Professional Documents
Culture Documents
Ishii Et Al-2012-Journal of Obstetrics and Gynaecology Research PDF
Uploaded by
Mario AlexanderOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ishii Et Al-2012-Journal of Obstetrics and Gynaecology Research PDF
Uploaded by
Mario AlexanderCopyright:
Available Formats
doi:10.1111/j.1447-0756.2011.01625.x J. Obstet. Gynaecol. Res. Vol. 38, No.
1: 102107, January 2012
Balloon tamponade during cesarean section is useful for
severe post-partum hemorrhage due to placenta previa jog_1625 102..107
Takako Ishii1, Kenjiro Sawada1, Shunsuke Koyama1, Aki Isobe1, Atsuko Wakabayashi1,
Tsuyoshi Takiuchi1, Takeshi Kanagawa1, Takuji Tomimatsu1, Kazuhide Ogita2 and
Tadashi Kimura1
1
Department of Obstetrics and Gynecology, Osaka University Graduate School of Medicine, Suita, and 2Department of
Obstetrics and Gynecology, Rinku General Medical Center, Izuminsano, Osaka, Japan
Abstract
Aim: Severe post-partum hemorrhage during cesarean section due to placenta previa is still one of the leading
causes of maternal mortality. The aim of this study was to evaluate the efficiency of intrauterine tamponade
with a Sengstaken-Blakemore tube (SB-tube) for the treatment of severe post-partum hemorrhage in cases of
placenta previa.
Material and Methods: Data were collected from our departmental clinical records on all patients who
underwent caesarian section due to placenta previa between 2007 and 2009.
Results: During the period analyzed, 37 patients underwent caesarian section due to placenta previa/low-
lying placenta. Four (11%) underwent hysterectomy due to placenta accreta and 33 (89%) were treated
conservatively. Of the 33 patients with conserved uterus, 10 (28%) patients required a SB-tube during the
cesarean section because of continuous post-partum hemorrhage despite appropriate medical treatment. The
median bleeding during the operation was 2030 860 mL in the patients who used SB-tube. None of them
presented severe complications related to these procedures or required any further invasive surgery.
Conclusion: Intrauterine balloon-tamponade could successfully control severe hemorrhage from a lower
uterine segment of a patient with placenta previa. This technique is simple to use, scarcely invasive, and
available at a low cost to all maternity wards, and should be considered as one of the first management options
to reduce the risk of undesirable hysterectomy.
Key words: balloon-tamponade, cesarean section, placenta previa, post-partum hemorrhage, Sengstaken-
Blakemore tube.
Introduction recent developments in transvaginal ultrasonography
allow clinicians to diagnose prenatally, it is still one of
The incidence of placenta previa at the time of birth the leading causes of maternal mortality.1
varies widely in published series, but on average it Hysterectomy can be an undesirable action to take,
occurs once in every 150250 live births. Obstetrical especially in the case of a low parity patient. Usually,
bleeding (intrapartum/post-partum) secondary to pla- this step is taken when other traditional measures to
centa previa with variable degrees of accretion is not stop hemorrhage fail.2 Various management options
uncommon. Post-partum bleeding is usually from the are utilized for control of bleeding caused by this clini-
placental bed at the lower uterine segment and occurs cal abnormality and conservative approaches are
immediately after the placenta is delivered. Although becoming increasingly used instead of hysterectomy.
Received: July 15 2010.
Accepted: March 3 2011.
