma. An alternative is the placement of a sequential compression device
on the limbs. The overall efficacy of DVT prophylaxis is
well established; it is important that prophylaxis be maintained for the duration of the hospital stay or at least
until the patient is fully mobile.71
Traumatic brain injury with intracranial hemorrhage
prohibits the use of chemoprophylaxis. Recent data have
demonstrated a three- to fourfold increased risk of DVT
in brain-injured patients. This patient population
requires early application of appropriate nonpharmacologic measures and an early decision on the placement
of inferior vena cava filters (removable, if possible) for
pulmonary embolism prophylaxis.72
STRESS GASTRITIS
Stress gastritis is common to the multiply injured intensive care unit population, and patients left untreated may
have clinically significant gastrointestinal bleeding. The
principal risk factors for stress gastritis are head injury,
mechanical ventilation, and abnormal coagulation profiles. Prophylaxis using histamine-2 receptor antagonists
or proton pump inhibitors is very effective.73
SUMMARY
Injury produces a series of physiologic changes mediated
by local and systemic agents and systemic effects, mainly
Metabolic Response to Trauma CHAPTER 1
cytokines, hormones, and activation of the sympathetic
nervous system. The metabolic response aims to promote
substrate delivery to the injured organs and promote
healing. However, in the setting of severe trauma, these
responses can result in organ injury, particularly to the
lungs. These consequences can produce significant morbidity and mortality. An appreciation of nuances of the
metabolic response allows the clinician to support the
patient through the physiologic changes associated with
the stress response caused by injury. Future research
offers the promise of directly tailoring treatment and
modulating the metabolic response to minimize the
impact of major trauma.
REFERENCES
1. Cuthbertson D: Observations on the disturbance of metabolism
produced by injury to the limbs. Q J Med 1:233, 1932.
2. Cuthbertson D: Postshock metabolic response. Lancet 1:433, 1942.
3. Cuthbertson D: The disturbance of metabolism produced by bony
and non-bony injury, with notes on certain abnormal conditions of
bone. Biochem J 24:1244, 1930.
4. Cree MG, Wolfe RR: Postburn trauma insulin resistance and fat
metabolism. Am J Physiol Endocrinol Metab 294:E1E9, 2007.
5. Birkhahn RH, Long CL, Fitkin D, et al: Effects of major skeletal
trauma on whole body protein in man measured by L-[1,14C]leucine. Surgery 88:294299, 1980.
6. Kien CL, Young VR, Rohrbaugh DK, et al: Increased rates of whole
body protein synthesis and breakdown in children recovering from
burns. Ann Surg 187:383391, 1978.
7. Rose H, Venn R: Recently published papers: Dying Swans and other
stories. Crit Care 10:152, 2006.
8. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wheeler AP,
Bernard GR, Thompson BT, et al: Pulmonary-artery versus central
venous catheter to guide treatment of acute lung injury. N Engl J
Med 354:22132224, 2006.
9. Cecconi M, Dawson D, Casaretti R, et al: A prospective study of the
accuracy and precision of continuous cardiac output monitoring
devices as compared to intermittent thermodilution. Minerva Anesthesiol 76:10101017, 2010.
10. Eachempati SR, Barie PS: Minimally invasive and non-invasive diagnosis and therapy in critically ill and injured patients. Arch Surg
134:11891196, 1999.
11. Pal JD, Victorino GP, Twomey P, et al: Admission serum lactate
levels do not predict mortality in the acutely injured patient.
J Trauma 60:583587, 2006.
12. McMahon CG, Yates DW, Campbell FM, et al: Unexpected contribution of moderate traumatic brain injury to death after major
trauma. J Trauma 47:891895, 1999.
13. Losiniecki A, Shutter L: Management of traumatic brain injury.
Curr Treat Options Neurol 12(2):142154, 2010.
14. Diringer MN, Videen TO, Yundt K, et al: Regional cerebrovascular
and metabolic effects of hyperventilation after severe traumatic
brain injury. J Neurosurg 96:103108, 2002.
15. Dempsey DT, Guenter P, Mullen JL, et al: Energy expenditure in
acute trauma to the head with and without barbiturate therapy.
