Professional Documents
Culture Documents
Your Scenarios Here Are Examples of The Three Types of Fluid Volume Deficit
Uploaded by
yabaeve0 ratings0% found this document useful (0 votes)
87 views2 pagesdonnnnnnn
Original Title
Your Scenarios Here Are Examples of the Three Types of Fluid Volume Deficit
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdonnnnnnn
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
87 views2 pagesYour Scenarios Here Are Examples of The Three Types of Fluid Volume Deficit
Uploaded by
yabaevedonnnnnnn
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
your scenarios here are examples of the three types of fluid volume deficit
(dehydration) that occur. this is fluid and electrolyte theory, to be sure. i happen
to have a very nice table that breaks all the information down on these three
types of dehydration and it's kind of hard to post the information, but i'll try.
this information is coming from page 477 of intravenous therapy: clinical
principles and practice, by judy terry, leslie baranowski, rose anne lonsway and
carolyn hedrick, published by the intravenous nurses society, 1995.
isotonic fluid volume deficit
type of loss: solute and water loss proportional, no change in plasma volume,
serum sodium level is decreased to 125-150 meq/l. the cause of the fluid loss is
gi fluid loss, urine loss and decreased oral intake.
clinical signs: poor skin turgor; cold, dry dusky skin; sunken eyes; dry
mucous membranes; depressed fontanelles in babies; rapid pulse; low b/p;
irritability or lethargy
fluid replacement guidelines: initially, a bolus of 0.9% sodium chloride or
ringer's lactate is given followed by 5% dextrose in water and 0.45% sodium
chloride. half of the deficit should be replaced in the first 8 hours and the
remaining half over the next 16 hours
hypotonic fluid volume deficit
type of loss: more solute is lost than water. plasma volume moves from the ecf
to the icf. serum sodium levels are decreased below 125 meq/l. the cause of the
fluid loss is often a gi fluid loss with hypotonic oral intake.
clinical signs: include very poor skin turgor; cold, clammy, dusky skin; sunken
eyes; slightly dry mucous membranes; depressed fontanelles in babies; rapid
pulse; very low blood pressure; lethargy; coma; seizures
fluid replacement guidelines: initially a bolus of 0.9% sodium chloride or
ringer's lactate followed by 5% dextrose in water and 0.9% sodium chloride. if
the patient is severely symptomatic 3% sodium chloride at 4ml/kg should be
given over 10 minutes with close monitoring. half of the fluid deficit should be
replaced in the first 8 hours and the remaining half over the next 16 hours.
hypertonic fluid volume deficit
type of loss: there is greater water loss than solute loss. volume moves from
the icf to the ecf. sodium levels are maintained at over 150 meq/l. the cause is
gi fluid loss with hypertonic oral intake, diabetes insipidus, fever and
hyperventilation.
clinical signs: include fair skin turgor; cold, thick and doughy skin; sunken
eyes; parched mouth; depressed fontanelles in babies; a moderately rapid
pulse; moderately low blood pressure; hyperirritability; high-pitched crying in
babies; seizures.
fluid replacement guidelines: 5% dextrose in water and 0.225% or 0.45%
sodium chloride. if the patient is hypertensive 0.9% sodium chloride or ringer's
lactate should be given at a rate of 20ml/kg over one hour. fluid replacement
should be given slow and gradual over 48 hours. 2 to 3 meq/kg of potassium
should be given per 24 hours. at least 2 meq/l/hour of sodium should also be
included in the iv fluids that are used.
