Professional Documents
Culture Documents
Absorption Windows
Uploaded by
Filip IlievskiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Absorption Windows
Uploaded by
Filip IlievskiCopyright:
Available Formats
REVIEWS
DDT Volume 10, Number 4 February 2005
Reviews KEYNOTE REVIEW
The transit of a drug (formulation) through the GI tract
will determine how long a compound will be in contact
with its preferred absorptive site. A good understanding of
gastrointestinal transit in humans and the effect of
factors such as food can be helpful in the design of drug
delivery systems.
Formulation strategies for
absorption windows
Stanley S.Davis
Absorption windows in the proximal gut can limit the
bioavailability of orally administered compounds and
can be a major obstacle to the development of
controlled release formulations for important drugs.
Methods to increase the residence of drug formulations
at or above the absorption window are discussed in
this review. Two main approaches are presently being
explored: (i) bioadhesive microspheres that have a
slow intestinal transit; and (ii) the gastroretentive
dosage system, which is based on multiparticulates or
large single unit systems. A good understanding of
gastrointestinal transit in humans and the effect of
factors such as food can be helpful in the design of
rational systems that will have clinical benefit.
Stanley S. Davis
Institute of Pharmaceutical
Sciences,
University of Nottingham,
University Park,
Nottingham,
UK, NG7 2RD
e-mail:
stanley.davis@nottingham.ac.uk
Oral drug administration still remains the route of choice for the
majority of clinical applications. Some drugs have ideal characteristics for good absorption to occur throughout the gastrointestinal (GI)
tract, whereas others present difficulties. The Biopharmaceutical
Classification System, introduced by the Food and Drug Administration
(FDA) in 1995, has categorized drugs in terms of their solubility and
intestinal permeability. Class I compounds are defined as those with
high solubility and high permeability, and are predicted to be well
absorbed when given orally. All other compounds (classes IIIV) suffer
from low solubility, low permeability or both, and will present challenges
to the development of products with acceptable oral bioavailabilities.
An increasing number of new chemical entities are to be found in
classes IIIV and many of these display variable absorption in different
regions of the human GI tract [1]. Polar compounds and those that
rely on some form of facilitated transport process generally display
good absorption from the upper GI tract, but are poorly absorbed in
the large intestine (or colon). As a consequence, their oral bioavailabilities can be affected by the limited absorptive site. In addition, the
development of a modified release product, such as those designed to
1359-6446/04/$ see front matter 2005 Elsevier Ltd. All rights reserved. PII: S1359-6446(04)03351-3
STANLEY S. DAVIS
Professor Stanley S. (Bob)
Davis obtained his
Bachelors degree in
Pharmacy from the School
of Pharmacy at the
University of London in
1964. He remained at the
same University to study for a PhD in colloid
science. In 1966, he was appointed Assistant
Lecturer in Pharmaceutics and then to Lecturer in
1967. He was awarded his Doctor of Science
degree (higher doctorate) in 1982. In 1968, he was
awarded a one-year Fulbright Scholarship to
undertake postdoctoral studies with Professor
Takeru Higuchi at the University of Kansas, USA, in
the field of solution thermodynamics. In 1970,
Davis moved to the University of Aston,
Birmingham, UK, as Senior Lecturer and Head of
the Pharmaceutics section, where he built an
active research group in drug delivery systems.
Davis took the position of Lord Trent Professor of
Pharmacy at the University of Nottingham, UK, in
1975, where he ran a large research group,
studying novel drug delivery systems.Topics of
research have included drug targeting (with
particular emphasis on colloidal carriers),
transmucosal delivery, oral and parenteral systems
for controlled release and product evaluation
through gamma scintigraphy. He became an
Emeritus Professor in 2003. Davis has published
over 700 papers and is co-editor of seven books.
He is the co-founder of two pharmaceutical
companies, Danbiosyst (UK) Ltd (now part of West
Pharmaceutical Services) and Pharmaceutical
Profiles Ltd. Davis has acted as a consultant to
various pharmaceutical companies, and has
served on numerous committees and panels,
including European Pharmacopoeia, Medicines
Commission, Science and Engineering Research
Council.
www.drugdiscoverytoday.com
249
DDT Volume 10, Number 4 February 2005
REVIEWS
Reviews KEYNOTE REVIEW
provide once-daily dosing, will be difficult, if not impossible. Hence, the concept of an absorption window has
become popular [2].
also seen after delivery to the colon, but the area under
the curve (AUC) and the maximum plasma concentration
(Cmax) values were markedly reduced.
Absorption windows
Gastrointestinal transit
Some drugs display region-specific absorption that can be
related to differential drug solubility and stability in
different regions of the intestine as a result of changes
in environmental pH, degradation by enzymes present in
the lumen of the intestine or interaction with endogenous
components such as bile [3]. Active transport mechanisms
for drugs involving carriers and pump systems have been
well described [4]. Compounds such as ACE inhibitors
and certain antibiotics exploit peptide transporters. The
importance of P450 metabolism in the intestinal mucosa
has now been recognized. The isoform P4503A4 (CYP3A4)
is dominant in gut wall metabolism and different levels
are found in different regions of the intestine. The
absorption of drugs can also be limited by efflux mechanisms, especially if compounds are lipophilic in nature. The
secretory transporter P-glycoprotein located on the mucosal
surface of epithelial cells is responsible for the low and
variable bioavailability of various compounds (e.g. propranolol, felodipine) [5]. Some drugs can be substrates for
both CYP3A4 and p-glycoprotein (e.g. cyclosporin, itraconazole) [6]. In theory, it should be possible to inhibit
efflux and metabolism processes by the use of inhibitors,
but such agents are not usually without their own pharmacological effects. The inhibitory effect of grapefruit
juice toward intestinal cytochrome P450 is a well known
example [7].
Today, it is possible to assess regional differences in
intestinal drug absorption by conducting a non-invasive
human drug absorption (HDA) study using a remotecontrolled delivery capsule [1]. Gamma scintigraphy is
used for real-time visualization of capsule location, and a
radio frequency signal is used to activate the capsule at
the target site. For example, in order to determine the
bioavailability and pharmacokinetic profile of faropenem
daloxate (a prodrug of a broad-spectrum antibiotic), this
drug was delivered in a particulate form to the proximal
small bowel, distal small bowel or ascending colon. The
pharmacokinetic profiles for delivery to the two sites in
the small intestine were similar and comparable to those
for a reference tablet (Table 1). Significant absorption was
The transit of a drug (formulation) through the GI tract
will determine how long a compound will be in contact
with its preferred absorptive site. In humans, the small
intestine transit time is reasonably constant: at around
three hours for a drug formulation (or for a meal) to pass
from the stomach to the ileo-caecal junction [8]. Transit
through the colon is much longer and can be 20 h or
more [9]. Hence, the time a drug will have in its absorption
window can be relatively short, more so if the drug is preferentially absorbed in the proximal small intestine (e.g.
jejunum) rather than throughout the small bowel.
Consequently, the bioavailability of a drug, which is
largely or exclusively absorbed from the upper GI tract,
will be affected by factors that change GI transit. For
example, the presence of food in the stomach will slow
the rate of gastric emptying and will thereby keep the
drug above or at the absorption window for a longer
period of time. An increase in bioavailability might then
be expected. However, if formulation excipients are used
that increase the rate of transit in the small intestine (e.g.
through an osmotic effect), the bioavailability can be
reduced as observed with cimetidine, a polar drug that is
almost exclusively absorbed from the small intestine [10].