Surg Gynecol Obstet 160:128134, 1985.
16. Masel BE: Hyperbaric oxygen therapy for traumatic brain injury:
Still an enigma. Arch Phys Med Rehabil 92:15191521, 2011.
17. Davies CL, Newman RJ, Molyneux SG, et al: The relationship
between plasma catecholamines and severity of injury in man.
J Trauma 24:99105, 1984.
18. Barton RN: Neuroendocrine mobilization of body fuels after injury.
Br Med Bull 41:218225, 1985.
19. Buckingham JC: Hypothalamo-pituitary responses to trauma. Br
Med Bull 41:203211, 1985.
20. Bessey PQ, Watters JM, Aoki TT, et al: Combined hormonal infusion stimulates the metabolic response to injury. Ann Surg 200:264
281, 1984.
21. Stoner HB: Metabolism after trauma and sepsis. Circ Shock 19:75
87, 1986.
22. Beutler B, Cerami A: Cachectin and tumour necrosis factor as two
sides of the same biological coin. Nature 320:584588, 1986.
23. Kaushansky K, Broudy VC, Harlan JM, et al: Tumor necrosis factor
alpha and tumor necrosis factor beta (lymphotoxin) stimulate the
production of granulocyte-macrophage colony-stimulating factor,
macrophage colony-stimulating factor and IL-1 in vivo. J Immunol
141:34103415, 1988.
24. Brown JM. Grosso MA, Harken AH: Cytokines sepsis and the
surgeon. Surg Gynecol Obstet 169:568575, 1989.
25. Dinarello CA, Wolff SM: Molecular basis of fever in humans.
Am J Med 72:799819, 1982.
26. Moser R, Schleiffenbaum B, Groscurth P, et al: Interleukin 1 and
tumor necrosis factor stimulate human vascular endothelial cells
to promote transendothelial neutrophil passage. J Clin Invest
83:444455, 1989.
27. Morimoto A, Sakata Y, Watanabe T, et al: Characteristics of fever
and acute phase response induced in rabbits by IL-1 and TNF.
Am J Physiol 256:R35R41, 1989.
28. Dinarello CA, Mier JW: Lymphokines. N Engl J Med 317:940945,
1987.
29. Atkins E, Wood WB, Jr: Studies on the pathogenesis of fever:
Identification of an endogenous pyrogen in the bloodstream
following insertion of typhoid vaccine. J Exp Med 102:499516,
1955.
30. Dinarello CA, Bernheim HA: Ability of human leukocytic pyrogen
to stimulate brain prostaglandin synthesis in vitro. J Neurochem
37:702708, 1981.
31. Dinarello C: Interleukin-1: Amino acid sequences, multiple biological sequences and comparison with tumour necrosis factor (cachectin). Year Immunol 2:6889, 1986.
32. Clowes GH, Jr, George BC, Villee CA, Jr, et al: Muscle proteolysis
induced by a circulating peptide in patients with sepsis or trauma.
N Engl J Med 308:545552, 1983.
33. Clowes GH, Jr, Hirsch E, George BC, et al: Survival from sepsis: The
significance of altered protein metabolism regulated by proteolysis
inducing factor, the circulating cleavage products of interleukin-1.
Ann Surg 202:446458, 1985.
34. Hirano T, Yasukawa K, Harada H, et al: Complementary DNA for
a novel human interleukin (BSF-2) that induces B lymphocytes to
produce immunoglobulin. Nature 324:7376, 1986.
35. Castell JV, Gmez-Lechn MJ, David M, et al: Acute-phase response
of human hepatocytes: Regulation of acute phase protein synthesis
by interleukin-6. Hepatology 12:11791186, 1990.
36. Cinat ME, Waxman KS, Vaziri ND, et al: Soluble cytokine receptors
and receptor agonists are sequentially released after trauma.
J Trauma 39:112118, 1995.
37. Johannes F, Marcus M, Jochen K, et al: Circulating inflammatory
and metabolic parameters to predict organ failure after multiple
trauma. Eur J Trauma 28:333339, 2002.
