Professional Documents
Culture Documents
3750 Full
Uploaded by
ferOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3750 Full
Uploaded by
ferCopyright:
Available Formats
JOURNAL OF CLINICAL MICROBIOLOGY, Nov. 2011, p.
37503755
0095-1137/11/$12.00 doi:10.1128/JCM.01186-11
Copyright 2011, American Society for Microbiology. All Rights Reserved.
Vol. 49, No. 11
Viral-Bacterial Interactions and Risk of Acute Otitis Media
Complicating Upper Respiratory Tract Infection
Melinda M. Pettigrew,1* Janneane F. Gent,1 Richard B. Pyles,2 Aaron L. Miller,2
Johanna Nokso-Koivisto,2 and Tasnee Chonmaitree2
Yale School of Public Health, Yale School of Medicine, New Haven, Connecticut,1 and
University of Texas Medical Branch, Galveston, Texas2
Received 15 June 2011/Returned for modification 1 August 2011/Accepted 29 August 2011
pathogens that colonize the nasopharynx (28). Epidemiologic
studies have not consistently identified interactions between
specific viruses and bacteria and increased risk of AOM (2, 21,
22). Inconsistent results may be due to differences in study
design and methods used to detect viruses and bacteria. For
example, the risk of AOM complicating URI due to specific
viruses was most strongly associated with viruses detected by
culture as opposed to molecular methods, perhaps because
culture captures infections associated with higher viral loads
(10).
The understanding of relationships between viruses, bacteria, and AOM risk is changing as new viruses are discovered
and new methods are developed to quantify pathogen loads.
Human bocavirus (hBOV) is a parvovirus that was first described in 2005 (1). Several studies have detected hBOV in
nasal samples from children with URI and in middle ear fluid
samples from children with AOM (5, 14, 29, 30). However, the
role of hBOV as a causative URI pathogen has been debated
(3, 23, 25). Human metapneumovirus (hMPV), described in
2001 (32), also has been isolated from middle ear fluid samples
from children with AOM (29, 31). Retrospective analyses indicated that more than half of URI episodes due to hMPV
were complicated by AOM (35). However, the risk of AOM
due to hMPV did not differ significantly from that of other
respiratory viruses, such as RSV (35). Additional studies are
needed to accurately determine the risk of AOM complicating
URI due to these relatively new viruses.
The prevalence of AOM has declined slightly during the past
decade due in part to the use of pneumococcal conjugate
Acute otitis media (AOM) is one of the most common
diseases seen in pediatric practice and is a major reason for
antibiotic use in the United States (15, 33, 37). AOM pathogenesis involves complex interactions between bacteria, viruses, and the host inflammatory response. Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis
colonize the nasopharynx and are the three most frequent
AOM pathogens (9). While AOM is often considered a bacterial infection, its pathogenesis involves complex interactions
among viruses and bacteria (4). The majority of AOM episodes
occur as complications of viral upper respiratory tract infection
(URI) (10, 17). Viral URI increases the risk of bacterial AOM
by promoting the replication of bacteria and increasing inflammation in the nasopharynx and Eustachian tube, which subsequently facilitates bacterial entry into the middle ear space (4).
Respiratory viruses can coinfect the middle ear with bacterial
AOM pathogens and have been identified as the sole causative
agent of AOM (19, 29).
Viral URI is a major risk factor for AOM; however, specific
viruses differ in their propensity to cause disease (10, 21).
Respiratory syncytial virus (RSV) has been identified as being
strongly associated with AOM (10, 21, 27). The risk of AOM
differs depending on the number and type of bacterial AOM
* Corresponding author. Mailing address: Yale University School of
Public Health, 60 College Street, New Haven, CT 06520-8034. Phone:
(203) 785-5220. Fax: (203) 785-6130. E-mail: melinda.pettigrew@yale
.edu.
Published ahead of print on 7 September 2011.
3750
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
Acute otitis media (AOM) is a common complication of upper respiratory tract infection whose pathogenesis
involves both viruses and bacteria. We examined risks of acute otitis media associated with specific combinations of respiratory viruses and acute otitis media bacterial pathogens. Data were from a prospective study of
children ages 6 to 36 months and included viral and bacterial culture and quantitative PCR for respiratory
syncytial virus (RSV), human bocavirus, and human metapneumovirus. Repeated-measure logistic regression
was used to assess the relationship between specific viruses, bacteria, and the risk of acute otitis media
complicating upper respiratory tract infection. In unadjusted analyses of data from 194 children, adenovirus,
bocavirus, Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis were significantly associated with AOM (P < 0.05 by 2 test). Children with high respiratory syncytial virus loads (>3.16 107
copies/ml) experienced increased acute otitis media risk. Higher viral loads of bocavirus and metapneumovirus
were not significantly associated with acute otitis media. In adjusted models controlling for the presence of key
viruses, bacteria, and acute otitis media risk factors, acute otitis media risk was independently associated with
high RSV viral load with Streptococcus pneumoniae (odds ratio [OR], 4.40; 95% confidence interval [CI], 1.90
and 10.19) and Haemophilus influenzae (OR, 2.04; 95% CI, 1.38 and 3.02). The risk was higher for the presence
of bocavirus and H. influenzae together (OR, 3.61; 95% CI, 1.90 and 6.86). Acute otitis media risk differs by the
specific viruses and bacteria involved. Acute otitis media prevention efforts should consider methods for
reducing infections caused by respiratory syncytial virus, bocavirus, and adenovirus in addition to acute otitis
media bacterial pathogens.
VOL. 49, 2011
VIRAL-BACTERIAL INTERACTIONS AND AOM COMPLICATING URI
vaccines (33, 37). AOM is a polymicrobial disease; further
advances in AOM prevention will depend upon the identification of critical polymicrobial interactions that influence AOM
risk to prioritize bacterial and viral targets for intervention
strategies. We tested the hypothesis that specific combinations
of respiratory viruses and bacteria were associated with an
increased risk for AOM. Data are from a prospective cohort
study of healthy children monitored for 1 year for AOM complicating URI (10). Culture-based data were used to assess
infection by respiratory viruses and bacterial colonization. In
addition, newly developed quantitative PCR (qPCR) assays
were used to assess the relationship between viral loads of
RSV, hBOV, and hMPV and the risk of AOM.
Study design and subjects. Data are from a prospective cohort study of AOM
complicating symptomatic URI (10). A detailed study description has been
provided elsewhere (10, 28). Subjects were enrolled and specimens were collected at the University of Texas Medical Branch (UTMB) at Galveston. The
study was approved by the UTMB institutional review board. Parents provided
written informed consent for all subjects. Healthy children living in Galveston,
between 6 months to 3 years of age, were enrolled between January 2003 and
March 2007 and monitored for 1 year. Children with chronic medical problems
or anatomical or physiological defects of the ear or nasopharynx were excluded.