You might also like
- Pediatrics in Review. Dehydration 2015Document14 pagesPediatrics in Review. Dehydration 2015Jorge Eduardo Espinoza Rios100% (2)
- Electrolyte DisordersDocument10 pagesElectrolyte DisordersSlavicaNo ratings yet
- Medical Surgical Fluid and Electrolytes FVD FVEDocument7 pagesMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadNo ratings yet
- FLUID AND ELECTOLYTE IMBALANCE FinalDocument27 pagesFLUID AND ELECTOLYTE IMBALANCE FinalShiva BiradarNo ratings yet
- Dehydration Isonatremic, Hyponatremic, andDocument15 pagesDehydration Isonatremic, Hyponatremic, andalfredoibcNo ratings yet
- Environmental Science SyllabusDocument4 pagesEnvironmental Science Syllabusyabaeve100% (5)
- Fluid and Electrolyte BalanceDocument5 pagesFluid and Electrolyte BalanceBumi Zulheri HermanNo ratings yet
- NUR108 2014 Student (1) .PPTX 1Document129 pagesNUR108 2014 Student (1) .PPTX 1LLLJJJ100% (1)
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDocument17 pagesFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.No ratings yet
- New Fluid and Electrolytes Therapy Toyinoriginali2againDocument55 pagesNew Fluid and Electrolytes Therapy Toyinoriginali2againt.baby100% (1)
- LESSON PLAN BronchitisDocument3 pagesLESSON PLAN BronchitisDiana Laura Lei100% (1)
- Ewing's SarcomaDocument16 pagesEwing's SarcomaChacha Zakiya100% (1)
- Generalized Anxiety Disorder Screener GAD7Document2 pagesGeneralized Anxiety Disorder Screener GAD7Indira Damar PangestuNo ratings yet
- Blood Bank ManualDocument29 pagesBlood Bank ManualMarice Ferrufino SchmidtNo ratings yet
- Clinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateDocument12 pagesClinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateNedelcu MirunaNo ratings yet
- Fluid GuidelinesDocument8 pagesFluid GuidelinesAya SalahNo ratings yet
- Club Election ScriptDocument2 pagesClub Election ScriptyabaeveNo ratings yet
- Vulvar Lesions: CAPT Mike Hughey, MC, USNRDocument31 pagesVulvar Lesions: CAPT Mike Hughey, MC, USNRlalalala50% (2)
- Carpal Tunnel SyndromeDocument2 pagesCarpal Tunnel Syndromeurkevet100% (1)
- Earthquake and Fire DrillDocument51 pagesEarthquake and Fire Drillyabaeve100% (1)
- Fluid Calculation For Iv InfusionDocument8 pagesFluid Calculation For Iv InfusionAsma SaleemNo ratings yet
- Fluid Management For The Pediatric Surgical Patient POWERPOINTDocument34 pagesFluid Management For The Pediatric Surgical Patient POWERPOINTDipta Anggara100% (2)
- DeshidratacionpedDocument6 pagesDeshidratacionpedKaren Alejandra RiveraNo ratings yet
- DeshidratacionDocument14 pagesDeshidratacionAlvaro Andres Flores JimenezNo ratings yet
- Iv Fluids Insertion by Josephat John & Fidelis StephanoDocument40 pagesIv Fluids Insertion by Josephat John & Fidelis StephanoAmani Twaha MsemakweliNo ratings yet
- Dehydration: Paul R. EarlDocument31 pagesDehydration: Paul R. EarlJaya Prabha100% (1)
- Pedia Alhamdollilah FluidsDocument80 pagesPedia Alhamdollilah FluidsArwyn AncogNo ratings yet
- Dehydration: Paul R. EarlDocument26 pagesDehydration: Paul R. EarlAndreeaHumaNo ratings yet
- Alteration in Fluid and Electrolyte Status Lecture NotesDocument11 pagesAlteration in Fluid and Electrolyte Status Lecture Notes0912247251No ratings yet
- Case Study On DehydrationDocument4 pagesCase Study On DehydrationDustin Dela CruzNo ratings yet
- Aged Care Brochure PDFDocument12 pagesAged Care Brochure PDFMuhammad ZubaidiNo ratings yet
- Extracellular Fluid Volum DeficitDocument22 pagesExtracellular Fluid Volum DeficitKhushi Devgan SharmaNo ratings yet