38. Woiciechowsky C, Shhoning B, Cobanov J, et al: Early IL-6 plasma
concentrations correlate with severity of brain injury and pneumonia in brain-injured patients. J Trauma 52:339345, 2002.
39. Hoch RC, Rodriguez R, Manning T, et al: Effects of accidental
trauma on cytokine and endotoxin production. Crit Care Med
21:839845, 1993.
40. Donnelly TJ, Meade P, Jagels M, et al: Cytokine, complement, and
endotoxin profiles associated with the development of the adult
respiratory distress syndrome after severe injury. Crit Care Med
22:768776, 1994.
41. Moore FA, Moore EE, Poggetti R, et al: Gut bacterial translocation
via the portal vein: A clinical perspective in patients with major
torso trauma. J Trauma 31:629638, 1991.
42. Botha AJ, Moore FA, Moore EE, et al: Early neutrophil sequestration after injury: A pathogenic mechanism for multiple organ
failure. J Trauma 39:411417, 1995.
43. Botha AJ, Moore FA, Moore EE, et al: Effects of accidental trauma
on cytokine and endotoxin production. Crit Care Med 22:894,
1994.
44. Cerra FB: Hypermetabolism, organ failure and metabolic support.
Surgery 101:114, 1987.
45. Fink MP: Another negative trial of a new agent for the treatment
of sepsis: Rethinking the process of developing adjuvant treatments
for serious infection [editorial]. Crit Care Med 23:989, 1995.
46. Bernard GR, Wheeler AP, Russel JA, et al: The effects of ibuprofen
on the physiology and survival of patients with sepsis. N Engl J Med
336:912918, 1997.
PART I Principles in the Management of Traumatic Injuries
47. Van Den Berghe G, Wouters P, Weeker F, et al: Intensive insulin
therapy in the critically ill patients. N Engl J Med;345:13591367,
2001.
48. Finfer S, Chittock DR, Su SY, et al: Intensive versus conventional
glucose control in critically ill patients. N Engl J Med 360:12831297,
2009.
49. Cooper MS, Stewart PM: Corticosteroid insufficiency in acutely ill
patients. N Engl J Med 348:727734, 2003.
50. Albert SG, Ariyan S, Rather A, et al: The effect of etomidate on
adrenal function in critical illness: A systematic review. Intensive Care
Med 37:901910, 2011.
51. Sprung CL, Annane D, Keh D, et al: Hydrocortisone therapy for
patients with septic shock. N Engl J Med 358:111124, 2008.
52. Annane D, Sbille V, Charpentier C, et al: Effect of treatment with
low doses of hydrocortisone and fludrocortisone on mortality in
patients with septic shock. JAMA 288:862871, 2002.
53. Annane D, Bellissant E, Bollaert PE, et al: Corticosteroids in the
treatment of severe sepsis and septic shock in adults: A systematic
review. JAMA 301:23622375, 2009.
54. Roquilly A, Mahe PJ, Seguin P, et al: Hydrocortisone therapy for
patients with multiple trauma. JAMA 305:12011209, 2011.
55. Roberts I, Yates D, Sandercock P, et al: Effect of intravenous corticosteroids on death within 14 days in 10,008 adults with clinically
significant head injury (MRC CRASH trial): Randomised placebocontrolled trial. Lancet 354:16711684, 2004.
56. Bernard GR, for the Recombinant Human Activated Protein C
Worldwide Evaluation in Severe Sepsis (PROWESS) Study Group:
Efficacy and safety of recombinant human activated protein C for
severe sepsis. N Engl J Med 344:699709, 2001.
57. European Medicines Agency: Xigris [drotrecogin alfa (activated)]
to be withdrawn due to lack of efficacy, (http://www.ema.europa.eu/
ema/index.jsp?curl=pages/news_and_events/news/2011/10/
news_detail_001373.jsp&mid=WC0b01ac058004d5c1&jsenabled=
true). 2011.
58. Hildebrand F, Mommsen P, Frink M, et al: Genetic predisposition
for development of complications in multiple trauma patients.
Shock 35:440448, 2011.