At enrollment, demographic and AOM risk factor data were collected (e.g.,
antibiotic use, duration of breastfeeding, daycare attendance, and exposure to
environmental tobacco smoke). Children were brought to the study office for a
sick visit at the onset of URI symptoms (nasal congestion, rhinorrhea, cough,
sore throat, or fever). At each study visit, data were recorded on URI symptoms
and otoscopic findings. Within a few days of the sick visit, children had a repeat
study visit to evaluate their middle ear status. Criteria for AOM diagnosis
included the acute onset of symptoms (fever, irritability, or earache), signs of
tympanic membrane inflammation, and the presence of fluid documented by
pneumatic otoscopy and/or tympanometry. AOM episodes occurring within a
month of URI onset were considered a complication of URI. In addition to
parental reports of URI, study personnel called parents twice monthly for current URI symptoms and missed URI or AOM episodes. Medical records were
reviewed when children completed the study to identify missed URI and AOM
episodes.
Two hundred ninety-four children were enrolled in the original study (10).
Included in these analyses are data from 194 children who were seen by the study
group at the onset of URI, were monitored for AOM, and had the following
microbiologic data available: bacterial culture, viral culture, and quantitative
PCR (qPCR) (n 640 episodes). Analyses were restricted to specimens collected during the first study visit of each URI episode.
Viral and bacterial specimens. Nasopharyngeal secretion specimens were collected for viral studies, and nasopharyngeal swabs were collected for bacterial
culture as previously described (10, 28). Viral and bacterial cultures were performed by standard methods (10, 28). qPCR was performed on thawed frozen
specimens as described below.
Nucleic acids were extracted from nasopharyngeal specimens using a Tecan
Evo (Mannedorf, Switzerland) automated liquid handler within the Assay Development Service Division of the Galveston National Laboratory, followed by
processing using MagMAX Total Nucleic Acid isolation kits (Ambion/Applied
Biosystems, Austin, TX). For the quantification of hMPV and RSV, cDNA was
synthesized using the iScript synthesis kit (Bio-Rad, Hercules, CA). A duplex
qPCR, with primers amplifying RSV and hMPV targets, was completed on
cDNA (6). hBOV DNA was quantified using the methods of Lu et al. (24).
Separate qPCRs for human glyceraldehyde 3-phosphate dehydrogenase assessed
sample quality (7). For all targets, starting quantity values were extrapolated
from standard curves established by parallel amplification of known amounts of
cloned PCR targets. The viral load was calculated as copies/ml of the original
specimen considering all sample dilutions.
Statistical methods. Statistical analyses were conducted using SAS version 9.2
(Cary, NC). Unadjusted associations between AOM and other variables were
examined with 2 analyses. Since each of the 194 subjects could contribute data
from multiple separate URI episodes, we examined patterns of virus infection
and bacterial colonization using repeated-measure logistic regression with generalized estimating equations (GEE) and specified an autoregressive correlation
TABLE 1. Characteristics of subjects (n 194) and acute otitis
media diagnosis
Characteristic
Age at enrollment, mo
612
1218
1824
2436
Gender
Female
Male
Race
White
Black
Hispanic
Other
Day care
No
Yes
Breastfed for 3 months
No
Yes
Environmental tobacco
smoke exposure
No
Yes
Antibiotic use within 7
days of URI
None
Any
a
b
Total no.
(%)
No. (%)
diagnosed with
AOM (anya)
84 (43)
55 (28)
28 (14)
27 (14)
59 (70)
31 (56)
17 (61)
15 (56)
95 (49)
99 (51)
58 (61)
64 (65)
39 (20)
56 (29)
83 (43)
16 (8)
25 (64)
32 (57)
51 (61)
14 (88)
133 (69)
61 (31)
85 (64)
37 (61)
127 (66)
67 (34)
83 (65)
39 (58)
P valueb
0.30
0.60
0.17
0.66
0.33
0.37
141 (73)
53 (27)
86 (61)
36 (68)
0.003
171 (88)
23 (12)
101 (59)
21 (91)
One or more acute otitis media diagnoses per subject.
P values from 2 tests. Significant P values (0.05) are shown in boldface.
structure (AR1). Results of qPCR for RSV, hBOV, and hMPV were categorized
into a four-level variable (no, low, medium, or high copies/ml) prior to analysis
to determine dose-response relationships to AOM. Boundaries of viral load
categories were determined by dividing the distribution of copies/ml (excluding
0 copies/ml) into thirds. Separate logistic regression analyses of each of the
viruses identified by culture were used to determine which were associated with
an increased risk of AOM and should be included in final models. Separate
analyses also were performed to examine potential interactions between each of
the viruses identified by qPCR (RSV, hBOV, and hMPV) and AOM bacterial
pathogens (S. pneumoniae, H. influenzae, and M. catarrhalis). The final model
included variables representing coinfections between RSV and S. pneumoniae
(as a four-level categorical variable representing the presence or absence of a
high viral load of RSV and S. pneumoniae) and hBOV and H. influenzae (as a
four-level categorical variable representing the presence or absence of each) in
addition to the presence or absence of hMPV, adenovirus, and M. catarrhalis. All
models were adjusted for the following AOM risk-related covariates: age of the
child at the time of nasopharyngeal specimen collection, ethnicity, daycare attendance, breastfed for 3 months, exposure to environmental tobacco smoke,
and antibiotic use within the previous 7 days.
RESULTS
The subset of 194 children available for this study did not
differ significantly from the larger original enrollment (n
294) by age, gender, or race (P 0.10, 0.99, and 0.52, respectively; 2 test). Participant characteristics are in Table 1. Mean
age at enrollment was 14.2 months (standard deviations [SD],
7.6). The children experienced a mean of 3.3 (SD, 2.7) URI
episodes (range, 1 to 15) and 1.2 diagnoses of AOM (range, 0
to 7). AOM episodes occurred within 1 and 17 days of URI
onset; the mean time between the onset of URI and the development of AOM symptoms was 5.6 days (SD, 3.2). The
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
MATERIALS AND METHODS
3751
3752
PETTIGREW ET AL.
J. CLIN. MICROBIOL.
TABLE 2. Distribution of subjects by number of URI episodesa
No. of
URI episodes
No. (%) of
subjects
1 ...............................................................................................62 (32)
2 ...............................................................................................41 (21)
34 ...........................................................................................42 (21)
5............................................................................................49 (25)
a
A total of 194 subjects were examined.
Virus/bacteria
No. (%) of
specimens
No. (%) of
specimens with
AOM diagnosis
Total
640
239 (37)
Adenovirus by culture
Absent
Present
619 (97)
21 (3)
226 (36)
13 (62)
548 (86)
92 (14)
200 (36)
39 (42)
483 (75)
157 (25)
170 (35)
69 (44)
596 (93)
44 (7)
223 (37)
16 (36)
353 (55)
287 (45)
110 (31)
129 (45)
446 (70)
194 (30)
138 (31)
101 (52)
226 (35)
414 (65)
60 (27)
179 (43)
Virus by PCR
RSV
Absent
Present
hBOV
Absent
Present
hMPV
Absent
Present
Bacteria by culture
S. pneumoniae
Absent
Present
H. influenzae
Absent
Present
M. catarrhalis
Absent
Present
a
P valuea
0.02
0.28
0.05
0.89
0.0003
<0.0001
<0.0001
P values are from 2 tests. Significant P values (0.05) are shown in boldface.
