Professional Documents
Culture Documents
57.205 - ExpBBF - BLANK Form Pengkajian Pparan Jarum Darah Cairan Tubuh
Uploaded by
Mavika Tarika NusratOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
57.205 - ExpBBF - BLANK Form Pengkajian Pparan Jarum Darah Cairan Tubuh
Uploaded by
Mavika Tarika NusratCopyright:
Available Formats
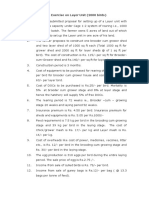
OMB No.
0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 1 of 7
*required for saving
Facility ID#: _____________________
*HCW ID#: _____________________
HCW Name, Last: _________________
Exposure Event #: __________________
First: ___________________
Middle: ___________________
*Gender: F M Other
*Work Location: ______________________________
*Occupation: ______________________ If occupation is physician, indicate clinical specialty:___________________
Section I General Exposure Information
*Date of Birth: _____ /_____ /______
Y
N
1a. If No, specify name of facility in which exposure occurred: _____________________________
1. *Did exposure occur in this facility:
AM PM
2. *Date of exposure: _____ /_____ /______
3. *Time of exposure: _______
4. Number of hours on duty: _________
5. Is exposed person a temp/agency employee?
Y N
6. *Location where exposure occurred: ______________
7. *Type of exposure: (Check all that apply)
7a. Percutaneous: Did exposure involve a clean, unused needle or sharp object?
Y N (If No, complete Q8, Q9, Section II and Section V-XI)
7b. Mucous membrane (Complete Q8, Q9, Section III and Section V-XI)
7c. Skin: Was skin intact? Y N Unknown (If No, complete Q8, Q9, Section III & Section V-XI)
7d. Bite (Complete Q9 and Section IV-XI)
8. *Type of fluid/tissue involved in exposure: (Check one)
Blood/blood products
Solutions (IV fluid, irrigation, etc.): (Check one)
Visibly bloody
Not visibly bloody
Tissue
Other (specify): _________________________
Unknown
9. *Body site of exposure: (Check all that apply)
Hand/finger
Eye
Arm
Leg
Foot
Mouth
Nose
Other (specify):
Body fluids: (Check one)
Visibly bloody
Not visibly bloody
If body fluid, indicate one body fluid type:
Amniotic
CSF
Pericardial
Peritoneal
Pleural
Semen
Synovial
Vaginal fluid
Saliva
Sputum
Tears
Urine
Feces/stool
Other (Specify):
_____________________
____________________
Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is
collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the
consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)).
Public reporting burden of this collection of information is estimated to average 1 hour per response, including the time for reviewing instructions, searching existing data
sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is
not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other
aspect of this collection of information, including suggestions for reducing this burden to CDC, Reports Clearance Officer, 1600 Clifton Rd., MS D-74, Atlanta, GA 30333,
ATTN: PRA (0920-0666).
CDC 57.205 (Front), v6.6
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 2 of 7
Section II Percutaneous Injury
1. *Was the needle or sharp object visibly contaminated with blood prior to exposure?
Y N
2. Depth of the injury: (Check one)
Superficial, surface scratch
Moderate, penetrated skin
Deep puncture or wound
Unknown
3. What needle or sharp object caused the injury (Check one)
Device (select one)
Non-device sharp object (specify): ___________________
Unknown sharp object
Hollow-bore needle
Arterial blood collection device
Hypodermic needle, attached to
syringe
IV catheter central line
Prefilled cartridge syringe
Hemodialysis needle
Winged-steel (Butterfly type)
needle
Biopsy needle
Hypodermic needle, attached to IV
tubing
Bone marrow needle
Unattached hypodermic needle
IV catheter peripheral line
IV stylet
Dental aspirating syringe w/ needle
Huber needle
Spinal or epidural needle
Vacuum tube holder/needle
Hollow-bore needle, type unknown
Other hollow-bore needle
Bur
Explorer
Lancet
Razor
Scaler/curette
Tenaculum
Electrocautery device
Extraction forceps
Microtome blade
Retractor
Scalpel blade
Trocar
Blood collection tube
Slide
Medication ampule/vial/bottle
Specimen/test/vacuum tube
Blood collection tube
Specimen/test/vacuum tube
Suture needle
Suture needle
Other solid sharps
Bone cutter
Elevator
File
Pin
Rod (orthopedic)
Scissors
Wire
Glass
Capillary tube
Pipette
Plastic
Capillary tube
Non-sharp safety device
Blood culture adapter
Catheter securement device
Other known device (specify): _________________________________
4. Manufacturer and Model: _____________________________________
CDC 57.205 (Back), v6.6
IV delivery system
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 3 of 7
5. Did the needle or other sharp object involved in the injury have a safety feature?
Y N
5a. If Yes, indicate type of safety feature: (Check one) If No, skip to Q6.
