Professional Documents
Culture Documents
Refraksi 1
Uploaded by
Elyani RahmanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Refraksi 1
Uploaded by
Elyani RahmanCopyright:
Available Formats
1040-5488/16/9304-0344/0 VOL. 93, NO. 4, PP.
344Y352
OPTOMETRY AND VISION SCIENCE
Copyright * 2016 American Academy of Optometry
ORIGINAL ARTICLE
Myopia Control with Bifocal Contact Lenses:
A Randomized Clinical Trial
Thomas A. Aller*, Maria Liu, and Christine F. Wildsoet
ABSTRACT
Purpose. Most studies have reported only minimal reductions in myopia progression with bifocal or progressive multifocal
spectacles, although somewhat larger, although mostly still clinically insignificant, effects have been reported in children
with nearpoint esophoria and/or accommodative dysfunctions. The CONTROL study was a 1-year, prospective, randomized, clinical trial of bifocal contact lenses for control of myopia in children with eso fixation disparities at near.
Methods. Eighty-six myopic subjects, aged 8 to 18 years, were enrolled in the study after passing the screening examination. Of these, 79 completed lens assignment and 78 completed the study. The mean refractive error of these 79 subjects
was j2.69 T 1.40D (SD), and all had progressed by j0.50D or more since their last examination. All subjects also had eso
fixation disparity at near. Subjects were randomly assigned to wear either Vistakon Acuvue 2 (single-vision soft contact
lenses [SVSCLs]) or Vistakon Acuvue Bifocal (bifocal soft contact lenses [BFSCLs]). Bifocal adds were selected to neutralize
the associated phoria. Treatment outcomes included cycloplegic autorefraction and axial length, assessed in terms of
changes after 6 and 12 months of treatment from pretreatment baseline values.
Results. The BFSCLs significantly slowed myopia progression, with statistically significant differences between the treatment groups after 6 months. After 12 months of treatment, the SVSCL group had progressed by j0.79 T 0.43D compared
with j0.22 T 0.34D for the BFSCL group (cycloplegic objective spherical equivalent, average of two eyes). Corresponding
axial length changes were 0.24 T 0.17 mm and 0.05 T 0.14 mm, respectively. All of these differences were found to be
statistically significant (unpaired t-tests, p G 0.001).
Conclusions. The distance center bifocal contact lenses tested in this study achieved greater control over myopia progression and axial elongation (970%) compared with most published results with multifocal spectacles. Further studies are
warranted to identify the critical factors and mechanisms underlying this myopia control effect.
(Optom Vis Sci 2016;93:344Y352)
Key Words: myopia control, myopia, bifocal contact lenses, esophoria, associated phoria, fixation disparity
yopia is the focus of growing attention and concern
because of the now extremely high prevalence of
myopia in some East Asian populations. Remarkably,
myopia prevalence figures in the mid to high 90 percent have
been reported in some studies of university student populations in
Taiwan1 and Shanghai,2 with a figure of 96.5% being reported
for young adult Korean male conscripts in Seoul.3 Equivalent
prevalence figures for the United States have also been trending
upward, albeit lagging behind those of East Asia. For example, comparison of data from two studies of the same population
*OD
OD, PhD
PhD, DipAppScOptom, FAAO
Vision Cooperative Research Centre, Sydney, New South Wales, Australia
(TAA); and School of Optometry, University of California, Berkeley, Berkeley,
California (ML, CFW).
across the periods 1971 to 1972 and 1999 to 2004 revealed an
increase in the prevalence of myopia from 25% to 41.6% for
the 12- to 54-year age range (after adjustment for differences
in the methods used to detect myopia).4 These figures would
not be of concern were it not for the well-established link between myopia and sight-threatening ocular pathologies. Importantly, and as well summarized in a recent review by Flitcroft,5
even low myopia is associated with an increased risk of pathology, with the latter, measured in terms of odds ratios, simply
increasing with increasing myopia. Myopes are at an increased
risk of myopic maculopathy, retinal detachment, cataracts, and
glaucoma, with myopic maculopathy now the leading cause of
monocular blindness in Japan and of new cases of blindness
in Shanghai.6,7
The rapidly changing myopia prevalence figures are consistent
with the increasing acceptance of the role that environmental
influences play in the development of myopia. Some but not all
Optometry and Vision Science, Vol. 93, No. 4, April 2016
Myopia Control with Bifocal Contact LensesVAller et al.
studies have linked myopia with increased near work, for example,
books read,8 and one recent German study showed a correlation
between years of formal education with level of myopia.9 There
are other studies pointing to outdoor activities being protective
against the development of myopia.10 Although unresolved are the
specific factors contributing to myopia development and progression, that visual experience seems to play a central role has
refocused attention on the possibility that myopia progression can
and should be controlled.
Studies involving animal models for myopia (chicks, guinea
pigs, marmosets, rhesus monkeys) provide compelling evidence
for active emmetropization and a role for optical defocus in ocular
growth modulation.11,12 Specifically, hyperopic defocus imposed
on young eyes accelerates eye growth while imposed myopia slows
it.13,14 Local retinal mechanisms have been implicated,15 with the
peripheral retina apparently playing an important role in ocular
growth regulation.16Y19 Of relevance to the current study, in recent animal model studies, multifocal lenses incorporating zones
of positive power were found to inhibit eye growth, even when
these zones are limited to the periphery of the lenses.20Y22 For
already myopic eyes, both stabilization of myopia and reversal
have been described.21,23
The above observations with animal models, translated to
human myopia, raise the possibility of increased progression with
standard corrective spectacle and soft contact lenses, given that the
image shell providing accurate on-axis focus typically falls increasingly behind the retina with increasing distance off-axis.24
Furthermore, more prolate eye shapes, a common finding in
myopia, are expected to exaggerate this problem.25 Conversely,
prescribing optical devices that impose peripheral myopic defocus
is predicted to slow myopia progression, consistent with results
from a number of independent myopia control studies involving
orthokeratology,26Y29 which produces a relative myopic shift in
peripheral retinal defocus, a consequence of induced corneal shape
changes.30
The Control Of NearsightednessYTRial Of Lenses (CONTROL)
study reported here investigated myopia progression with distance
center multi-ring bifocal soft contact lenses (BFSCLs) compared
with single-vision soft contact lenses (SVSCLs) in children. It
was prospective and double masked. Motivation for the study
came partly from promising retrospective data collected from
the practice of one of the authors (TA), in which BFSCLs had
been prescribed as a substitute for bifocal spectacles to address
the compliance issues (Aller et al., OVS 2000;77(12s):182).