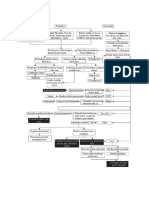
We next evaluated the risk of AOM associated with categories of viral load for RSV, hBOV, and hMPV. The repeatedmeasure logistic regression model included these three viruses
as well as variables representing the presence or absence of
adenovirus and each AOM bacterial pathogen (Table 4). The
model was adjusted for the AOM risk-related covariates. The
boundaries for the viral load categories for each virus are in
the footnote of Table 4. For RSV, there was a threshold effect:
low and intermediate levels of RSV viral load were not associated with AOM any more frequently than the level of no
RSV. However, children with an RSV viral load of greater than
3.16 107 copies/ml experienced a significantly increased risk
of AOM (Table 4). Increasing viral loads of hBOV and hMPV
were not significantly associated with an increased risk of
AOM complicating URI. The presence of adenovirus, H. influenzae, and M. catarrhalis was independently associated with
increased risk of AOM (Table 4). Of the AOM risk-related
covariates, increasing age and having been breastfed for 3
months were associated with decreased risk of AOM. Each 1
month of age increase was associated with a 4% decreased risk
of AOM (OR, 0.96; 95% CI, 0.94 and 0.99), and breastfeeding
was associated with a 40% decreased risk of AOM (OR, 0.60;
95% CI, 0.36 and 0.99). Antimicrobial therapy within the previous 7 days was associated with an increased risk of AOM
complicating URI (OR, 2.65; 95% CI, 1.14 and 6.15).
Repeated-measure logistic regression evaluation of statistical interactions between RSV, hBOV, and hMPV and the
three AOM bacterial pathogens was significant for RSV with S.
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
distribution of URI episodes by child is in Table 2. Approximately 25% of the children contributed 55% of the specimens.
The proportion of children with any AOM diagnoses was
highest among children 6 to 12 months of age and those who
had antibiotics within the 7 days prior to the URI study visit
(Table 1). The proportion of children with at least one AOM
episode did not significantly differ by gender, race, daycare,
breastfeeding history, or environmental tobacco smoke exposure (Table 1). More than 99% (n 635) of the 640 specimens
were collected from study participants who received at least
one dose of the 7-valent pneumococcal conjugate vaccine
(PCV7) at the time of specimen collection.
The following viruses were detected by culture in 640 specimens: rhinovirus, n 33 (5.2%); parainfluenza types 1 to 3,
n 20 (3.1%); adenovirus, n 21 (3.3%); influenza A and B
viruses, n 21 (3.3%); enterovirus, n 14 (2.2%); and RSV,
n 12 (1.9%). Respiratory viruses were not isolated by culture
for 499 (78%) samples. Separate repeated-measure logistic
regression models were used to evaluate the risk of AOM
complicating URI with individual viruses detected by culture.
Adjusted models included each AOM bacterial pathogen and
AOM risk-related covariates. The presence of rhinovirus,
parainfluenza virus, influenza virus, enterovirus, and RSV by
culture were not significantly associated with an increased risk
of AOM (data not shown). These viruses were not considered
in further models. In contrast, adenovirus was significantly
associated with an increased risk of AOM (odds ratio [OR],
2.90; 95% CI, 1.30 and 6.46). The distribution of adenovirus is
in Table 3.
qPCR analyses detected the presence of RSV in 14%,
hBOV in 24%, and hMPV in 7% of specimens (Table 3). Of
the respiratory viruses identified by culture or qPCR, 49% of
the specimens were negative for all viruses, 40% were positive
for one virus, 10.5% were positive for two viruses, and 0.5%
were positive for three respiratory viruses (data not shown). Of
640 specimens, 45, 30, and 65% were positive for S. pneumoniae, H. influenzae, and M. catarrhalis, respectively (Table
3). The presence of hBOV by PCR and adenovirus, S. pneumoniae, H. influenzae, and M. catarrhalis by culture were associated with an AOM diagnosis (P 0.05; 2 test) (Table 3).
Among samples positive by qPCR, the viral load for each
ranged from 3.99 103 to 1.20 1011 copies/ml for RSV,
3.23 103 to 1.73 1012 copies/ml for hBOV, and 2.73 104
to 1.03 1010 copies/ml for hMPV. There was a significant
association between the season of sampling and viral load of
RSV (P 0.0005; 2 test) but not for hBOV (P 0.32) or
hMPV (P 0.13). During June, July, and August, 112 samples
were collected from children with URI. Of these, 11 (9.8%)
specimens were positive for RSV, but none were in the highest
viral load category.
TABLE 3. Unadjusted association of AOM diagnosis with presence
of viruses and bacteria on 640 nasal specimens taken
from 194 subjects
VOL. 49, 2011
VIRAL-BACTERIAL INTERACTIONS AND AOM COMPLICATING URI
TABLE 4. Association between viral load of RSV, hBOV, and
hMPV and risk of AOM complicating URId
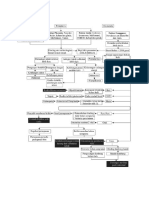
TABLE 5. Polymicrobial interactions and risk of AOM
complicating URIb
OR (95% CI)
Factor(s)
RSVa
None (reference)
Low
Med
High
548 (85.6)
31 (4.8)
30 (4.7)
31 (4.8)
1.00
1.16 (0.65, 2.04)
0.96 (0.42, 2.18)
2.60 (1.30, 5.20)
hBOVb
None (reference)
Low
Med
High
483 (75.5)
51 (8.0)
54 (8.4)
52 (8.1)
hMPVc
None (reference)
Low
Med
High
596 (93.1)
15 (2.3)
15 (2.3)
14 (2.2)
Adenovirus
Absent (reference)
Present
619 (96.7)
21 (3.3)
No. (%) of
samples
OR (95% CI)
High-viral-load RSV and S.