Reprint request to: Dr Kenjiro Sawada, Department of Obstetrics and Gynecology, Osaka University Graduate School of Medicine, 2-2
Yamadaoka, Suita, Osaka, Japan. Email: daasawada@gyne.med.osaka-u.ac.jp
102 2011 The Authors
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
Balloon tamponade for placenta previa
Arterial embolization under fluoroscopic guidance centa edge to the internal os was less than 2 cm. Of 37
requires expertise in interventional radiology and spe- patients, four patients (11%) required hysterectomy
cialized equipment, although the success rate is high because the placenta did not separate from the uterus
and the procedure has the potential to preserve fertil- due to placenta accretion. Six patients (16%) had no
ity. This procedure is limited to centers with a high major troubles because the placenta separated
degree of expertise.3 promptly and bleeding was controlled easily. In the
Nowadays, the use of intrauterine balloons has been remaining 27 cases, after delivery of the placenta, PPH
well described in the literature for the control of originating from the placental site continued to be
massive post-partum hemorrhage (PPH) due to atonic resistant to medical therapies, which included intrave-
uterus not responding to oxytocics such as prostaglan- nous infusions of oxytocin (1020 U), intravenous ergo-
dins.4 Placement of a uterine balloon tamponade Foley,5 metrine (0.5 mg), intra muscular prostaglandin F2a or
Bakri balloon,6 or Sengstaken-Blakemore tube (SB- rectal insertion of misoprostol (400 mg). In 10 of those
tube),7 which may be inserted either after cesarean with no response to these medical treatments, the
section or vaginal delivery, is an option with interesting SB-tube was inserted into the uterine cavity during the
advantages, and is thus often preferred to gauze operation. The insertion of the tube was performed by
packing. Placement of a uterine balloon can act as a a single qualified operator (K. S.). In the remaining 17
diagnostic test to screen those women who need hys- cases, rolled gauze was used to control severe PPH.
terectomy. In addition, it minimizes the risk of occult The insertion of SB-tube was based on the method
bleeding and removal of the balloon is not a painful reported by Condous et al.10 Briefly, after cutting the
procedure. However, the efficacy of the use of intrau- distal end of the tube beyond the balloon, the insertion
terine balloon in PPH after cesarean section compli- was facilitated by grasping the anterior and lateral
cated by placenta previa remains unclear because only margins of the cervix with sponge forceps and placing
a small series of a few cases have been reported.8,9 the esophageal or stomach balloon into the uterine
With these points in mind, we analyzed the clinical cavity via the cervix. The balloon was positioned to fit
outcomes of uterine tamponade with SB-tube for the the cervix of the uterus and inflated with 200300 mL
treatment of severe PPH due to placenta previa in a of saline as appropriate for the uterine size. Applying
larger series. In all 10 cases analyzed, hemostasis was gentle traction confirmed that the SB-tube was firmly
adequately achieved after the insertion of the tube and fixed in situ in the uterine cavity and good control of
no patient required any further invasive surgical pro- the hemorrhage was provided. A representative picture
cedures. Uterine balloon-tamponade was highly effec- of the procedure is shown in Figure 1. The hysterotomy
tive in controlling PPH originating from the placental incision was carefully sutured with VicrylR 10 without
site and should be considered as the first step in order entrapping the balloon. Broad-spectrum antibiotic
to reduce undesirable hysterectomy.
Methods
Between January 2007 and December 2009, there were
1731 deliveries in the Perinatal Medical Center of
Osaka University Hospital (Osaka, Japan). Of these, 37
(2.1%) underwent caesarian section due to placenta
previa/low-lying placenta. All were Asian, aged
2741 years and from a middle-class community in
Osaka or Hyogo prefecture in Japan. Since our unit
accepts high-risk pregnant women who can not be
treated in usual neighborhood hospitals, the percent-
age of placenta previa/low-lying placenta was rela-
tively high. Placenta previa was diagnosed by
transvaginal ultrasonography in late pregnancy and it
was confirmed that the placental edge overlapped the
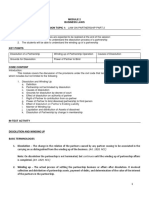
internal cervical os just before the operation. Low-lying Figure 1 A representative picture of Sengstaken-
placenta was diagnosed when the distance of the pla- Blakemore tube inserted from hysterotomy incision.
2011 The Authors 103
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
T. Ishii et al.
therapy was systematically used just before the
Postoperative
operation in all cases. In several cases, prophylactic
antibiotics were used after the procedure based on the
operators decision. The blood drainage was collected
fever
Yes
through the distal end of the shaft by attaching a col-
No
No
No
No
No
No
No
No
No
lection bag, and closely observed. SB-tube was
after operation
removed 24 h after the operation and complete hemo-
stasis was confirmed.
Antibiotics
Clinical data were collected from medical records.
