Professional Documents
Culture Documents
Br. J. Anaesth.-2013-Desmet-445-52
Uploaded by
Siva SankarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Br. J. Anaesth.-2013-Desmet-445-52
Uploaded by
Siva SankarCopyright:
Available Formats
British Journal of Anaesthesia 111 (3): 44552 (2013)
Advance Access publication 15 April 2013 . doi:10.1093/bja/aet109
PAIN
I.V. and perineural dexamethasone are equivalent
in increasing the analgesic duration of a single-shot
interscalene block with ropivacaine for shoulder surgery:
a prospective, randomized, placebo-controlled study
M. Desmet1*, H. Braems 2, M. Reynvoet 1, S. Plasschaert 1, J. Van Cauwelaert3, H. Pottel 4, S. Carlier1,
C. Missant 2 and M. Van de Velde2
1
Department of Anesthesiology, AZ Groeninge, Loofstraat 43, 8500 Kortrijk, Belgium
Department of Anesthesiology, University Leuven, University Hospitals Gasthuisberg, Herestraat 49, 3000 Leuven, Belgium
3
Department of Orthopedic Surgery, AZ Groeninge, Burg. Vercruysselaan 5, 8500 Kortrijk, Belgium
4
Interdisciplinary Research Center Catholic University Leuven, Campus Kortrijk, Etienne Sabbelaan 53, 8500 Kortrijk, Belgium
2
Editors key points
Regional analgesia can
be effective in improving
postoperative pain
control after shoulder
surgery.
Background. Interscalene brachial plexus block (ISB) provides excellent, but time-limited
analgesia. Dexamethasone added to local anaesthetics prolongs the duration of a singleshot ISB. However, systemic glucocorticoids also improve postoperative analgesia.
The hypothesis was tested that perineural and i.v. dexamethasone would have an
equivalent effect on prolonging analgesic duration of an ISB.
Perineural
dexamethasone can
prolong the duration of
analgesia, although not
specifically licensed for
this use.
Methods. We performed a prospective, double blind, randomized, placebo-controlled study.
Patients presenting for arthroscopic shoulder surgery with an ISB were randomized into
three groups: ropivacaine 0.5% (R); ropivacaine 0.5% and dexamethasone 10 mg (RD);
and ropivacaine 0.5% with i.v. dexamethasone 10 mg (RDiv). The primary outcome was
the duration of analgesia, defined as the time between performance of the block and
the first analgesic request. Standard hypothesis tests (t-test, MannWhitney U-test) were
used to compare treatment groups. The primary outcome was analysed by KaplanMeier
survival analysis with a log-rank test and Coxs proportional hazards regression.
This study compares
effects of perineural or i.v.
dexamethasone on the
duration of ropivacaine
analgesia.
Results. One hundred and fifty patients were included after obtaining ethical committee
approval and patient informed consent. The median time of a sensory block was equivalent
for perineural and i.v. dexamethasone: 1405 min (IQR 10151710) and 1275 min (IQR 1095
2035) for RD and RDiv, respectively. There was a significant difference between the
ropivacaine group: 757 min (IQR 635910) and the dexamethasone groups (P,0.0001).
Route of dexamethasone
administration did not
impact on improved
duration for interscalene
brachial plexus block
(ISB).
Conclusions. I.V. dexamethasone is equivalent to perineural dexamethasone in prolonging the
analgesic duration of a single-shot ISB with ropivacaine. As dexamethasone is not licensed for
perineural use, clinicians should consider i.v. administration of dexamethasone to achieve an
increased duration of ISB.
Keywords: anaesthetic techniques, i.v. regional; anaesthetic techniques, regional, brachial
plexus; anaesthetics local, ropivacaine; analgesia, postoperative; analgesics antiinflammatory, steroid
Accepted for publication: 24 January 2013
Shoulder surgery can be very painful surgery after which the
use of opioids is often required. The well-known side-effects
of opioids (e.g. respiratory depression, somnolence, nausea,
vomiting, and pruritus) limit their use in so called fast
track surgery and anaesthesia programmes. ISB provides excellent analgesia minimizing the side-effects of opioids and
is widely accepted as the gold standard in the management
of acute pain after shoulder surgery.1
Although a single-shot ISB is useful for pain relief in the
early postoperative period, it is often insufficient as postoperative pain can persist for several days. For patients requiring analgesia for .24 h, a continuous ISB (CISB) can be
& The Author [2013]. Published by Oxford University Press on behalf of the British Journal of Anaesthesia. All rights reserved.
For Permissions, please email: journals.permissions@oup.com
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
* Corresponding author. E-mail: matthias.desmet@azgroeninge.be
BJA
Methods
The trial was registered on clinicaltrials.be (#B396201110645).