Emerging results from animal studies showing that imposed
myopic defocus is a potent inhibitor of eye growth, as discussed
above, provided additional motivation. The study was limited to
myopes with associated esophoria at near based on reports from
earlier intervention studies that bifocal spectacles were more
effective in slowing myopia progression in those with near
esophoria31,32 and results from subgroup analysis in the original
COMET study that revealed subjects with near esophoria to be
among those to show least myopia progression.33
We report here highly clinically and statistically significant
slowing of myopia progression with BFSCLs, exceeding results
from all published optical intervention trials for control of myopia
progression to date and directly reflecting a slowing of axial
elongation relative to changes with SVSCLs. The study design and
345
results are described in the following sections, and implications are
discussed in the context of potential underlying mechanisms and
the broader topic of control of myopia progression. Study results
have also been reported in abstract form previously.34,35
METHODS
Study Design
This study involved a randomized double-masked design, with
two treatment groups of young progressing myopes wearing either
distance center (alternating 5-ring) BFSCLs (Vistakon Acuvue
Bifocal) or SVSCLs (Vistakon Acuvue 2). Both were made from
58% etafilcon A visibility tinted material. In both cases, lenses
were worn on a daily wear basis for 12 months, with a 2-week
replacement schedule and Optifree solutions (provided by
Alcon) used for cleaning, rinsing, and disinfection.
The lenses were delivered to the subjects in their original
containers with tamper-proof opaque masking labels. Because of
the relatively small group (sample) sizes involved, a modified
covariate adaptive randomization approach was used to allocate
treatments. Specifically, subjects were randomly assigned a treatment
by the masked off-site clinical trial coordinator who used an adaptive
biased coin toss design to increase the probability that successive
subjects were assigned to the group with the smaller sample size
with respect to age, refractive error, amount of eso-associated near
phoria, sex, and Asian versus non-Asian ethnicity.36,37 The study
examiner, office staff, subjects, and parents were not aware of the
lens assignments before the end of the study.
Subjects were required to attend a maximum of six office visits,
which included an initial measurement session to collect baseline
ocular biometric and refraction data, and follow-up measurement
sessions at 6 and 12 months, at which biometric and refraction
data were again collected. Other sessions included a contact lens
fitting session, a contact lens dispensing/training session, and a
routine contact lens follow-up session to verify that the lenses fit
satisfactorily and were without adverse effects on ocular health.
The study was conducted in the clinical practice of TA after the
protocol was reviewed and approved by Quorum Review IRB.
The study followed the tenets of the Declaration of Helsinki and is
listed on clinicaltrials.gov (NCT00214487).38
Subject Selection
Informed assent was obtained from all subjects, and informed
consent was obtained from all parents or guardians. All subjects
also underwent an on-site vision screening before acceptance into
the study. Selection and exclusion criteria covered the refractive
error and binocular vision profiles of the subjects, freedom from
confounding ocular or systemic diseases, as well as ability to wear
soft contact lenses. In brief, based on manifest subjective refractions, eligible subjects were limited to those in whom each eye
exhibited j0.50D or more myopia in the least myopic meridian,
j6.00D or less myopia in the most myopic meridian, anisometropia of 2.00D or less, refractive astigmatism of 1.00D or less,
and best-corrected visual acuity of 20/20 or better in each eye.
All refractive error data here and elsewhere are referenced to
the corneal plane. In addition, subjects were required to have
Optometry and Vision Science, Vol. 93, No. 4, April 2016
346 Myopia Control with Bifocal Contact LensesVAller et al.
progressed by j0.50D or more in one or both eyes since their last
examination based on clinical records, results of spectacle neutralization, or written prescriptions. This selection criterion was
included to limit the study to those experiencing myopia progression, and thus the timing of the last eye examination of individual subjects was not itself limited. Only those with near esoassociated phoria through their distance correction, measured as
the amount of plus power required to neutralize their fixation
disparity at their habitual viewing distance and angle for reading,
were included.
Existing soft contact lens wearers, as well as nonYcontact lens
wearers, were accepted into the study, with current wearers being
required to discontinue wear for 1 week before initial evaluation
for this study. NonYcontact lens wearers underwent routine
clinical prefitting assessment to first verify their suitability for
contact lens wear, although there was no run-in period before
enrollment. Specific exclusion criteria included any pathology that
may alter eye growth (e.g., history of retinal detachment) and/or
adversely impact on their ability to successfully wear contact lenses
(e.g., moderate to severe, or poorly treated, chronic allergic
conjunctivitis) and prior ocular surgery. Also excluded were
subjects who had worn rigid contact lenses within the preceding
2 years or soft contact lenses on an extended wear basis within the
preceding 6 months. Other exclusion criteria included nursing or
pregnant mothers and participants who were unable to commit to
the 12 months of contact lens wear and follow-up testing or who
had a high likelihood of leaving the area within the 12-month
study period.
Study Methods
Key baseline measurements included refraction, ocular biometry, keratometry, and near associated phorias. All were undertaken either at the same time as the vision screening session or in a
follow-up session. Refractive errors were measured both objectively and subjectively with and without cycloplegia (30 min after
two drops of 1% tropicamide administered 5 min apart). Objective refraction data were obtained using a Nidek (Marco) ARK
700 auto-refractor, with nine valid readings averaged for each eye.
Monocular subjective refractions were followed by binocular
Polaroid balance using the endpoint of least minus power for bestcorrected visual acuity. Both procedures were repeated after
cycloplegia was achieved. Only objective refractive error data
obtained under cycloplegia are reported here. The distance powers
of selected SVSCL and BFSCL represented in each case the
minimum minus power providing monocular visual acuity of
20/30 or better. Axial lengths and anterior chamber depths were
measured after cycloplegia using a Zeiss IOLMaster, with reported
data for each eye based on an average of 10 and 3 valid measurements for axial length and anterior chamber depths, respectively.
Corneal curvatures were measured with a Marco keratometer. Near
heterophoria were measured at 33 cm through the subjects
manifest subjective spherocylindrical distance correction in a trial
frame set to their distance pupillary distance using the alternating
cover test method. The minimum amount of binocular plus power,
added in +0.25D steps, required to eliminate eso-fixation disparities, that is, near associated phoria, was similarly measured
while viewing through Polaroid filters, a Bernell Near Point
Examination card in a lighted box at 33 cm at their habitual
reading angle. Near associated esophorias were also measured in
trial contact lens fitting sessions through both SVSCLs and
BFSCLs. In determining the BFSCL prescription, a bifocal add
power one step higher than the previously measured near associated phoria was used as a starting point and the add power
subsequently adjusted to determine the minimum power necessary to completely eliminate or maximally reduce the near associated esophoria while maintaining acceptable distance visual
acuity. Both SVSCL and BFSCL prescriptions were submitted to
the off-site clinical trial coordinator responsible for allocating
treatments.