pneumoniae
Neither present (reference)a
S. pneumoniae alone
High-viral-load RSV alone
Both present
345 (53.9)
264 (41.2)
8 (1.2)
23 (3.6)
1.00
1.27 (0.86, 1.86)
2.01 (0.24, 4.77)
4.40 (1.90, 10.19)
1.00
1.00 (0.56, 1.79)
1.50 (0.92, 2.45)
0.97 (0.51, 1.88)
hBOV and H. influenzae
Neither present (reference)
H. influenzae alone
hBOV alone
Both present
346 (54.1)
137 (21.4)
100 (15.6)
57 (8.9)
1.00
2.04 (1.38, 3.02)
0.88 (0.54, 1.43)
3.61 (1.90, 6.86)
1.00
1.48 (0.53, 5.58)
0.75 (0.22, 2.53)
0.43 (0.15, 1.29)
hMPV
Absent (reference)
Present
596 (93.1)
44 (6.9)
1.00
0.81 (0.41, 1.59)
Adenovirus
Absent (reference)
Present
619 (96.7)
21 (3.3)
1.00
3.06 (1.36, 6.89)
M. catarrhalis
Absent (reference)
Present
226 (35.3)
414 (64.7)
1.00
1.85 (1.28, 2.68)
1.00
4.64 (1.42, 7.07)
S. pneumoniae
Absent (reference)
Present
353 (55.2)
287 (44.8)
1.00
1.25 (0.85, 1.84)
H. influenzae
Absent (reference)
Present
446 (69.7)
194 (30.3)
1.00
2.41 (1.66, 3.48)
M. catarrhalis
Absent (reference)
Present
226 (35.3)
414 (64.7)
1.00
1.91 (1.31, 2.78)
a
RSV (copies/ml): none, 0; low, 0 to 1.26 105; med (medium), 1.26 105
to 3.16 107; high, 3.16 107.
b
hBOV (copies/ml): none, 0; low, 0 to 5.01 105; med, 5.01 105 to
2.51 107; high, 2.51 107.
c
hMPV (copies/ml): none, 0; low, 0 to 3.16 106; med, 3.16 106 to
6.31 108; high, 6.31 108.
d
OR and 95% CI are from repeated-measure logistic regression analysis of
640 specimens from 194 subjects. Significant ORs and 95% CIs are in boldface.
The model included viral loads of RSV, hBOV, and hMPV as well as variables
representing the presence or absence of adenovirus, each AOM bacterial pathogen by culture, and AOM risk-related covariates.
pneumoniae (P 0.01) and hBOV with H. influenzae (P
0.003). The model examined the independent risk of AOM
associated with the highest level of RSV viral load and S.
pneumoniae, hBOV, and H. influenzae and the presence of
hMPV, adenovirus, and M. catarrhalis (Table 5). The model
was adjusted for AOM risk-related covariates. S. pneumoniae
had a synergistic relationship with RSV; children whose samples revealed a high viral load of RSV and the presence of S.
pneumoniae experienced a 4-fold increased risk of AOM compared to that of samples with neither high-viral-load RSV nor
S. pneumoniae. Compared to samples with neither H. influenzae nor hBOV, increased risk for AOM complicating URI was
independently associated with H. influenzae (OR, 2.04; 95%
CI, 1.38 and 3.02), and the risk was even higher for hBOV and
H. influenzae together (OR, 3.61; 95% CI, 1.90 and 6.86).
Specimens were collected during the first study visit of each
URI episode and linked to the development of AOM within a
1-month period. Some children may have acquired a new
a
The reference category includes samples where S. pneumoniae was not present and the viral load for RSV was not high (i.e., 3.16 107 copies/ml).
b
OR and 95% CI are from repeated-measure logistic regression analysis of
640 specimens from 194 subjects. Significant ORs and 95% CIs are in boldface.
The model included significant interactions between RSV and S. pneumoniae
and that between human bocavirus hBOV and H. influenzae. hMPV, adenovirus,
M. catarrhalis, and AOM risk covariates also were included in the model.
AOM pathogen between the time of sample collection and the
development of AOM. Of the 239 AOM episodes, 80.3% (n
192) occurred within 7 days of URI onset. Repeated-measure
logistic regression was used to evaluate interactions between
RSV, hBOV, and hMPV and the three AOM bacterial pathogens using data restricted to children who had specimens collected within 7 days of URI onset and diagnoses made within
7 days of URI onset. The associations between viruses, bacteria, and AOM (n 614 specimens) were similar to data presented in Table 5. The significant associations were the following: high viral load of RSV and the presence of S. pneumoniae
(OR, 6.19; 95% CI, 2.47 and 15.49), H. influenzae alone (OR,
1.86; 95% CI, 1.23 and 2.88), hBOV and H. influenzae together
(OR, 3.65; 95% CI, 1.86 and 7.14)], adenovirus (OR, 3.27; 95%
CI, 1.47 and 7.28)], and M. catarrhalis (OR, 1.66; 95% CI, 1.13
and 2.44).
DISCUSSION
Researchers have proposed that combined bacterium-virus
vaccine formulations would have the most significant and longterm impact on AOM (12). Our data suggest that viruses and
bacteria differ in their association with risk of AOM complicating URI. RSV had a synergistic interaction with S. pneumoniae when children experienced higher RSV viral loads.
Since the introduction of PCV7, the proportion of AOM episodes associated with S. pneumoniae vaccine serotypes has
decreased while the proportion with H. influenzae has in-
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
No. (%) of
samples
Factor
3753
3754
PETTIGREW ET AL.
We previously showed that AOM risk was higher in children
with one or more AOM bacterial pathogens in the nasopharynx than in those with no AOM bacterial pathogens (28). The
use of antibiotics prior to URI development could lead to a
reduction of nasopharyngeal colonization with bacterial AOM
pathogens, thereby lowering the risk of AOM complicating
URI. Other researchers showed that 7 days of amoxicillinclavulanate, given early in the course of URI, did not prevent
AOM (20). We hypothesized that the apparent increased
AOM risk associated with antibiotic use is due in part to these
children generally being more prone to URI and AOM. Post
hoc analyses were done to compare the mean number of URI
and AOM episodes in children who did and did not use antibiotics within the 7 days prior to swab collection; the children
who used antibiotics averaged more URI episodes (means of
6.57 versus 2.86; P 0.0001; t test) and more AOM episodes
(means of 2.61 versus 1.05 AOM; P 0.001; t test) compared
to those who did not. The number of children who received
antibiotics within the 7 days prior to URI was low (n 23).
Further studies with a larger number of children are required
to determine whether antibiotic use prior to URI could increase the risk of AOM complicating URI.
Our study had several strengths, including the longitudinal
prospective study design, careful documentation and diagnosis
of AOM by team members, and our analyses of two recently
identified viruses, hBOV and hMPV. Multiple viruses are frequently detected within children (10, 18, 26). We detected
more than one respiratory virus in 11% of our specimens and
controlled for the presence of AOM-associated viruses in our
multivariate models. A recent study identified OM during
asymptomatic URI (36). Since the children in our study all
were experiencing URI symptoms, a limitation of our study is
that we may have missed AOM associated with asymptomatic
URI episodes.
In summary, we have identified specific bacterial and viral
interactions associated with an increased risk of AOM complicating URI. These data will be useful for the targeting and
design of effective AOM prevention and intervention strategies.
ACKNOWLEDGMENTS
This work was supported by the National Institute on Deafness and
other Communication Disorders at the National Institutes of Health
(R01 DC005841 to T.C.) and the National Institute of Allergy and
Infectious Diseases at the National Institutes of Health (R01 AI068043
to M.M.P.). The study was conducted at the Clinical Research Center
at the University of Texas Medical Branch, which is supported by the
Clinical and Translational Science Award from the National Center for
Research Resources at the National Institutes of Health (UL1
RR029876). The Galveston National Laboratorys assay development
services division received support from the National Institute of Allergy and Infectious Diseases at the National Institutes of Health
(AI057156).