The clinical, biochemical and hematological data were
Yes
Yes
Yes
Yes
Yes
Yes
No
No
No
No
recovered together with data on age, number of preg-
nancies, parity, gestational age, duration of time
Transfusion
between delivery of baby and placenta, estimated
RCC 8U
RCC 6U
blood loss and volume of blood transfused. Postopera-
None
None
None
None
None
None
None
None
tive fever was defined as a temperature rise above 38C
maintained over 24 h or recurring during the period
from the 1st to the 10th day after childbirth.
loss (mL)
Drainage
Statistical analysis was performed with Stat View
blood
(Abacus Conceptus Inc, Berkeley, CA, USA). Statistical
120
56
121
40
170
40
320
140
125
125
differences between groups were analyzed by Kruskal-
Wallis test along with post hoc test (Scheffes test).
Estimated
loss (mL)
Table 1 Summary of clinical outcomes of the patients who used Sengstaken-Blakemore tube
blood
3160
1000
3220
1300
1500
1700
1360
1450
2830
2780
Result
Balloon tamponade with SB-tube was used in a total of baby delivery and
Duration between
10 patients during cesarean section due to uterine hem- placenta delivery
orrhage resistant to medical therapy. The clinical out-
comes of those 10 patients are summarized in Table 1.
Complete hemostasis was achieved in all cases. The
5 min
1 min
2 min
4 min
4 min
8 min
5 min
4 min
6 min
2 min
drainage blood was continuously monitored until the
next morning after the operation. The median drainage
blood until the next morning was 125.7 81.3 (40320)
Low lying placenta
Low lying placenta
mL. The median age of the women was 34.3 2.8 years.
Previa totalis
Previa totalis
Previa totalis
Previa totalis
Previa totalis
Previa totalis
Previa totalis
Previa totalis
The median gestational age was 36.5 weeks of gestation.
Position of
Six women (60%) were nulliparas and three were para 1.
placenta
The median birth weight was 2.74 0.21 kg and none of
the neonates had apparent congenital abnormalities.
The median bleeding during the operation was
2030 860 mL. Two cases (cases 1 and 3) required
Gestation
37w0d
36w1d
36w3d
34w6d
36w3d
37w3d
36w5d
36w6d
37w0d
36w0d
transfusion due to massive bleeding during the opera-
tions. One (case 5) experienced postoperative fever.
There were no severe adverse events in any cases and
and parity
no further invasive surgical procedures were required.
Gravidity
RCC, red cell concentrate.
Next, we compared clinical outcomes among the
G4P0
G2P1
G5P4
G2P0
G2P0
G1P0
G2P0
G2P1
G1P0
G2P1
treatment options employed in Table 2. The median
blood loss of six patients who required no further treat-
ments was 935 271 mL and significantly lesser than
Age
(y)
37
30
34
34
35
29
37
37
36
34
that of rolled gauze (P = 0.043). The median bleeding
during the operation was 2030 860 mL in the patients
Case
No.
who used SB-tube and 2241 1378 mL in those that
1
2
3
4
5
6
7
8
9
10
used the gauze. No significant differences were noted
104 2011 The Authors
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
Balloon tamponade for placenta previa
Table 2 The summary of clinical outcomes of the cases of cesarean section due to placenta previa
Sengstaken- Rolled No Hysterectomy
Blakemore tube gauze treatment required
Number 10 17 6 4
Age (y) 34.3 2.8 33.7 5.2 35.0 2.4 35.3 4.0
Previous cesarean section 0/10 2/17 1/6 4/4
Previous myomectomy 1/10 1/17 0/6 0/4
Estimated blood loss (mL) 2030 860 2241 1378 935 271 3300 1764
Uterine artery embolization required 0/10 1/17 0/6 N.A.
Transfusion 2/10 3/17 0/6 3/4
Postoperative fever 2/10 8/17 1/6 2/4
N.A., not applicable.
Table 3 Summary of clinical outcomes of the patients who required hysterectomy
Case Age Gravity and Previous Gestation Prenatal Estimated Transfusion Pathological
(y) parity CS diagnosis blood loss (mL) required diagnosis
1 31 G2P1 1 35w2d Yes 2900 RCC 4U Placenta percreta
2 37 G4P3 2 35w4d No 5000 RCC 8U FFP 8U Placenta accreta
3 40 G4P2 2 36w0d Yes 4300 RCC 8U Placenta accreta
4 33 G3P1 1 35w3d Yes 1000 None Placenta increta
Estimated blood loss during the initial cesarean section. CS, cesarean section; FFP, fresh frozen plasma; RCC, red cell concentrate.