Statistical Analysis
Although many ocular parameters were monitored during
the treatment period, reported data analyses are limited to
those parameters most likely to offer insight into myopia progression. Two primary outcome measures were used: (1) changes
from baseline in spherical equivalent refractive errors based on
cycloplegic autorefraction measurements and (2) changes in axial
lengthVboth parameters being objective and thus free of subjective biases. Anterior chamber depth, corneal curvature, and near
associated phoria data were also included in some analyses. Initial
comparison of primary outcome data for right and left eyes revealed no significant differences between them, and so the data for
the two eyes of individual subjects were averaged for use in subsequent analyses. Follow-up analyses used to evaluate treatment
effects included unpaired t-tests with Bonferroni correction to
examine differences between the two treatment groups (SVSCLs
vs. BFSCLs) in outcome measures at both 6 and 12 months. To
understand the origin of refractive error changes, correlations
between changes in refractive errors and biometric parameters
were analyzed using Pearson correlations. Finally, multivariate
analyses of variance were used to examine the influence on
treatment outcomes of various factors, including age, sex, baseline
refractive error, near associated phorias, and BFSCL add power.
RESULTS
Subject Profiles
Eighty-six myopic subjects were recruited, comprising an ethnically diverse group, with 27 white, 24 Asian (Chinese, Japanese,
Korean, and Indian), 23 Hispanic, 9 Filipino or Pacific Islander
children, and 3 children of African descent. In total, approximately 300 subjects were screened by telephone to determine their
potential eligibility, with 125 subjects undergoing in-office
screening. Thirty-nine screened subjects (18 male, 21 female)
either failed the screening (N = 33) or qualified but declined to
participate for various reasons (N = 6). Seventy-eight subjects of
the 86 recruited completed all aspects of the study. There were no
significant differences in any of the measured baseline measures
between these two groups. Five subjects were dispensed lenses,
with two completing only the dispensing visit and three completing only the 2-week follow-up visit. The other three subjects
wore contact lenses for 6 months or more, one of whom wore
lenses for 6 months but declined to undergo cycloplegia as part of
Optometry and Vision Science, Vol. 93, No. 4, April 2016
Myopia Control with Bifocal Contact LensesVAller et al.
347
TABLE 1.
Baseline profiles for BFSCL and SVSCL groups (mean T SD)
Treatment group
Age, yr
Refractive error, D
Axial length, mm
Associated phoria, D
BFSCL (N = 39)
SVSCL (N = 40)
13.0 T 2.5
13.5 T 2.2
j2.57 T 1.34
j2.81 T 1.46
24.68 T 0.91
24.63 T 0.68
1.2 T 0.6
1.2 T 0.7
the 6-month follow-up visit and was thus dropped from the study;
of the remaining two subjects, one completed the 6-month visit
but not the 12-month visit and the other completed the 12-month
visit only. The data for both of the latter two subjects were included in the analyses. The subject pool had a distinct female sex
bias (60 of 86 subjects, 70%), which was preserved within each
group; there were 27 females and 11 males in the BFSCL group
and 27 females and 13 males in the SVSCL group. The subjects
ranged in age from 8 to 18 years, their median age being 13.6 years,
with 38 subjects (44%) being 13 years or younger.
Baseline Parameters
Summary statistics for both SVSCL and BFSCL groups are
given in Table 1. The groups were not significantly different from
each other (p 9 0.05, unpaired t-tests in all cases). All subjects fell
into the category of low to moderate myopia, based on cycloplegic
autorefractions, which ranged from j0.25 to j6.00D in the least
myopic meridian, with mean equivalent spherical refractive errors
ranging from j0.75 to j5.82D and astigmatism ranging from
0 to j1.00D. Axial lengths ranged from 22.58 to 26.41 mm, with
anterior chamber depths ranging from 2.21 to 4.33 mm. Corneal
curvatures, averaged across the two principal meridians, ranged
from 41.06 to 47.03D. All subjects exhibited near associated
esophorias, the plus power required to neutralize the latter ranging
from +0.25 to +3.75D. Corresponding near heterophorias ranged
from 8 PD exophoria to 18 PD esophoria, with a mean of 5.5 PD
esophoria.
Treatment Effects
Changes in refractive error and axial length during the study
period are summarized for both treatment groups in Table 2 and
shown graphically in Fig. 1. There were significant changes in
both refractive error and axial lengths from baseline in each group
and at both 6 and 12 months (p G 0.001 in all cases). However,
for both parameters, changes were significantly less for the
BFSCL group than for the SVSCL group at both 6 and 12 months
(p G 0.001), the finding at 6 months implying a rapid onset
of the myopia control effect of the BFSCLs. Note also that at
the 6-month time point, hyperopic shifts in refractive error
were recorded for five subjects in the BFSCL group compared
with one subject in the SVSCL group (Fig. 1, left panel, data
above zero). A slightly larger number of subjects in the
BFSCL group also recorded reductions in axial length (Fig. 1, right
panel). To better illustrate the contrasting effects of the two
treatments, refractive error data were categorized according to
whether or not there was progression during the treatment period.
Using this binary outcome measure, the number of subjects
showing either no progression of myopia or a hyperopic shift in
refractive error represents 26% and 29% of the BFSCL treatment
group at 6 and 12 months, respectively, compared with 5% (two
subjects) for the SVSCL treatment group at both time points.
Also note that only one subject in the BFSCL group progressed by
1D or more during the 12-month study period compared with
11 subjects in the SVSCL group. These figures further reinforce the
significant differences between the two groups in terms of myopia
progression.
During the total 12-month study period, changes in refractive
error were well predicted by changes in axial length (R2 = 0.64,
p G 0.001) but not by changes in anterior chamber depth (R2 =
j0.012; p = 0.79). Indeed, both the BFSCL and SVSCL groups
recorded significant reductions rather than increases in anterior
chamber depth (p G 0.01), presumably reflecting the growth of the
crystalline lens in these young eyes, as the magnitude of the change
was not significantly different between the groups (p = 0.94).
There was no significant change of corneal curvature for either
group during the 12-month treatment period (p = 0.40).
A series of multivariate analyses of variance were also conducted
to identify potentially significant associations. Only the most
TABLE 2.