- DehydrationDocument16 pagesDehydrationBenben LookitandI'mNo ratings yet
- Simulation Lab 20 Instructions With AnswersDocument5 pagesSimulation Lab 20 Instructions With AnswersChristine Mccombs100% (3)
- Fluids and ElectrolyteDocument25 pagesFluids and Electrolytehammadkhan7126No ratings yet
- DehydrationDocument27 pagesDehydrationDivika ShilvanaNo ratings yet
- A Brief Guide & Summation Jackie Weisbein, D.O. Westchester General Hospital Miami, FloridaDocument35 pagesA Brief Guide & Summation Jackie Weisbein, D.O. Westchester General Hospital Miami, FloridaSalil MahajanNo ratings yet
- Dehydration Causes of Dehydration in Children: Salmonella CampylobacterDocument4 pagesDehydration Causes of Dehydration in Children: Salmonella CampylobacterNdor BariboloNo ratings yet
- Kidney Failure Kelompok 3Document14 pagesKidney Failure Kelompok 3Devi FitrianaNo ratings yet
- Clinical Assessment and Diagnosis of HypovolemiaDocument10 pagesClinical Assessment and Diagnosis of HypovolemiaCristobal Andres Fernandez CoentraoNo ratings yet
- Fluid Volume Deficit Nursing ManagementDocument5 pagesFluid Volume Deficit Nursing ManagementA.No ratings yet
- Etiology, Clinical Manifestations, and Diagnosis of Volume Depletion in Adults - UpToDateDocument17 pagesEtiology, Clinical Manifestations, and Diagnosis of Volume Depletion in Adults - UpToDateAlessandro De FredeNo ratings yet
- Fluid and Electrolyte 10 RDocument87 pagesFluid and Electrolyte 10 RHea YaNo ratings yet
- DEHIDRASIDocument7 pagesDEHIDRASISyaqiq balkhy AlwanyNo ratings yet
- Nutrition Noteworthy, 4 (1) Garcia, Marcela EsperanzaDocument7 pagesNutrition Noteworthy, 4 (1) Garcia, Marcela EsperanzadidikekoNo ratings yet
- Guidance For Intravenous Fluid and Electrolyte Prescription in AdultsDocument8 pagesGuidance For Intravenous Fluid and Electrolyte Prescription in AdultsfrakturhepatikaNo ratings yet
- Peds Fluid and ElectrolytesDocument12 pagesPeds Fluid and ElectrolytesAshleyNo ratings yet
- Fluid and Electrolytes ImbalanceDocument49 pagesFluid and Electrolytes ImbalanceMohamed Na3eemNo ratings yet
- Dehydration in Children - Pediatrics - MSD Manual Professional EditionDocument5 pagesDehydration in Children - Pediatrics - MSD Manual Professional EditionA.No ratings yet
- Dehydration Types Causes Symptoms and TreatmentDocument5 pagesDehydration Types Causes Symptoms and TreatmentmournamourNo ratings yet
- Dehydration PaedDocument28 pagesDehydration Paednkamiabam2No ratings yet
- A Fluids and ElectrolytesDocument8 pagesA Fluids and ElectrolytesAnastasiafynnNo ratings yet
- Fluid TherapyDocument5 pagesFluid TherapyPrabina SahuNo ratings yet
- Module 9 Fluid and Electrolyte Management Hevinkumar PatelDocument5 pagesModule 9 Fluid and Electrolyte Management Hevinkumar PatelhevinpatelNo ratings yet
- Fluid and Electrolyte Balance: Daily RequirementsDocument7 pagesFluid and Electrolyte Balance: Daily RequirementsChristian JaraNo ratings yet
- Referat Ayu - MilaDocument24 pagesReferat Ayu - MilaMiladiyah AlrosyadNo ratings yet
- Hary-Fluid Management Part 1Document49 pagesHary-Fluid Management Part 1Keta PatelNo ratings yet
- g2 9321 Alteration in Fluids ElectrolytesDocument88 pagesg2 9321 Alteration in Fluids ElectrolytesKRIZIELL KATE ALIGANNo ratings yet
- Diabetic Ketoacidosis (DKA) : BackgroundDocument9 pagesDiabetic Ketoacidosis (DKA) : Backgroundalyssa_flores_3No ratings yet