We thank Janak Patel and Krystal Revai for their clinical contribution; Syed Ahmad, Michelle Tran, M. Lizette Rangel, Kyralessa B.
Ramirez, Liliana Najera, Rafael Serna, and Carolina Pillion for assistance with study subjects; and Sangeeta Nair and Ying Xiong for
assistance with study specimens.
REFERENCES
1. Allander, T., et al. 2005. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc. Natl. Acad. Sci. U. S. A. 102:12891
12896.
2. Alper, C. M., B. Winther, E. M. Mandel, J. O. Hendley, and W. J. Doyle.
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
creased (9, 13). The increased risk of AOM during hBOV
infection and H. influenzae colonization is of concern given
their high prevalence and the lack of vaccines for either pathogen.
Consistently with another study in the southern United
States (16), we detected RSV infections year round. However,
the highest RSV viral load occurred in winter months. Some
studies have identified RSV as the most common virus in
middle ear fluid samples (8, 19), and RSV is frequently detected as a middle ear pathogen in the absence of AOM bacterial pathogens (22). Our finding that high RSV load in the
presence of S. pneumoniae is associated with increased risk of
AOM suggests that RSV detection methods that quantify viral
load will help identify subjects at the highest risk of AOM. The
expanded use of the 13-valent pneumococcal conjugate vaccine
may be associated with further reductions in AOM due to S.
pneumoniae. However, the number of AOM episodes due to S.
pneumoniae nonvaccine serotypes increased after the introduction of PCV7, and concerns remain regarding the potential for
serotype replacement (9, 13).
The precise role of hBOV as a respiratory pathogen has
been debated (11, 23, 25). hBOV has been identified in approximately 3 to 4% of middle ear fluid samples from children
with AOM (9, 16). Martin et al. studied URI in young children
attending daycare and identified hBOV in 44% of asymptomatic children at enrollment (25). hBOV viral load did not differ
based on whether or not the children had URI symptoms (25).
Moreover, hBOV-infected children can shed virus for several
months (25, 34). Longtin et al. postulated that hBOV plays an
important pathogenic role in AOM and that the high rates of
hBOV in asymptomatic children could be due in part to prior
hBOV-associated AOM episodes (23). In children experiencing symptomatic URI, we found that, regardless of the viral
load, the presence of hBOV was associated with an increased
risk of AOM among children colonized with H. influenzae.
We did not identify an increased risk of AOM complicating
URI associated with hMPV. A prospective study in Finland
indicated that AOM developed in more than 60% of children
less than 3 years of age with hMPV (18). Our findings are
consistent with a retrospective analysis of hMPV in children
5 years of age covering a 20-year period. While half of the
children with hMPV were diagnosed with AOM, it was not
associated with excess risk of AOM compared to that of other
common respiratory viruses (35).
Previous studies have not conclusively identified interactions
between specific viruses and bacteria and an increased risk of
AOM. Investigators analyzing combined data from the Finnish
OM cohort study and the Finnish OM vaccine trial were unable to detect significant associations between specific viruses
and bacteria (22). All children in this study had AOM at the
time of virus and bacterium sampling, whereas our study examined children with URI and monitored them for the development of AOM. Alper et al. prospectively followed children
from 1 to 5 years of the age for URI symptoms and incident
OM (2). While 56% of RSV infections were associated with
OM, differences between specific viruses and OM were not
statistically significant; data on bacterial colonization were not
included in this analysis.
Our incidental finding of increased AOM risk associated
with antibiotic use within the 7 days prior to URI is interesting.
J. CLIN. MICROBIOL.
VOL. 49, 2011
3.
4.
5.
6.
7.
8.
9.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
2009. Rate of concurrent otitis media in upper respiratory tract infections
with specific viruses. Arch. Otolaryngol. Head Neck Surg. 135:1721.
Arnold, J. C. 2010. Human bocavirus in children. Pediatr. Infect. Dis. J.
29:557558.
Bakaletz, L. O. 2010. Immunopathogenesis of polymicrobial otitis media.
J. Leukoc. Biol. 87:213222.
Beder, L. B., et al. 2009. Clinical and microbiological impact of human
bocavirus on children with acute otitis media. Eur. J. Pediatr. 168:13651372.
Bonroy, C., A. Vankeerberghen, A. Boel, and H. De Beenhouwer. 2007. Use
of a multiplex real-time PCR to study the incidence of human metapneumovirus and human respiratory syncytial virus infections during two winter
seasons in a Belgian paediatric hospital. Clin. Microbiol. Infect. 13:504509.
Bourne, N., et al. 2005. Screening for hepatitis C virus antiviral activity with
a cell-based secreted alkaline phosphatase reporter replicon system. Antiviral Res. 67:7682.
Bulut, Y., et al. 2007. Acute otitis media and respiratory viruses. Eur. J. Pediatr. 166:223228.
Casey, J. R., D. G. Adlowitz, and M. E. Pichichero. 2010. New patterns in the
otopathogens causing acute otitis media six to eight years after introduction
of pneumococcal conjugate vaccine. Pediatr. Infect. Dis. J. 29:304.
Chonmaitree, T., et al. 2008. Viral upper respiratory tract infection and otitis
media complication in young children. Clin. Infect. Dis. 46:815823.
Christensen, A., S. A. Nordbo, S. Krokstad, A. G. Rognlien, and H. Dollner.
2010. Human bocavirus in children: mono-detection, high viral load and
viraemia are associated with respiratory tract infection. J. Clin. Virol. 49:
158162.
Cripps, A. W., and D. C. Otczyk. 2006. Prospects for a vaccine against otitis
media. Expert Rev. Vaccines 5:517534.
Dupont, D., et al. 2010. Evolving microbiology of complicated acute otitis
media before and after introduction of the pneumococcal conjugate vaccine
in France. Diagn. Microbiol. Infect. Dis. 68:8992.
Franz, A., et al. 2010. Correlation of viral load of respiratory pathogens and
co-infections with disease severity in children hospitalized for lower respiratory tract infection. J. Clin. Virol. 48:239245.
Grijalva, C. G., J. P. Nuorti, and M. R. Griffin. 2009. Antibiotic prescription
rates for acute respiratory tract infections in US ambulatory settings. JAMA
302:758766.
Halstead, D. C., and S. G. Jenkins. 1998. Continuous non-seasonal epidemic
of respiratory syncytial virus infection in the southeast United States. South.
Med. J. 91:433436.
Heikkinen, T., and T. Chonmaitree. 2003. Importance of respiratory viruses
in acute otitis media. Clin. Microbiol. Rev. 16:230241.
Heikkinen, T., R. Osterback, V. Peltola, T. Jartti, and R. Vainionpaa. 2008.
Human metapneumovirus infections in children. Emerg. Infect. Dis. 14:101
106.
