Professional Documents
Culture Documents
Chronic Hyperplastic
Uploaded by
rerez0 ratings0% found this document useful (0 votes)
100 views3 pagesBPH
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBPH
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
100 views3 pagesChronic Hyperplastic
Uploaded by
rerezBPH
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Chronic Hyperplastic
Candidiasis of the Oral
Mucosa: Case Report
Case Report
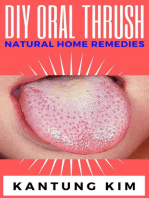
A 50 year-old man made his first visit to the CEU-Cardenal Herrera Dentistry
Clinic. The reason of the visit was to carry out a checkup and mouth cleaning
seeing as it had been 3 years since his last visit to the dentist. The patient
was smoker of 10 cigarettes perday, without other systemic diseases. We
observed a painless, well demarcated whitish plaque that did not detach
upon rasping, located on the cheek mucosa, and on both lip retrocommissures (Figure 1) the patient did not know how long he had had those
lesions. The clinical features of the white lesions could be diagnosed as
Chronic Hyperplastic Candidiasis (CHC). Therefore, differential diagnosis of all
the white lesions that could not be removed should be made as leukoplakia.
We counseled the patient about quitting smoking. To establish a definitive
diagnosis we made a biopsy with local anesthesia (Figure 2) and a
complementary microbiological culture.
The biopsy of the lesions is usually obtained and was stained with
hematoxylin-eosin, the results showed pseudoepitheliomatous oral mucosa
with very marked hyperkeratosis without dysplasia and superficial
candidiasis associated with stromal inflammation psedoliquenoide pattern.
The biopsy of the lesions is usually obtained and was stained with
hematoxylin-eosin, the results showed pseudoepitheliomatous
oral mucosa with very marked hyperkeratosis without dysplasia and
superficial candidiasis associated with stromal inflammation psedoliquenoide
pattern.
The result of the microbiological culture was a growth of Candida albicans
colonies (Figure 3) we treated the lesions with miconazole gel 3 times a day
for 2 months. The control made after two months revealed an improvement
in the lesions (Figure 4) and total remission was observed after 6 months.
Material and Methods
Swab samples were taken from the oral mucosa. The samples were spread in
the Sabouraud dextrose agar medium and the CHROMagar Candida
(Becton Dickinson, Germany) medium and were incubated at 37C during
48h. The results were observed after 24 and 48 hours. Sabouraud dextrose
agar (Becton Dickinson, Germany) is the medium most commonly used for
the isolation of Candida spp. And other yeasts with clinical origin [24].
CHROMagar Candida (Becton Dickinson, Germany) is a selective and
differential culture medium that facilitates the isolation and presumptive
identification of some clinically relevant species such as C. albicans, C.
krusei, C. tropicalis and C. glabrata. This medium allows the specific
identification of C. albicans colonies due to their green color; C. tropicalis
colonies appear blue with a pink halo around them; C. krusei colonies are
pink with a soft appearance and C. glabrata present a brown color [25,26].
Once the primary isolation of the yeast was made, fast methods such as the
filamentation test in serum were applied to find C. albicans. Furthermore,
nutrient assimilation methods were used to corroborate the identification
(API 20 C AUX, bioMrieux, France).