between these two groups. One case of gauze packing operation day, transcatheter angiographic uterine arte-
group required uterine artery embolization due to con- rial embolization was conducted with gelatin sponge
tinuous bleeding after the procedure. In the remaining particles and platinum coils; one week later, total hys-
26 cases in which SB-tube or rolled gauze was used, terectomy was carried out. In Table 3, the blood loss
adequate hemostasis (less than 100 mL/2 h) was during the initial cesarean section was shown. In case 2,
achieved soon after the insertion and no further treat- although the placenta was partially separated spontane-
ments were required. Two cases (20%) of SB-tube ously, the other part of placenta was tightly attached to
group and three cases (18%) of gauze packing required the uterine wall and massive bleeding occurred. Since
transfusion due to massive bleeding during the opera- the operator considered it was not possible to control
tions. Two (20%) of the SB-tube group and eight (47%) bleeding, the hysterectomy was emergently performed.
of gauze group experienced postoperative fever. Both
uterine gauze packing and balloon-tamponade were Discussion
similarly effective in controlling PPH, and there were
no severe adverse events (i.e. severe infectious symp- Post-partum hemorrhage in cases of placenta previa
toms) in any cases. remains a serious obstetric complication. Successful
In Table 3, the clinical outcomes of the cases required control of bleeding can often be achieved medically
hysterectomy are summarized. In case 1, 3 and 4, pla- using uterotonics including oxytocin, ergometrine,
centa accrete was strongly suspected prenatally by MRI 15-methyl prostaglandin F2a and misoprostol.9
and Doppler ultrasonography. Since a 25% to 50% inci- However, once these medical treatments fail, it is often
dence of placenta accreta in patients with placenta necessary to intervene surgically with uterine or inter-
previa with prior cesarean delivery has been well nal iliac ligation, uterine compression sutures or hys-
recognized, the patient and her family agreed with hys- terectomy. When dealing with young women who may
terectomy when placenta was not separated spontane- wish to have more children, the cesarean-hysterectomy
ously. In case 4, to avoid the risk of hemorrhage, we without delay, resulting in devastating emotional
scheduled and performed stepwise treatment sug- and/or cultural consequences, should be avoided
gested by Sumigama et al. in Nagoya University.11 The wherever possible.12 Actually, in our reports, six
brief procedure was as follows: a cesarean section was women were nulliparas and all 10 cases who used
performed without separation of the placenta; on the SB-tube strongly wished to preserve fertility.
2011 The Authors 105
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
T. Ishii et al.
While a variety of surgical techniques have been pro- tamponade balloon in two cases of placenta previa
posed to avoid hysterectomy, a suitable conservative together with additional surgical procedures such as
technique is still lacking in the literature and all the bilateral hypogastric ligation.6 Recently, Condous et al.
advantages shown by the proposed options are coun- reported the use of SB-tube in the management of
terbalanced by some risks.2 Herein, we described that PPH.10 In this series of 17 cases, two patients experi-
not only uterine gauze packing but uterine balloon enced severe PPH complicated by placenta previa but
tamponade with a SB-tube showed similarly high effi- were successfully treated without any further invasive
cacy in controlling PPH originating from the placental procedures. Those reports offer evidence that further
site of the lower uterine segment during caesarian sec- clinical attention should be given to this procedure,
tions. Historically, the use of uterine gauze packing in and herein we reported a larger series of 10 cases and
the management of PPH fell into disfavor after the demonstrated that intrauterine balloon tamponade
1960s, following concerns of concealing ongoing hem- should be considered as a management option before
orrhage, development of infection and its non- performing surgical procedures in PPH resulting from
physiological approach.13 Condous et al. commented, placental site bleeding.