Heikkinen, T., M. Thint, and T. Chonmaitree. 1999. Prevalence of various
respiratory viruses in the middle ear during acute otitis media. N. Engl.
J. Med. 340:260264.
Heikkinen, T., O. Ruuskanen, T. Ziegler, M. Waris, and H. Puhakka. 1995.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
3755
Short-term use of amoxicillin-clavulanate during upper respiratory tract infection for prevention of acute otitis media. J. Pediatr. 126:313316.
Henderson, F. W., et al. 1982. A longitudinal study of respiratory viruses and
bacteria in the etiology of acute otitis media with effusion. N. Engl. J. Med.
306:13771383.
Kleemola, M., et al. 2006. Is there any specific association between respiratory viruses and bacteria in acute otitis media of young children? J. Infect.
52:181187.
Longtin, J., J. B. Gubbay, S. Patel, and D. E. Low. 2010. High prevalence of
asymptomatic bocavirus in daycare: is otitis media a confounder? J. Infect.
Dis. 202:1617.
Lu, X., et al. 2006. Real-time PCR assays for detection of bocavirus in human
specimens. J. Clin. Microbiol. 44:32313235.
Martin, E. T., et al. 2010. Frequent and prolonged shedding of bocavirus in
young children attending daycare. J. Infect. Dis. 201:16251632.
Moore, H. C., et al. 2010. The interaction between respiratory viruses and
pathogenic bacteria in the upper respiratory tract of asymptomatic aboriginal
and non-aboriginal children. Pediatr. Infect. Dis. J. 29:540545.
Patel, J. A., D. T. Nguyen, K. Revai, and T. Chonmaitree. 2007. Role of
respiratory syncytial virus in acute otitis media: implications for vaccine
development. Vaccine 25:16831689.
Revai, K., D. Mamidi, and T. Chonmaitree. 2008. Association of nasopharyngeal bacterial colonization during upper respiratory tract infection and
the development of acute otitis media. Clin. Infect. Dis. 46:e34e37.
Ruohola, A., et al. 2006. Microbiology of acute otitis media in children with
tympanostomy tubes: prevalences of bacteria and viruses. Clin. Infect. Dis.
43:14171422.
Song, J. R., et al. 2010. Novel human bocavirus in children with acute
respiratory tract infection. Emerg. Infect. Dis. 16:324327.
Suzuki, A., et al. 2005. Detection of human metapneumovirus from children
with acute otitis media. Pediatr. Infect. Dis. J. 24:655657.
van den Hoogen, B. G., et al. 2001. A newly discovered human pneumovirus
isolated from young children with respiratory tract disease. Nat. Med. 7:719
724.
Vergison, A., et al. 2010. Otitis media and its consequences: beyond the
earache. Lancet Infect. Dis. 10:195203.
von Linstow, M. L., M. Hogh, and B. Hogh. 2008. Clinical and epidemiologic
characteristics of human bocavirus in Danish infants: results from a prospective birth cohort study. Pediatr. Infect. Dis. J. 27:897902.
Williams, J. V., et al. 2006. The role of human metapneumovirus in upper
respiratory tract infections in children: a 20-year experience. J. Infect. Dis.
193:387395.
Winther, B., C. M. Alper, E. M. Mandel, W. J. Doyle, and J. O. Hendley.
2007. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children
followed through a typical cold season. Pediatrics 119:10691075.
Zhou, F., A. Shefer, Y. Kong, and J. P. Nuorti. 2008. Trends in acute otitis
media-related health care utilization by privately insured young children in
the United States, 19972004. Pediatrics 121:253260.
Downloaded from http://jcm.asm.org/ on October 22, 2016 by guest
10.
VIRAL-BACTERIAL INTERACTIONS AND AOM COMPLICATING URI
You might also like
- ZJM 3750Document6 pagesZJM 3750Hervi LaksariNo ratings yet
- Acute Otitis Media Complicating Upper Viral-Bacterial Interactions and Risk ofDocument7 pagesAcute Otitis Media Complicating Upper Viral-Bacterial Interactions and Risk ofYohana VeronicaNo ratings yet
- THT - 12 Acute Otitis Media and Other Complication of Viral Respiratory InfectionDocument12 pagesTHT - 12 Acute Otitis Media and Other Complication of Viral Respiratory InfectionWelly SuryaNo ratings yet
- Clin Infect Dis. 2011 Wald S277 83Document7 pagesClin Infect Dis. 2011 Wald S277 83Tara WandhitaNo ratings yet
- Acute Otitis Media and Acute Bacterial SinusitisDocument7 pagesAcute Otitis Media and Acute Bacterial SinusitisMonica Fradisha ZukhriNo ratings yet
- New Insights Into The Treatment of Acute Otitis MediaDocument13 pagesNew Insights Into The Treatment of Acute Otitis MediaAGUS DE COLSANo ratings yet
- Viral-Bacterial Interactions in Acute Otitis MediaDocument12 pagesViral-Bacterial Interactions in Acute Otitis MediasnrarasatiNo ratings yet
- Oma Dan AbsDocument7 pagesOma Dan AbsGianna_OshinNo ratings yet
- Bacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisDocument5 pagesBacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisResianaPutriNo ratings yet
- 08 0119 PDFDocument8 pages08 0119 PDFAnailil MoralesNo ratings yet
- Potensi Penyebaran Infeksi Nosokomial Instalasi Rawat Inap Khusus Tuberkulosis (Irina C5) Blu Rsup Prof. Dr. R. D. Kandou ManadoDocument9 pagesPotensi Penyebaran Infeksi Nosokomial Instalasi Rawat Inap Khusus Tuberkulosis (Irina C5) Blu Rsup Prof. Dr. R. D. Kandou ManadoMentariNo ratings yet
- Pediatric Acute Bacterial Sinusitis Following Viral URIDocument15 pagesPediatric Acute Bacterial Sinusitis Following Viral URIBrhajan Jhosmel CañariNo ratings yet
- Etiology of Acute Otitis Media in Children Less Than 5 Years of AgeDocument9 pagesEtiology of Acute Otitis Media in Children Less Than 5 Years of AgeadyNo ratings yet
- The Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewDocument15 pagesThe Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewPutu Sukma RadhanaNo ratings yet
- Seminar: Olli Ruuskanen, Elina Lahti, Lance C Jennings, David R MurdochDocument12 pagesSeminar: Olli Ruuskanen, Elina Lahti, Lance C Jennings, David R MurdochChika AmeliaNo ratings yet