Baseline data and changes in ocular parameters (mean T SD) for BFSCL and SVSCL groups after 6 and 12 months of lens wear
BFSCL
Ocular parameter
Cycloplegic spherical equivalent
refractive error, D
Axial length, mm
Anterior chamber depth, mm
Corneal curvature, D
SVSCL
Baseline
Time, months
Change
Baseline
Time, months
Change
j2.57 T 1.34
6
12
6
12
6
12
6
12
j0.17 T 0.30*
j0.22 T 0.34*
0.03 T 0.10*
0.05 T 0.14*
j0.20 T 0.43
j0.36 T 0.53
j0.09 T 0.26
j0.06 T 0.24
j2.81 T 1.46
6
12
6
12
6
12
6
12
j0.48 T 0.30
j0.79 T 0.43
0.14 T 0.11
0.24 T 0.17
j0.16 T 0.56
j0.37 T 0.53
j0.04 T 0.22
j0.01 T 0.21
24.68 T 0.91
3.56 T 0.47
43.66 T 1.45
24.63 T 0.68
3.44 T 0.47
43.73 T 1.19
*Significant differences between treatment groups (unpaired t-test, p G 0.001).
Optometry and Vision Science, Vol. 93, No. 4, April 2016
348 Myopia Control with Bifocal Contact LensesVAller et al.
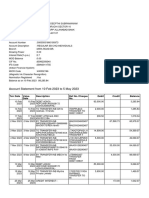
FIGURE 1.
Boxplots with scatterplots overlaid, showing changes in cycloplegic objective spherical equivalent refractive errors and axial lengths after 6 and 12 months
of treatment, split by treatment group (single-vision [SV] or bifocal [BF] soft contact lenses). ***p G 0.001; length of whiskers denotes 1.5 interquartile range.
efficient model, that is, with the least number of variables without
affecting the goodness of fit of the model, is reported, with changes
in axial length and in refractive error as dependent continuous
variables and six independent variables, treatment, sex, age,
baseline refractive error, baseline near associated phoria, and
BFSCL add power. Of these six variables, only age, considered as a
continuous variable, and contact lens treatment proved to be
significantly associated with changes in refractive error and axial
length (Wilks L = 0.579, F2,74 = 26.86, p G 0.0001 for age; and
Wilks L = 0.533, F2,74 = 32.41, p G 0.0001 for contact lens
treatment, respectively).
Our study specifically targeted subjects with near associated
esophorias based on early reports linking near dissociated
esophoria with better myopia control with multifocal spectacle
lenses.31Y33 As expected, the BFSCL group showed a significant
reduction in residual associated esophorias (associated phoria
measured with contact lenses in place) relative to that of the
SVSCL group (j1.10 T 0.52D vs. j0.16 T 0.43D, p G 0.0001).
Nonetheless, neither baseline associated phorias nor residual associated phorias were significantly associated with overall changes
in refractive error (F1,73 = 0.17, p = 0.68; F1,73 = 1.13, p = 0.29 for
baseline near associated phoria and change in near associated
phoria across 12 months, respectively).
DISCUSSION
The CONTROL study described here provides compelling
evidence for the efficacy of bifocal contact lenses as a myopia
control treatment. The strong myopia control effect found in this
study, that is, an overall 72% reduction in progression, based on
cycloplegic autorefraction, and 80% reduction in the rate of axial
elongation, far exceeds the size of treatment effects reported in
previous myopia control studies involving optical devices in
humans,29Y31,39,39Y41 and only daily 1.0% topical atropine has
comparable results of the pharmacological treatments studied.40
Nonetheless, the results are consistent with an already published
identical twin case study by the authors.41 However, the CONTROL study provides more convincing evidence that myopia
progression can be effectively controlled through optical intervention, being a well-controlled, albeit small-scale, doublemasked clinical trial with treatments randomly assigned and
groups well matched with regard to sex, ethnicity, refractive error,
and degree of near associated phoria. As a 12-month study, it is
not possible to comment on the enduring nature of this treatment
effect, although related more recent contact lens studies have
reported significant treatment effects beyond the first year.42,43
Given that many of the sight-threatening ocular complications of
myopia are linked to excessive ocular elongation,5,44 it is also
important to note that the BFSCL control effect reported here was
achieved through reduced ocular elongation.
The large control effects reported here contrast with the
somewhat small effects reported in two COMET studies,45,46
which represent the largest and best-controlled of clinical trials
involving multifocal spectacle lenses for myopia in children to
date. Both COMET studies used progressive addition lenses
(PALs). In the first study, subgroup analyses revealed that subjects
with either low baseline levels of myopia and reduced accommodative responses or near esophoria and larger than normal
lags of accommodation all benefited significantly from PALs,
recording treatment effects of 0.55 and 0.64D less myopia progression, respectively, across 3 years compared with that of singlevision spectacle wearers. The reduction in progression rates with
PALs was 0.20D overall, and for near exophores, 0.05D. Curiously, in a 3-year follow-up study (COMET II), which was
limited to children with high accommodative lags and near
esophoria,46 the treatment effect was very small, averaging 0.28D,
and another shorter study (STAMP),47 which was likewise limited
to children with high accommodative lags, also reported only a
small, 0.18D, treatment effect across 12 months. Additional selection criteria for the latter study included either myopia less than
Optometry and Vision Science, Vol. 93, No. 4, April 2016
Myopia Control with Bifocal Contact LensesVAller et al.
j2.25D or myopia higher than j2.25D combined with
esophoria at near. Although all three studies were United States
based, results from studies involving multifocal spectacles in East
Asia have also not revealed consistent clinically significant myopia
control benefits for those with near esophorias or high lags of
accommodation.48,49
Since the completion of the study reported here, there have
been a number of other myopia controlYrelated bifocal contact
lens studies, and as reported here, most have demonstrated better
efficacy than related multifocal spectacle lens studies. Two such
studies, the DISC study50 and the Dual Focus51 study, involved
two different custom multifocal soft contact lens designs, which
both had distance and near powers arranged in some form of
multiple concentric rings, as with the lens design used in the
current study. Both studies reported significant slowing of
myopia progression in the wearers of their device relative to those
receiving the single-vision control treatment, although less than in
the current study, that is, 36% slower progression in both the
DISC study overall and in the first 10 months of the crossover
Dual Focus study. In the first year of yet another multiyear study
comparing myopia progression with a soft contact lens design with
peripheral plus power and single-vision soft contact lenses, an
adjusted 34% relative reduction was reported.52 Finally, a 1-year
study comparing myopia progression in wearers of a distance
center multifocal soft lens with a +2.00D add with historical
controls involving wearers of single-vision daily disposable soft
contact lenses reported a 50% relative reduction in myopia progression and a 29% relative reduction in axial elongation.53
Why are bifocal soft contact lenses apparently more effective in
controlling myopia progression than bifocal or PAL spectacles?