- Perioperative Fluid Management in ChildrenDocument31 pagesPerioperative Fluid Management in ChildrenRashmi SahaNo ratings yet
- Intravenous Fluids: Composition & UsesDocument41 pagesIntravenous Fluids: Composition & UsesFathima BanuzNo ratings yet
- DehydrationDocument19 pagesDehydrationIlyes FerenczNo ratings yet
- 05 Diarrhea in Children SMS 5 021110Document10 pages05 Diarrhea in Children SMS 5 021110AnastasiafynnNo ratings yet
- DehydrationDocument23 pagesDehydrationazharzharmehmoodmNo ratings yet
- Principles+ +LU6Document35 pagesPrinciples+ +LU6Alvin Ray JuanNo ratings yet
- Gastro Ent It IsDocument9 pagesGastro Ent It IsAbed ElharazinNo ratings yet
- Fluid and Electrolytes ManagmentDocument13 pagesFluid and Electrolytes ManagmentSunardiasih100% (1)
- Fluid ManagementDocument10 pagesFluid ManagementdradaadNo ratings yet
- SOCIETY Culture With Family PlanningDocument1 pageSOCIETY Culture With Family PlanningyabaeveNo ratings yet
- DEPED UNICEF Disaster Risk Reduction Resource ManualDocument94 pagesDEPED UNICEF Disaster Risk Reduction Resource ManualNicolai AquinoNo ratings yet
- Heat Capacity FormulaDocument6 pagesHeat Capacity FormulayabaeveNo ratings yet
- The Four Priorities For ActionDocument2 pagesThe Four Priorities For ActionyabaeveNo ratings yet
- HttpsDocument4 pagesHttpsyabaeveNo ratings yet
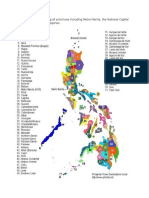
- Philippine Map Indicating All Provinces Including Metro Manila, The National Capital Region (NCR) of The PhilippinesDocument1 pagePhilippine Map Indicating All Provinces Including Metro Manila, The National Capital Region (NCR) of The PhilippinesyabaeveNo ratings yet
- Disaster Readiness and Risk Reduction HandoutsDocument4 pagesDisaster Readiness and Risk Reduction HandoutsyabaeveNo ratings yet
- Answer SheetsDocument1 pageAnswer SheetsyabaeveNo ratings yet
- IDRN 1300 Spear v5 20120110Document6 pagesIDRN 1300 Spear v5 20120110yabaeveNo ratings yet
- E213 Bleeding Control Shock ManagementDocument1 pageE213 Bleeding Control Shock ManagementyabaeveNo ratings yet
- Anatomy SyllabusDocument7 pagesAnatomy SyllabusyabaeveNo ratings yet
- How To Remove System Volume Info in Usb DriveDocument1 pageHow To Remove System Volume Info in Usb DriveyabaeveNo ratings yet
- I2Document9 pagesI2yabaeveNo ratings yet
- Biology Finals 1bDocument1 pageBiology Finals 1byabaeveNo ratings yet
- Weather and Climate ChangeDocument6 pagesWeather and Climate ChangeyabaeveNo ratings yet
- General ScienceDocument147 pagesGeneral ScienceyabaeveNo ratings yet
- Community First Aid and Emergency Extrication Training Course SyllabusDocument1 pageCommunity First Aid and Emergency Extrication Training Course SyllabusyabaeveNo ratings yet
- Food Production and DistributionDocument9 pagesFood Production and DistributionyabaeveNo ratings yet
- DocDocument8 pagesDocyabaeveNo ratings yet
- Lesson 1Document5 pagesLesson 1yabaeveNo ratings yet
- Guide On Childhood Immunization 2014Document1 pageGuide On Childhood Immunization 2014yabaeveNo ratings yet
- Computer Safety Do and No ListDocument18 pagesComputer Safety Do and No ListyabaeveNo ratings yet
- BayabanDear SirDocument1 pageBayabanDear SirEduard Espeso Chiong-Gandul Jr.No ratings yet
- Geological SyllabusDocument3 pagesGeological SyllabusyabaeveNo ratings yet
- China Is A Socialist Country. The Government Owns and Controls Almost All Natural ResourcesDocument6 pagesChina Is A Socialist Country. The Government Owns and Controls Almost All Natural ResourcesyabaeveNo ratings yet