Results and Discussion
The clinical diagnosis was of hyperplastic candidiasis and was established
using a biopsy from the lesion and the detection of Candida in the
microbiological culture. Chronic Hyperplastic Candidiasis (CHC) is a variant of
oral candidiasis that typically appears as well-demarcated palpable, raised
lesions that may vary from small translucent whitish areas to large opaque
plaques that cannot be rubbed off. The most common site for these lesions is
the buccal mucosa, especially the commissures areas [20]. The palate and
tongue may also be involved, although less frequently. The major etiologic
agent of the disease is the oral fungal pathogen Candida predominantly
belonging to Candida albicans, although other systemic co-factors, such as
vitamin deficiency and generalized immune suppression, may play a
contributory role. In this case, the patient had not taken antibiotics or
steroids for an extended period of time. However, these are factors that are
more commonly related to other types of oral candidiasis such as the acute
erythematous candidiasis. In our case, the patient presented tobacco and
deficient oral hygiene as risk factors. These risk factors are related with
chronic hyperplastic candidiasis. The smoking habit has a direct link to CHC,
due to: induction of increased epithelial keratinization; reduction in salivary
immunoglobulin A levels; and possible depression of polymorphonuclear
leukocyte function [20]. Clinically, the lesions are symptomless and regress
after appropriate antifungal therapy and correction of underlying nutritional
or other deficiencies. The regression of a significant proportion of CHC
lesions as a result of antifungal therapy is an indication that hyperplasia is a
protective response of the host mucosa against a disseminated infection by
Candida [20]. If the lesions are untreated, a minor proportion may
demonstrate dysplasia and
develop into carcinomas. In this case, the clinical improvement of the lesions
was observed after two months of treatment with miconazole and total
remission was observed after 6 months. Histopathological examination of a
suspected lesion is essential for the diagnosis of CHC [20]. Because this form
may mimic other lesions, particularly squamous cell carcinoma, a biopsy is
highly recommended. Histopathological examination will reveal epithelial
parakeratosis with polymorphonuclear leukocytes in the superficial layers. In
our case, the diagnosis was carried out with a biopsy and a microbiological
culture. This case was interesting for us because it is a type of candidiasis
has a low prevalence if it is compared to other clinical types such as pseudo
membranous or erythematous candidiasis. Moreover, its importance also lies
in the fact that an exhaustive clinical monitoring must be conducted seeing
as it has a risk of malignancy. Furthermore, this case is important because, in
order to conduct the differential diagnosis of hyperplastic candidiasis, it is
necessary to carry out a biopsy to discard other leukoplakia.
Conclusion
The diagnosis of CHC is complicated seeing as its characteristics are similar
to those of a leukoplakia infected with Candida. For this reason, it is the key
to carry out a differential diagnosis using a biopsy and a microbiological
culture. The total remission of the lesion after antifungal treatment confirms
the diagnosis of CHC.
You might also like
- Drug-Induced Oral Candidiasis - A Case ReportDocument4 pagesDrug-Induced Oral Candidiasis - A Case ReportFajarRahmantiyoNo ratings yet
- HIMSS EMRAM CriteriaDocument2 pagesHIMSS EMRAM CriteriaReinhard Harianja100% (1)
- Chronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFDocument3 pagesChronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFGita Dwi DesianiNo ratings yet