- Is Virus Coinfection A Predictor of Severity in Children With Viral Respiratory Infections?Document6 pagesIs Virus Coinfection A Predictor of Severity in Children With Viral Respiratory Infections?castillocavazos09No ratings yet
- Neumonia Por InfluenzaDocument19 pagesNeumonia Por InfluenzaEdgar GavilanesNo ratings yet
- FIX Clin. Vaccine Immunol. 2014 Tamir 1189 91Document3 pagesFIX Clin. Vaccine Immunol. 2014 Tamir 1189 91Finty ArfianNo ratings yet
- Jurnal 2Document11 pagesJurnal 2elvanNo ratings yet
- Microbial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaDocument4 pagesMicrobial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaiisisiisNo ratings yet
- New MOC ResourcesDocument22 pagesNew MOC ResourcesYidnekachew Girma AssefaNo ratings yet
- Epidemiological Profile of Acute Typical Bacterial Pneumonia at The National Reference University Hospital Center of NDjamena Risk Factors and Antibiotic ResistanceDocument13 pagesEpidemiological Profile of Acute Typical Bacterial Pneumonia at The National Reference University Hospital Center of NDjamena Risk Factors and Antibiotic ResistanceAthenaeum Scientific PublishersNo ratings yet
- Gereige 2013 PneumoniaDocument21 pagesGereige 2013 PneumoniaLuis Carlos OlguínNo ratings yet
- Clinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptDocument5 pagesClinico - Seroepidemiological Evaluation of Toxocariasis in Asthmatic Pediatric Children in Mansoura City in EgyptInternational Medical PublisherNo ratings yet
- Throat and Nasal Swabs For Molecular Detection of Respiratory Viruses in Acute PharyngitisDocument4 pagesThroat and Nasal Swabs For Molecular Detection of Respiratory Viruses in Acute PharyngitisFriskyShandy BadiNo ratings yet
- 1 s2.0 S1198743X14632079 MainDocument9 pages1 s2.0 S1198743X14632079 MainAizaz HassanNo ratings yet
- Resistencia de Uropatógenos en Infecciones de Tracto Urinario en Leon NicaraguaDocument4 pagesResistencia de Uropatógenos en Infecciones de Tracto Urinario en Leon NicaraguaMiguel AnguianoNo ratings yet
- Role of Human Viruses in PeriodontologyDocument52 pagesRole of Human Viruses in PeriodontologySai SuriyaNo ratings yet
- Bacterial AgentDocument10 pagesBacterial AgentDyah Ayu Puspita AnggarsariNo ratings yet
- Viral Etiology and Symptoms of Acute Upper Respiratory Tract Infections in ChildrenDocument7 pagesViral Etiology and Symptoms of Acute Upper Respiratory Tract Infections in ChildrenSeptian Sapta HadiNo ratings yet
- BronchiolitisDocument4 pagesBronchiolitisFlavia RochmanNo ratings yet
- Hand, Foot and Mouth Disease: Spatiotemporal Transmission and ClimateDocument10 pagesHand, Foot and Mouth Disease: Spatiotemporal Transmission and ClimateAisah AisahNo ratings yet
- Extraintestinal Focal Infections in Adults With Nontyphoid Salmonella 2006Document10 pagesExtraintestinal Focal Infections in Adults With Nontyphoid Salmonella 2006Carlos Antonio Arrieta NieblesNo ratings yet
- Bacteremia in Children-JTPDocument5 pagesBacteremia in Children-JTPRomica MarcanNo ratings yet
- Absceso CerebralDocument6 pagesAbsceso Cerebralkreacher3000No ratings yet
- ContentServer AspDocument12 pagesContentServer AspNanda Nurdara TaharaNo ratings yet
- Jurnal OtomikosissDocument7 pagesJurnal Otomikosissrahmy kubangunNo ratings yet
- Tuberculosis as a cause or comorbidity of childhood pneumoniaDocument9 pagesTuberculosis as a cause or comorbidity of childhood pneumoniairenaNo ratings yet
- How Contagious Is Tuberculosis?Document9 pagesHow Contagious Is Tuberculosis?fryancakaNo ratings yet
- Meningite Aguda Bacteriana Rev Lancet 2016Document12 pagesMeningite Aguda Bacteriana Rev Lancet 2016elsonverdadeNo ratings yet
- 1 s2.0 S168411821400173X MainDocument9 pages1 s2.0 S168411821400173X MainRosiyantiNo ratings yet
- CAP - PrinaDocument12 pagesCAP - PrinaSalNo ratings yet
- 2013 34 438 Rani S. Gereige and Pablo Marcelo Laufer: Pediatrics in ReviewDocument21 pages2013 34 438 Rani S. Gereige and Pablo Marcelo Laufer: Pediatrics in ReviewAlvaro Andres Flores JimenezNo ratings yet
- otitis media paper 2024Document10 pagesotitis media paper 2024shakeel.ahmedNo ratings yet
- Human Infectious Diseases and Risk of Preeclampsia: An Updated Review of The LiteratureDocument12 pagesHuman Infectious Diseases and Risk of Preeclampsia: An Updated Review of The LiteratureasfwegereNo ratings yet
- NASAL CARRIAGE OF MULTI-DRUG RESISTANT PANTON VALENTINE LEUKOCIDIN POSITIVE STAPHYLOCOCCUS AUREUS IN HEALTHY INDIVIDUALS OF TUDUN-WADA, GOMBE STATE, NIGERIA.Document10 pagesNASAL CARRIAGE OF MULTI-DRUG RESISTANT PANTON VALENTINE LEUKOCIDIN POSITIVE STAPHYLOCOCCUS AUREUS IN HEALTHY INDIVIDUALS OF TUDUN-WADA, GOMBE STATE, NIGERIA.Tunde OdetoyinNo ratings yet
- Abstract - Sinusitis Et OtitisDocument5 pagesAbstract - Sinusitis Et OtitisGazmend SH BojajNo ratings yet
- 2018 Article 296 PDFDocument10 pages2018 Article 296 PDFDiego RomaNo ratings yet
- Pneumonia Etiology Research for Child Health Project: A 21st Century Childhood Pneumonia Etiology StudyDocument9 pagesPneumonia Etiology Research for Child Health Project: A 21st Century Childhood Pneumonia Etiology StudyZuna QaziNo ratings yet
- 7 PDFDocument4 pages7 PDFZaka Jauhar FirdausNo ratings yet
- Epidemiology of Acute Pharyngitis.Document3 pagesEpidemiology of Acute Pharyngitis.veronika ratihNo ratings yet
- J Infect Dis. 2007 Turner 765 6Document2 pagesJ Infect Dis. 2007 Turner 765 6Academe Home TuitionNo ratings yet
- 235 Article 637 1 10 20180924Document8 pages235 Article 637 1 10 20180924Mazin AlmaziniNo ratings yet
- 2010, Bronchiolitis ObliteransDocument7 pages2010, Bronchiolitis ObliteransValTazzeeNo ratings yet
- Sample Chapter TwoDocument2 pagesSample Chapter TwoMohamed Ali Abdi MahadalleNo ratings yet
- Meningitis Bacteriana Aguda en El AdultoDocument12 pagesMeningitis Bacteriana Aguda en El AdultoJulian AlbarracínNo ratings yet