Some important drugs have absorption windows in the
small intestine and, as a result, they often display low
bioavailability after oral dosing. In addition, they are difficult to formulate into extended release products because
on arrival in the colon (or even before), absorption will
be low or non-existent (Box 1). Efforts have been made
to improve absorption, and various different strategies
have been described in the scientific literature and in published patents. This article will review some of the strengths
and weaknesses, and outlines some of the more promising
current developments.
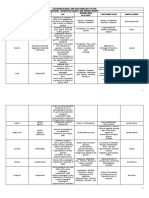
TABLE 1
Pharmacokinetic parameters for faropenem (free acid) following siteselected delivery to different regions of the human gastrointestinal
a
tract
IR tablet
Proximal small Distal small
intestine
intestine
Ascending colon
AUC (mg hour-1 l-1) 25.8
22.7
20.1
8.6
Cmax (mg l-1)
11.8
10.0
2.3
15.3
Data obtained from Ref. [1]. Abbreviations: AUC, area under curve; Cmax, maximum plasma
concentration; IR, immediate release.
250
www.drugdiscoverytoday.com
Preformulation studies
Before one can attempt to solve a problem, it is useful to
first understand why a drug displays low and site-specific
absorption. Data gathered in preformulation studies will
often provide some insight into crucial characteristics,
such as drug solubility and drug stability. Similarly, in vitro
permeability studies using cultured cell systems such as
Caco-2 can give an indication of potential problems [11].
Formulation strategies to improve dissolution rate and
drug stability can be investigated. For example, Terao et al.
[12] investigated the feasibility of widening the absorption
window of furosemide by controlling the pH in distal
parts of the intestine using a methacylate polymer. Good
results were obtained with an in vitro rat model, but
extrapolation to clinical practice is uncertain. Enteric coatings to prevent drug exposure to the adverse conditions
BOX 1
Drugs that would benefit from increased residence
in the small intestines or stomach
There are several examples of drugs that would benefit from
an increase in the time that a formulated product resides in
the stomach or small intestine.These are listed as follows:
Acyclovir
Bisphosphonates
Captopril
Furosemide
Metformin
Gabapentin
Levodopa
Baclofen
Ciprofloxacin
in the stomach are a standard approach. Coating strategies
are also available to deliver the drug to a preferred region
in the distal intestines where drug stability (physical and
metabolic) or even absorption could be better [13].
Poor permeability can sometimes be improved by the
use of an absorption enhancer. Current research is focusing
on agents that can modify the tight junctions between
cells in a transient manner [14]. Interestingly, several
materials such as surfactants that are well-known excipients
can enhance the absorption of drugs displaying low
bioavailabilities. This approach is most relevant to polar
compounds, including peptides and proteins.
Methods designed to provide longer contact of the drug
or delivery system with the crucial absorption region fall
into two different categories: (i) those that attempt to slow
down transit through the small intestine; and (ii) those
that attempt to hold the drug formulation above the
absorption window through gastroretention.
Modification of small intestine transit
Pharmacological methods
It is well known that drugs can alter GI transit. For
example, scintigraphic data have indicated that pre-treatment with metoclopramide decreased gastric emptying
time and increased GI motility, whereas pre-treatment
with propantheline had the opposite effect [15]. The
extent of metformin absorption (a drug primarily absorbed
from the small intestine) is improved when the GI motility
is slowed. Drug combinations that contain gastrokinetic
agents such as metoclopramide have been marketed, but
it would be difficult to imagine that regulatory authorities
would accept the addition of a second drug to improve
the bioavailability of another. (Similar considerations
apply to the use of inhibitors discussed above.)
Natures methods
Dietary components such as fats, certain amino acids and
peptides can slow gastric emptying and intestinal transit
[16,17]. A lesser-known phenomenon is the ileal brake
[18]. There are particular dietary components, for example,
REVIEWS
fats and fatty acids, that are infused into the terminal
ileum and can cause a slowing of intestinal transit. This
braking mechanism appears to be a feedback process for
the improved digestion of dietary components. Studies
have been performed in humans to identify optimal ileal
brake activators (quality and quantity). One of which
investigated whether ileal brake activators could alter the
bioavailability of atenolol from the small intestine by
slowing intestinal transit and thereby increasing the time
available for absorption [19]. Oleic acid and a monoglyceride
were formulated into modified release capsules that were
targeted to the small intestine. The results showed that,
in some volunteers, an increase in small intestine transit
time led to an increase in the quantity of drug absorbed.
However, drug absorption was related not only to the total
time spent by the drug in the small intestine, but also
other factors such as the proportion of such time spent at
the ileo-caecal junction. This study highlighted the complexities of exploiting natural GI processes to enhance the
oral bioavailability of drugs.
Kroening et al. have recently reported that tapeworms
can slow the transit of intestinal contents [20]. Of the
tapeworm-secreted compounds tested, only lumenal infusion of guanosine 3,5-cyclic monophosphate (cGMP)
induced contractile patterns that mimicked those observed
during tapeworm infection. As a consequence, it has been
suggested that cGMP might be used in proprietary pharmaceutical formulations to improve drug absorption;
Wisconsin investigators have filed for a patent on the
idea of adding cGMP to drugs to lengthen the amount
of time they spend in the gut and thus increase how much
medicine a person absorbs (http://www.sciencenews.
org/articles/20030322/fob6.asp).
Unfortunately, the patent position will be less than
certain because, in 1982, the Escherichia coli heat-stable
toxin was reported to activate the cGMP system [21],
which altered motor activity thus slowing transit and
enabled bacterial proliferation and invasion.
Bacteria have other strategies that help to promote
invasion. Fimbriae are long filamentous protein projections
on the surface of certain organisms that allow them to
adhere to receptors on the brush borders of villous enterocytes [22]. Caston et al. investigated the use of purified
fimbriae from E. coli as a natural bioadhesive [23]. The fimbriae were attached to small microspheres. Encouraging
data were reported for a rat model in terms of an increase
in small intestine transit, but the system has yet to be
investigated in humans. In a similar fashion, various
groups have studied the use of plant lectins to target the
lumenal surface of the small intestine. Once again, animal
studies have been supportive. For example, two plant
lectins selected by Montisci et al. (Lycopersicon esculentum
L. and Lotus tetragonolobus lectins) were reported to be
specific for oligomers of N-acetyl-D-glucosamine and
L-fucose, respectively, and were conjugated to small
radiolabeled poly (lactide) microspheres [24]. The transport
www.drugdiscoverytoday.com
251
Reviews KEYNOTE REVIEW
DDT Volume 10, Number 4 February 2005
DDT Volume 10, Number 4 February 2005
REVIEWS
Reviews KEYNOTE REVIEW
and distribution of the particles along the intestine, as
well as their interactions with the intestinal mucosa, were
determined after oral administration in rat. The overall
transit of the particles was delayed when the microspheres
were conjugated to the lectins, mainly because of gastric
retention. A significant fraction of the conjugates adhered
to the gastric and intestinal mucosae, but the interaction
process appeared to be largely a result of non-specific
interactions. Apparently, premature adsorption of soluble
mucin glycoprotein limited specific (lectin-mediated) adhesion. Some 15 years ago, a similar conclusion was reached
concerning the role of soluble (non-adherent) mucin from
studies conducted in humans. Using the technique of gastroscopy, we examined the mucoadhesive properties of
small bioadhesive tablets, which carry a net positive
charge. In vitro studies had shown that such a charge provided a good interaction with the negatively charged sialic
acid groups on gastric mucus [25]. The video films obtained demonstrated that it was a easy to attach mucus
to the small tablets, but the reverse process of attaching
small tablets to the mucus adhering to the stomach wall
was a different matter. Mucus adherence and turn over
still represents an obstacle when trying to slow small
intestinal transit.