While the current study was relatively short-term (12 months),
and it is possible that treatment effects may have declined with
time, had our study been extended, the picture is likely more
complex. In this context, the practical limitations of bifocal and
PAL spectacles for children and adolescents and their implications
for compliance cannot be ignored. Once inserted, contact lenses
are more likely to be left in place throughout the day than spectacle
lenses for practical reasons, thereby favoring compliance. Furthermore, assuming that the maximum treatment effects of
multifocal spectacle lenses requires children to use the near addition during near work, then compared with presbyopic adults,
children are likely to be less compliant because of the unusual head
and eye postures required (head up and eyes lowered) and because
of the optical distortions encountered on viewing obliquely
through the lower regions of such spectacle lenses. Indeed, video
monitoring of children participating in one myopia control study
found that they commonly dropped their heads while reading.54
Thus, although most studies report training their subjects in the
proper use of multifocal spectacles and many of them also sought
to monitor compliance, it is not clear how effective these strategies
were in ensuring their proper use in everyday tasks. Furthermore,
with the extensive use by todays children and adolescents of
computers with screens at or above eye level, one could argue that
the more traditional multifocal spectacle lens designs are not
practical for these age groups. Lending weight to these arguments
is the impressive sustained myopia control reported in a study
using high-set executive-style bifocal spectacles with or without
base-in prism for rapidly progressing Chinese Canadian children
349
with high accommodative lags and/or with esophoria at near,55
that is, 39 and 51% slowing in myopia progression and 30 and
34% slowing in axial elongation, respectively, relative to changes
with single-vision spectacles across 3 years. The children are likely
to have had difficulty in looking over the top of the near segments
during reading, and the addition of base-in prism may have improved visual comfort and thus compliance in those with induced
near exophoric tendencies. The bifocal soft contact lenses used in
the current study represent the end of this continuum, exposure to
the near addition having no dependence on gaze direction and/or
training, the only requirement being that the lenses are worn on a
daily basis.
The arguments presented above rest on an assumption that
accommodative lags stimulate eye elongation, that the adds in
bifocal lenses and PALs served to correct them, and that the superiority of bifocal contact lenses reflects the near addition being
available at all angles of gaze and near distances. A number of
studies have attempted to directly measure the effects of bifocal
soft contact lenses on accommodation, with significant differences in their outcomes. In one such study, myopes as well as
emmetropes were reported to overaccommodate when wearing
bifocal soft contact lenses, whereas only emmetropes showed
this behavior for single-vision contact lenses incorporating the
near addition power and only at some distances.56 However,
two other studies have reported near normal accommodation in
nonpresbyopic users of bifocal contact lenses,50,51 suggesting that
they ignored the near zones of the lenses. Although different
methodologies, including instrumentation, were used in these
three studies, nonetheless, taken together, these results suggest that
a simple analogy between bifocal spectacles and bifocal contact
lenses is not appropriate here. Induced changes in net optical
aberrations, including spherical aberration, are likely to also impact on accommodation, greater in the case of bifocal contact
lenses than equivalent spectacle lenses, and these effects are also
likely to be lens design dependent,57,58 a subject of an ongoing
study. The possibility that such changes might contribute to the
apparently greater efficacy of some bifocal contact lens designs
cannot be ruled out.58
It is perhaps important to note that all CONTROL subjects exhibited near associated esophorias, with the bifocal adds
being selected to maximally neutralize them and without which
they could be expected to exhibit larger lags of accommodation as reduced accommodative effort is one way of reducing
accommodative convergence by way of compensating for near
esophorias. Based on animal model studies, the resulting retinal
(hyperopic) defocus can be expected to contribute to myopic
progression and bifocal adds to slow progression by attenuating
such focusing errors. In this context, myopes exhibiting near esofixation disparities may represent a special subset likely to benefit
significantly from near additions. Note also that most other
multifocal lens studies have used standardized additions, with no
selection criteria related to binocular vision status, perhaps contributing to the lower efficacies reported.
Other characteristics of bifocal soft contact lenses may also have
contributed to their apparently greater effectiveness than spectacle
lenses as myopia control treatments. Specifically, the improved
efficacy of bifocal contact lenses over their spectacle lens equivalents may be related to differences in the defocus experience,
Optometry and Vision Science, Vol. 93, No. 4, April 2016
350 Myopia Control with Bifocal Contact LensesVAller et al.
including more sustained myopic defocus provided with the
former. Animal studies have shown that the imposition of
sustained myopic defocus over a sufficiently large area of retina
(central or peripheral) strongly inhibits eye growth.21 The designers of the DISC study have argued that their contact lens
imposes frequent near constant myopic defocus, distributed relatively evenly across the retina, thereby providing a robust stop
signal to eye growth. The bifocal contact lens design used in the
current study included alternating rings of distance and near
powers. Interestingly, Fresnel spectacle lens designs incorporating
rings of positive power have also been shown to have strong inhibitory effects on eye growth in both chick and guinea pig
models.20,21,23The prolate eye shape commonly linked to human
myopia may also be of relevance, as it is generally coupled to
peripheral hyperopic defocus, which will be reduced, or even
reversed in sign, at least during distance viewing, with bifocal
contact lens designs incorporating peripheral adds, as used in the
current study. The myopia control effect of such lenses would also
be improved further if, during near viewing, nonpresbyopic
wearers did not reduce their accommodation, as reported in two of
the studies described above.37,38
The observed decreases in axial length and apparent myopia
regression, mostly limited to the BFSCLs group, warrant some
comment. A similar pattern of response was observed previously
by us in a myopia control case study involving BFSCLs and
identical twins,41 as well as in both an unrelated study involving
orthokeratology59 and the ATOM 1 study.60 In the current study,
13 subjects in the BFSCL group recorded reductions in axial
length, and eight subjects recorded hyperopic shifts in cycloplegic
spherical equivalent refractive error, that is, regression in myopia,
based on the average for the two eyes. These observations contrast
with findings for the SVSCL group, in which only one subject
showed a decrease in axial length and one subject showed a decrease in myopia. Such changes were more commonly encountered in older (13 years and older) subjects, with both cases in the
SVSCL group, as well as 11 of 13 cases of axial shrinkage and 5
of 8 cases of myopia regression in the BFSCL group falling within
this age range. Reductions in accommodative tone across the
treatment period may have contributed to these refractive error
changes, that is, apparent myopia regression, although such effects
are expected to be very small, given that reported refractive error
data were obtained under cycloplegia. Also no treatment-induced
corneal changes were observed to provide an alternative optical
explanation for this finding. Noteworthy and more challenging
to explain are the observed decreases in axial length in some of
our subjects, given that a small amount of eye elongation, not
shrinkage, can be expected among growing children, even in
the absence of myopic progression. Indeed, in a study involving
Nepalese children aged 6 to 18 years, the vitreous chamber depths
of nonmyopic subjects were reported to increase at a rate of
0.07 mm/year.61 Because the average axial length change for the
BFSCL group is very small, that is, 0.05 mm, measurement error
cannot be ruled out as the explanation for some of the cases of
apparent shrinkage. However, choroidal thickening in response to
imposed myopic defocus is offered as one of two alternative explanations of some of these cases. First reported in chicks, defocusdriven choroidal thickening has since been reported in other
animal models13,62,63 and most recently in young adult subjects.64
The effect of choroidal thickening is to move the retina forward,
thereby leading to a reduction of axial length as referenced to the
retinal pigment epithelium and measured with the IOLMaster.