- Occurrence of Candida Albicans in Periodontitis PDFDocument7 pagesOccurrence of Candida Albicans in Periodontitis PDFAbdoNo ratings yet
- Haider OralllllllllllllllllllllllDocument13 pagesHaider OralllllllllllllllllllllllAli YehyaNo ratings yet
- Lingual Bony ProminencesDocument9 pagesLingual Bony ProminencesAgustin BiagiNo ratings yet
- Fungal Diseases of The Oral MucosaDocument5 pagesFungal Diseases of The Oral MucosaManar AlsoltanNo ratings yet
- Oral CandidasisDocument39 pagesOral CandidasisArmada Eka FredianNo ratings yet
- 588 Article+Text 1884 1 10 20220107Document9 pages588 Article+Text 1884 1 10 20220107Dave PutraNo ratings yet
- Aop 157Document4 pagesAop 157rochmandrg dokter gigiNo ratings yet
- Faecal Microbiota Transplantation in The Treatment of C - 2020 - Human Microbiome JournalDocument5 pagesFaecal Microbiota Transplantation in The Treatment of C - 2020 - Human Microbiome Journalbig.ben.bar.123No ratings yet
- Atrophic CandidiasisDocument5 pagesAtrophic Candidiasisdup11No ratings yet
- Microscopia DirectaDocument5 pagesMicroscopia Directanydiacastillom2268No ratings yet
- Clostridium Difficile EpidemiologyDocument36 pagesClostridium Difficile EpidemiologyIsha BhattNo ratings yet
- Oral CandidiasisDocument4 pagesOral CandidiasisAnish RajNo ratings yet
- Mucormycosis The Deadly Fungus A Case Report.50Document5 pagesMucormycosis The Deadly Fungus A Case Report.50rinakartikaNo ratings yet
- Pseudomembranous Candidiasis Induced byDocument5 pagesPseudomembranous Candidiasis Induced byGenevieve Florencia Natasya SaraswatiNo ratings yet
- Bacterial Colonization of Blood Pressure Cuff: A Potential Source of Pathogenic Organism: A Prospective Study in A Teaching HospitalDocument3 pagesBacterial Colonization of Blood Pressure Cuff: A Potential Source of Pathogenic Organism: A Prospective Study in A Teaching HospitalvickaNo ratings yet
- Assessment of Oral Sample Collection Technique For The Isolation of Candida Albicans From Patients Having Denture StomatitisDocument4 pagesAssessment of Oral Sample Collection Technique For The Isolation of Candida Albicans From Patients Having Denture StomatitisDebby ApriliaNo ratings yet
- Journal Reading - Muhamad Al Hafiz - 1920221169Document12 pagesJournal Reading - Muhamad Al Hafiz - 1920221169David Al Haviz100% (1)
- Pathogenesis and Treatment of Oral CandidosisDocument20 pagesPathogenesis and Treatment of Oral CandidosiselisabethpriskaNo ratings yet
- Cabt 10 I 1 P 1Document5 pagesCabt 10 I 1 P 1Hanifah Nailul AmaniaNo ratings yet
- Oral Leishmaniasis Report of Two Cases 2020Document5 pagesOral Leishmaniasis Report of Two Cases 2020MARIE SELENE RAMIREZ REVOLLARNo ratings yet
- Red and White Lesions of The Oral Mucosa: DR - Wisam RasoolDocument43 pagesRed and White Lesions of The Oral Mucosa: DR - Wisam RasoolFlorida ManNo ratings yet
- GRUPO 8 ParacoccidioidomicosisDocument3 pagesGRUPO 8 ParacoccidioidomicosisSHARICK EDITH GUZMAN RODRÍGUEZNo ratings yet
- DentalDocument12 pagesDentalVeena PatilNo ratings yet
- Candidosis A New ChallengeDocument7 pagesCandidosis A New ChallengeSalvador contreras huertaNo ratings yet
- The Concordance of Three Diagnostic Test For MalasDocument7 pagesThe Concordance of Three Diagnostic Test For Malassea meei meeiNo ratings yet
- Oral CandidiasisDocument22 pagesOral CandidiasisSherlocknovNo ratings yet
- CandidiasisDocument51 pagesCandidiasisLincy JohnyNo ratings yet
- 446 P Singh - 0620188 PDFDocument9 pages446 P Singh - 0620188 PDFVibhor Kumar JainNo ratings yet
- Odontogenic Infections Microbiology and ManagementDocument5 pagesOdontogenic Infections Microbiology and ManagementJeninNo ratings yet
- Chromoblastomycosis: Differential DiagnosesDocument4 pagesChromoblastomycosis: Differential DiagnosesPranab ChatterjeeNo ratings yet