59. The Acute Respiratory Distress Syndrome Network: Ventilation
with lower tidal volumes as compared with traditional tidal volumes
for acute lung injury and the acute respiratory distress syndrome.
N Engl J Med 342:13011308, 2000.
60. Derdak S, Mehta S, Stewart TE, et al: High-frequency oscillatory
ventilation for acute respiratory distress syndrome in adults.
Am J Resp Crit Care Med 166:801808, 2002.
61. Gattinoni L, Tognoni LG, Pesenti A, et al: Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl
J Med 345:568573, 2001.
62. Shapiro MB, Anderson HL, 3rd, Bartlett RH: Respiratory failure:
Conventional and high-tech support. Surg Clin North Am 80:871
883, 2000.
63. Peek GJ, Mugford M, Tiruvoipati R, et al: Efficacy and economic
assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure
(CESAR): A multicentre randomised controlled trial. Lancet
374:13511363, 2009.
64. Li J, Kudsk KA, Gocinski B, et al: Effects of parenteral and enteral
nutrition on gut-associated lymphoid tissue. J Trauma 39:4452,
1995.
65. Fong YM, Marano MA, Barber A, et al: Total parenteral nutrition
and bowel rest modify the metabolic response to endotoxin in
humans. Ann Surg 210:449457, 1989.
66. Goeters C, Wenn A, Mertes N, et al: Parenteral l-alanyl-l-glutamine
improves 6-month outcome in critically ill patients. Crit Care Med
30:20322037, 2002.
67. Billiar TR, Bankey PE, Svingen BA, et al: Fatty acid intake and
Kupffers cell function: Fish oil alters eicosanoid and monokine
production to endotoxin stimulation. Surgery 104:343349, 1988.
68. Rice TW, Wheeler AP, Thompson BT, et al: Enteral omega-3 fatty
acid, gamma-linolenic acid, and antioxidant supplementation in
acute lung injury. JAMA 306:15741581, 2011.
69. Pontes-Arruda A, Martins LF, de Lima SM, et al: Investigating Nutritional Therapy with EPA, GLA and Antioxidants Role in Sepsis
Treatment (INTERSEPT) Study Group: Enteral nutrition with
eicosapentaenoic acid, gamma-linolenic acid and antioxidants in
the early treatment of sepsis: Results from a multicenter, prospective, randomized, double-blinded, controlled study: The INTERSEPT Study. Crit Care 5:R144, 2011.
70. Engelman DT, Gabram SG, Allen L, et al: Hypercoagulability following multiple trauma. World J Surg 20:510, 1996.
71. Davidson BL, Sullivan SD, Kahn SR, et al: The economics of venous
thromboembolism prophylaxis: a primer for clinicians. Chest
124:393S396S, 2003.
72. Reiff DA, Haricharan RN, Bullington NM, et al: Traumatic brain
injury is associated with the development of deep venous thrombosis independent of pharmacologic prophylaxis. J Trauma 66:
14361440, 2009.
73. Steinberg KP: Stress-related mucosal disease in the critically ill
patient: risk factors and strategies to prevent stress-related bleeding
in the intensive care unit. Crit Care Med 30:S362S364, 2002.