As the second more speculative explanation, it is plausible that
co-contraction of resident myofibroblasts in the human sclera
could lead to a decrease in axial length, although little is known
about the role of these cells and the signal pathway that regulates
their activity.65 Suffice it to say, it remains beyond the scope of this
report to conclusively identify the mechanism underlying the
observed reductions in axial length in otherwise growing children.
No clinical trial is without its limitations. Limiting our subjects
to those having eso fixation disparity at near prevents generalization of our conclusions about the treatment effects found with
BFSCLs. The relatively short duration of our study is also a
limitation. A follow-up longer-term study is needed to address the
question of whether good control over myopia progression is
maintained with BFSCLs beyond 12 months. Future studies
should also aim for a more balanced representation by sex and
include a wider range of ethnicities to cover the possibility of
genetic differences in the evolution of myopia, as proposed by
Yang et al.,49 among others. Finally, it will also be important to
understand how early intervention influences the course of later
progression on discontinuation of treatment.
CONCLUSIONS
Acuvue BFSCLs, prescribed to maximally neutralize near associated esophoria in children and adolescents, are effective
in limiting the rate of myopia progression and axial elongation relative to conventional single-vision contact lenses during a
12-month treatment period. Understanding the specific factors
contributing to the efficacy of this contact lens design in controlling myopia progression will be important for refining related
clinical protocols.
ACKNOWLEDGMENTS
Supported in part by a grant from Vistakon, a Division of Johnson and
Johnson. Solutions were provided by Alcon. The first author has less than 50
shares of stock in Johnson and Johnson, a manufacturer of some of the bifocal
and standard lenses used in the study, purchased in 1983. The first author has
received a patent on the use of bifocal contact lenses for myopia progression
control (U.S. Patent No. 6,752,499 B2; issued June 22, 2004), and he is a
coauthor of several other patents in the area of myopia control.
Results of the study have been previously reported in abstract form at the
International Myopia Conference, Singapore, 2006, and at the American
Academy of Optometry meeting in Denver, Colorado, November 12, 2014.
Received April 5, 2015; accepted November 3, 2015.
REFERENCES
1. Lin LL, Shih YF, Lee YC, Hung PT, Hou PK. Changes in ocular
refraction and its components among medical studentsVa 5-year
longitudinal study. Optom Vis Sci 1996;73:495Y8.
2. Sun J, Zhou J, Zhao P, Lian J, Zhu H, Zhou Y, Sun Y, Wang Y, Zhao
L, Wei Y, Wang L, Cun B, et al. High prevalence of myopia and high
myopia in 5060 Chinese university students in Shanghai. Invest
Ophthalmol Vis Sci 2012;53:7504Y9.
Optometry and Vision Science, Vol. 93, No. 4, April 2016
Myopia Control with Bifocal Contact LensesVAller et al.
3. Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its
association with body stature and educational level in 19-year-old
male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci
2012;53:5579Y83.
4. Vitale S, Ellwein L, Cotch MF, Ferris FL 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999Y2004. Arch
Ophthalmol 2008;126:1111Y9.
5. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012;
31:622Y60.
6. Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H,
Kitazawa Y, Tajimi Study G. Prevalence and causes of low vision
and blindness in a Japanese adult population: the Tajimi Study.
Ophthalmology 2006;113:1354Y62.
7. Wu L, Sun X, Zhou X, Weng C. Causes and 3-year-incidence of
blindness in Jing-An District, Shanghai, China 2001Y2009. BMC
Ophthalmol 2011;11:10.
8. Saw SM, Wu HM, Seet B, Wong TY, Yap E, Chia KS, Stone RA, Lee
L. Academic achievement, close up work parameters, and myopia in
Singapore military conscripts. Br J Ophthalmol 2001;85:855Y60.
9. Mirshahi A, Ponto KA, Hoehn R, Zwiener I, Zeller T, Lackner K,
Beutel ME, Pfeiffer N. Myopia and level of education: results from
the Gutenberg Health Study. Ophthalmology 2014;121:2047Y52.
10. Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P.
Outdoor activity reduces the prevalence of myopia in children.
Ophthalmology 2008;115:1279Y85.
11. Wallman J, Winawer J. Homeostasis of eye growth and the question
of myopia. Neuron 2004;43:447Y68.
12. Wildsoet CF. Active emmetropizationVevidence for its existence
and ramifications for clinical practice. Ophthalmic Physiol Opt
1997;17:279Y90.
13. Wildsoet C, Wallman J. Choroidal and scleral mechanisms of
compensation for spectacle lenses in chicks. Vision Res 1995;35:
1175Y94.
14. Hammond DS, Wallman J, Wildsoet CF. Dynamics of active
emmetropisation in young chicksinfluence of sign and magnitude
of imposed defocus. Ophthalmic Physiol Opt 2013;33:215Y26.
15. Wildsoet C. Neural pathways subserving negative lens-induced
emmetropization in chicksVinsights from selective lesions of the
optic nerve and ciliary nerve. Curr Eye Res 2003;27:371Y85.
16. Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF.
Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci 2005;46:
3965Y72.
17. Smith EL 3rd, Hung LF, Huang J, Blasdel TL, Humbird TL,
Bockhorst KH. Effects of optical defocus on refractive development
in monkeys: evidence for local, regionally selective mechanisms.
Invest Ophthalmol Vis Sci 2010;51:3864Y73.
18. Wallman J, Gottlieb MD, Rajaram V, Fugate-Wentzek LA. Local
retinal regions control local eye growth and myopia. Science 1987;
237:73Y7.
19. Charman WN, Radhakrishnan H. Peripheral refraction and the
development of refractive error: a review. Ophthalmic Physiol Opt
2010;30:321Y38.
20. Liu Y, Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young
chicks. Invest Ophthalmol Vis Sci 2011;52:1078Y86.
21. Liu Y, Wildsoet C. The effective add inherent in 2-zone negative lenses inhibits eye growth in myopic young chicks. Invest Ophthalmol Vis Sci 2012;53:5085Y93.