Bioadhesion
For years pharmaceutical scientists have been fascinated
by the concept of bioadhesion. Various attempts have
been made to identify putative bioadhesive or mucoadhesive materials using in vitro and in vivo tests. Unfortunately,
in many cases, such tests have been based on a poor
understanding of relevant behavior of the human GI tract.
As a result, systems that performed well in vitro or in
animal models failed to live up to expectations in humans. The rat, dog and pig are not good models for the
human GI tract especially where transit processes are
concerned.
Bioadhesive microspheres based on the pharmaceutically acceptable cationic polymer chitosan have been of
special interest [26]. Chitosan is known to bind well to
mucus, and microparticles coated with chitosan adhere
well in the intestine of animals [27]. However, good
adhesion and delayed transit do not always translate into
improved bioavailability of an administered drug. Clearly,
with a system like bioadhesive microspheres, the incorporated drug must be released at an appropriate rate and
be stable in the lumen to have a chance for absorption.
Shimoda et al. reported that their chitosan microsphere
system showed good adhesion to the intestinal mucosa,
but scarcely facilitated absorption of insulin [28]. This is
in line with expectation because insulin is very poorly
permeable and would be degraded rapidly in the lumen.
Claims of bioadhesion of microparticles in the human
GI tract are often based on circumstantial evidence in the
form of altered pharmacokinetic profiles rather than the
direct measurement of transit using properly labeled
252
www.drugdiscoverytoday.com
formulations and techniques such as gamma scintigraphy. For example, two kinds of sustained-release microspheres, adhesive and non-adhesive, containing furosemide
and riboflavin, were prepared and administered to fasted
volunteers in hard gelatine capsules [29]. Areas under the
plasma concentrationtime curves (AUC) were 1.8 times
larger for furosemide and the urinary recovery was 2.4
times higher for riboflavin when adhesive microspheres
were used as compared with the non-adhesive system.
These are interesting results, but no hard data on altered
transit were provided.
Flamel Technologies have described the design of a proprietary drug delivery system (Micropump microparticles) that is claimed to be bioadhesive and which allows
an extended transit time in the small intestine with mean
residence time in the plasma extended up to 24 h (http://
www.flamel.com/micropump.htm). This system is stated
to be particularly suitable for short-lived drugs known
to be absorbed only in the small intestine. However, as
far as can be ascertained, the extended intestinal transit
has yet to be demonstrated in humans. Indeed, it is hard
to find any published evidence to demonstrate that strategies of bioadhesion will change transit through the small
intestine of humans (an effect on gastric emptying has
been found, as described below). As aforementioned, the
transit of food and pharmaceuticals through the small
intestine is reasonably constant in humans with a mean
value of around three hours. It is little affected by fed
state, age, particle size, shape, density or disease condition
[9]. This is not too surprising because the small intestine
has a role of moving material to the colon by a process of
peristalsis. The mucus that lines the intestine has a protective role and a quick turnover. Moreover, the surface
of administered particles can be rapidly conditioned by
the adsorption of endogenous components such as nonadherent mucus. Notwithstanding, it has been has been
postulated that, because of their size, very small particles
could perhaps become trapped between the villae of the
small intestine (and also in the folds of the stomach). To
test this proposal, Brown et al. followed the transit of very
small particles (in the ranges of 7080 m, 110 m and
500 nm) in the human gut [30] using gamma scintigraphy.
The results showed that the particles all had similar transit
behaviors and that the measured transit times were
in broad agreement with those reported previously for
conventional multiparticulate systems such as pellets.
Recently, a new approach to delaying transit has been
proposed using super-porous hydrogels that swell rapidly
in water and in so doing should slow intestinal transit
[31]. Various in vitro experiments have been described,
together with some data obtained in an animal model
(pig) [32]. In the pig model, the hydrogel enhanced the
intestinal absorption of insulin. However, human investigations are apparently ongoing and the same type of
hydrogel is also being evaluated for its gastroretentive
properties.
REVIEWS
DDT Volume 10, Number 4 February 2005
Gastroretention
BOX 2
In theory, an elegant and simple way to improve drug
absorption is to hold a drug delivery system above the
absorption window and for the drug to be released at an
appropriate rate. Because most absorption windows are
thought to be located in the proximal small intestine, the
obvious strategy will be to hold the formulation in the
stomach (i.e. gastroretention). This concept was advanced
many years ago and has been the subject of extensive
research, publications and patents filings, with some successes, but many failures. The Holy Grail remains the
retention of a delivery system in the fasting human stomach using a system that will be safe and effective.
The process of GI transit in humans and its implications
for drug delivery are now well understood (Box 2) [9].
Dosage forms administered to a fed stomach will have
delayed emptying. A multiparticulate system, such as one
containing microspheres or pellets, can become mixed
with the food and, as a consequence, will usually empty
with the food over an extended period of time [33]. If the
administered particles are large, they will not be able to
pass through the constricted pylorus with the digested
food, and will have to wait until the stomach is empty
and in the fasted state. There has been some debate in the
past as to the cut-off size for retention in the fed stomach.
Unfortunately, data obtained in the dog have been extrapolated directly to human without any attempt at scaling.
In general, particles up to ~10 mm in size can be expected
to empty from the fed stomach. Exactly when the particles
empty will also depend on their number and their relative positions within the stomach. Hence, a dosage form
larger than 15 mm and administered with food is expected
to achieve gastroretention. Such a dosage form will then
have an opportunity to empty after the food has left the
stomach when the fasted state occurs. In the fasted stomach,
different levels of activity occur in the form of contractions or waves [9]. One particular wave called the housekeeper wave is very relevant. This wave, as its name suggests, can function to clear undigested material from the
stomach through the relaxed and open pylorus into the
intestine. Such waves occur about every two hours in
humans, but are inhibited by food. Hence, if the stomach
is maintained in the fed state, for instance, by repeated
administration of small meals, a single unit could have
extended retention. Unfortunately, this process of repeated
feeding will not be a sensible strategy for achieving gastroretention in a clinical setting.
A single unit system (or a multiparticulate) can empty
rapidly from the fasted stomach. Exactly when it will
empty will also depend on the timing of the housekeeper
wave in relation to dosing. The open pylorus has a diameter of ~15 mm in humans. An object greater than this size
will have difficulty in passing into the small intestine in
the fasted (or fed) state. Based on this knowledge, various
approaches have been devised for gastroretention. These
fall into two main classes: (i) small particles that have
Gastrointestinal transit of pharmaceutical dosage
forms
Gastric emptying is controlled by feeding status
Objects less than 10 mm in size can empty from the fed
stomach
Large objects (>20 mm in size) will be retained in the fed
stomach
The transit time in the small intestine is ~3 h
A dosage form can reach the colon in 45 h in fasted
subjects
Transit in the colon is lengthy (~20 h)
bioadhesive properties (and also a propensity to float on
the stomach contents); and (ii) large swelling objects that
will be retained in the stomach because of their size. These
swelling systems might also have floating characteristics,
usually provided by the generation of carbon dioxide. The
early literature on gastroretentive systems has been wellreviewed elsewhere [34,35], and only the more recent
developments and strategies will be considered here.
Attention will be focused on systems that have been
tested in humans. As discussed earlier, promising results
obtained in vitro and in animal models have not always
translated well to human. In many cases, the realities of
human gastric emptying have been neglected. Floating
systems require fluid in the stomach to function. While
this might be the case for the fed stomach, the fasted
stomach will contain little fluid and a liquid given at the
time of dosing will empty rapidly. Thus, for the fasted
state, floating will be transient but might allow other
mechanisms to operate such as mucoadhesion. Floating
systems could also have their limitations in the fed state
because a change in body position to supine will have a
direct effect on the floating system and its proximity to
the pylorus.