based on their experiences, that uterine packing with In this report, uterine tamponade with SB-tube con-
gauze packs is outdated and should only be reserved in trolled PPH during cesarean section for placenta previa
cases when a balloon catheter is unavailable.10 Control in all 10 patients, although the success rate of uterine
of PPH by uterine balloon packing itself is not a new balloon tamponade as a single measure for the man-
idea. Although some of the balloons, such as the Rusch agement of major PPH has been reported as 77.588.8%
balloon and the condom catheter, are reported to be in a recent systematic review.13 One possible reason for
effective,14 they do not allow blood drainage from the this discrepancy is that the use of a balloon tamponade
uterine cavity. On the contrary, in SB-tube system, the has been reported in the management of severe PPH
blood drainage is collected through the distal end of mainly resulting from uterine atony. In our experience,
the shaft by attaching a collection bag. This drainage a balloon tamponade is more effective in cases of
system helps prevent blood collection inside the placenta previa than those of uterine atony. The intrau-
uterine cavity and provide an accurate estimation of terine balloon is considered to act by exerting in
bleeding. Besides, if the procedure fails to stop the inward-to-outward pressure that is greater than the
bleeding, the failure is immediately visible, as opposed systemic arterial pressure to prevent continual bleed-
to the use of the conventional balloons as tamponade. ing.18 Since the uterine cavity itself is well contracted in
With these reasons, we consider SB-tube system to be cases of placenta previa, adequate inward-to-outward
superior to the other treatment options such as rolled pressure produced by the tube is likely to be achieved
gauze or the conventional balloon. easily. In addition, by halting ongoing hemorrhage
Reports are accumulating suggesting that methods from the placental bed promptly during the operation,
of uterine tamponade are effective to avoid hysterec- consumptive coagulopathy can be reversed in most
tomy in frequently unstable patients and can preserve cases. Further data from a larger prospective study are
fertility, especially in the case of severe PPH secondary needed to verify our hypothesis.
to uterine atony.15 A recent American College of Obste- One possible problem with using the SB-tube for
tricians and Gynecologists practice bulletin suggests placenta previa is that it takes some time to insert the
that tamponade of the uterus can be an effective way to SB-tube because it must be inserted into the uterine
decrease hemorrhage secondary to uterine atony, and cavity transvaginally during the operation. The
procedures such as uterine artery ligation or B-Lynch SB-tube has two separated drainage catheters with
suture may be used to obviate the need for hysterec- attached parts, which might cause further tearing of
tomy. Furthermore, it is suggested that if hysterectomy the lower uterine segment if inserted through the hys-
is performed for uterine atony, there should be docu- terotomy incision because the uterine cervical canal of
mentation of these therapies attempts.16 On the other the patients is usually almost closed in cases of pla-
hand, the use of a balloon tamponade in severe PPH centa previa. Since PPH occurs immediately after the
due to placenta previa has been reported only in a placenta is delivered, even a few minutes of lost time
small series of a few cases. Bowen et al. reported the might cause additional bleeding. In that sense, the
first attempt to archive hemostasis in case of PPH com- more simple and flexible tamponade balloon, which is
plicated by placenta previa by compression using a specially designed for a uterus and can be inserted
Foley catheter.17 Bakri et al. used a self-made original through the hysterotomy incision, might decrease
106 2011 The Authors
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
Balloon tamponade for placenta previa
PPH during the operation. Indeed, the SOS Bakri 5. De Loor JA, van Dam PA. Foley catheters for uncontrollable
Tamponade Balloon Catheter is designed just for obstetric or gynecologic hemorrhage. Obstet Gynecol 1996; 88:
737.
the uterus and is reported easily administered,
6. Bakri YN, Amri A, Abdul Jabbar F. Tamponade-balloon for
although this type of catheter is not commercially obstetrical bleeding. Int J Gynaecol Obstet 2001; 74: 139142.
available in Japan. Such an improved device should 7. Katesmark M, Brown R, Raju KS. Successful use of a
be examined to achieve better outcomes in cases of Sengstaken-Blakemore tube to control massive postpartum
severe PPH. haemorrhage. Br J Obstet Gynaecol 1994; 101: 259260.
8. Seror J, Allouche C, Elhaik S. Use of Sengstaken-Blakemore
In conclusion, the uterine balloon-tamponade was
tube in massive postpartum hemorrhage: A series of 17 cases.
effective in controlling PPH originating from the pla- Acta Obstet Gynecol Scand 2005; 84: 660664.
cental site, although our results are from a retrospec- 9. Ferrazzani S, Guariglia L, Triunfo S, Caforio L, Caruso A.
tive study of a small series. This method is very Successful treatment of post-cesarean hemorrhage related to
effective, simple to use, scarcely invasive, and available placenta praevia using an intrauterine balloon. Two case
reports. Fetal Diagn Ther 2006; 21: 277280.
at a low cost for all maternity wards. It should be con-
10. Condous GS, Arulkumaran S, Symonds I, Chapman R,
sidered as the first step in order to reduce undesirable Sinha A, Razvi K. The tamponade test in the management
hysterectomy. of massive postpartum hemorrhage. Obstet Gynecol 2003; 101:
767772.