The AZ Groeninge Institutional Review board approved all
aspects of the trial (#11 009, 16/02/2011, Chairman Dr
L. Van Lysebeth). The Federal Agency of Medicines and
Health Products has been informed regarding the study protocol with the off-label use of dexamethasone. It did not
request an Investigational New Drug approval. Written
informed consent was obtained from all patients. All patients
planned for arthroscopic shoulder surgery (rotator cuff repair
and shoulder decompressions) were eligible for inclusion in
the study. Exclusion criteria were: age ,18 yr, brachial
plexus neuropathies, severe bronchopulmonary disease, coagulopathies, systemic glucocorticoid use, pregnancy, routine
use of opioid medications, intolerance for one or more medications of the study protocol and diabetes. All the patients
were operated by the same surgeon (J.V.C.) and the ISB was
performed by experienced staff anaesthesists, with at least
10 yr experience with interscalene blocks.
Using a computer generated random number table,
patients were randomized in three-treatment groups: ropivacaine 0.5% (Group R), ropivacaine 0.5% and perineural
446
dexamethasone 10 mg (Group RD), and ropivacaine 0.5%
with i.v. dexamethasone 10 mg (Group RDiv). Sealed
opaque envelopes with the study group allocation were
opened before the blocks were performed. Medication was
prepared by a staff member who was not involved in the
study and delivered in unidentifiable syringes.
Patients were premedicated with lorazepam 2.5 mg p.o.
1 h before the surgical procedure, monitored with electrocardiography, pulse oximetry and non-invasive arterial pressure,
and sedated with i.v. midazolam (2 mg) and sufentanil
(2.5 mg).
After skin disinfection and infiltration with lidocaine 1%,
the interscalene brachial plexus was identified using a short
bevel 50 mm, 22 gauge stimulating needle (Stimuplex A;
B. Braun Melsungen AG, Germany) connected to a Stimuplex
(Stimuplex-HNS II A; B. Braun Melsungen AG, Germany)
nerve stimulator. The initial setting was a current of 0.8 mA
with a stimulating frequency of 2 Hz. The direction of the
needle was similar as in the modified lateral approach of
Borgeat and Ekatodramis10 was applied in all patients. Contractions of the biceps, triceps, or any muscle contraction of
the hand or forearm with a current of 0.30.5 mA indicated
correct placement of the needle. A 2 ml solution containing
normal saline for Groups R and RDiv and 10 mg dexamethasone for Group RD was administered perineurally. Then,
without repositioning the needle, all patients received 30 ml
ropivacaine 0.5%. At the time of the ISB, a 2 ml solution containing normal saline for Groups R and RD and dexamethasone 10 mg for Group RDiv was administered i.v. Thus, all
patients received an ISB with 30 ml of ropivacaine 0.5%
with an i.v. and perineural solution of 2 ml containing the
study drugs according to randomization.
All brachial plexus injections were administered slowly
with repeated aspiration to prevent or detect early intravascular injection.
General anaesthesia was induced and maintained using
propofol (target controlled infusion 35 mg ml21), remifentanil (loading dose 1 mg kg21, continuous infusion 0.05 0.3 mg
kg21 min21), and cisatracurium (0.15 mg kg21). Patients were
intubated and ventilated with an oxygen/air admixture.
Maintenance of anaesthesia was left to the discretion of
the attending anaesthesiologist. Intraoperatively, no other
analgesics were administered. At the beginning of the procedure finger stick blood glucose was measured.
On arrival in the recovery room pain was evaluated using a
4-point verbal rating score (VRS) (1no pain, 2mild pain,
3moderate pain, and 4severe pain). Paracetamol i.v.
(1 g) was administered for VRS2 or on patient request.
In case of insufficient analgesia, diclofenac i.v. (50 mg)
was administered. Rescue analgesia with piritramide i.m.
(15 20 mg) was administered if necessary. Piritramide is a
synthetic opioid with relatively fast onset after i.m. administration (15 20 min) with the duration of action of 46 h.
It has a relative potency of 0.7 compared with morphine.11
A motor block was evaluated using a 3-point motor
block score (MBS) (1unable to move fingers, 2able to
move fingers but weaker than the non-operated arm, and
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
used. The placement of a CISB is more invasive and complex
than a single-shot ISB and requires an extensive postoperative follow-up. As there is a trend towards shorter hospital admissions after arthroscopic shoulder surgery, CISB
has been promoted in the ambulatory setting.2 However,
the practical problems of the postoperative follow-up limit
the use of CISB in an outpatient setting.
The use of additives to local anaesthetics can prolong the
duration of a single-shot ISB which can be useful when a
CISB is not possible. Various additives such as vasoconstrictors, clonidine, ketamine, and steroids have been studied,
but most of them failed to prolong the duration of peripheral
nerve blocks.3 5
I.V. dexamethasone attenuates the postoperative need
for analgesics in different clinical settings (orofacial,
general, urological, and orthopaedic surgery).6 In a study
with paediatric patients receiving a caudal block for orchidopexy, i.v. dexamethasone decreased postoperative pain and
analgesia requirements.7 Dexamethasone also prolongs peripheral nerve block when added to short-acting local anaesthetics.8 Cummings and colleagues9 observed a 1.9-fold and
1.5-fold increase in the duration of ISB when dexamethasone
was added to ropivacaine and bupivacaine, respectively.