- Etiology of Gingivitis: September 2011Document19 pagesEtiology of Gingivitis: September 2011Phúc BùiNo ratings yet
- Jurnal OM 2Document6 pagesJurnal OM 2Reiza PrabandanaNo ratings yet
- Second Primary OSCC 2Document6 pagesSecond Primary OSCC 2James BondNo ratings yet
- Oral Candidiasis: Etiology and PathogenesisDocument5 pagesOral Candidiasis: Etiology and PathogenesisNovita Indah PratiwiNo ratings yet
- Chapter 18interactions Between Candida Species and Bacteria in Mixed InfectionsDocument13 pagesChapter 18interactions Between Candida Species and Bacteria in Mixed InfectionsRisca ArianiNo ratings yet
- No. 4 Prevalence - of - Oral - Candida PDFDocument8 pagesNo. 4 Prevalence - of - Oral - Candida PDFPrisillia MottohNo ratings yet
- Tinea Corporis Caused by Microsporum Audouinii: Case ReportDocument5 pagesTinea Corporis Caused by Microsporum Audouinii: Case ReportArasti Qisthi VanzifaNo ratings yet
- 455.full CandidiasisDocument6 pages455.full CandidiasisIdris Siddiq CuakepNo ratings yet
- Presentation 2Document32 pagesPresentation 2Dr. Bashir MehrNo ratings yet
- CandidiasisDocument20 pagesCandidiasisMoustafa Hazzaa100% (1)
- C. Diff Toxin AssayDocument15 pagesC. Diff Toxin AssayMaira KhanNo ratings yet
- Fungal Infection Case StudiesDocument4 pagesFungal Infection Case StudiesJape GarridoNo ratings yet
- Candida Infection in Oral Leukoplakia An Unperceived Public Health ProblemDocument5 pagesCandida Infection in Oral Leukoplakia An Unperceived Public Health ProblemBrili AnenoNo ratings yet
- ReferenceDocument163 pagesReferenceAjay IyerNo ratings yet
- Oral Candidiasis: A Retrospective Study of 276 Brazilian PatientsDocument5 pagesOral Candidiasis: A Retrospective Study of 276 Brazilian PatientsYuganya SriNo ratings yet
- Candidiasis MedscapeDocument36 pagesCandidiasis MedscapesummiyaNo ratings yet
- 10 1016@j Mycmed 2018 08 002Document5 pages10 1016@j Mycmed 2018 08 002Feni SyawelmiNo ratings yet
- V37n3a02 en IdDocument8 pagesV37n3a02 en IdIip RyanNo ratings yet
- Otolaryngologic Manifestations of HIV Infection: ReviewsDocument6 pagesOtolaryngologic Manifestations of HIV Infection: ReviewsSo NicNo ratings yet
- Art:10.1007/s13555 016 0158 XDocument5 pagesArt:10.1007/s13555 016 0158 XMaya LarasNo ratings yet
- White and Red Lesion Lecture 1 - DR Ameena Ryhan DiajilDocument43 pagesWhite and Red Lesion Lecture 1 - DR Ameena Ryhan Diajilفاطمة احمد غضبان الزياديNo ratings yet
- Acne and Bacteria Research PaperDocument7 pagesAcne and Bacteria Research Paperqwmojqund100% (1)
- Jurnal BM 2Document6 pagesJurnal BM 2Husnul KhatimahNo ratings yet
- ContempClinDent111-3628383 - 100443 HIVDocument5 pagesContempClinDent111-3628383 - 100443 HIVthomas purbaNo ratings yet
- Plasmablastico NavalDocument7 pagesPlasmablastico NavalLuis Javier Dulanto MoscosoNo ratings yet
- DL KeylaDocument1 pageDL KeylarerezNo ratings yet
- Acute Heart FailureDocument31 pagesAcute Heart FailurererezNo ratings yet
- SK Tim Directly Observed Treatment ShortcourseDocument2 pagesSK Tim Directly Observed Treatment ShortcoursererezNo ratings yet
- September 2021Document60 pagesSeptember 2021rerezNo ratings yet
- VCN KCVNJCVNJKBMDocument1 pageVCN KCVNJCVNJKBMrerezNo ratings yet
- Treatment Recommendations For HCVDocument35 pagesTreatment Recommendations For HCVrerezNo ratings yet
- C GkjxcfhsDocument1 pageC GkjxcfhsrerezNo ratings yet
- Knsdjbfulsnshomkvbsbsc C DJKBVDocument1 pageKnsdjbfulsnshomkvbsbsc C DJKBVrerezNo ratings yet
- HngvfgyifnjbDocument1 pageHngvfgyifnjbrerezNo ratings yet
- Glossitis Showing Hypertrophic Papillae With Granulomatous Ulcerations in A Case of Oral Mucosal CandidiasisDocument3 pagesGlossitis Showing Hypertrophic Papillae With Granulomatous Ulcerations in A Case of Oral Mucosal CandidiasisrerezNo ratings yet