You might also like
- Respuesta Metabolica Al Trauma Cap 1 FonsecaDocument6 pagesRespuesta Metabolica Al Trauma Cap 1 FonsecaJulio Magaña QuiñonesNo ratings yet
- Response To Trauma and Metabolic Changes: Posttraumatic MetabolismDocument13 pagesResponse To Trauma and Metabolic Changes: Posttraumatic MetabolismCar OrdzNo ratings yet
- Systemic Response To InjuryDocument5 pagesSystemic Response To InjuryJohn Christopher LucesNo ratings yet
- 1 Metabolic Response To InjuryDocument15 pages1 Metabolic Response To InjuryDelete AccountNo ratings yet
- 250 Latest Surgical Background Multiple - HTML PDFDocument32 pages250 Latest Surgical Background Multiple - HTML PDFazizNo ratings yet
- Corticosteroid Adverse Effects - StatPearls - NCBI BookshelfDocument12 pagesCorticosteroid Adverse Effects - StatPearls - NCBI Bookshelfantonio.mastrangelo.999No ratings yet
- General Surgery MCQDocument190 pagesGeneral Surgery MCQلمسة مصمم100% (1)
- General Surgery MCQDocument249 pagesGeneral Surgery MCQShriyansh Chahar88% (8)
- "Metabolic Staging" After Major Trauma - A Guide For Clinical Decision Making?Document3 pages"Metabolic Staging" After Major Trauma - A Guide For Clinical Decision Making?Marani MalikNo ratings yet
- 001-Basic Surgical BackgroundDocument101 pages001-Basic Surgical BackgroundAhmed Zaghw100% (1)
- 1 Metabolic Response To InjuryDocument5 pages1 Metabolic Response To InjuryMohamad AlfarisNo ratings yet
- Clinical CaseDocument25 pagesClinical CaseRussell Talan CilotNo ratings yet
- 204 Enhanced Recovery After Surgery (ERAS) PDFDocument9 pages204 Enhanced Recovery After Surgery (ERAS) PDFomkitNo ratings yet
- Response To Trauma and Metabolic Changes: Posttraumatic MetabolismDocument7 pagesResponse To Trauma and Metabolic Changes: Posttraumatic MetabolismHeartfiliaNo ratings yet
- Response To Trauma and Metabolic Changes: Posttraumatic MetabolismDocument7 pagesResponse To Trauma and Metabolic Changes: Posttraumatic MetabolismFanny BudimanNo ratings yet
- Shock EmergenciesDocument19 pagesShock Emergenciesjinopic306No ratings yet
- Enhanced Recovery After Surgery (Eras) Anaesthesia Tutorial of The Week 204 8 November 2010Document9 pagesEnhanced Recovery After Surgery (Eras) Anaesthesia Tutorial of The Week 204 8 November 2010Abhishek LonikarNo ratings yet
- Metabolic Response To InjuryDocument55 pagesMetabolic Response To InjuryMuhammad NaveedNo ratings yet
- Stress ResponseDocument8 pagesStress ResponseBharathi DasanNo ratings yet
- 003Document358 pages003Gordana UzelacNo ratings yet
- Use Pre Post OperativeDocument9 pagesUse Pre Post Operativesam mehraNo ratings yet
- Response To SurgeryDocument5 pagesResponse To SurgerySarda KangabamNo ratings yet
- Acute Fluid Management of Large Burns Pathophysiology, Monitoring, and ResuscitationDocument9 pagesAcute Fluid Management of Large Burns Pathophysiology, Monitoring, and ResuscitationEduardo Espin LanzNo ratings yet
- Metabolic Response To The Stress of Critical IllnessDocument10 pagesMetabolic Response To The Stress of Critical IllnessNguyen van ChienNo ratings yet
- Leucocytosis A Mild Anemia Resulting From Both Bone Marrow Suppression and Iatrogenic Blood-Taking Is Common ThrombocytopeniaDocument2 pagesLeucocytosis A Mild Anemia Resulting From Both Bone Marrow Suppression and Iatrogenic Blood-Taking Is Common ThrombocytopeniaMuhammad Edwin IndraNo ratings yet
- Bailey 5th Ed. 2014 (1125-1318) - TraumaDocument194 pagesBailey 5th Ed. 2014 (1125-1318) - TraumaelFadhlyNo ratings yet