Whether the main mechanism of action of glucocorticoids
is a systemic anti-inflammatory effect or a local effect on
peripheral nerves remains unknown.
We hypothesized that dexamethasone prolongs analgesia
after a single-shot ISB regardless of the route of administration. We, therefore, conducted a prospective, double blind,
randomized, placebo-controlled study to evaluate the effect
of i.v., and perineural dexamethasone on the duration of a
single-shot ISB with ropivacaine 0.5% for postoperative analgesia after shoulder surgery.
Desmet et al.
BJA
The effect of dexamethasone on interscalene block
Sample size considerations
At the time of our study, no studies were published concerning the effect of dexamethasone on interscalene plexus
blocks with ropivacaine. Based on our experience with ropivacaine 0.5%, we assumed a block duration of 720 min with a
standard deviation (SD) of 500 min. A difference of 360 min
between the treatment and the control group was considered clinically relevant and a sample size (power90% and
a0.05) of 42 patients per group was calculated (twosample t-test). To correct for failed blocks and patient drop
out, 50 patients per group were included in the study.
Statistical analysis
The primary endpoint was the length of the sensory block
defined as the time between the performance of the block
and the first administration of analgesia. Secondary outcomes were pain scores, MBSs, analgesic need, sleep disturbance, and overall satisfaction as measures for patient
comfort. Finally, pre- and postoperative blood glucose measures were analysed and compared between groups. Descriptive statistics are used to present baseline characteristics for
the three groups. Standard hypothesis tests (t-test, Mann
Whitney U-test) were used to compare these baseline
values between treatment groups. Continuous variables
were assessed for normality and are presented as mean
(SD) or median with interquartile range (IQR) as appropriate.
Categorical variables were assessed using frequency tables
and x 2 or Fishers exact test. The interval between the
onset of the sensory block and the initial use of analgesia
was analysed by KaplanMeier survival analysis with a
log-rank test and Coxs proportional hazards regression to
estimate likelihood ratios adjusted for covariates. The
primary analysis is the comparison between survival curves.
All other statistical tests are secondary and performed at
the 5% significance level, without correction for multiple
testing, and should be interpreted accordingly.
All statistical analyses were performed with SAS 9.3 (SAS
Institute, Cary, NC, USA).
Results
From March to December 2011, 234 patients presented for
arthroscopic shoulder surgery, 84 were ineligible because of
exclusion criteria or refusal to participate, and 150 patients
were enrolled in the study. Six patients had no primary
or secondary outcome result because of inadherence to
the protocol. These patients were not included in the
intention-to-treat (ITT) analysis. Figure 1 presents the allocation process according to the Consolidated Standards of
Reporting Trials (CONSORT) statement.
A total of 144 patients were included for the ITT analysis
(Group R n46, Group RD n49, Group RD iv n49). Five
patients, evenly distributed over the three study groups
(Group R n2, Group RD n1, Group RD iv n2) were
deemed to have failed blocks, but were analysed in their
assigned groups according to ITT principles. These patients
were given the outcome at the time of recovery. Eleven
patients did not require analgesics during the first 48 h
after operation (no primary outcome). These patients were
also evenly distributed over the three study groups (Group
R n2, Group RD n4, Group RDiv n5, respectively) and
were censored in the survival analysis. The mean age of
the study population was 52 (14) yr, the mean body mass
index (BMI) was 27.2 (4.4), and 45% were men. There were
significantly more cuff repairs in men than in women (78.9
vs 59.5%, P0.002) but the different procedures were
equally distributed in the three groups (Table 1).
Dexamethasone significantly prolonged the duration of
analgesia, independent of the mode of administration. In
Group R, the primary endpoint of the study was reached
after a median of 757 min with an IQR of 635 2910 min,
for Groups RD and RDiv this was 1405 (1015 1710) and
1275 (1095 2035), respectively. Kruskal Wallis followed by
the correction for multiple testing showed statistically significant differences between Groups R and RD (P,0.0001),
Groups R and RDiv (P,0.0001), but not between Groups RD
and RDiv. KaplanMeier curves for the first analgesic
request with patients not receiving any analgesics after 48
h censored to the right are presented in Figure 2. Significant
differences between these curves (log-rank test) were
obtained between Group R and the combined groups RD
and RDiv (P,0.0001), but not between Groups RD and RDiv
(P0.6254).
A Cox proportional hazards model for time to first analgesic was performed using the following variables: study
group, sex, age, and type of surgery. Patients included in
Group R had a 3.91 times (95% CI 2.635.81) higher probability for analgesic need during the first 48 h compared
with patients in Groups RD and RDiv (P,0.0001). None of
the other variables differed significantly.
447
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
3equal strength in both hands). If patients had a pain score
3 and a MBS of 3 on arrival in the recovery room the ISB
was qualified as failed.