Microparticulates
Gastroretentive microparticles have been investigated,
but few studies have demonstrated success in clinical
investigations. Pivotal studies in Nottingham University,
UK, have revealed that oral dose forms containing finely
divided ion-exchange resins can provide prolonged gastric
residence and uniform distribution within the stomach
[36]. For such an effect, the particles will need to be small
from a mechanical consideration and of low density so
that they might be able to float. A positive charge should
also confer an advantage. Adherence to the wall of the
stomach will be possible during the emptying process in
both the fed and fasted state, assuming that the mucoadhesive properties of the particles have not been modified
by the stomach contents, in particular, non-adherent
mucus (Figure 1).
www.drugdiscoverytoday.com
253
Reviews KEYNOTE REVIEW
There are many factors that control the gastrointestinal
transit of pharmaceutical dosage forms, summarized below:
DDT Volume 10, Number 4 February 2005
REVIEWS
Reviews KEYNOTE REVIEW
Microspheres float on stomach contents
Microspheres adhere to stomach wall during gastric emptying
Drug Discovery Today
FIGURE 1
Proposed mechanism for retention of bioadhesive microspheres in the human stomach. A capsule containing the bioadhesive microspheres is
administered with water and the released microspheres float on the fluid in the stomach. During the process of gastric empyting, a proportion of the
bioadhesive microspheres adheres to the stomach wall to provide gastroretention.
Chitosan, a popular choice as a coating material because
of its regulatory status and its positive charge, binds to
mucus [26] (Figure 2). In constructing controlled release
chitosan formulations, it is important to retain the positive
nature of the material. Sakkinen et al. have described a
gamma scintigraphic evaluation of the fate of microcrystalline chitosan granules in the fasted human stomach [37].
The in vivo mucoadhesion of the chitosan formulations
was better than that of a control but was erratic, and the
authors concluded that, in their present form, the formulations studied were not reliable gastroretentive drug
delivery systems. No data were provided as to the charged
nature of the chitosan, and no attempt was made to provide a floating effect and enhanced contact with the gastric
mucosa. Chitosan-based systems for local delivery of
antibiotics in the stomach have been described by Torrado
et al. [38], who studied a swelling chitosan-poly (acrylic)
acid-based controlled drug release system in humans. The
gastric half-emptying time of the polyionic complex was
significantly delayed when compared with that of a reference formulation. An interesting gastroretentive floating
chitosan-based system is described by West Pharmaceutical
Services (http://www.westpharma.com/drug%20delivery/
oral_delivery.asp) in the form of controlled release lowdensity microspheres. It is stated that the microspheres
float on the stomach contents, and then adhere to the
mucous lining as the stomach empties. The release of drug
from the system can be controlled to coincide with the
half-life emptying of the system from the stomach. Full
clinical data have yet to be provided.
Swelling and expanding systems
FIGURE 2
Interaction of mucin with chitosan. An enhanced electron
micrograph showing mucin as long strands attached to chitosan
aggregates. Chitosan interacts with mucin through charge interaction
and hydrogen-bonding mechanisms.
254
www.drugdiscoverytoday.com
Perhaps the most promising approach to achieving gastroretention is that of creating a swelling or expanding
system in situ. This is easier said than done. Any system
will need to expand to a size large enough to be retained
in the (fasted) stomach, but to do so in a safe and reliable
manner. It must not swell or expand in the oesophagus
or in the intestines, if it is emptied prematurely from the
stomach (e.g. problems could arise from the formation of
an insoluble mass known as a bezoar). The gastroretentive system will also need to display controlled release
properties so that the drug is released at an appropriate
rate for optimal absorption from the absorption window.
The system should have sufficient rigidity to remain intact in the stomach and to withstand the mechanical
forces therein. Last but not least, it will need to decrease
in size (degrade) after it has performed its function and
then transit through the intestines in the normal way.
The various systems described in the literature (to include
numerous patents) usually achieve an increase in size
through processes of expansion or swelling, or through
unfolding. Expansion and swelling processes have either
involved the generation of gas, in the form of carbon
dioxide, or have exploited the properties of compressed
porous materials such as hydrogels. Some earlier systems
were based on novel geometries, such as long worm-like
structures [34,35].
The fasted stomach presents a severe challenge in
terms of the limited time available for a size increase
and for retention to be achieved. By contrast, the lightly
fed stomach can provide sufficient residence time for a
suitable size increase. Therefore, it is not surprising to
find that the majority of studies conducted on putative
(a)
(b) (i)
(ii)
Drug Discovery Today
FIGURE 3
The Depomed Gastric Retention (GR) System. (a) The Gastric Retention (GR,
Depomed) system in the non-swollen and swollen state is indicated, with a coin for
comparison. (b) Gamma scintiscans showing the retention of the system in the stomach
of a healthy volunteer.The formulation was labelled with two radionuclides of different
energy characteristics to allow visualization of: (i) the retention of the swollen matrix
in the stomach; and (ii) the erosion and gastric empyting of the drug-containing layer.
gastroretentive systems in human have involved the
fed state.
Super-porous hydrogel composites have been described
as a strategy to delay small intestine transit. These devices,
which have a very high swelling capacity because of the
presence of numerous large pores, have also been investigated as gastroretentive systems [39]. Evaluation has been
made in dogs, both under fasted and fed conditions, but
these systems have yet to be tested in humans. Under
fasted conditions, the composites remained in the stomach
of the dog for two to three hours before breaking into two
pieces and then emptied. When food was given before the
experiment, the composite remained in the stomach for
more than 24 h, although the fed condition was maintained only for the first few hours. Such results are
encouraging, but I am reminded of our own studies performed some years ago on so-called gastroretentive systems
[40]. Tablets formulated using hydrophilic polymers were
tested in dogs and were found to have excellent gastroretentive properties (greater than 12 h) even in the fasted
state. Sadly, when these systems were tested in human
volunteers using scintigraphy, the average time for emptying from the fasted stomach was just 33 minutes. Hence,
the dog is not a good model for human. The pig is a better
model than dog, but pigs have a longer gastric retention of
pellets and tablets than that in humans [41]. The best
model for human is human.
The drug delivery company Depomed have described
gastroretentive tablets that swell in the stomach which
treats the tablet like undigested food, and wont let it pass
into the small intestine. The tablet is retained by the stomach for several hours, where it can deliver its payload
of drug as quickly or slowly as desired (http://www.
depomedinc.com/products_pipeline.htm).
These systems are based on polyethylene oxide (PEO)
in combination with hydroxypropyl methylcellulose
(HPMC) to produce a sustained-release matrix tablet that
can swell. According to the company, candidate molecules include metformin, gabapentin ciprofloxacin and
furosemide. Recent press releases state that Depomed has
completed Phase III clinical trials with once-daily metformin
for the treatment of Type II diabetes and with once-daily
ciprofloxacin for the treatment of urinary tract infections,
and that new drug applications (NDA) for both products have been filed with the FDA. The company is also
conducting a Phase II trial with the diuretic furosemide.
No full publications are yet available and, the degree
and/or rate of swelling achieved might not be sufficient
to allow retention of the dosage form in the fasted state.
A recent abstract has described a dual-labelled scintigraphic study of controlled release furosemide gastric
*Louie-Helm, J. et al. (2003) Dual-labeled pharmacoscintigraphic study
of furosemide gastric retention (GRTM) tablets in healthy volunteers.