11. Sumigama S, Itakura A, Ota T et al. Placenta previa increta/
Acknowledgments percreta in Japan: A retrospective study of ultrasound find-
ings, management and clinical course. J Obstet Gynaecol Res
This work was supported in part by a Grant-in-Aid for 2007; 33: 606611.
scientific research from the Ministry of Education, 12. Tshibangu KC, de Jongh MA, Mamabolo MY, Peranovic V,
Sooboo VM. Surgical conservation of the uterus in the man-
Science, Sports and Culture of Japan. The authors are agement of third-trimester placenta percreta using tubal and
grateful to Remina Emoto and Ayako Okamura for uterine artery ligation and uterine packing. S Afr Med J 2004;
their secretarial assistance. 94: 180182.
13. Dildy GA, 3rd. Postpartum hemorrhage: New management
options. Clin Obstet Gynecol 2002; 45: 330344.
References 14. Georgiou C. Balloon tamponade in the management of post-
partum haemorrhage: A review. BJOG 2009; 116: 748757.
1. Maier RC. Control of postpartum hemorrhage with uterine 15. Tamizian O, Arulkumaran S. The surgical management of
packing. Am J Obstet Gynecol 1993; 169: 317321; discussion postpartum haemorrhage. Curr Opin Obstet Gynecol 2001; 13:
2123. 127131.
2. Zaki ZM, Bahar AM, Ali ME, Albar HA, Gerais MA. Risk 16. ACOG Practice Bulletin. Clinical Management Guidelines for
factors and morbidity in patients with placenta previa accreta Obstetrician-Gynecologists Number 76, October 2006: Post-
compared to placenta previa non-accreta. Acta Obstet Gynecol partum hemorrhage. Obstet Gynecol 2006; 108: 10391047.
Scand 1998; 77: 391394. 17. Bowen LW, Beeson JH. Use of a large Foley catheter balloon
3. Doumouchtsis SK, Papageorghiou AT, Arulkumaran S. Sys- to control postpartum hemorrhage resulting from a low pla-
tematic review of conservative management of postpartum cental implantation. A report of two cases. J Reprod Med 1985;
hemorrhage: What to do when medical treatment fails. Obstet 30: 623625.
Gynecol Surv 2007; 62: 540547. 18. Cho Y, Rizvi C, Uppal T, Condous G. Ultrasonographic visu-
4. Condie RG, Buxton EJ, Payne ES. Successful use of alization of balloon placement for uterine tamponade in
Sengstaken-Blakemore tube to control massive postpartum massive primary postpartum hemorrhage. Ultrasound Obstet
haemorrhage. Br J Obstet Gynaecol 1994; 101: 10231024. Gynecol 2008; 32: 711713.
2011 The Authors 107
Journal of Obstetrics and Gynaecology Research 2011 Japan Society of Obstetrics and Gynecology
You might also like
- OutDocument7 pagesOutMario AlexanderNo ratings yet
- Yang Et Al-2006-Ultrasound in Obstetrics & GynecologyDocument5 pagesYang Et Al-2006-Ultrasound in Obstetrics & GynecologyMario AlexanderNo ratings yet
- Ishii Et Al-2012-Journal of Obstetrics and Gynaecology ResearchDocument6 pagesIshii Et Al-2012-Journal of Obstetrics and Gynaecology ResearchMario AlexanderNo ratings yet
- 82 241 1 PB PDFDocument3 pages82 241 1 PB PDFMario AlexanderNo ratings yet
- Tinnitus Ringing in The EarsDocument11 pagesTinnitus Ringing in The EarsWibi GunawanNo ratings yet
- 310 615 1 SMDocument8 pages310 615 1 SMMario AlexanderNo ratings yet
- SelulitisDocument12 pagesSelulitisMario AlexanderNo ratings yet
- PBL Blok26 MarioDocument26 pagesPBL Blok26 MarioMario AlexanderNo ratings yet
- PBL Paradigma SehatDocument6 pagesPBL Paradigma SehatMario AlexanderNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Equity Inv HW 2 BHDocument3 pagesEquity Inv HW 2 BHBen HolthusNo ratings yet