Recovery room discharge criteria were stable vital parameters, absence of nausea and vomiting, and a VRS,2.
VRS, MBS, and blood glucose concentrations were assessed
upon recovery room discharge.
The morning after surgery, all patients were reassessed for
pain, motor block, and overall satisfaction. The timing and
dosage of analgesics was recorded and also the quality of
sleep (1no sleep disturbance because of pain, 2sleep disturbance because of pain). Patients were contacted by telephone on Day 2 after surgery to evaluate the same
parameters. Patient satisfaction concerning the procedure
was assessed using a 2-point scale (1satisfied, I would
want the same anaesthesia/analgesia method for the next
surgery, 2unsatisfied, I would want a different anaesthesia/analgesia method for the next surgery). Specific reasons
for dissatisfaction were noted. A telephone assessment
34 months after surgery was performed to detect late
complications. All postoperative scoring was performed by
an independent, blinded investigator.
BJA
Desmet et al.
234 patients
assessed for eligibility
Primary exclusion:
Exclusion criteria: 72
Refusal by patient: 12
150 patients randomized
Group RD
n = 50
Group R
n = 50
Exclusion:
inadherence to
protocol: 4
Group RDiv
n = 50
Exclusion:
inadherence to
protocol: 1
Exclusion:
inadherence to
protocol: 1
Analysed:
49
Analysed:
49
Fig 1 Allocation process according to CONSORT.
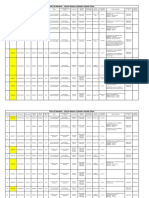
Table 1 Patient and procedure characteristics
Group R
(n546)
Group RD
(n549)
Group RDiv
(n549)
Sex M/F (n)
21/25
21/28
23/26
Mean age (SD)
51.1 (14.3)
53.0 (13.9)
51.6 (14.0)
Mean BMI (SD)
26.7 (4.2)
27.6 (4.7)
27.2 (4.5)
Procedure type:
decompression/
repair (n)
15/31
17/32
14/35
Failed blocks (n)
When pain scores were dichotomized in VRS scores 1 and
2 (no to mild pain) vs VRS scores 3 and 4 (moderate to severe
pain), there was a significant difference between groups after
24 and 48 h (P,0.0001) (Figs 3 and 4).
There was a statistically significant difference in analgesic
use in the three groups. We only present the data for paracetamol and diclofenac as only seven patients needed
opioids. Of note is that five of these patients had blocks
that were qualified as failed. The mean paracetamol use (in
gram) in Group R was 3.8 compared with 2.6 in Group RD
and 2.3 in Group RDiv during the first 48 h (P,0.0001). The
mean diclofenac use after 48 h was also significantly different: 101 mg for Group R compared with 59 and 56 mg for
Group RD and RDiv (P0.03).
There was no significant difference in MBS in the three
groups on admission in the post anaesthesia care unit, and
at 24 and 48 h.
448
During the first night, there was a significant higher proportion of patients with sleep disturbance because of pain
in Group R (59%) compared with Group RD (29%) and
Group RDiv (22%) (P0.0004). Overall satisfaction for the
three groups was excellent: 85 98% of the patients would
like a similar anaesthesia and analgesia protocol for future
shoulder surgery (Table 2).
There was an increase of mean postoperative blood
glucose concentrations in both groups receiving dexamethasone with a mean increase of 3.8 (1.2) mg dl21 for Group RD
(P0.026) and 5.1 (13) mg dl21 (P0.0095) for Group RDiv.
There were no differences in the incidence of hoarseness,
dyspnoea, or Horners syndrome after operation.
Patients were contacted 26 months after surgery. There
was one patient in Group RD who complained of hypoaesthesia in the deltoid region 4 months after surgery. However,
neurological and radiological examination revealed spinal
disc herniation at the level of C4 5 with a disc-radicular conflict. One patient in Group R had a superficial wound infection
requiring no further therapy but local incision and drainage.
Discussion
The present study demonstrates that dexamethasone effectively prolongs the duration of ropivacaine ISB analgesia.
There is, on average, a 1.8-fold increase in the duration of
analgesia when dexamethasone is used as an adjunct to
ropivacaine 0.5%. This is concordant with other results in
the literature.8 9 12 13 Interestingly, this effect is independent
of the route of administration as both perineural and i.v.
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
Analysed:
46
BJA
The effect of dexamethasone on interscalene block
Proportion of patients NOT requesting
analgesia
1.0
0.9
0.8
Group R
Group RDiv
Group RD
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
500
1000
1500
2000
Time to first analgesic request (min)
2500
3000
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
Fig 2 Kaplan Meier survival plot.
100
90
Percentage of patients
80
70
60
VRS <2
50
VRS >2
40
30
20
10
0
Group R
Group RD
Group RDiv
Fig 3 Maximal VRS scores at 24 h after operation (*P,0.05; NS).
administration of dexamethasone produced similar results.