Abstract no. 118, Proceedings of the Controlled Release Society 30th
Annual Meeting held 1923 July 2003, in Glasgow, UK.
www.drugdiscoverytoday.com
255
Reviews KEYNOTE REVIEW
REVIEWS
DDT Volume 10, Number 4 February 2005
DDT Volume 10, Number 4 February 2005
REVIEWS
Reviews KEYNOTE REVIEW
retentive tablets in healthy volunteers*. The dual-labelling
procedure permitted separate characterization of the erosion and swelling. The tablets (and an immediate release
control) were administered after a high-fat breakfast.
Gastric residence of the swelling tablets was sufficiently
long to deliver the drug to the upper GI tract (Figure 3).
Consequently, the plasma concentration of the drug was
extended and, furthermore, unlike previous slow release
formulations reported in the literature, there was no
reduction in bioavailability. From a standpoint of patient
compliance, the gastroretentive tablet provided gradual
diuresis and natriuresis, rather than the brief and intense
diuresis of short onset time experienced by patients taking
conventional immediate release furosemide tablets.
Workers in Israel have developed an interesting unfolding expandable compressed-dosage form comprising
an inner polymeric and/or drug matrix layer with two
shielding outer layers containing a coating of microcrystalline cellulose to prevent adhesion [42]. The usual type
of dog study has been conducted with a demonstration
of an enhanced bioavailability for the marker compounds.
More importantly, two clinical studies have also been
reported where the gastroretentive dosage form containing
furosemide was given to volunteers [43]. This provided
altered pharmacokinetics and pharmacodynamics, which
were related to a longer residence in the stomach. In a
second study, the unfolding and physical integrity of the
dosage systems were evaluated in vitro and in vivo (by
gastroscopy and radiology) [44]. A combination of rigidity and large dimension of the dosage forms was considered to be a decisive parameter to ensure prolonged gastroretention of five hours or longer. A significant extension
of the absorption phase was demonstrated for levodopa;
a drug with a narrow absorption window, but it is noteworthy that the system was dosed with a light breakfast.
Further clinical data are awaited with interest for all the
systems described above. Data obtained by combining
gamma scintigraphy with pharmacokinetics will be decisive
in the selection of candidate systems before detailed evaluation takes place in Phase II clinical investigations [45,46].
Conclusions
While recent results from recent clinical studies are promising, convincing results have yet to be presented for a
gastroretentive system that displays the necessary performance behaviour (as listed above) and which is retained
in the fasted stomach of humans for a sensible period of
time after dosing. A swelling or expanding system appears
to be the best option, but rapid change in dimensions will
have to be achieved in a fail-safe manner. Furthermore,
the system will need to retain its integrity for an extended
period of time in the harsh conditions present in the
human stomach. Alternative approaches, such as attempts
to modify small intestine transit using bioadhesion, could
be frustrated by the efficient process of peristalsis and the
presence of non-adherent mucus.
References
1 Wilding, I. and Prior, D.V. (2003) Remote
controlled release capsules in human drug
absorption (HDA) studies. Crit. Rev. Ther. Drug
Carrier Syst. 20, 405431
2 Corrigan, O.I. (1997) The biopharmaceutic drug
classification and drugs administered in
extended release (ER) formulations. Adv. Exp.
Med. Biol. 423, 111128
3 Macheras, P. et al. (1995) Biopharmaceutics of
Orally Administered Drugs, Ellis Horwood
4 Bardelmeijer, H.A. et al. (2000) The oral route for
the administration of cytotoxic drugs: strategies
to increase the efficiency and consistency of
drug delivery. Invest. New Drugs 18, 231241
5 Siegmund, W. et al. (2003) Variability of
intestinal expression of P-glycoprotein in
healthy volunteers as described by absorption
of talinolol from four bioequivalent tablets.
J. Pharm. Sci. 92, 604610
6 Tamura, S. et al. (2003) The site-specific
transport and metabolism of tacrolimus in rat
small intestine. J. Pharmacol. Exp. Ther. 306,
310316
7 Kakar, S.M. et al. (2004) 67Dihydroxybergamottin contributes to the
grapefruit juice effect. Clin. Pharmacol. Ther. 75,
569579
8 Davis, S.S. et al. (1986) Transit of pharmaceutical
dosage forms through the small intestine. Gut 27,
886892
9 Washington, N. et al. (2001) Physiological
Pharmaceutics, Barriers to Drug Absorption
(2nd edn), Taylor and Francis
10 Adkin, D.A. et al. (1995) The effect of mannitol
256
www.drugdiscoverytoday.com
11
12
13
14
15
16
17
18
19
on the oral bioavailability of cimetidine. J. Pharm.
Sci. 84, 14051409
Sun, D. et al. (2004) In vitro testing of drug
absorption for drug developability assessment:
forming an interface between in vitro preclinical
data and clinical outcome. Curr. Opin. Drug
Discov. Devel. 7, 7585
Terao, T. et al. (2001) Improvement in site-specific
intestinal absorption of furosemide by Eudragit
L100-55. J. Pharm. Pharmacol. 53, 433440
Hirsch, S. et al. (1999) Lauroyldextran and
crosslinked galactomannan as coating materials
for site-specific drug delivery to the colon.
Eur. J. Pharm. Biopharm. 47, 6171
Salama, N.N. et al. (2004) The effect of DeltaG
on the transport and oral absorption of
macromolecules. J. Pharm. Sci. 93, 13101319
Marathe, P.H. et al. (2000) Effect of altered
gastric emptying and gastrointestinal motility
on metformin absorption. Br. J. Clin. Pharmacol.
50, 325332
Singh, B.N. (1999) Effects of food on clinical
pharmacokinetics. Clin.Pharmacokinet. 37,
213255
Lin, H.C. et al. (2003) Slowing of intestinal
transit by fat or peptide YY depends on betaadrenergic pathway. Am. J. Physiol. Gastrointest.
Liver Physiol. 285, G1310G1316
Van Citters, G.W. and Lin, H.C. (1999) The ileal
brake: a fifteen-year progress report. Curr.
Gastroenterol. Rep. 1, 404409
Dobson, C.L. et al. (2002) The effect of ileal
brake activators on the oral bioavailability of
atenolol in man. Int. J. Pharm. 248, 6170
20 Kroening, K.D. et al. (2003) Guanosine 3,5cyclic monophosphate: a tapeworm-secreted
signal molecule communicating with the rat
hosts small intestine. J. Parasitol. 89, 11361141
21 Mathias, J.R. et al. (1982) Escherichia coli heatstable toxin: its effect on motility of the small
intestine. Am. J. Physiol. 242, G360G363
22 Cleary, J. et al. (2004) Enteropathogenic
Escherichia coli (EPEC) adhesion to intestinal
epithelial cells: role of bundle-forming pili
(BFP), EspA filaments and intimin. Microbiology
150, 527538
23 Caston, A.J. et al. (1990) The potential of
fimbrial proteins for delaying intestinal transit
of oral drug delivery systems. Proc. Intern. Symp.
Control. Rel. Bioact. Mater. 17, 313314
24 Montisci, M.J. et al. (2001) Gastrointestinal
transit and mucoadhesion of colloidal
suspensions of Lycopersicon esculentum L. and
Lotus tetragonolobus lectin-PLA microsphere
conjugates in rats. Pharm. Res. 18, 829837
25 Jordon, D.E. (1990) Gastroretention in
controlled drug delivery. In Bioadhesion
Possibilities and Future Trends, (Gurney, R. and
Junginger, H.E., eds), pp. 165176,
Wissenschaftliche Verlag
26 He, P. et al. (1999) Chitosan microspheres
prepared by spray drying. Int. J. Pharm. 187, 5365
27 Takishima, J. et al. (2002) Prolonged intestinal
absorption of cephradine with chitosan-coated
ethylcellulose microparticles in rats. Biol. Pharm.