- Episode 8Document11 pagesEpisode 8annieguillermaNo ratings yet
- ModalsDocument13 pagesModalsJose CesistaNo ratings yet
- Environmental Science PDFDocument118 pagesEnvironmental Science PDFJieyan OliverosNo ratings yet
- Preparation For Exercise1-1 CompleteDocument28 pagesPreparation For Exercise1-1 CompleteSimon GranNo ratings yet
- What Blockchain Could Mean For MarketingDocument2 pagesWhat Blockchain Could Mean For MarketingRitika JhaNo ratings yet
- Module 6: 4M'S of Production and Business ModelDocument43 pagesModule 6: 4M'S of Production and Business ModelSou MeiNo ratings yet
- Improve Your Social Skills With Soft And Hard TechniquesDocument26 pagesImprove Your Social Skills With Soft And Hard TechniquesEarlkenneth NavarroNo ratings yet
- Astrology - House SignificationDocument4 pagesAstrology - House SignificationsunilkumardubeyNo ratings yet
- HERBAL SHAMPOO PPT by SAILI RAJPUTDocument24 pagesHERBAL SHAMPOO PPT by SAILI RAJPUTSaili Rajput100% (1)
- Business Law Module No. 2Document10 pagesBusiness Law Module No. 2Yolly DiazNo ratings yet
- MVD1000 Series Catalogue PDFDocument20 pagesMVD1000 Series Catalogue PDFEvandro PavesiNo ratings yet
- BCIC General Holiday List 2011Document4 pagesBCIC General Holiday List 2011Srikanth DLNo ratings yet
- 2020 Book WorkshopOnFrontiersInHighEnerg PDFDocument456 pages2020 Book WorkshopOnFrontiersInHighEnerg PDFSouravDeyNo ratings yet
- Cost Allocation Methods & Activity-Based Costing ExplainedDocument53 pagesCost Allocation Methods & Activity-Based Costing ExplainedNitish SharmaNo ratings yet
- 2C Syllable Division: Candid Can/dDocument32 pages2C Syllable Division: Candid Can/dRawats002No ratings yet
- Opportunity, Not Threat: Crypto AssetsDocument9 pagesOpportunity, Not Threat: Crypto AssetsTrophy NcNo ratings yet
- 2015 Ssang Yong Rexton Y292 Service ManualDocument1,405 pages2015 Ssang Yong Rexton Y292 Service Manualbogdanxp2000No ratings yet
- 4AD15ME053Document25 pages4AD15ME053Yàshánk GøwdàNo ratings yet
- IJAKADI: A Stage Play About Spiritual WarfareDocument9 pagesIJAKADI: A Stage Play About Spiritual Warfareobiji marvelous ChibuzoNo ratings yet
- Supreme Court declares Pork Barrel System unconstitutionalDocument3 pagesSupreme Court declares Pork Barrel System unconstitutionalDom Robinson BaggayanNo ratings yet
- Red Orchid - Best PracticesDocument80 pagesRed Orchid - Best PracticeslabiaernestoNo ratings yet
- Note-Taking StrategiesDocument16 pagesNote-Taking Strategiesapi-548854218No ratings yet
- Autos MalaysiaDocument45 pagesAutos MalaysiaNicholas AngNo ratings yet
- 1 - Nature and Dev - Intl LawDocument20 pages1 - Nature and Dev - Intl Lawaditya singhNo ratings yet
- Tadesse JaletaDocument160 pagesTadesse JaletaAhmed GemedaNo ratings yet
- Ghaziabad Resume Amresh Kumar Upadhyay Desktop EngineerDocument2 pagesGhaziabad Resume Amresh Kumar Upadhyay Desktop EngineerRipunjay MishraNo ratings yet
- Page 17 - Word Connection, LiaisonsDocument2 pagesPage 17 - Word Connection, Liaisonsstarskyhutch0% (1)
- Product Packaging, Labelling and Shipping Plans: What's NextDocument17 pagesProduct Packaging, Labelling and Shipping Plans: What's NextShameer ShahNo ratings yet
- HERMAgreenGuide EN 01Document4 pagesHERMAgreenGuide EN 01PaulNo ratings yet