Not only the analgesia duration but also the quality of analgesia indicated by outcome measures such as sleep disturbance and postoperative analgesic use were favourably
influenced by dexamethasone.
Acute postoperative pain has different components (e.g.
nociceptive, inflammatory, and neuropathic because of
direct nerve injury) all of them possible targets for
postoperative analgesic strategies. The precise mechanism
of action of dexamethasone added to local anaesthetics is
unknown. Some studies described a direct effect of glucocorticoids on nerve conduction while others reported that dexamethasone induced perineural vasoconstriction with
concomitant slower absorption of the administered local
anaesthetics.14 15 However, such effects of dexamethasone
do not explain the results of our study as the systemic
449
BJA
Desmet et al.
100
90
Percentage of patients
80
70
60
*
50
40
VRS <2
VRS >2
30
20
Group RD
Group R
Group RDiv
Fig 4 Maximal VRS scores at 48 h after operation (*P,0.05; NS).
Table 2 Secondary outcome parameters
Group R
(n546)
Group
RD
(n549)
Group
RDiv
(n549)
P-value
Mean paracetamol
use (g) at 48 h
3.8
2.6
2.3
,0.0001
Mean diclofenac
use (mg) at 48 h
101
59
56
0.03
Patients with
residual motor
block at 24 h (n)
1/46
5/49
3/49
NS
Sleep disturbance
at 24 h (n)
27/46
14/49
11/49
0.004
Percentage of
patients satisfied
84
92
94
NS
Incidence of
Horner syndrome
(%)
45
48
41
NS
Incidence of
hoarseness (%)
30
23
23
NS
Incidence of
dyspnoea (%)
NS
administration of dexamethasone was equally effective. This
interesting observation is in accordance with the work
of Yilmaz and colleagues16, who could not detect an
effect of dexamethasone on the compound action potential
of A- and C-fibres in isolated sciatic rat nerves. As a direct
effect of dexamethasone on the nerve is unlikely, the anti-
450
inflammatory properties of dexamethasone are probably
responsible for prolonged analgesia after ISB. After intracellular uptake, glucocorticoids will activate cytoplasmatic
glucocorticoid receptors which will bind to glucocorticoid response elements in the DNA. This leads to both a decreased
production of inflammatory proteins [COX-2, iNOS, cytoplasmatic PLA2, interleukins (ILs), inflammatory chemokines,
etc.], and an increased production of anti-inflammatory proteins [lipocortin-1 (IL-1) receptor antagonist].17
To our knowledge, there are no pharmacokinetic data on
the absorption of perineurally administered dexamethasone.
Because absorption in the systemic circulation and gene
transcription is time consuming, one could argue that clinically relevant anti-inflammatory effects of steroids, would
come too late after perineural administration with shortacting local anaesthetics. However, Movafegh and colleagues8 demonstrated that dexamethasone also prolongs the
duration of an axillary block when added to lidocaine (242
vs 98 min). This proves that perineural dexamethasone has
a clinical effect within 2 h of administration. Therefore, we
should aim further research towards the ideal dose and
timing of dexamethasone administration.
We acknowledge that our study has some limitations.
First, we did not assess the duration of the sensory block
in our patients using repeated neurological examinations.
As most patients were treated in an ambulatory setting, it
was impossible to perform such an assessment of the
sensory block. We, therefore, decided to use the duration
until first analgesic request as a marker of the sensory
block. With our study protocol, we were unable to discriminate if the prolonged analgesia was associated with a
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
10
BJA
The effect of dexamethasone on interscalene block
diminish the protective effects of the surrounding vasculature and fibrous tissues and is unable to study the effect
on distal axons.18 Neurone isolation techniques commonly
used to study detrimental effects of drugs may not fully
appreciate the mechanisms of neural injury after peripheral
nerve blocks. In clinical practice, neurological damage is
the result of multiple factors where there is a complex interplay between neurotoxicity of administered drugs, puncture
technique and possible pre-existing neural injury.23
Regarding the inconclusive data on the safety of perineural dexamethasone, we would like to remind clinicians
that this off-label use needs approval of the appropriate
regulatory health institutions. Fortunately, with the results
of our trial the debate on the perineural administration of
dexamethasone may become obsolete.
In conclusion, this study demonstrates that perineural or
i.v. dexamethasone in a dose of 10 mg prolongs significantly
the duration of effective postoperative analgesia resulting
from a single-shot ISB with ropivacaine 0.5%. We, therefore,
propose that i.v. dexamethasone should be considered for
routine use in patients having regional analgesia for the
postoperative pain management.
Declaration of interest
None declared.