351
22. Benavente-Perez A, Nour A, Troilo D. Axial eye growth and refractive
error development can be modified by exposing the peripheral retina
to relative myopic or hyperopic defocus. Invest Ophthalmol Vis Sci
2014;55:6765Y73.
23. McFadden SA, Tse DY, Bowrey HE, Leotta AJ, Lam CS, Wildsoet
CF, To CH. Integration of defocus by dual power Fresnel lenses
inhibits myopia in the mammalian eye. Invest Ophthalmol Vis Sci
2014;55:908Y17.
24. Smith EL 3rd. Spectacle lenses and emmetropization: the role of
optical defocus in regulating ocular development. Optom Vis Sci
1998;75:388Y98.
25. Atchison DA, Jones CE, Schmid KL, Pritchard N, Pope JM,
Strugnell WE, Riley RA. Eye shape in emmetropia and myopia.
Invest Ophthalmol Vis Sci 2004;45:3380Y6.
26. Chen C, Cheung SW, Cho P. Myopia control using toric
orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci 2013;
54:6510Y7.
27. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology
research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res 2005;30:71Y80.
28. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, GutierrezOrtega R. Myopia control with orthokeratology contact lenses in
Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci
2012;53:5060Y5.
29. Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia
progression. Br J Ophthalmol 2009;93:1181Y5.
30. Kang P, Swarbrick H. Time course of the effects of orthokeratology
on peripheral refraction and corneal topography. Ophthalmic Physiol
Opt 2013;33:277Y82.
31. Goss DA, Grosvenor T. Rates of childhood myopia progression with
bifocals as a function of nearpoint phoria: consistency of three
studies. Optom Vis Sci 1990;67:637Y40.
32. Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of
single-vision vs. bifocal lenses on myopia progression in children with
esophoria. Optom Vis Sci 2000;77:395Y401.
33. Gwiazda JE, Hyman L, Norton TT, Hussein ME, Marsh-Tootle W,
Manny R, Wang Y, Everett D. Accommodation and related risk
factors associated with myopia progression and their interaction with
treatment in COMET children. Invest Ophthalmol Vis Sci 2004;
45:2143Y51.
34. Aller TA, Wildsoet C. Results of a one-year prospective clinical trial
(CONTROL) of the use of bifocal soft contact lenses to control
myopia progression. Ophthal Physiol Opt 2006;26(Suppl. 1):6.
35. Aller T, Wildsoet C, Liu M. CONTROL: a 12 month, randomized
bifocal soft contact lens trial targeting myopia progression. Optom
Vis Sci 2014;91:E-abstract 140007.
36. Zelen M. Randomized consent designs for clinical trials: an update.
Stat Med 1990;9:645Y56.
37. Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and
Proportions, 3rd ed. J. Wiley: Hoboken, NJ; 2003.
38. ClinicalTrials.gov. Aller TA. Bifocal Soft Contact Lenses and their
Effect on Myopia Progression in Children and Adolescents. Updated
2005. Available at: https://clinicaltrials.gov/ct2/show/NCT00214487?
term=thomas+aller&rank=2. Accessed November 3, 2015.
39. Hasebe S, Ohtsuki H, Nonaka T, Nakatsuka C, Miyata M,
Hamasaki I, Kimura S. Effect of progressive addition lenses on
myopia progression in Japanese children: a prospective, randomized,
double-masked, crossover trial. Invest Ophthalmol Vis Sci 2008;
49:2781Y9.
Optometry and Vision Science, Vol. 93, No. 4, April 2016
352 Myopia Control with Bifocal Contact LensesVAller et al.
40. Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL,
Tan D. Atropine for the treatment of childhood myopia. Ophthalmology 2006;113:2285Y91.
41. Aller TA, Wildsoet C. Bifocal soft contact lenses as a possible myopia
control treatment: a case report involving identical twins. Clin Exp
Optom 2008;91:394Y9.
42. Cho P, Cheung SW. Retardation of Myopia in Orthokeratology
(ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci 2012;53:7077Y85.
43. Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Longterm effect of overnight orthokeratology on axial length elongation
in childhood myopia: a 5-year follow-up study. Invest Ophthalmol
Vis Sci 2012;53:3913Y9.
44. Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt 2005;
25:381Y91.
45. Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D,
Leske MC, Manny R, Marsh-Tootle W, Scheiman M. A randomized
clinical trial of progressive addition lenses versus single vision lenses
on the progression of myopia in children. Invest Ophthalmol Vis Sci
2003;44:1492Y500.
46. Gwiazda J, Chandler DL, Cotter SA, Everett DF, Hyman L,
Kaminski BM, Kulp MT, Lyon DW, Manny RE, Marsh-Tootle
WL, Matta NS, Melia BM, et al. Progressive-addition lenses versus
single-vision lenses for slowing progression of myopia in children with
high accommodative lag and near esophoria. Correction of Myopia
Evaluation Trial (COMET) 2 Study Group for the Pediatric Eye Disease Investigator Group. Invest Ophthalmol Vis Sci 2011;52:2749Y57.
47. Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial
using progressive addition lenses to evaluate theories of myopia
progression in children with a high lag of accommodation. Invest
Ophthalmol Vis Sci 2012;53:640Y9.
48. Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong
progressive lens myopia control study: study design and main
findings. Invest Ophthalmol Vis Sci 2002;43:2852Y8.
49. Yang Z, Lan W, Ge J, Liu W, Chen X, Chen L, Yu M. The effectiveness of progressive addition lenses on the progression of myopia
in Chinese children. Ophthalmic Physiol Opt 2009;29:41Y8.
50. Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in
Hong Kong Chinese schoolchildren: a 2-year randomised clinical
trial. Br J Ophthalmol 2014;98:40Y5.
51. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear
on axial myopia progression in children. Ophthalmology 2011;118:
1152Y61.
52. Sankaridurg P, Holden B, Smith E 3rd, Naduvilath T, Chen X, de la
Jara PL, Martinez A, Kwan J, Ho A, Frick K, Ge J. Decrease in rate
of myopia progression with a contact lens designed to reduce relative
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci
2011;52:9362Y7.
Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal
contact lens myopia control. Optom Vis Sci 2013;90:1207Y14.
Hasebe S, Nakatsuka C, Hamasaki I, Ohtsuki H. Downward deviation
of progressive addition lenses in a myopia control trial. Ophthalmic
Physiol Opt 2005;25:310Y4.
Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and
prismatic bifocal spectacles on myopia progression in children: threeyear results of a randomized clinical trial. JAMA Ophthalmol 2014;
132:258Y64.
Tarrant J, Severson H, Wildsoet CF. Accommodation in emmetropic
and myopic young adults wearing bifocal soft contact lenses. Ophthalmic Physiol Opt 2008;28:62Y72.