Bluntable needle, sharp
Hinged guard/shield
Retractable needle/sharp
Sliding/gliding guard/shield
Needle/sharp ejector
Mylar wrapping/plastic
Other safety feature (specify):____________________
Unknown safety mechanism
5b. If the device had a safety feature, when did the injury occur? (Check one)
Before activation of the safety feature was
Safety feature failed, after activation
appropriate
During activation of the safety feature
Safety feature improperly activated
Safety feature not activated
Other (specify): _____________________________
6. When did the injury occur? (Check one)
Before use of the item
During use of the item
After use of the item before disposal
During or after disposal
Unknown
7. For what purpose or activity was the sharp device being used? (Check one)
Obtaining a blood specimen percutaneously
Performing phlebotomy
Performing arterial puncture
Performing a fingerstick/heelstick
Other blood-sampling procedure
(specify): ___________________________________
Giving a percutaneous injection
Giving an IM injection
Giving a SC injection
Placing a skin test (e.g., tuberculin, allergy, etc.)
Performing a line related procedure
Inserting or withdrawing a catheter
Obtaining a blood sample from a central or
Injecting into a line or port
Connecting an I.V. line
peripheral I.V. line or port
Performing surgery/autopsy/other invasive procedure
Suturing
Incising
Palpating/exploring
Specify procedure: ____________________________
Performing a dental procedure
Hygiene (prophylaxis)
Restoration (amalgam composite, crown)
Root canal
Periodontal surgery
Oral surgery
Simple extraction
Surgical extraction
Handling a specimen
Transferring BBF into a specimen container
Processing specimen
Other
Other diagnostic procedure (e.g., thoracentesis)
Unknown
Other (specify): ____________________________
CDC 57.205 (Back), v6.6
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 4 of 7
8. What was the activity at the time of injury? (Check one)
Cleaning room
Collecting/transporting waste
Decontamination/processing used equipment
Disassembling device/equipment
Handling equipment
Opening/breaking glass container (e.g., ampule)
Performing procedure
Placing sharp in container
Recapping
Transferring/passing/receiving device
Other (specify): _____________________________________
9. Who was holding the device at the time the injury occurred? (Check one)
Exposed person
Co-worker/other person
No one, the sharp was an uncontrolled sharp in the environment
10. What happened when the injury occurred? (Check one)
Patient moved and jarred device
Contact with overfilled/punctured sharps container
Device slipped
Improperly disposed sharp
Device rebounded
Other (specify): _______________________________
Sharp was being recapped
Unknown
Collided with co-worker or other person
CDC 57.205 (Back), v6.6
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 5 of 7
Section III Mucous Membrane and/or Skin Exposure
1. Estimate the amount of blood/body fluid exposure: (Check one)
Small (<1 tsp or 5cc)
Moderate (>1 tsp and up to cup, or 6-50 cc)
Large (> cup or 50cc)
Unknown
2. Activity/event when exposure occurred: (Check one)
Airway manipulation (e.g., suctioning airway,
inducing sputum)
Bleeding vessel
Patient spit/coughed/vomited
Changing dressing/wound care
Phlebotomy
Surgical procedure (e.g., all surgical procedures
Cleaning/transporting contaminated equipment
Tube placement/removal/manipulation (e.g., chest,
Endoscopic procedures
IV or arterial line insertion/removal/manipulation
Irrigation procedures
Manipulating blood tube/bottle/specimen
Vaginal delivery
Other (specify): _______________________________
Unknown
including C-section)
endotracheal, NG, rectal, urine catheter)
container
3. Barriers used by the worker at the time of exposure: (Check all that apply)
Face shield
Gloves
Goggles
Gown
Mask/respirator
Other (specify): _______________________________
No barriers
Section IV Bite
1. Wound description: (Check one)
No spontaneous bleeding
Spontaneous bleeding
Tissue avulsed
Unknown
2. Activity/event when exposure occurred: (Check one)
During dental procedure
During oral examination
Providing oral hygiene
Providing non-oral care to patient
CDC 57.205 (Back), v6.6
Assault by patient
Other (specify): _______________________________
Unknown
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 6 of 7
Note: Section V-IX are required when following the protocols for Exposure Management.