References
1 Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia
for shoulder surgery: a critical appraisal and review of current
techniques. Anaesthesia 2010; 65: 60824
2 Fredrickson MJ, Ball CM, Dalgleish AJ. Successful continuous interscalene analgesia for ambulatory shoulder surgery in a private
practice setting. Reg Anesth Pain Med 2008; 33: 122 8
3 Culebras X, Van Gessel E, Hoffmeyer P, Gamulin Z. Clonidine
combined with a long acting local anesthetic does not prolong
postoperative analgesia after brachial plexus block but
does induce hemodynamic changes. Anesth Analg 2001; 92:
199 204
4 Lee IO, Kim WK, Kong MH, et al. No enhancement of sensory and
motor blockade by ketamine added to ropivacaine interscalene
brachial plexus blockade. Acta Anaesthesiol Scand 2002; 46:
821 6
5 Sinnott CJ, Cogswell LP III, Johnson A, Strichartz GR. On the
mechanism by which epinephrine potentiates lidocaines peripheral nerve block. Anesthesiology. 2003; 98: 181 8
6 De Oliveira GS, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative
pain: a meta-analysis of randomized controlled trials. Anesthesiology 2011; 115: 575 88
7 Hong JY, Han SW, Kim WO, Kim EJ, Kil HK. Effect of dexamethasone in combination with caudal analgesia on postoperative
pain control in day-case paediatric orchiopexy. Br J Anaesth
2010; 105: 506 10
8 Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus
blockade. Anesth Analg 2006; 102: 2637
9 Cummings KC III, Napierkowski DE, Parra-Sanchez I, et al. Effect of
dexamethasone on the duration of interscalene nerve blocks with
ropivacaine or bupivacaine. Br J Anaesth 2011; 107: 446 53
451
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
prolongation of the sensory block. Although a point deserving further study, it is irrelevant for daily practice. Indeed,
for patients, pain is the most important parameter to
define satisfaction after surgery.
Secondly, we did not use ultrasound (US) to perform ISB.
At the time of the study, we considered our experience
with US-guided locoregional anaesthesia insufficient to use
a US-based technique. The success rate of our blocks was
97%, which is similar to that reported in the literature.18
We assume that our study results would not have been
different with the use of US.19
Thirdly, analgesics were only administered on request and
a postoperative regimen with regular analgesic administration might have impacted our secondary outcomes. Such a
regimen is often not easy to implement in an ambulatory
setting. We think that our study better represents routine
clinical practice where patient adherence to pain protocols
can be surprisingly low. The overall opioid use in our
study groups was very low. In contrast, all patients with
failed blocks needed opioids in addition to paracetamol
and diclofenac for postoperative analgesia indicating severe
postoperative pain emphasizing the efficiency of interscalene
blocks in this setting.
Fourthly, there are safety concerns regarding the perineural use of dexamethasone. In the absence of human clinical trials, we can only rely on laboratory research. Williams
and colleagues20 studied the effect of ropivacaine and different adjuvants on isolated sensory neurone cell bodies of rats.
In contrast to ropivacaine, dexamethasone did not increase
cell death after 24 h exposure. There was no increased
neurone cell death after 2 h exposure to low-dose dexamethasone and ropivacaine compared with ropivacaine
alone. Ma and colleagues21 reported on the protective
effect of dexamethasone on bupivacaine-induced neurone
injury in rats through a threonine-serine protein kinase
B-dependent mechanism. When the electrophysiological,
behavioural and histological effects of topical dexamethasone on sciatic nerve in rats was studied, it was discovered
that although dexamethasone temporarily attenuated conduction, it had no significant long term effects.14
More than 250 patients received perineural dexamethasone as an adjunct to local anaesthetics in clinical trials.
None of the clinical trials reported an increased incidence
of serious adverse effects compared with the control
groups but all were underpowered to detect an increase in
the incidence of serious adverse effect.8 10 12 It is clear
that with an incidence of 0.4%, 16 000 patients are needed
to reliably detect a doubling of adverse effects.9 So far no
safety trial on the use of perineural dexamethasone has
been performed and it is highly unlikely that such a trial
will ever be conducted. However, local, perineural steroid injection has been used for many years in the treatment of
carpal tunnel syndrome and is acknowledged to be an effective and safe therapy.22 We should also caution to extrapolate
in vitro and in vivo observations with regard to the possible
neurotoxicity of dexamethasone. The isolation technique of
neural cell bodies will inherently lead to neural damage,
BJA
17 Barnes PJ. Anti-inflammatory actions of glucocorticoids: molecular mechanisms. Clin Sci 1998; 94: 55772
18 Davis JJ, Swenson JD, Greis PE, Burks RT, Tashjian RZ. Interscalene
block for postoperative analgesia using only ultrasound guidance:
the outcome in 200 patients. J Clin Anesth 2009; 21: 2727
19 Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance
improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med 2008; 33: 253 8
20 Williams BA, Hough KA, Tsui BYK, et al. Neurotoxicity of adjuvants
used in perineural anesthesia and analgesia in comparison with
ropivacaine. Reg Anesth Pain Med 2011; 36: 22530
21 Ma R, Wang X, Lu C, et al. Dexamethasone attenuated
bupivacaine-induced neuron injury in vitro through a threonineserine protein kinase B-dependent mechanism. Neuroscience
2010; 167: 329 42
22 Marshall SC, Tardif G, Ashworth NL. Local corticosteroid injection
for carpal tunnel syndrome. Cochrane Database Syst Rev 2007;