- Glossitis Showing Hypertrophic Papillae With Granulomatous Ulcerations in A Case of Oral Mucosal CandidiasisDocument3 pagesGlossitis Showing Hypertrophic Papillae With Granulomatous Ulcerations in A Case of Oral Mucosal CandidiasisrerezNo ratings yet
- Listening ScriptsDocument3 pagesListening ScriptsNghi QuachNo ratings yet
- Effects of Mental Health On Physical WellDocument3 pagesEffects of Mental Health On Physical WellYash RaiNo ratings yet
- Pregnancy - Preparing To Be A MomDocument16 pagesPregnancy - Preparing To Be A MomTes B FourieNo ratings yet
- Foot Care Module and ChecklistDocument4 pagesFoot Care Module and ChecklistBeatrice AdorinoNo ratings yet
- Basics For IV PreparationDocument46 pagesBasics For IV PreparationOmayma IzzeldinNo ratings yet
- Findings From Arnold Ventures' Request For Information On The Dual-Eligible ExperienceDocument10 pagesFindings From Arnold Ventures' Request For Information On The Dual-Eligible ExperienceArnold VenturesNo ratings yet
- V-Gel Cleaning & User GuideDocument3 pagesV-Gel Cleaning & User GuideInstrulife OostkampNo ratings yet
- Ballad Scarce Resource Allocation Patient Notification LetterDocument2 pagesBallad Scarce Resource Allocation Patient Notification LetterJosh Smith100% (1)
- DD4 Practice Activities - AnswersDocument2 pagesDD4 Practice Activities - Answersgery sumualNo ratings yet
- Prosto 1Document11 pagesProsto 1saliamaharaniNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakajacksonmpNo ratings yet
- Peptic Ulcers: H.pylori Infection Is Usually Contracted in Childhood, Perhaps ThroughDocument2 pagesPeptic Ulcers: H.pylori Infection Is Usually Contracted in Childhood, Perhaps ThroughMike PalmaNo ratings yet
- NAS - Reimbursement Claim FormDocument2 pagesNAS - Reimbursement Claim FormPIANGO40% (5)
- Child Infection Diseases 9 Semester 5 Year Question PaperDocument2 pagesChild Infection Diseases 9 Semester 5 Year Question PaperDikshant DaswatNo ratings yet
- Slide Jurnal WHODocument24 pagesSlide Jurnal WHOJelly OeiyanoNo ratings yet
- WORKING SLIDES For AmpalayaDocument32 pagesWORKING SLIDES For Ampalayaapi-3700579No ratings yet
- Soft Skills For Pharmacist 2Document5 pagesSoft Skills For Pharmacist 2shailendra patilNo ratings yet
- Who Is A ScientistDocument7 pagesWho Is A ScientistTianna MorganNo ratings yet
- Referral PhilippinesDocument42 pagesReferral Philippinesemed vsmmcNo ratings yet
- Transfusion RXNsDocument67 pagesTransfusion RXNsSuha Abdullah100% (1)
- CARE Checklist English 2013 PDFDocument1 pageCARE Checklist English 2013 PDFNithin NairNo ratings yet
- .. Uploads Lecture Implant Overdenture 200702Document21 pages.. Uploads Lecture Implant Overdenture 200702siddu76100% (1)
- Liga NG Mga Barangay: Republic of The Philippines Province of Camarines SurDocument2 pagesLiga NG Mga Barangay: Republic of The Philippines Province of Camarines SurRave PerezNo ratings yet
- Correlation of Hearing Impairment With Site of Tympanic Membrane PerforationDocument4 pagesCorrelation of Hearing Impairment With Site of Tympanic Membrane PerforationAzwar RidhwanNo ratings yet
- Mice Rats in Biomedical Research FBRDocument2 pagesMice Rats in Biomedical Research FBRChikondi TemboNo ratings yet
- Bio DoopDocument6 pagesBio DoopAnaconda Warriors 12 ANo ratings yet
- Belo. Nur 192. Session 13 LecDocument3 pagesBelo. Nur 192. Session 13 LecTam BeloNo ratings yet
- International Postnatal Growth Standards For Preterm InfantsDocument3 pagesInternational Postnatal Growth Standards For Preterm InfantsNovalinda KasihNo ratings yet
- KDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFDocument102 pagesKDIGO 2023 Lupus Nephritis Guideline - Public Review - 9 Mar 2023 PDFlucasnatalia21bNo ratings yet