- Left Ventricular Hypertrophy: CirculationDocument20 pagesLeft Ventricular Hypertrophy: Circulationprok prokNo ratings yet
- Multiple Organ Dysfunction SyndromeDocument21 pagesMultiple Organ Dysfunction SyndromeRo-Anne LozadaNo ratings yet
- Systemic Effects of Surgical Stress: M.Bharathidasan MVM 13048Document32 pagesSystemic Effects of Surgical Stress: M.Bharathidasan MVM 13048Bharathi DasanNo ratings yet
- The First 24 Hours Burn Shock Resuscitation and Early ComplicationsDocument11 pagesThe First 24 Hours Burn Shock Resuscitation and Early Complicationskarely EspinozaNo ratings yet
- Ns. Fetreo Negeo Putra, S.Kep.,M.KepDocument67 pagesNs. Fetreo Negeo Putra, S.Kep.,M.KepAnggraini DarmawinantiNo ratings yet
- ShockDocument43 pagesShocklax prajapatiNo ratings yet
- Administering Corticosteroids in Neurologic Diseases3724Document12 pagesAdministering Corticosteroids in Neurologic Diseases3724Carmen BritoNo ratings yet
- L08: Inflammation (Acute and Chronic), Healing, Repair and OsteomyelitisDocument9 pagesL08: Inflammation (Acute and Chronic), Healing, Repair and Osteomyelitishstest842No ratings yet
- Mechanobiology and Diseases of Mechanotransduction: Donald E IngberDocument14 pagesMechanobiology and Diseases of Mechanotransduction: Donald E IngberTezar AndreanNo ratings yet
- Stress Hyperglycemia and Innate Immune System CellsDocument9 pagesStress Hyperglycemia and Innate Immune System CellsJuan Fernando BolivarNo ratings yet
- Early Hemodynamic Management of Critically Ill Burn PatientsDocument7 pagesEarly Hemodynamic Management of Critically Ill Burn PatientsItzel TextaNo ratings yet
- Introduction To Surgery Short NotesDocument580 pagesIntroduction To Surgery Short Notesgizachew assefaNo ratings yet
- Surgical Nutrition PDFDocument21 pagesSurgical Nutrition PDFXana SoaresNo ratings yet
- Lesson 2 Life Treathening ConditionDocument53 pagesLesson 2 Life Treathening ConditionMonasque PamelaNo ratings yet
- Pathophysiology of Traumatic Shock: International Traumacare (Itaccs)Document4 pagesPathophysiology of Traumatic Shock: International Traumacare (Itaccs)Irina OdajiuNo ratings yet
- Total Scar Management: From Lasers to Surgery for Scars, Keloids, and Scar ContracturesFrom EverandTotal Scar Management: From Lasers to Surgery for Scars, Keloids, and Scar ContracturesRei OgawaNo ratings yet
- Muscle Injury FWRDocument8 pagesMuscle Injury FWREdward TimbancayaNo ratings yet
- Metabolic Response To The Stress of Critical IllnessDocument10 pagesMetabolic Response To The Stress of Critical IllnessValentina bustamanteNo ratings yet
- Anesthesia, Analgesia, and The Surgical Stress ResponseDocument8 pagesAnesthesia, Analgesia, and The Surgical Stress Responsejannatin aliya indrinaNo ratings yet
- Shock UciDocument16 pagesShock UciTania Parra MoralesNo ratings yet
- General Adaptation Syndrome TheoriesDocument4 pagesGeneral Adaptation Syndrome TheoriesHema JothyNo ratings yet
- Hyperinsulin Dan MakrofagDocument10 pagesHyperinsulin Dan Makrofageki_herawatiNo ratings yet
- Multiple Organ Dysfunction SyndromeDocument4 pagesMultiple Organ Dysfunction SyndromeAna Reyes100% (1)
- Mclarty 2012Document7 pagesMclarty 2012Gisele CanelaNo ratings yet
- What, How, Andhow Muchshouldpatients Withburnsbefed?Document21 pagesWhat, How, Andhow Muchshouldpatients Withburnsbefed?Zahira Gomez CarmonaNo ratings yet
- Patho Final Study GuideDocument55 pagesPatho Final Study GuideBritNo ratings yet
- Indirect Calorimetry in Clinical PracticeDocument19 pagesIndirect Calorimetry in Clinical PracticeivanovichNo ratings yet
- Crush InjuryDocument4 pagesCrush InjuryMuhammad Nur ArifinNo ratings yet