- Geological Science Final Examination: 1. Stages of Thunder Storm 10-12 (Plate Boundaries)Document1 pageGeological Science Final Examination: 1. Stages of Thunder Storm 10-12 (Plate Boundaries)yabaeveNo ratings yet
- Daftar Pustaka: Universitas Sumatera UtaraDocument3 pagesDaftar Pustaka: Universitas Sumatera UtaradestyannisaNo ratings yet
- CD Part 2 - Communicable Diseases With Pics (1) ConDocument239 pagesCD Part 2 - Communicable Diseases With Pics (1) ConMackoi SalamanesNo ratings yet
- Occupational Health and Safety Including PadamsDocument27 pagesOccupational Health and Safety Including PadamsFerlyn SanorjoNo ratings yet
- Proposal 300Document15 pagesProposal 300Atul A SharanNo ratings yet
- Care Plan Prep May 13 Rheumatic FeverDocument16 pagesCare Plan Prep May 13 Rheumatic Feverapi-256360167No ratings yet
- Cornea and External DiseaseDocument26 pagesCornea and External Diseaserajeshwari saravananNo ratings yet
- 139-Article Text-416-1-10-20180204Document3 pages139-Article Text-416-1-10-20180204Kriti KumariNo ratings yet
- Eating DisordersDocument15 pagesEating DisordersJana Marie CorpuzNo ratings yet
- Application of Derivatives in The Field of MedicineDocument1 pageApplication of Derivatives in The Field of MedicineSolaimanNo ratings yet
- Ophtalmology Record Corneal Ulcer: Anggi Lewis R P Aruan 1161050113Document7 pagesOphtalmology Record Corneal Ulcer: Anggi Lewis R P Aruan 1161050113LewishoppusNo ratings yet
- Abstract Apicon Category Section Title Author Name Author Name and Contact NumberDocument6 pagesAbstract Apicon Category Section Title Author Name Author Name and Contact NumberKriti KumariNo ratings yet
- Adji Suranto. Khasiat Dan Manfaat Madu Herbal (Jakarta: Agromedia Pustaka, 2004)Document2 pagesAdji Suranto. Khasiat Dan Manfaat Madu Herbal (Jakarta: Agromedia Pustaka, 2004)Dania Shafa AlmasaNo ratings yet
- Morbidity and Mortality Conference Er Census JUNE 2019Document9 pagesMorbidity and Mortality Conference Er Census JUNE 2019AnneCanapiNo ratings yet
- Environmental Science and Engineering: Case Study #7: Covid-19 Name: Manglo, John Andrae BDocument1 pageEnvironmental Science and Engineering: Case Study #7: Covid-19 Name: Manglo, John Andrae BJohn Andrae MangloNo ratings yet
- President Rodrigo DuterteDocument1 pagePresident Rodrigo DuterteBea Garcia AspuriaNo ratings yet
- Communicable Disease ReviewDocument7 pagesCommunicable Disease Reviewjudith dela cruzNo ratings yet
- Lupus: PrintDocument24 pagesLupus: Printmelodia gandezaNo ratings yet
- Unknown PDFDocument56 pagesUnknown PDFMuhammad AdiNo ratings yet
- This Is Known As Student DiversityDocument3 pagesThis Is Known As Student DiversityAngela Marie Hilario PacursaNo ratings yet
- Diagnosa 0523Document36 pagesDiagnosa 0523RSUD BESUKINo ratings yet
- Good Shepherd Hospital (Swaziland) TB Infection Control Policy Dec 2014Document30 pagesGood Shepherd Hospital (Swaziland) TB Infection Control Policy Dec 2014COMDIS-HSDNo ratings yet
- Lec 1 Gangrene: C. Upper Extremities Are More Commonly Involved Than Lower ExtremitiesDocument13 pagesLec 1 Gangrene: C. Upper Extremities Are More Commonly Involved Than Lower ExtremitiesarbazNo ratings yet
- Anemia in CKDDocument36 pagesAnemia in CKDmaymawziNo ratings yet
- Virtual Watcher's Class: Covid-19 N-E-W-S: Everything You Need To "Navigate" Through The New NormalDocument27 pagesVirtual Watcher's Class: Covid-19 N-E-W-S: Everything You Need To "Navigate" Through The New NormalValerie FischerNo ratings yet