Bull. 25, 14981502
28 Shimoda, J. et al. (2001) Bioadhesive
characteristics of chitosan microspheres to the
29
30
31
32
33
34
mucosa of rat small intestine. Drug Dev. Ind.
Pharm. 27, 567576
Akiyama, Y. et al. (1998) Evaluation of oral
mucoadhesive microspheres in man on the
basis of the pharmacokinetics of furosemide
and riboflavin, compounds with limited
gastrointestinal absorption sites. J. Pharm.
Pharmacol. 50, 159166
Brown, J. et al. (1998) What is the gastrointestinal
transit of very small particles in humans? Proc.
Int.Symp.Control.Rel.Bioact.Mater. 25, 126127
Polnok, A. et al. (2004) In vitro evaluation of
intestinal absorption of desmopressin using
drug-delivery systems based on superporous
hydrogels. Int. J. Pharm. 269, 303310
Dorkoosh, F.A. et al. (2002) Intestinal
absorption of human insulin in pigs using
delivery systems based on superporous hydrogel
polymers. Int. J. Pharm. 247, 4755
Davis, S.S. et al. (1987) Gastrointestinal transit
of controlled release pellet formulation of
tiaprofenic acid and the effect of food. Int.
J. Pharm. 35, 253258
Hou, S.Y. et al. (2003) Gastric retentive dosage
35
36
37
38
39
40
forms: a review. Crit. Rev. Ther. Drug Carrier Syst.
20, 459497
Reddy, L.H. and Murthy, R.S. (2002) Floating
dosage systems in drug delivery. Crit. Rev. Ther.
Drug Carrier Syst. 19, 553585
Burton, S. et al. (1995) Intragastric distribution
of ion-exchange resins: a drug delivery system
for the topical treatment of the gastric mucosa.
J. Pharm. Pharmacol. 47, 901906
Sakkinen, M. et al. (2004) Gamma scintigraphic
evaluation of the fate of microcrystalline
chitosan granules in human stomach. Eur.
J. Pharm. Biopharm. 57, 133143
Torrado, S. et al. (2004) Chitosan-poly(acrylic)
acid polyionic complex: in vivo study to
demonstrate prolonged gastric retention.
Biomaterials 25, 917923
Chen, J. et al. (2000) Gastric retention
properties of superporous hydrogel composites.
J. Control. Release 64, 3951
Wilding, I.W. et al. (1993) Gastrointestinal
transit of a matrix tablet formulation:
Comparison of canine and human data.
Int. J. Pharm. 94, 235238
41 Davis, S.S. et al. (2001) Gastrointestinal transit
of dosage forms in the pig. J. Pharm. Pharmacol.
53, 3339
42 Klausner, E.A. et al. (2003) Novel levodopa
gastroretentive dosage form: in vivo evaluation
in dogs. J. Control. Release 88, 117126
43 Klausner, E.A. et al. (2003) Furosemide
pharmacokinetics and pharmacodynamics
following gastroretentive dosage form
administration to healthy volunteers. J. Clin.
Pharmacol. 43, 711720
44 Klausner, E.A. et al. (2003) Novel gastroretentive
dosage forms: evaluation of gastroretentivity
and its effect on levodopa absorption in
humans. Pharm. Res. 20, 14661473
45 Martin, N.E. et al. (2003) Pharmacoscintigraphic
assessment of the regional drug absorption of
the dual angiotensin-converting
enzyme/neutral endopeptidase inhibitor,
M100240, in healthy volunteers. J. Clin.
Pharmacol. 43, 529538
46 Wilding, I.R. et al. (2001) The role of
-scintigraphy in oral drug delivery. Advan. Drug
Deliv. Rev. 46, 103124
Related articles in other Elsevier journals
Predicting the intestinal absorption potential of hits and leads
Hmlinen, M.D. and Frostell-Karlsson, A. (2004) Drug Discov.Today: Technologies 1, 397405
Formulation design: new drugs from old
Crowley, P.J. and Martini, L.G. (2004) Drug Discov.Today: Therapeutic Strategies 1, 537542
Intestinal solute carriers: an overview of trends and strategies for improving oral drug absorption
Steffansen, B. et al. (2004) Eur. J. Pharm. Sci. 21, 316
Application of formulation technologies in lead candidate selection and optimization
Chaubal, M.V. (2004) Drug Discov.Today 9, 603609
Localisation of drug permeability along the rat small intestine, using markers of the paracellular, transcellular
and some transporter routes
Lacombe, O. et al. (2004) Eur. J. Pharm. Sci. 23, 385391
www.drugdiscoverytoday.com
257
Reviews KEYNOTE REVIEW
REVIEWS
DDT Volume 10, Number 4 February 2005
You might also like
- Diet-Microbe Interactions in the Gut: Effects on Human Health and DiseaseFrom EverandDiet-Microbe Interactions in the Gut: Effects on Human Health and DiseaseKieran TuohyRating: 4.5 out of 5 stars4.5/5 (2)
- Gastroretentive Drug Delivery SystemDocument33 pagesGastroretentive Drug Delivery SystemSaid Muhammad WazirNo ratings yet
- Floating drug delivery: A potential alternative to conventional therapyDocument11 pagesFloating drug delivery: A potential alternative to conventional therapyonovNo ratings yet
- In Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsDocument29 pagesIn Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsAnton SikorskyiNo ratings yet
- Gastro Retentive Drug Delivery SystemDocument10 pagesGastro Retentive Drug Delivery SystemKrunal SamejaNo ratings yet
- RJPBCS April June2013 42 1819 1827.Document10 pagesRJPBCS April June2013 42 1819 1827.sadafNo ratings yet
- A Brief Review On Floating Bilayer Tablet As A Convenient Gastroretentive Drug Delivery SystemDocument11 pagesA Brief Review On Floating Bilayer Tablet As A Convenient Gastroretentive Drug Delivery SystemPh SamerNo ratings yet
- GRDDSDocument31 pagesGRDDSMuhammad Azam TahirNo ratings yet
- CoatingDocument105 pagesCoatingFaress RabiNo ratings yet
- Akash ProjectDocument14 pagesAkash Projectvijay860766No ratings yet
- Syahri Septiana RevisiDocument15 pagesSyahri Septiana RevisiSyahri SeptianaNo ratings yet
- Grdds ReviewDocument33 pagesGrdds ReviewvaibhavbpatelNo ratings yet
- Pharmaceutics 11 00095Document24 pagesPharmaceutics 11 00095fruitsbasketNo ratings yet
- Chapter 1 IntroductionDocument16 pagesChapter 1 IntroductionSandeepNo ratings yet
- Dapu EudragitDocument23 pagesDapu EudragitYohanesMarioPutraKitaNo ratings yet
- 363 PDF PDFDocument7 pages363 PDF PDFEko Setyo BudiNo ratings yet
- Colon Targeted Drug Delivery SystemsDocument14 pagesColon Targeted Drug Delivery SystemsGajendra GowdaNo ratings yet
- JURNALDocument12 pagesJURNAL19 095 Gina Nafsiah PutriNo ratings yet
- Floating Effervescent Tablets A ReviewDocument6 pagesFloating Effervescent Tablets A ReviewsherepunjabNo ratings yet
- Physiological Modeling of The Small Intestine in Drug AbsorptionDocument30 pagesPhysiological Modeling of The Small Intestine in Drug AbsorptionHussain Ali MurtazaNo ratings yet
- Ceutics CAT 2Document9 pagesCeutics CAT 2Ria KitlerNo ratings yet