- CC CC: YY YYDocument54 pagesCC CC: YY YYnyzgirl17No ratings yet
- Modifying Stress Response A CL 2021Document11 pagesModifying Stress Response A CL 2021Alejandra SanchezNo ratings yet
- Practical Class - Absolute Eosinophil CountDocument10 pagesPractical Class - Absolute Eosinophil CountZainMalik75% (4)
- TrematodesDocument4 pagesTrematodesBlitzen BusaingNo ratings yet
- Case Report Metabolic SyndromeDocument57 pagesCase Report Metabolic SyndromeAnugrah Wulan Fitri100% (1)
- Reviewer: Mendelian Inheritance X-Linked Dominant Inheritance X-Linked Dominant InheritanceDocument3 pagesReviewer: Mendelian Inheritance X-Linked Dominant Inheritance X-Linked Dominant InheritanceMary Rose FabianNo ratings yet
- Anesthesia For Diabetic PatientsDocument25 pagesAnesthesia For Diabetic PatientsfirlaflaNo ratings yet
- Geriatric Physical TherapyDocument6 pagesGeriatric Physical Therapyirdasriwahyuni0% (1)
- Bovine Ephemeral FeverDocument4 pagesBovine Ephemeral FeverAbdullah SaleemNo ratings yet
- NCM 105 SyllabusDocument8 pagesNCM 105 SyllabuslouradelNo ratings yet
- ACC Handbook Ascvd Type 2 Diabetes: On andDocument10 pagesACC Handbook Ascvd Type 2 Diabetes: On andZH. omg sarNo ratings yet
- Scrub TyphusDocument4 pagesScrub TyphusVijaya Aditya TadepalliNo ratings yet
- WPC AssignmentDocument2 pagesWPC AssignmentPragya SinghNo ratings yet
- The Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-AnalysisDocument52 pagesThe Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-Analysiseduardobar2000100% (1)
- STRABISMDocument30 pagesSTRABISMCindy ChristensenNo ratings yet
- Alcohol and Alcohol-Related Problems in Caraka SamhitaDocument14 pagesAlcohol and Alcohol-Related Problems in Caraka SamhitaAshu SinghNo ratings yet
- BANDAGINGDocument12 pagesBANDAGINGKAREN CARI�ONo ratings yet
- MedicationsDocument2 pagesMedicationsanon_580894596No ratings yet
- SucralfateDocument3 pagesSucralfateViziteu AlexandraNo ratings yet
- Case AnaDocument12 pagesCase AnaBiel DelcanoNo ratings yet
- Outwitting Our Nerves A Primer of Psychotherapy by Jackson and SalisburyDocument71 pagesOutwitting Our Nerves A Primer of Psychotherapy by Jackson and SalisburyДмитрий ГвоздевNo ratings yet
- In-Patient Claim Form: (To Be Filled by Claimant Employee)Document2 pagesIn-Patient Claim Form: (To Be Filled by Claimant Employee)Khan LalaNo ratings yet
- Basic Clinical Chemistry PDFDocument72 pagesBasic Clinical Chemistry PDFJacc jaccNo ratings yet
- Health Promot. Int.-2009-Peerson-285-96 PDFDocument12 pagesHealth Promot. Int.-2009-Peerson-285-96 PDFPooja KapoorNo ratings yet
- The Right To Die EssayDocument1 pageThe Right To Die EssayVerdurecikNo ratings yet
- MOH PAPER Prometric ExamDocument58 pagesMOH PAPER Prometric ExamRPh Farhatain100% (3)
- Mestinon: Ame of The MedicineDocument6 pagesMestinon: Ame of The MedicinekhanztheconzNo ratings yet
- Epidemiology of Typhoid Fever in The PhilippinesDocument5 pagesEpidemiology of Typhoid Fever in The Philippinesjessica_nava_8No ratings yet
- Assessing The Signs of DementiaDocument5 pagesAssessing The Signs of DementiaastrogliaNo ratings yet
- Tetanus (Deadly Diseases and Epidemics)Document101 pagesTetanus (Deadly Diseases and Epidemics)Russel Floyd Sulit100% (1)
- Cardiology High Blood Pressure - University of Nigeria Nsukka 73rd-Inaugural-Lecture - OnwubereDocument29 pagesCardiology High Blood Pressure - University of Nigeria Nsukka 73rd-Inaugural-Lecture - OnwubereAnonymous 9QxPDpNo ratings yet
- TrajectoryDocument29 pagesTrajectoryDithaALkunaNo ratings yet