18: CD001554
23 Barrington MJ, Snyder GL. Neurologic complications of regional
anesthesia. Curr Opin Anaesthesiol 2011; 24: 554 60
Handling editor: L. Colvin
452
Downloaded from http://bja.oxfordjournals.org/ at JIPMER on April 18, 2014
10 Borgeat A, Ekatodramis G. Anaesthesia for shoulder surgery.
Best Pract Res Clin Anaesthesiol 2002; 16: 211 225
11 Kumar N, Rowbotham DJ. Piritramide. Br J Anaesth 1999; 82: 3 5
12 Tandoc MN, Fan L, Kolesnikov S, Kruglov A, Nader ND. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene
block: a prospective randomized trial. J Anesth 2011; 25: 7049
13 Parrington SJ, ODonnell D, Chan VWS, et al. Dexamethasone
added to mepivacaine prolongs the duration of analgesia after
supraclavicular brachial plexus blockade. Reg Anesth Pain Med
2010; 35: 422 6
14 Wang PH, Tsai CL, Lee JS, Wu KC, Cheng KI, Jou IM. Effects of
topical corticosteroids on the sciatic nerve: an experimental
study to adduce the safety in treating carpal tunnel syndrome.
J Hand Surg Eur Vol 2011; 36: 236 43
15 Shishido H, Kikuchi S, Heckman H, Myers RR. Dexamethasone
decreases blood flow in normal nerves and dorsal root ganglia.
Spine 2002; 27: 581 6
16 Yilmaz-Rastoder E, Gold MS, Hough KA, Gebhart GF, Williams BA.
Effect of Adjuvant Drugs on the Action of Local Anesthetics in
Isolated Rat Sciatic Nerves. Reg Anesth Pain Med 2012; 37: 403 9
Desmet et al.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Bank StatementDocument3 pagesBank Statementsaravanan_sfp100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Forensic Science From The Crime Scene To The Crime Lab 2nd Edition Richard Saferstein Test BankDocument36 pagesForensic Science From The Crime Scene To The Crime Lab 2nd Edition Richard Saferstein Test Bankhilaryazariaqtoec4100% (25)
- TOGAF 9 Foundation Part 1 Exam Preparation GuideDocument114 pagesTOGAF 9 Foundation Part 1 Exam Preparation GuideRodrigo Maia100% (3)
- Pub - Essentials of Nuclear Medicine Imaging 5th Edition PDFDocument584 pagesPub - Essentials of Nuclear Medicine Imaging 5th Edition PDFNick Lariccia100% (1)
- Co MonitoringDocument9 pagesCo MonitoringSiva SankarNo ratings yet
- CamScanner Docs Scanned QuicklyDocument3 pagesCamScanner Docs Scanned QuicklySiva SankarNo ratings yet
- Indian Bank ChallanDocument1 pageIndian Bank ChallanSiva SankarNo ratings yet
- Perioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureDocument3 pagesPerioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureSiva SankarNo ratings yet
- My Garden Class 1Document20 pagesMy Garden Class 1Siva SankarNo ratings yet
- Sedation and Anesthesia in GI Endoscopy 2008Document12 pagesSedation and Anesthesia in GI Endoscopy 2008Siva SankarNo ratings yet
- Elsevier Opinion Piece Nov2017Document3 pagesElsevier Opinion Piece Nov2017Jilani ShaikNo ratings yet
- ARDSDocument7 pagesARDSSiva SankarNo ratings yet
- Transfer Professional LicenseDocument8 pagesTransfer Professional LicenseSiva SankarNo ratings yet
- Guidelines For PhysiciansDocument38 pagesGuidelines For PhysiciansSiva SankarNo ratings yet
- An Unusual Cause of Fat Embolism Syndrome.36Document3 pagesAn Unusual Cause of Fat Embolism Syndrome.36Siva SankarNo ratings yet
- DNB Final BS Revised 2016Document68 pagesDNB Final BS Revised 2016Kaustubh LanjeNo ratings yet
- H, C Radiolabeled Compounds and Their Applications in Metabolism StudyDocument5 pagesH, C Radiolabeled Compounds and Their Applications in Metabolism StudySiva SankarNo ratings yet
- Ultrasound Guided Regional Nerve BlocksDocument32 pagesUltrasound Guided Regional Nerve BlocksSiva SankarNo ratings yet
- Tranexa Topical IVDocument5 pagesTranexa Topical IVSiva SankarNo ratings yet
- Obesity 2Document12 pagesObesity 2Siva SankarNo ratings yet
- Uterine Dehiscence During Initiation of Spinal.1Document2 pagesUterine Dehiscence During Initiation of Spinal.1Siva SankarNo ratings yet
- Br. J. Anaesth.-2010-Hong-506-10Document5 pagesBr. J. Anaesth.-2010-Hong-506-10Siva SankarNo ratings yet