Section V Source Information
1. Was the source patient known?
Y N
2. Was HIV status known at the time of exposure?
Y N
3. Check the test results for the source patient (P=positive, N=negative, I=indeterminate, U=unknown, R=refused, NT=not tested)
Hepatitis B
P
HBsAg
HBeAg
Total anti-HBc
Anti-HBs
Hepatitis C
Anti-HCV EIA
Anti-HCV supplemental
PCR-HCV RNA
HIV
EIA, ELISA
Rapid HIV
Confirmatory test
Section VI For HIV Infected Source
1. Stage of disease: (Check one)
End-stage AIDS
AIDS
Acute HIV illness
__________
NT
Other symptomatic HIV, not AIDS
HIV infection, no symptoms
Unknown
2. Is the source patient taking anti-retroviral drugs?
2a. If yes, indicate drug(s):
Y N U
__________
__________
__________
3. Most recent CD4 count: ________mm3
Date: ____ /______ (mo/yr)
4. Viral load: _____ copies/ml _____ undetectable
Section VII Initial Care Given to Healthcare Worker
1. HIV postexposure prophylaxis:
Date: ____ /______ (mo/yr)
Offered? Y N U
__________
__________
Taken: Y N U (If Yes, complete PEP form)
2. HBIG given? Y N U
Date administered: ____ /____ /_______
3. Hepatitis B vaccine given: Y N U
Date 1st dose administered: ____ /____ /_______
4. Is the HCW pregnant?
4a. If yes, which trimester?
CDC 57.205 (Back), v6.6
Y N U
1 2 3 U
OMB No. 0920-0666
Exp. Date: 12-31-2015
www.cdc.gov/nhsn
Exposure to Blood/Body Fluids
Page 7 of 7
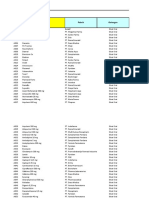
Section VIII Baseline Lab Testing
Was baseline testing performed on the HCW? Y N U If Yes, indicate results
Test
Date
Result
Test
HIV EIA
__ /__ /____ P N
I
R ALT
HIV Confirmatory
__ /__ /____ P N
I
R Amylase
Hepatitis C anti-HCV-EIA
__ /__ /____ P N
I
R Blood glucose
Hepatitis C anti-HCV-supp
__ /__ /____ P N
I
R Hematocrit
Hepatitis C PRC HCV RNA __ /__ /____ P N
I
Hemoglobin
Hepatitis B HBs Ag
__ /__ /____ P N
I
Platelets
Hepatitis B IgM anti-HBc
__ /__ /____ P N
I
Blood cells in Urine
Hepatitis B Total anti-HBc
__ /__ /____ P N
I
WBC
Hepatitis B Anti-HBs
__ /__ /____ _____ mIU/mL
Creatinine
Result Codes: P=Positive, N=Negative, I=Indeterminate, R=Refused Other: __________
Date
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
__ /__ /____
Result
____ IU/L
____ IU/L
____ mmol/L
____ %
____ gm/L
____ x109/L
____ #/mm3
____ x109/L
____ mol/L
___________
Section IX Follow-up
1. Is it recommended that the HCW return for follow-up of this exposure?
1a. If Yes, will follow-up be performed at this facility?
Y N
Y N
Section X Narrative
In the workers words, how did the injury occur?
Section XI Prevention
In the workers words, what could have prevented the injury?