- GSRTDocument9 pagesGSRTRajani D'souzaNo ratings yet
- GRDDS 2021Document94 pagesGRDDS 2021Shubh AgarwalNo ratings yet
- A Review On Current Approaches in Gastro Retentive Drug Delivery SystemDocument18 pagesA Review On Current Approaches in Gastro Retentive Drug Delivery SystemAreerietinqitink Onenkonenk TazqimaninaaNo ratings yet
- Floating Tablets and Its PolymersDocument9 pagesFloating Tablets and Its PolymersN. IndupriyaNo ratings yet
- Advance Pharmaceutics Topic: Floating Drug Delivery System Group No. 10Document9 pagesAdvance Pharmaceutics Topic: Floating Drug Delivery System Group No. 10Noor ChwdriiNo ratings yet
- Biopharmaceutics and Clinical PharmacokineticsDocument302 pagesBiopharmaceutics and Clinical PharmacokineticsBalisa MosisaNo ratings yet
- 09 - Chapter 1Document47 pages09 - Chapter 1gritty gallantNo ratings yet
- Coarting Materials Used in Pharmaceutical FormulationsDocument105 pagesCoarting Materials Used in Pharmaceutical FormulationsJeanleaf0929No ratings yet
- 12.floating NanoparticlesDocument5 pages12.floating NanoparticlesBaru Chandrasekhar RaoNo ratings yet
- Gastroretentive floating and mucoadhesive drug delivery systems insights and applicationsDocument8 pagesGastroretentive floating and mucoadhesive drug delivery systems insights and applicationsdian oktavianiNo ratings yet
- Colon Targeted Drug Delivery System: Dr. Kunal N. Patel Associate Professor SSSPC, ZundalDocument52 pagesColon Targeted Drug Delivery System: Dr. Kunal N. Patel Associate Professor SSSPC, ZundalHely PatelNo ratings yet
- Gastrointestinal Mucoadhesive Drug Delivery System: A ReviewDocument6 pagesGastrointestinal Mucoadhesive Drug Delivery System: A Reviewcool121086No ratings yet
- Rectal SuppositoriesDocument6 pagesRectal SuppositoriesLinh PhamNo ratings yet
- Design and Application of Oral Colon Administration SystemDocument8 pagesDesign and Application of Oral Colon Administration SystemditaNo ratings yet
- Gastroretentive Drug Delivery SystemDocument26 pagesGastroretentive Drug Delivery SystemQA Dhq OkaraNo ratings yet
- Floating Drug Delivery System-: An Approach To Prolong Gastric RetentionDocument29 pagesFloating Drug Delivery System-: An Approach To Prolong Gastric Retentionapi-19985983No ratings yet
- Unit 6 Targeted Drug DeliveryDocument42 pagesUnit 6 Targeted Drug Deliveryabdullah2020100% (1)
- General Pharmacology ExerciseDocument7 pagesGeneral Pharmacology ExerciseElijah MtishibeNo ratings yet
- Gastroretentive Dosage Forms: A Review With Special Emphasis On Floating Drug Delivery SystemsDocument15 pagesGastroretentive Dosage Forms: A Review With Special Emphasis On Floating Drug Delivery Systemstsamrotul layyinahNo ratings yet
- A Review On Delivery of Drugs Used For Acid Reflux Treatment Using Buccal DrugDocument18 pagesA Review On Delivery of Drugs Used For Acid Reflux Treatment Using Buccal DrugAnjali Sahil MittalNo ratings yet
- Novel Pharmaceutical Approaches For Colon-Specific Drug Delivery: An OverviewDocument9 pagesNovel Pharmaceutical Approaches For Colon-Specific Drug Delivery: An OverviewMud MuddNo ratings yet
- 23 Ref For FloatingDocument9 pages23 Ref For FloatingLakshmiNo ratings yet
- Drug Delivery On Rectal Absorption: Suppositories: Review ArticleDocument7 pagesDrug Delivery On Rectal Absorption: Suppositories: Review ArticleNindah IkaNo ratings yet
- Floating Tablets - Final With CorrectionDocument70 pagesFloating Tablets - Final With Correctionkharemix100% (1)
- Introduction to pharmacology 2020-2021Document40 pagesIntroduction to pharmacology 2020-2021jamila ilNo ratings yet
- Australian Prescriber (1988) Bioavailability and First Past ClearanceDocument3 pagesAustralian Prescriber (1988) Bioavailability and First Past Clearance1234chocoNo ratings yet
- Perspectives of Biodegradable Natural Polysaccharides For Site-Specific Drug Delivery To The ColonDocument43 pagesPerspectives of Biodegradable Natural Polysaccharides For Site-Specific Drug Delivery To The ColonIndah PideNo ratings yet
- ISHAN 1 (1)Document75 pagesISHAN 1 (1)Arshdeep SinghNo ratings yet
- Pharmaceutical Approaches To Colon Targeted Drug Delivery SystemsDocument34 pagesPharmaceutical Approaches To Colon Targeted Drug Delivery SystemsKumar GalipellyNo ratings yet
- 698 PDF PDFDocument8 pages698 PDF PDFMuh Indra SudirjaNo ratings yet
- Gastroretentive drug delivery systemsDocument7 pagesGastroretentive drug delivery systemsDeslina Setria MitaNo ratings yet
- 1.1 Novel Drug Delivery System: Chapter-1Document32 pages1.1 Novel Drug Delivery System: Chapter-1Raja AbhilashNo ratings yet
- Commercial Challenges and Emerging Trends in Oral Delivery of Peptide and Protein Drugs3Document15 pagesCommercial Challenges and Emerging Trends in Oral Delivery of Peptide and Protein Drugs3Arvind SharmaNo ratings yet
- Jurnal FarmakokinetikDocument15 pagesJurnal FarmakokinetikVebry AeyniNo ratings yet
- A Review On Gastroretentive Drug Delivery SystemDocument10 pagesA Review On Gastroretentive Drug Delivery Systemharshita SinghNo ratings yet
- Teaching Note - GITractDocument7 pagesTeaching Note - GITractArdiellaputriNo ratings yet
- Overview of Factors Affecting Oral Drug AbsorptionDocument11 pagesOverview of Factors Affecting Oral Drug Absorptionmahveen balochNo ratings yet
- Gastroretentive-Drug-Delivery-System L-13 L-59 L-67 L-01 L-46Document9 pagesGastroretentive-Drug-Delivery-System L-13 L-59 L-67 L-01 L-46Bilal AsgharNo ratings yet
- Unit 4 Factors Affecting Drug AbsorptionDocument53 pagesUnit 4 Factors Affecting Drug Absorptiondiadiaida100% (1)
- Bhattacharjee Et Al-2018-Advanced MaterialsDocument7 pagesBhattacharjee Et Al-2018-Advanced MaterialsIslam HelazaNo ratings yet
- Average and Standard Deviation of The Error Function For Random Genetic Codes With Standard Stop CodonsDocument16 pagesAverage and Standard Deviation of The Error Function For Random Genetic Codes With Standard Stop CodonsFilip IlievskiNo ratings yet
- Up-Regulation of Luciferase Gene Expression With Antisense Oligonucleotides: Implications and Applications in Functional Assay DevelopmentDocument5 pagesUp-Regulation of Luciferase Gene Expression With Antisense Oligonucleotides: Implications and Applications in Functional Assay DevelopmentFilip IlievskiNo ratings yet
- Seminar on absorption rate constantsDocument42 pagesSeminar on absorption rate constantsFilip Ilievski50% (2)