Tarrant J, Roorda A, Wildsoet CF. Determining the accommodative
response from wavefront aberrations. J Vis 2010;10:4.
Tarrant J. Spherical Aberration, Accommodation and Myopia.
PhD dissertation. Berkeley, CA: University of California, Berkeley;
2010. Available at: http://digitalassets.lib.berkeley.edu/etd/ucb/text/
Tarrant_berkeley_0028E_10860.pdf. Accessed November 3, 2015.
Swarbrick HA, Alharbi A, Watt K, Lum E, Kang P. Myopia control
during orthokeratology lens wear in children using a novel study
design. Ophthalmology 2015;122:620Y30.
Tong L, Huang XL, Koh AL, Zhang X, Tan DT, Chua WH.
Atropine for the treatment of childhood myopia: effect on myopia
progression after cessation of atropine. Ophthalmology 2009;116:
572Y9.
Garner LF, Stewart AW, Owens H, Kinnear RF, Frith MJ. The
Nepal Longitudinal Study: biometric characteristics of developing
eyes. Optom Vis Sci 2006;83:274Y80.
Troilo D, Nickla DL, Wildsoet CF. Choroidal thickness changes
during altered eye growth and refractive state in a primate. Invest
Ophthalmol Vis Sci 2000;41:1249Y58.
Wallman J, Wildsoet C, Xu A, Gottlieb MD, Nickla DL, Marran L,
Krebs W, Christensen AM. Moving the retina: choroidal modulation
of refractive state. Vision Res 1995;35:37Y50.
Chakraborty R, Read SA, Collins MJ. Hyperopic defocus and diurnal changes in human choroid and axial length. Optom Vis Sci
2013;90:1187Y98.
Poukens V, Glasgow BJ, Demer JL. Nonvascular contractile cells
in sclera and choroid of humans and monkeys. Invest Ophthalmol
Vis Sci 1998;39:1765Y74.
Optometry and Vision Science, Vol. 93, No. 4, April 2016
Thomas A. Aller
711 Kains Ave
San Bruno, CA 94066
e-mail: cptreyes@earthlink.net
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Calculus of Finite Differences: Andreas KlappeneckerDocument30 pagesCalculus of Finite Differences: Andreas KlappeneckerSouvik RoyNo ratings yet
- Lecture No. 11Document15 pagesLecture No. 11Sayeda JabbinNo ratings yet
- Starex Is BTSDocument24 pagesStarex Is BTSKLNo ratings yet
- Dark Energy Survey DES CollaborationDocument38 pagesDark Energy Survey DES CollaborationgeorgcantorNo ratings yet
- Rewriting Snow White As A Powerful WomanDocument6 pagesRewriting Snow White As A Powerful WomanLaura RodriguezNo ratings yet
- Citing Correctly and Avoiding Plagiarism: MLA Format, 7th EditionDocument4 pagesCiting Correctly and Avoiding Plagiarism: MLA Format, 7th EditionDanish muinNo ratings yet
- Pitch AnythingDocument8 pagesPitch AnythingDoland drumb100% (1)
- Dashrath Nandan JAVA (Unit2) NotesDocument18 pagesDashrath Nandan JAVA (Unit2) NotesAbhinandan Singh RanaNo ratings yet
- NST 029Document123 pagesNST 029Riaz Ahmad BhattiNo ratings yet
- L Rexx PDFDocument9 pagesL Rexx PDFborisg3No ratings yet
- Analog Electronics-2 PDFDocument20 pagesAnalog Electronics-2 PDFAbhinav JangraNo ratings yet
- American J of Comm Psychol - 2023 - Palmer - Looted Artifacts and Museums Perpetuation of Imperialism and RacismDocument9 pagesAmerican J of Comm Psychol - 2023 - Palmer - Looted Artifacts and Museums Perpetuation of Imperialism and RacismeyeohneeduhNo ratings yet
- SAP Environment, Health, and Safety (EHS)Document13 pagesSAP Environment, Health, and Safety (EHS)SAFETY VOFPLNo ratings yet
- Project ProposalDocument2 pagesProject Proposalqueen malik80% (5)
- Sunrise - 12 AB-unlockedDocument81 pagesSunrise - 12 AB-unlockedMohamed Thanoon50% (2)
- Debate Lesson PlanDocument3 pagesDebate Lesson Planapi-280689729No ratings yet
- Feb-May SBI StatementDocument2 pagesFeb-May SBI StatementAshutosh PandeyNo ratings yet
- Development of PBAT Based Bio Filler Masterbatch: A Scientific Research Proposal OnDocument15 pagesDevelopment of PBAT Based Bio Filler Masterbatch: A Scientific Research Proposal OnManmathNo ratings yet
- Ce Project 1Document7 pagesCe Project 1emmaNo ratings yet
- CBLM - Interpreting Technical DrawingDocument18 pagesCBLM - Interpreting Technical DrawingGlenn F. Salandanan89% (45)
- All Siae Skus: SF Product Name SIAE Product Code Descrip:on Availability Product Family Unit LIST Price ($)Document7 pagesAll Siae Skus: SF Product Name SIAE Product Code Descrip:on Availability Product Family Unit LIST Price ($)Emerson Mayon SanchezNo ratings yet
- B205A TMA Project Spring 2021 - UpdatedDocument6 pagesB205A TMA Project Spring 2021 - UpdatedIoan 23No ratings yet
- Approximate AnalysisDocument35 pagesApproximate AnalysisSyahir HamidonNo ratings yet
- Ugtt April May 2019 NewDocument48 pagesUgtt April May 2019 NewSuhas SNo ratings yet
- Ems Speed Sensor Com MotorDocument24 pagesEms Speed Sensor Com MotorKarina RickenNo ratings yet
- CSCI 123 - Final ExamDocument15 pagesCSCI 123 - Final ExamBrianYoungNo ratings yet
- AM-FM Reception TipsDocument3 pagesAM-FM Reception TipsKrishna Ghimire100% (1)
- Investigation of The Microstructures, Properties, and Toughening Mechanism of Polypropylene/calcium Carbonate Toughening Masterbatch CompositesDocument16 pagesInvestigation of The Microstructures, Properties, and Toughening Mechanism of Polypropylene/calcium Carbonate Toughening Masterbatch CompositesHatchi KouNo ratings yet
- Comsol - Guidelines For Modeling Rotating Machines in 3DDocument30 pagesComsol - Guidelines For Modeling Rotating Machines in 3DtiberiupazaraNo ratings yet
- Ojt Evaluation Forms (Supervised Industry Training) SampleDocument5 pagesOjt Evaluation Forms (Supervised Industry Training) SampleJayJay Jimenez100% (3)