Custom Fields
Label
_________________________
_________________________
_________________________
_________________________
_________________________
_________________________
Comments
CDC 57.205 (Back), v6.6
____/____/_____
______________
______________
______________
______________
______________
Label
_________________________
_________________________
_________________________
_________________________
_________________________
_________________________
____/____/_____
______________
______________
______________
______________
______________
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pescatarian Mediterranean Diet Cookbook 2 - Adele TylerDocument98 pagesPescatarian Mediterranean Diet Cookbook 2 - Adele Tylerrabino_rojoNo ratings yet
- Recommended Practice For Corrosion Management of Pipelines in Oil & Gas Production and TransportationDocument123 pagesRecommended Practice For Corrosion Management of Pipelines in Oil & Gas Production and Transportationsaifoa100% (2)
- Insulating Oil TestingDocument6 pagesInsulating Oil TestingnasrunNo ratings yet
- Lesson Plan On Tuberculosis (Health Talk)Document8 pagesLesson Plan On Tuberculosis (Health Talk)Priyanka Jangra100% (2)
- Hema Lec HematopoiesisDocument8 pagesHema Lec HematopoiesisWayne ErumaNo ratings yet
- Presentation On "Insurance Sector": Submitted By: Faraz Shaikh Roll No: 9 Mba MarketingDocument16 pagesPresentation On "Insurance Sector": Submitted By: Faraz Shaikh Roll No: 9 Mba MarketingFakhruddin DholkawalaNo ratings yet
- Chapter 1 Fundamentals of Taxation by Cruz, Deschamps, Miswander, Prendergast, Schisler, and TroneDocument25 pagesChapter 1 Fundamentals of Taxation by Cruz, Deschamps, Miswander, Prendergast, Schisler, and TroneReese Parker100% (4)
- Study of Behavior of Bacterial ConcreteDocument20 pagesStudy of Behavior of Bacterial ConcreteGodwin KopelliNo ratings yet
- DET Tronics: Unitized UV/IR Flame Detector U7652Document2 pagesDET Tronics: Unitized UV/IR Flame Detector U7652Julio Andres Garcia PabolaNo ratings yet
- Pieces 1 Cod Amount Product Detail 36 Cotton Pant RemarksDocument4 pagesPieces 1 Cod Amount Product Detail 36 Cotton Pant RemarksFaizan AhmadNo ratings yet
- Report Text: General ClassificationDocument7 pagesReport Text: General Classificationrisky armala syahraniNo ratings yet
- Plastic As Soil StabilizerDocument28 pagesPlastic As Soil StabilizerKhald Adel KhaldNo ratings yet
- 48V 100ah LiFePO4 Battery Spec With CommunicationDocument6 pages48V 100ah LiFePO4 Battery Spec With CommunicationsoulmuhNo ratings yet
- Toxic RelationshipDocument1 pageToxic RelationshipwidyasNo ratings yet
- HOPE 3-Module 8-Week 5-6Document9 pagesHOPE 3-Module 8-Week 5-6Freya SalorNo ratings yet
- Case Exercise On Layer Unit (2000 Birds)Document2 pagesCase Exercise On Layer Unit (2000 Birds)Priya KalraNo ratings yet
- Leave of Absence Form (Rev. 02 072017)Document1 pageLeave of Absence Form (Rev. 02 072017)KIMBERLY BALISACANNo ratings yet
- Gratuity SlidesDocument11 pagesGratuity SlidesK V GondiNo ratings yet
- Boli Vertebro MedulareDocument12 pagesBoli Vertebro MedulareHalit DianaNo ratings yet
- Osh e MeerDocument3 pagesOsh e MeerfatduckNo ratings yet
- RIASEC Personality TestDocument2 pagesRIASEC Personality TestSarah Jane NomoNo ratings yet
- Impact of Job Design On Employee Engagement: A Theoretical and Literature ReviewDocument6 pagesImpact of Job Design On Employee Engagement: A Theoretical and Literature ReviewAnonymous CwJeBCAXpNo ratings yet
- EBANX Beyond Borders 2020Document71 pagesEBANX Beyond Borders 2020Fernanda MelloNo ratings yet
- 1979 The Cult Phenomenon in The United States - DR John Gordon ClarkDocument8 pages1979 The Cult Phenomenon in The United States - DR John Gordon ClarkFrederick BismarkNo ratings yet
- MINUZA Laptop Scheme Programs ThyDocument9 pagesMINUZA Laptop Scheme Programs Thyanualithe kamalizaNo ratings yet
- Philips Healthcare: Field Change Order ServiceDocument5 pagesPhilips Healthcare: Field Change Order ServiceJimNo ratings yet
- Data Obat VMedisDocument53 pagesData Obat VMedismica faradillaNo ratings yet
- Ca 2013 39Document40 pagesCa 2013 39singh1699No ratings yet
- Self Reflection 1Document5 pagesSelf Reflection 1api-270873994No ratings yet
- BRS PDFDocument14 pagesBRS PDFGautam KhanwaniNo ratings yet