- Fox - Appendix R-Cox-regressionDocument18 pagesFox - Appendix R-Cox-regressionlinadiazbejarNo ratings yet
- Statistics - Paediatric SurgeryDocument9 pagesStatistics - Paediatric SurgerySiva SankarNo ratings yet
- AllotemntResultMedical PDFDocument170 pagesAllotemntResultMedical PDFShoyeb KhanNo ratings yet
- SR-JR Leave FormDocument5 pagesSR-JR Leave FormSiva SankarNo ratings yet
- Statistics - Paediatric SurgeryDocument9 pagesStatistics - Paediatric SurgerySiva SankarNo ratings yet
- Ot 1 &2 Total Time Jan 2014Document6 pagesOt 1 &2 Total Time Jan 2014Siva SankarNo ratings yet
- OT1&2time-ASA, Surgery Stat FormDocument1 pageOT1&2time-ASA, Surgery Stat FormSiva SankarNo ratings yet
- Polytrauma Patient Death from Sepsis ComplicationsDocument3 pagesPolytrauma Patient Death from Sepsis ComplicationsSiva SankarNo ratings yet
- Case of Adverse Cardiac EventDocument17 pagesCase of Adverse Cardiac EventSiva SankarNo ratings yet
- Log Book JuneDocument10 pagesLog Book JuneSiva SankarNo ratings yet
- Requesting A Query in Zemanta Using PHPDocument10 pagesRequesting A Query in Zemanta Using PHPAther SajjadNo ratings yet
- Family Service and Progress Record: Daughter SeptemberDocument29 pagesFamily Service and Progress Record: Daughter SeptemberKathleen Kae Carmona TanNo ratings yet
- JurnalDocument9 pagesJurnalClarisa Noveria Erika PutriNo ratings yet
- 20 Ua412s en 2.0 V1.16 EagDocument122 pages20 Ua412s en 2.0 V1.16 Eagxie samNo ratings yet
- Rohit Patil Black BookDocument19 pagesRohit Patil Black BookNaresh KhutikarNo ratings yet
- Jfif 1.02Document9 pagesJfif 1.02Berry Hoekstra100% (1)
- Insider Threat ManagementDocument48 pagesInsider Threat ManagementPatricia LehmanNo ratings yet
- Chem 102 Week 5Document65 pagesChem 102 Week 5CAILA CACHERONo ratings yet
- Lecture Ready 01 With Keys and TapescriptsDocument157 pagesLecture Ready 01 With Keys and TapescriptsBảo Châu VươngNo ratings yet
- Table of Specification for Pig Farming SkillsDocument7 pagesTable of Specification for Pig Farming SkillsYeng YengNo ratings yet
- Petty Cash Vouchers:: Accountability Accounted ForDocument3 pagesPetty Cash Vouchers:: Accountability Accounted ForCrizhae OconNo ratings yet
- AsiaSat 7 at 105Document14 pagesAsiaSat 7 at 105rahman200387No ratings yet
- Thin Film Deposition TechniquesDocument20 pagesThin Film Deposition TechniquesShayan Ahmad Khattak, BS Physics Student, UoPNo ratings yet
- Built - in BeamsDocument23 pagesBuilt - in BeamsMalingha SamuelNo ratings yet
- Three-D Failure Criteria Based on Hoek-BrownDocument5 pagesThree-D Failure Criteria Based on Hoek-BrownLuis Alonso SANo ratings yet
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniNo ratings yet
- House Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Document4 pagesHouse Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Raphael Eyitayor TyNo ratings yet
- John Titor TIME MACHINEDocument21 pagesJohn Titor TIME MACHINEKevin Carey100% (1)
- Biagioli Did Galileo Copy The TelescopeDocument28 pagesBiagioli Did Galileo Copy The TelescopeGregory HooNo ratings yet
- Sri S T Kalairaj, Chairman: Income Tax TaxesDocument3 pagesSri S T Kalairaj, Chairman: Income Tax TaxesvikramkkNo ratings yet
- DELcraFT Works CleanEra ProjectDocument31 pagesDELcraFT Works CleanEra Projectenrico_britaiNo ratings yet
- HenyaDocument6 pagesHenyaKunnithi Sameunjai100% (1)
- If V2 would/wouldn't V1Document2 pagesIf V2 would/wouldn't V1Honey ThinNo ratings yet
- Inventory Control Review of LiteratureDocument8 pagesInventory Control Review of Literatureaehupavkg100% (1)
- 3 - Performance Measurement of Mining Equipments by Utilizing OEEDocument8 pages3 - Performance Measurement of Mining Equipments by Utilizing OEEGonzalo GarciaNo ratings yet
- Sanhs Ipcrf TemplateDocument20 pagesSanhs Ipcrf TemplateStephen GimoteaNo ratings yet
- System: Boehringer Mannheim/Hitachi AnalysisDocument20 pagesSystem: Boehringer Mannheim/Hitachi Analysismaran.suguNo ratings yet