- BMC Pulmonary MedicineDocument15 pagesBMC Pulmonary MedicineAndra GulinNo ratings yet
- Jurnal Tonsilitis 1Document4 pagesJurnal Tonsilitis 1Anonymous WtbEp0No ratings yet
- Occurrence and Antibiotic Susceptibility of Patients That Attended Federal Medical Centre Umuahia, Abia StateDocument4 pagesOccurrence and Antibiotic Susceptibility of Patients That Attended Federal Medical Centre Umuahia, Abia StateRizky NugrohoNo ratings yet
- Woc BBLRDocument1 pageWoc BBLRferNo ratings yet
- PDFDocument8 pagesPDFferNo ratings yet
- TpselftestresultDocument1 pageTpselftestresultferNo ratings yet
- Woc BBLRDocument1 pageWoc BBLRferNo ratings yet
- Aaron Et Al 2001Document7 pagesAaron Et Al 2001ferNo ratings yet
- HTTP Journals - Plos.org Plosmedicine Article Asset Id 10.1371 Journal - Pmed.1001444 PDFDocument12 pagesHTTP Journals - Plos.org Plosmedicine Article Asset Id 10.1371 Journal - Pmed.1001444 PDFferNo ratings yet
- Pneumoni JurnalDocument4 pagesPneumoni JurnalferNo ratings yet
- Woc BBLRDocument1 pageWoc BBLRferNo ratings yet
- Woc BBLRDocument1 pageWoc BBLRferNo ratings yet
- J Infect Dis. 2005 Esper 492 8Document7 pagesJ Infect Dis. 2005 Esper 492 8ferNo ratings yet
- Mother's Education, Knowledge and Caring for Toddlers with ARIDocument8 pagesMother's Education, Knowledge and Caring for Toddlers with ARICinDy Advenia SiarNo ratings yet
- Jurnal Keperawatan Volume II No 1 April 2014 Sri Hayati 62-67 PDFDocument6 pagesJurnal Keperawatan Volume II No 1 April 2014 Sri Hayati 62-67 PDFferNo ratings yet
- J Infect Dis. 2006 Williams 387 95Document9 pagesJ Infect Dis. 2006 Williams 387 95ferNo ratings yet
- Ne W Engl and Journal MedicineDocument8 pagesNe W Engl and Journal MedicineferNo ratings yet
- GERN Et Al-2000Document6 pagesGERN Et Al-2000ferNo ratings yet
- Clin Infect Dis. 2008 Chonmaitree 815 23Document9 pagesClin Infect Dis. 2008 Chonmaitree 815 23ferNo ratings yet
- Jurnal Keperawatan Volume II No 1 April 2014 Sri Hayati 62-67 PDFDocument6 pagesJurnal Keperawatan Volume II No 1 April 2014 Sri Hayati 62-67 PDFferNo ratings yet
- Secondary Bacterial Infections in CovidDocument4 pagesSecondary Bacterial Infections in Covidnanang hidayatullohNo ratings yet
- Lectins - Function Structure Biological Properties andDocument22 pagesLectins - Function Structure Biological Properties andOrlando Pérez DelgadoNo ratings yet
- 60 Item Medical Surgical Nursing : Musculoskeletal Examination AnswersDocument10 pages60 Item Medical Surgical Nursing : Musculoskeletal Examination AnswersApril Kirstin ChuaNo ratings yet
- AIDS 30 Years PDFDocument11 pagesAIDS 30 Years PDFbadboy6.868510No ratings yet
- Chest X-Ray Appearances in Pneumonia and BronchiolitisDocument7 pagesChest X-Ray Appearances in Pneumonia and BronchiolitisMariani AniNo ratings yet
- Viral Structure and Characterization MethodsDocument3 pagesViral Structure and Characterization MethodsKeanne GanironNo ratings yet
- CHN ReviewerDocument36 pagesCHN ReviewerRezideh75% (4)
- ASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONDocument5 pagesASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONRussel SantosNo ratings yet
- 20 Soal Latihan Report Text Dalam Bahasa InggrisDocument6 pages20 Soal Latihan Report Text Dalam Bahasa InggrisRizkhi CliQuerz Chayanx UnGuNo ratings yet
- Candida Auris 1690952022Document10 pagesCandida Auris 16909520225n5przwzfsNo ratings yet
- BIONAIDDocument16 pagesBIONAIDAnonymous Wie6lbepNo ratings yet
- 17 Alterations With Infectious Inflammatory and Immunologic ResponsesDocument100 pages17 Alterations With Infectious Inflammatory and Immunologic ResponsesBea Bianca Cruz100% (1)
- Epidemiology Quiz On Chapter 1Document3 pagesEpidemiology Quiz On Chapter 1drng48No ratings yet
- Endodontics in Systemically Compromised PatientsDocument30 pagesEndodontics in Systemically Compromised Patientscarolina pavezNo ratings yet
- HIV and AIDS explainedDocument1 pageHIV and AIDS explainedKevinNo ratings yet
- Resveratrol and Its Effects On Human Health and LongevityDocument367 pagesResveratrol and Its Effects On Human Health and LongevityArnulfo Yu LanibaNo ratings yet
- Actual Nursing Care Plan 2Document16 pagesActual Nursing Care Plan 2Alyanna Evangelista100% (2)
- Icd 10 2015 Who OnlineDocument1,256 pagesIcd 10 2015 Who OnlineMuhammad Ulul AmrieNo ratings yet
- Lung Abscess in Adults - UpToDateDocument32 pagesLung Abscess in Adults - UpToDateAntonela Esther Quijada BenitoNo ratings yet
- Jocd 13115Document5 pagesJocd 13115Tâm ViệtNo ratings yet
- Circulatory and Respiratory Systems Learning PlanDocument6 pagesCirculatory and Respiratory Systems Learning PlanMary-Rose CasuyonNo ratings yet
- Klinoski Rachael L 200709 MSCDocument128 pagesKlinoski Rachael L 200709 MSCDrashua AshuaNo ratings yet
- The Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Document13 pagesThe Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Alex Del PieroNo ratings yet
- Contingency Plan for COVID-19 at Bagocboc National High SchoolDocument12 pagesContingency Plan for COVID-19 at Bagocboc National High SchoolanneNo ratings yet
- Group 5 explores airborne microorganismsDocument54 pagesGroup 5 explores airborne microorganismsBeauty LiciousNo ratings yet
- E W C O F: Arly Ound ARE IN PEN RacturesDocument3 pagesE W C O F: Arly Ound ARE IN PEN RacturesMatheis Laskar PelangiNo ratings yet
- Ab 6Document7 pagesAb 6KhushnoodNo ratings yet
- Surgical Site Infection (SSI) Event: Monthly Reporting PlanDocument31 pagesSurgical Site Infection (SSI) Event: Monthly Reporting PlanDRMC InfectioncontrolserviceNo ratings yet
- Professional Cordless Electrostatic Handheld Sprayerltyap PDFDocument4 pagesProfessional Cordless Electrostatic Handheld Sprayerltyap PDFSchroederGormsen7No ratings yet
- Chapter 10Document5 pagesChapter 10Apryll DarlineNo ratings yet