- Academic Internships Event - Saturday 24th November 2018Document2 pagesAcademic Internships Event - Saturday 24th November 2018Filip IlievskiNo ratings yet
- Maeda 2001Document17 pagesMaeda 2001Filip IlievskiNo ratings yet
- Lipid-Based Transfection Reagents Exhibit Cryo-InducedDocument11 pagesLipid-Based Transfection Reagents Exhibit Cryo-InducedFilip IlievskiNo ratings yet
- Ribosome Collisions in Bacteria Promote Ribosome Rescue by Triggering Mrna Cleavage by SMRBDocument26 pagesRibosome Collisions in Bacteria Promote Ribosome Rescue by Triggering Mrna Cleavage by SMRBFilip IlievskiNo ratings yet
- Optimization of Polyplex Formation Between DNA Oligonucleotide and Poly (-Lysine) : Experimental Study and Modeling ApproachDocument15 pagesOptimization of Polyplex Formation Between DNA Oligonucleotide and Poly (-Lysine) : Experimental Study and Modeling ApproachFilip IlievskiNo ratings yet
- Bacteria As Gene Carrier VectorsDocument12 pagesBacteria As Gene Carrier VectorsFilip IlievskiNo ratings yet
- Art. Application of The BiopharmaceuticalDocument5 pagesArt. Application of The BiopharmaceuticalDeisy SantodomingoNo ratings yet
- 10.1038s41551 017 0137 2Document15 pages10.1038s41551 017 0137 2Filip IlievskiNo ratings yet
- Review: Graeme J Hankey, John W EikelboomDocument12 pagesReview: Graeme J Hankey, John W EikelboomFilip IlievskiNo ratings yet
- Microsponges QBDDocument15 pagesMicrosponges QBDFilip Ilievski100% (1)
- LiposomesDocument9 pagesLiposomesFilip IlievskiNo ratings yet
- HVA VaccineDocument10 pagesHVA VaccineFilip IlievskiNo ratings yet
- Depo FoamDocument12 pagesDepo FoamFilip IlievskiNo ratings yet
- ProjectARS PDF 449Document16 pagesProjectARS PDF 449Filip IlievskiNo ratings yet
- Encyclopedia of Pharmaceutical Technology, Third EditionDocument23 pagesEncyclopedia of Pharmaceutical Technology, Third EditionFilip IlievskiNo ratings yet
- Topic 9 - SuppositoriesDocument21 pagesTopic 9 - SuppositoriesFilip IlievskiNo ratings yet
- Analiticka PraktikumDocument24 pagesAnaliticka PraktikumFilip IlievskiNo ratings yet
- Magistri (Elektroliza) NovaDocument11 pagesMagistri (Elektroliza) NovaFilip IlievskiNo ratings yet
- Cae Reading Part 1Document6 pagesCae Reading Part 1AndChrissNo ratings yet
- Predavanje 10 Novo (F-Elementi)Document17 pagesPredavanje 10 Novo (F-Elementi)Filip IlievskiNo ratings yet
- BayesDocument9 pagesBayesSiddhesh ParabNo ratings yet
- Drugs Acting On Blood and Blood Forming OrgansDocument42 pagesDrugs Acting On Blood and Blood Forming OrgansNazmul NabilNo ratings yet
- Essential Health Services and PlansDocument4 pagesEssential Health Services and Planszahara mahalNo ratings yet
- First International congress on clinical Hypnosis & Related Sciences programDocument91 pagesFirst International congress on clinical Hypnosis & Related Sciences programGolnaz BaghdadiNo ratings yet
- Dhatupaushtik ChurnaDocument6 pagesDhatupaushtik ChurnaShoeb MirzaNo ratings yet
- Mood Disorders - Bipolar Disorder: Professor Macdonald, MSN, RNDocument47 pagesMood Disorders - Bipolar Disorder: Professor Macdonald, MSN, RNmaha abdallahNo ratings yet
- Pornography Statistics: 250+ Facts, Quotes, and Statistics About Pornography Use (2013 Edition)Document33 pagesPornography Statistics: 250+ Facts, Quotes, and Statistics About Pornography Use (2013 Edition)Zinc MarquezNo ratings yet
- Superannuation Benefits SessionDocument49 pagesSuperannuation Benefits SessionfunshareNo ratings yet
- Plant Based Diet A Way To Healthier Life: September 2020Document9 pagesPlant Based Diet A Way To Healthier Life: September 2020MihryazdNo ratings yet
- AcupunctureDocument15 pagesAcupuncturezextorcNo ratings yet
- Biochem SGD 3Document4 pagesBiochem SGD 3Hemanth KokaNo ratings yet
- Pain Scales and Assessment UnhasDocument93 pagesPain Scales and Assessment Unhashaphahap0% (1)
- ZZZZZZZZZZZZZZDocument8 pagesZZZZZZZZZZZZZZchloramphenicolNo ratings yet
- Borderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergDocument23 pagesBorderline Personality Disorder, Bipolar Disorder, Depression, Attention ... Narcissistic Personality Disorder, Diferential Diagnostic, KernbergjuaromerNo ratings yet
- Tumors of The Pituitary Gland: John W. Gittinger, JRDocument4 pagesTumors of The Pituitary Gland: John W. Gittinger, JRBilly UntuNo ratings yet
- Adhd SD 550 Graphic Organizer 3 PDFDocument4 pagesAdhd SD 550 Graphic Organizer 3 PDFapi-534368950No ratings yet
- Fungi Classes ChartDocument1 pageFungi Classes ChartManav SinghNo ratings yet
- Non-Profit Organization Funds Gregory Grabovoi TeachingsDocument95 pagesNon-Profit Organization Funds Gregory Grabovoi Teachingsssss87va93% (27)
- AllergiesDocument11 pagesAllergiesAficionadoNo ratings yet
- Vitamin B12 Deficiency in Type 2 Diabetics on MetforminDocument5 pagesVitamin B12 Deficiency in Type 2 Diabetics on MetforminMuhammad ZubairNo ratings yet
- Envis Newsletter April 2014Document16 pagesEnvis Newsletter April 2014Mikel MillerNo ratings yet
- Physical Education Mcqs For All Govt ExamDocument108 pagesPhysical Education Mcqs For All Govt Examrabiaghafar855No ratings yet
- Baterial & Fungal Corneal UlcersDocument28 pagesBaterial & Fungal Corneal UlcersVasishta NadellaNo ratings yet
- GASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXDocument11 pagesGASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXRhealyn LegaspiNo ratings yet
- Severe Acute Respiratory Syndrome Coronavirus 2Document31 pagesSevere Acute Respiratory Syndrome Coronavirus 2Ian VillacrusisNo ratings yet
- Sas 1# - CHNDocument16 pagesSas 1# - CHNZymer Lee Perez AbasoloNo ratings yet
- Lesson 1: Health and Skill Related FitnessDocument2 pagesLesson 1: Health and Skill Related FitnessCrhystal Joy ReginioNo ratings yet
- MidtermDocument22 pagesMidtermEmvie Loyd Pagunsan-ItableNo ratings yet
- Common Medical Surgical MedicationsDocument36 pagesCommon Medical Surgical MedicationsAshley Etheredge100% (1)
- 2023061-21 Seminar On The Development and Application of Mobile PaymentDocument3 pages2023061-21 Seminar On The Development and Application of Mobile PaymentMunkhuu NasaaNo ratings yet
- Govorno Jezicki Poremecaji Razvojnog Doba Speech and Language Disorders at Developmental AgeDocument259 pagesGovorno Jezicki Poremecaji Razvojnog Doba Speech and Language Disorders at Developmental AgeVeljko BorovinaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)